Abstract
Objective
The authors performed a retrospective study to assess the accuracy and clinical benefits of a navigation coupled with O-arm® system guided method in the thoracic and lumbar spines by comparing with a C-arm fluoroscopy-guided method.
Methods
Under the navigation guidance, 106 pedicle screws inserted from T7 to S1 in 24 patients, and using the fluoroscopy guidance, 204 pedicle screws from T5 to S1 in 45 patients. The position of screws within the pedicle was classified into four groups, from grade 0 (no violation cortex) to 3 (more than 4 mm violation). The location of violated pedicle cortex was also assessed. Intra-operative parameters including time required for preparation of screwing procedure, times for screwing and the number of X-ray shot were assessed in each group.
Results
Grade 0 was observed in 186 (91.2%) screws of the fluoroscopy-guided group, and 99 (93.4%) of the navigation-guided group. Mean time required for inserting a screw was 3.8 minutes in the fluoroscopy-guided group, and 4.5 minutes in the navigation-guided group. Mean time required for preparation of screw placement was 4 minutes in the fluoroscopy-guided group, and 19 minutes in the navigation-guided group. The fluoroscopy-guided group required mean 8.9 times of X-ray shot for each screw placement.
Conclusion
The screw placement under the navigation-guidance coupled with O-arm® system appears to be more accurate and safer than that under the fluoroscopy guidance, although the preparation and screwing time for the navigation-guided surgery is longer than that for the fluoroscopy-guided surgery.
Keywords: Cervical trauma, Sub-axial injury classification scale, Cervical spine injury, Interobserver agreement, Intraobserver reliability
INTRODUCTION
Since Magerl17) first placed trans-pediclular screw, pedicle screw placement has been considered as an indispensable procedure of spine surgery. Pedicle screw placement has been used to obtain immediate stabilization of the pathologic segment after surgery while the arthrodesis occurs. For safe placement of screws, various conventional techniques have been introduced focusing on the anatomical landmarks, entry point and insertion angle. However, misplacement rates of conventional techniques with or without X-ray guidance still have been noted up to 30% in the lumbar spine and up to 55% in the thoracic spine9,10,29,30). Misplacement of screw has a potential to violate neural, vascular, and visceral structures, which it may cause serious complication. To improve accuracy of pedicle screw placement, new methods using computer systems allowing real time image processing have been explored since early 1990s1,9,10,15,17,22,24-27,29). This computer-assisted navigated surgery is expected to carry out the precise placement of instruments by providing real time information of unexposed or partially exposed spinal structures.
O-arm® system (Medtronic, CO, USA) is one of the latest intraoperative imaging platforms to allow real-time multi-dimensional surgical imaging optimized for orthopedic or spine surgeries (Fig. 1). This system could simply interface with the navigation systems (Stealth Station®, Medtronic, CO, USA) providing the surgeon with information about the patient's anatomy for accurate placement of implants with minimum radiation exposure.
Fig. 1.
O-arm® system.
The authors have performed a prospective study to assess the accuracy and clinical benefits of a navigation coupled with O-arm® guided method in the placement of pedicle screw in the thoracic and lumbar spines by comparing with conventional fluoroscopy guided method since 2008. And, as far as we know, there has been no report of comparison between conventional C-arm fluoroscopy and navigation coupled with O-arm® guided methods.
MATERIALS AND METHODS
Data sampling
From January 2009 to July 2009, the patients who had thoracic or lumbar spine pathology required pedicle screw placement were enrolled in the present study under a pre-designed controlled protocol. During the first 4 months, pedicle screw placements were consecutively conducted under the fluoroscopy-guidance, and during the rest 2 months which O-arm® system was able to use, all surgeries were performed under the navigation guidance.
Surgical procedures
Single surgeon (K. S. R.) had placed all pedicle screws (Legacy system®, Medtronic, CO, USA). Posterior incision, muscle dissection, decompression and/or interbody fusion were performed in all patients. In the fluoroscopy-guided group, pedicle screw placement under the conventional fluoroscopy guidance was carried out. The entry point was defined by determining the anatomical landmarks such as transverse process, lateral facet border. The trajectory of screw insertion was confirmed with lateral fluoroscopic imaging. After determining the cancellous part within the pedicle by using pedicle sounder, sequentially, tapping, and screw placement were performed. The screw diameter varied from 5.5 to 7.5 mm according to the operated level. Finally, AP and lateral fluoroscopic images were obtained to check whether the screws were positioned properly or not.
In the navigation-guided group, the reference frame was clamped to the spinous process of the nearest vertebra to place the pedicle screws just before introducing O-arm® system to the radiolucent operation table. After O-arm® system was brought into the operation field and linked to the navigation system, 3-dimensional (3D) computed tomography (CT) images of target levels were obtained. Ordinary, minimally four segments of the spine could be checked by single scanning. O-arm® system was parked to allow maximum space of the surgical field for the operator and assist. The obtained images were automatically transferred and registered to the navigation system through a network connection, and immediate navigation was allowable at the navigation system in the axial, coronal, and sagittal planes. By using a navigated pointer, ideal entry point and trajectory of pedicle screws were defined. Preparing entry point with awl, probing, tapping and screw placement were sequentially performed by using a guider set-up for navigation with a tracking array and following the information of multiplanar images on the navigation display (Fig. 2). The diameter of screw was ranged from 5.5 to 7.5 mm according to the operated level.
Fig. 2.
Intraoperative photography showing the pedicle screw placement under the navigation guidance. Ideal entry point and trajectory of pedicle screws were defined by using a navigated pointer. Preparing entry point with awl, probing, tapping and screw placement were sequentially performed by using a guider set-up for navigation with a tracking arrayand following the information of multiplanar images on the navigation display.
Data assessment
By using postoperative high resolution CT scans, the position of pedicle screws after placement was analyzed. According to postoperative findings on the CT scan, the position of screw was classified into four groups : Group A : perfectly within the pedicle; Group B : violation the cortex less than 2 mm; Group C : violation the cortex 2-4 mm; Group D : violation the cortex more than 4 mm9,19). If the cortical violation by screw was noticed, the location of violated pedicle cortex was evaluated. Intraoperative parameters including preparation time of each image guiding system for screwing procedure, screwing time and number of total X-ray shots in each screwing procedure were assessed.
Statistical verification was determined using SPSS for Windows (version 11.0.1; SPSS Inc., Chicago, IL, USA). A p-value <0.05 was statistically significant.
RESULTS
Total 69 patients included in the present study. Forty-five patients underwent pedicle screws placement using the fluoroscopy. The fluoroscopy-guided groups included 21 males and 24 females (mean age 59.4 years, ranged from 33 to 72). Twenty-four patients were performed pedicle screw placement using the navigation. The navigation-guided group consisted of 10 males 14 females (mean age 57.7 years, ranged from 39 to 76). Fifty-six patients were diagnosed as degenerative spine diseases. Nine metastatic spine tumors and 4 spine traumas were treated with pedicle screw placement.
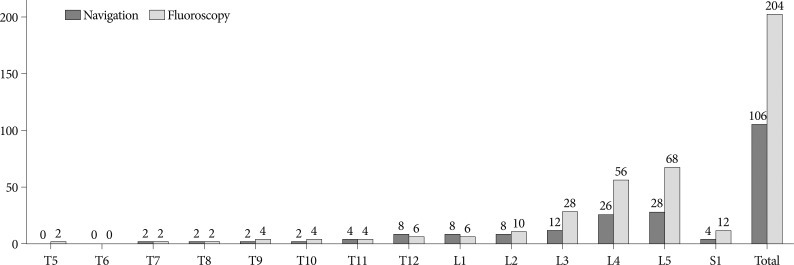
Using the fluoroscopy, 204 pedicle screws were placed from T5 to S1, and using the navigation, 106 pedicle screws inserted from T7 to S1. Distribution of the level operated in each group was shown on Fig. 3.
Fig. 3.
Bar graphs showing the distribution of the level operated in each group.
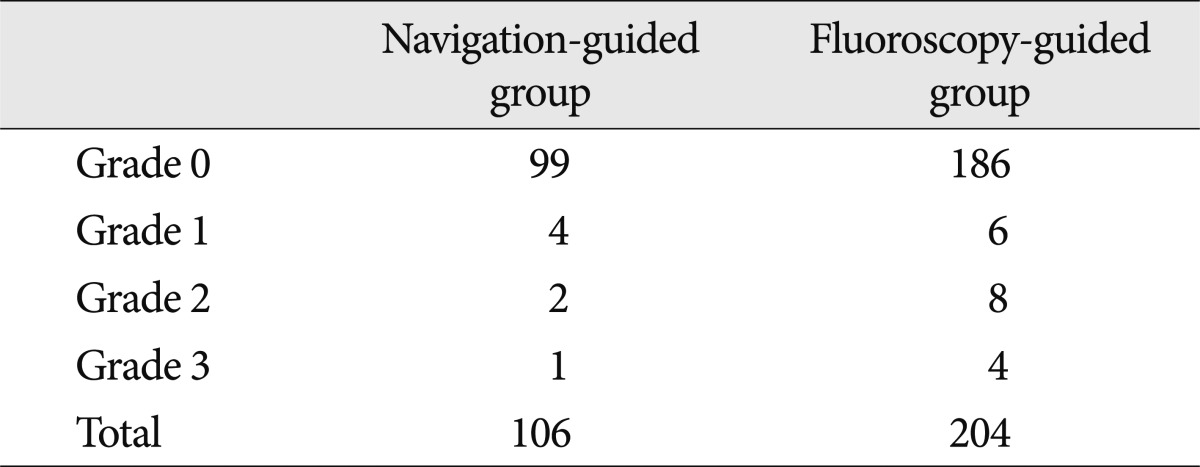
In the fluoroscopy-guided group, 186 (91.2%) were observed among in grade 0; whereas in the navigation-guided group, 99 (93.4%). Eighteen screws in the fluoroscopy-guided group violated the pedicle cortex, and 7 screws in the navigation-guided group. The distribution of misplaced screws in each group was listed on Table 1. Statistically, the fluoroscopy-guided group showed more frequent occurrence of a misplaced screw than the navigation-guided group (p<0.05, χ2 test). Regarding the position of the violated cortex, inferior cortex was most commonly involved on each group [the fluoroscopy-guided group; 9 (50%), the navigation-guided group; 4 (57.1%)]. In the fluoroscopy-guided group, there was no lateral cortex violation, and no medial cortex violation was observed in the navigation-guided group (Table 2).
Table 1.
Distribution of screws position
Table 2.
Distribution of violated cortex by the misplaced screw
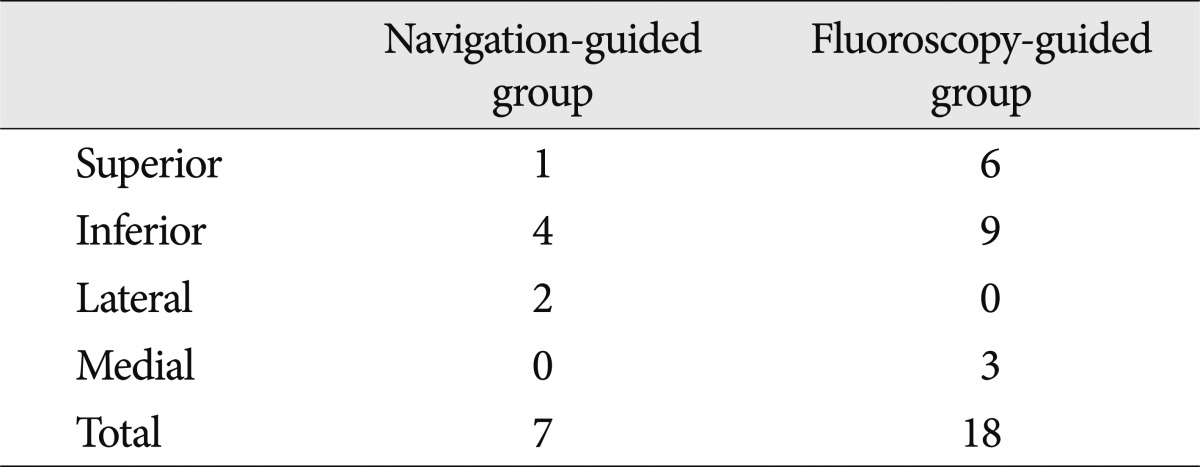
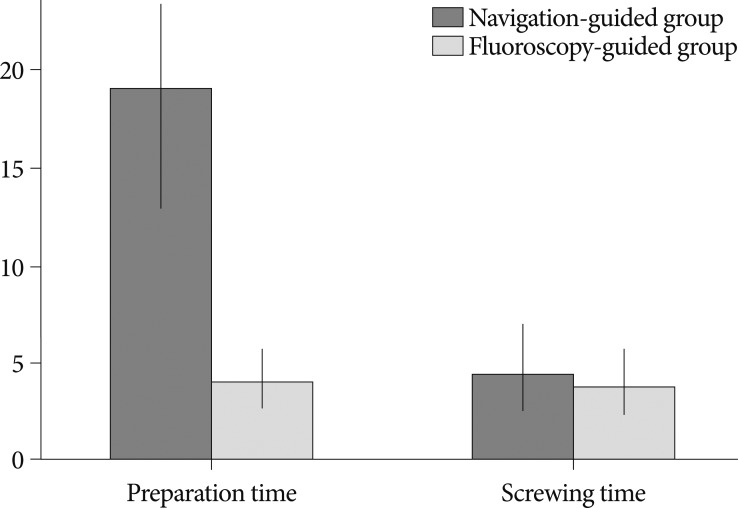
Intraoperative parameters were shown on Fig. 4. Mean preparation time for screw placement was about 4 minutes in the fluoroscopy-guided, and 19 minutes in the navigation-guided group. Longer preparation time was required in the navigation-guided group (p<0.05, t-test). Each screwing time was 1 to 12.8 minutes (average 3.8 minutes) in the fluoroscopy-guided group and 1.3 to 7.9 minutes (average 4.5 minutes) in the navigation-guided group. The navigation-guided group took more time in screwing procedure (p<0.05, t-test). Mean number of X-ray shot for each screw placement in the fluoroscopy-guided group was 8.9, while there was no radiation exposure during the screw placement procedure in the navigation-guided group.
Fig. 4.
Bar graphs showing mean preparation time for screw placement and screwing time in each group.
Postoperatively, 5 patients were operated using the fluoroscopy presented transient leg paresthesia related to misplacement of screw. Among them, one patients required reoperation for the reposition of screw. In the meantime, one patient using the navigation presented transient leg paresthesia correlated with intraoperative screw malposition postoperatively, which had been identified and corrected during operation.
DISCUSSION
With advance in computer technology, navigated operative techniques have been widely applied to various surgical fields. In instrumented spine surgery, navigated surgery has also evolved from the conventional surgery under serial radiography or C-arm fluoroscopy guidance.
Since early 1990s, a number of image guided navigation systems for the spine surgery have been introduced and clinically attempted1-4,6,7,9,10,14,16-18,20,21,23,24,26,27,29). Basically, most of those systems are CT-based units, which require registering the preoperative CT scans to the navigation workstation. Using skin surface markers for registration was a first try to apply navigation system in spine surgery. Roessler et al.21), noted the clinical results of 4 cases of frameless stereotactic navigated spinal surgery registered using skin surface markers. According to their results, the average accuracy was over 11.3 mm (range 5-20), thus it was to abandon the clinical use. Use of anatomical fiducial markers with dynamic reference array (DRA) has improved the accuracy of registration procedure. The reference frame (anatomical fiducial markers) is directly attached to a bony structure of the spine, and interacts with DRA. These tools contribute reduce the registration error by providing the flexible information of ever-changing bony anatomy during operation. However, preoperative CT scans should be obtained with the patient in one position (usually supine), which would be different to the real operating position. Dissimilarity between the positions could make a registration error causing by the alteration of intersegmental relation, then it could increase a risk of inaccurate placement of instruments. In cases of spinal instability such as unstable spondylolithesis or traumatic fractures, the disparity of intersegmental relation would be wider according to the body positions. In these conditions, the navigated surgery using the preoperative data would be inaccurate.
Emerging fluoroscopy-based navigation system using the conventional C-arm fluoroscope is expected to avoid the registration errors by providing real-time visualization during operation4,20). However, the images are limited in two-dimensional, which do not offer the information of the axial images. Thus, in cases of severe deformed spine, defining the exact configuration of the target anatomy by observing only 2-dimensional views would be difficult. Moreover, fluoroscopy-based procedure does not assure the reduction of occupational radiation exposure as much as CT-based navigation.
Kosmopoulos and Schizas15), had conducted a meta-analysis of the published literature to compare the accuracy of with-navigation and without-navigation pedicle screw placement in the human spine. They reported that, in thoracic spine, a median accuracy of the with-navigation subgroup (82.2%) was significantly lower than that of the without-navigation subgroup (94.3%), although overall accuracy (from cervical to lumbar) of the with-navigation subgroup was higher than that of the without-navigation subgroup (95.2% vs. 90.3%). In their study, most articles of the with-navigation subgroup had focused on CT-based or fluoroscope-based navigation. Regarding those results, the navigated surgery using preoperative CT or fluoroscope is not comparable to the conventional surgery especially in thoracic spine.
Recently, 3D fluoroscopy navigation systems have been merged and clinically used13,28,31). These systems are aimed at offering real-time 3D reconstructive images and obviating a need of a registration procedure by the immediate incorporation with a workstation. Isocenteric fluoroscopy automatically rotates around the patient positioned on the operating table, and automated images acquisition is undertaken. The obtained images are reconstructed to axial, sagittal, and coronal views, which provide the detailed information of the pertinent spinal anatomy of the patient. These images are immediately transferred to a computer workstation through an Ethernet network, and automatically registered for navigation procedure, which can save the time. And, a registration error due to the disparity of intersegmental relation between preoperative images and the intraoperative position of the preoperative CT-based system can be avoided. Lekovic et al., had compared two image guided techniques (virtual fluoroscope and isocentric C-arm 3D navigation) in thoracic pedicle screw placement of 37 patients and 277 pedicle screws, and noted that there were no statistical differences in rate or grade of cortical perforations between groups. Xu et al.30), had investigated the accuracy of three types of image-guided pedicle screw insertion (CT-based, 2D fluoroscope-based, and 3D fluoroscope-based) by a meta-analysis. According to their results, in the thoracic level, 3D-flouroscope based method obtained a median accuracy of 97.16%, compared with 90.76% for CT-based and 85.48% for 2D fluoroscope-based. However, although the clinical reports have noted the reliability of 3D fluoroscope-based navigation, there is still a concern of that the quality of reconstructive images is not proper to define the exact spine anatomy, which can reduce the accuracy of instrumentation.
O-arm® system is the latest intraoperative imaging system incorporating with a flat panel detector, which provides standard 2D fluoroscopic images and multi-planar 3D CT-quality images. Similar to the 3D fluoroscopy, all images data obtained are automatically transferred to the navigation computer workstation and automatically registered. Comparing with 3D fluoroscopy, O-arm® system has the several superiorities including high quality of multi-planar images, larger field of view, and robotic positioning. This innovative imaging system is expected to enhance the accuracy of spine instrumented surgeries.
Silbermann et al.23), recently reported the results of comparison study for assessment of accuracy in lumbo-sacral spine pedicle screw placement between free-hand and O-arm® based navigation techniques. And they noted that the accuracy rate was 94.1% in the free-hand group compared to 99% in the O-arm® navigated group. In the present study, 93.4% of screws in the navigation-guided group were perfectly located within the pedicle, comparing to 91.2% of screws in the fluoroscopy-guided group. Moreover, medial cortex violation was more frequently occurred in the fluoroscopy-guided group. Even in minor error, medial cortex violation could cause exiting nerve root irritation or injury. And in the thoracic spine, it can make serious spinal cord injury. According to the results stated above, it is clear that the navigation-guided surgery using O-arm® system is more accurate and safer than the conventional instrumented surgery.
The other major advantage of navigation-guided surgery is to minimize radiation exposure to the operator and assistants. The hazard of irradiation has been well-known, and a lot of case reports of occupational irradiation-related malignant tumors have been stated in the orthopedic or interventional medical area6,11,12,14,16,22,24,25). In the present study, mean number of X-ray shots for each screw placement in the fluoroscopy-guided group was 8.9, while there was no X-ray shot in the navigation-guided group. It is definite that the navigation-guided surgery significantly reduces the radian exposure to the operating staffs. Otherwise, there would be a concern about the radiation exposure to the patient. However, the amount of irradiation is only 60% of ordinary CT scan according to the data proposed by the manufactured company (Medtronic, USA), and it is not significantly harmful to the patient.
In using O-arm® system, there are also several shortcomings. Long preparation time is one of those. For the full setting O-arm® system, the machine should be moved to the operation table, covered with sterile plastic drape, and adjusted to the proper location to take images of targeted levels, with connecting to the navigation computer workstation as well. Carrying out all those steps could take a long time. In the present study, mean preparation time for screw placement was about 19 minutes in the navigation-guided group, compared to only 4 minutes in the fluoroscopy-guided group. At the beginning period, the authors had to spend more than 30 minutes to set O-arm® system. However, the setting time is getting shorten, and now it might spend under 15 minutes for full setting. After complete set of the navigation system, a screwing procedure did not demand much time. The present results of mean screwing time of each group showed 3.79 minutes in the fluoroscopy-guided group, and 4.45 minutes in the navigation-guided group. Even though there is statistical significance, the difference between both groups is not wide.
O-arm® system could provide the largest field of view among all kinds of intraoperative imaging systems. However, still it is not enough to operate multilevel surgery. Single scan of O-arm® system can make the images of maximum 4 levels in the lumbar spine. Therefore, for the multilevel surgeries, multiple scans should be required.
The expense of O-arm® system is one of the disadvantages. It is more expensive than any other navigation system, not to mention C arm fluoroscopy. Furthermore, O-arm® system needs a radiation shielding, larger operating room which is spacious enough to accommodate 823×2812×1933 mm sized equipment and additional staff who was trained to make machine operate is also needed.
Considering these drawbacks of O-arm® system, it is reasonable that using this system in inserting pedicle screws at lower thoracic or lumbar spine is cost-ineffective. Furthermore, the accuracy of fluoroscopy-assisted pedicle screw insertion was comparable with that of CT navigation5,8) and even free-hand technique in lumbar spine was safe and accurate23), it is unbeneficial and undesirable to using O-arm® system routinely in all transpedicular screw insertion cases, especially in lumbar spine. However, in cervical and upper thoracic spine, pedicle screw insertion is surgically demanding, risky and it would make surgeons and patients be exposed to radiation more frequently owing to anatomical difficulties such as narrow pedicle diameter and the vicinity of vital structures. Therefore, it is helpful and worth high expenses to use O-arm® system in cervical and upper thoracic spine, or in the situation of anatomical variation.
Others are common limitations of all navigation guided surgery. It is naturally complicated procedure than X-ray guided surgery. Movement of the reference frame by respiration or muscle traction can give inadequate information and result in misplacement of implant. And this frame should be fixed on the stable bony structure such as spinous process or pelvic wing. Because it is placed within the operation field, sometimes it can disturb the operation procedure. An operator or assistant may touch the frame unknowingly during operation, which it can cause loose connection and movement of the frame from original position. It can provide wrong navigation information.
Although the present study has the limitations such as a one-center and a single surgeon's series, and its retrospective nature in the small cohort, this study could demonstrate that the navigation-guided surgery using O-arm® system is more accurate and safer than the fluoroscopy-guided surgery in the thoracolumbar pedicle screw placement.
CONCLUSION
The present study demonstrates that the navigation-guided surgery using O-arm® system could substitute for the C-arm fluoroscopy-guided one for the pedicle screw placement in the thoracic and lumbar spines. The screw placement under the navigation-guidance coupled with O-arm® system appears to be more accurate and safer than that under the fluoroscopy guidance, although the preparation and screwing time for the navigation-guided surgery is longer than that for the fluoroscopy-guided surgery. Reduction of radiation exposure must be the most important advantage of navigation coupled O-arm guided method. Further larger series of prospective study is necessary to determine the comparability of the navigated spine surgery using O-arm® system.
References
- 1.Arand M, Hartwig E, Kinzl L, Gebhard F. Spinal navigation in tumor surgery of the thoracic spine : first clinical results. Clin Orthop Relat Res. 2002:211–218. doi: 10.1097/00003086-200206000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Arand M, Schempf M, Hebold D, Teller S, Kinzl L, Gebhard F. [Precision of navigation-assisted surgery of the thoracic and lumbar spine] Unfallchirurg. 2003;106:899–906. doi: 10.1007/s00113-003-0687-5. [DOI] [PubMed] [Google Scholar]
- 3.Austin MS, Vaccaro AR, Brislin B, Nachwalter R, Hilibrand AS, Albert TJ. Image-guided spine surgery : a cadaver study comparing conventional open laminoforaminotomy and two image-guided techniques for pedicle screw placement in posterolateral fusion and nonfusion models. Spine (Phila Pa 1976) 2002;27:2503–2508. doi: 10.1097/01.BRS.0000031274.34509.1E. [DOI] [PubMed] [Google Scholar]
- 4.Bolger C, Wigfield C. Image-guided surgery : applications to the cervical and thoracic spine and a review of the first 120 procedures. J Neurosurg. 2000;92:175–180. doi: 10.3171/spi.2000.92.2.0175. [DOI] [PubMed] [Google Scholar]
- 5.Choi WW, Green BA, Levi AD. Computer-assisted fluoroscopic targeting system for pedicle screw insertion. Neurosurgery. 2000;47:872–878. doi: 10.1097/00006123-200010000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Diffey BL. The risk of skin cancer from occupational exposure to ultraviolet radiation in hospitals. Phys Med Biol. 1988;33:1187–1193. doi: 10.1088/0031-9155/33/10/007. [DOI] [PubMed] [Google Scholar]
- 7.Foley KT, Smith MM. Image-guided spine surgery. Neurosurg Clin N Am. 1996;7:171–186. [PubMed] [Google Scholar]
- 8.Fu TS, Wong CB, Tsai TT, Liang YC, Chen LH, Chen WJ. Pedicle screw insertion : computed tomography versus fluoroscopic image guidance. Int Orthop. 2008;32:517–521. doi: 10.1007/s00264-007-0358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Grob D, Magerl F, McGowan DP. Spinal pedicle fixation : reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 1990;15:251. [PubMed] [Google Scholar]
- 11.Hallquist A, Hardell L, Degerman A, Wingren G, Boquist L. Medical diagnostic and therapeutic ionizing radiation and the risk for thyroid cancer : a case-control study. Eur J Cancer Prev. 1994;3:259–267. doi: 10.1097/00008469-199403030-00004. [DOI] [PubMed] [Google Scholar]
- 12.Hallquist A, Näsman A. Medical diagnostic X-ray radiation--an evaluation from medical records and dentist cards in a case-control study of thyroid cancer in the northern medical region of Sweden. Eur J Cancer Prev. 2001;10:147–152. doi: 10.1097/00008469-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Jaiswal A, Shetty AP, Rajasekaran S. Role of intraoperative Iso-C based navigation in challenging spine trauma. Indian J Orthop. 2007;41:312–317. doi: 10.4103/0019-5413.36993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones DP, Robertson PA, Lunt B, Jackson SA. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976) 2000;25:1538–1541. doi: 10.1097/00007632-200006150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy : a meta-analysis. Spine (Phila Pa 1976) 2007;32:E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 16.Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, Berrington de Gonzalez A. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat Res. 2010;174:793–808. doi: 10.1667/RR2014.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984:125–141. [PubMed] [Google Scholar]
- 18.Merloz P, Troccaz J, Vouaillat H, Vasile C, Tonetti J, Eid A, et al. Fluoroscopy-based navigation system in spine surgery. Proc Inst Mech Eng H. 2007;221:813–820. doi: 10.1243/09544119JEIM268. [DOI] [PubMed] [Google Scholar]
- 19.Mirza SK, Wiggins GC, Kuntz C, 4th, York JE, Bellabarba C, Knonodi MA, et al. Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance : a cadaver study. Spine (Phila Pa 1976) 2003;28:402–413. doi: 10.1097/01.BRS.0000048461.51308.CD. [DOI] [PubMed] [Google Scholar]
- 20.Nolte LP, Slomczykowski MA, Berlemann U, Strauss MJ, Hofstetter R, Schlenzka D, et al. A new approach to computer-aided spine surgery : fluoroscopy-based surgical navigation. Eur Spine J. 2000;9(Suppl 1):S78–S88. doi: 10.1007/PL00010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roessler K, Ungersboeck K, Dietrich W, Aichholzer M, Hittmeir K, Matula C, et al. Frameless stereotactic guided neurosurgery : clinical experience with an infrared based pointer device navigation system. Acta Neurochir (Wien) 1997;139:551–559. doi: 10.1007/BF02750999. [DOI] [PubMed] [Google Scholar]
- 22.Schonfeld SJ, Lee C, Berrington de González A. Medical exposure to radiation and thyroid cancer. Clin Oncol (R Coll Radiol) 2011;23:244–250. doi: 10.1016/j.clon.2011.01.159. [DOI] [PubMed] [Google Scholar]
- 23.Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, Gutberlet M. Computer tomography assessment of pedicle screw placement in lumbar and sacral spine : comparison between free-hand and O-arm based navigation techniques. Eur Spine J. 2011;20:875–881. doi: 10.1007/s00586-010-1683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simpson AK, Whang PG, Jonisch A, Haims A, Grauer JN. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech. 2008;21:409–412. doi: 10.1097/BSD.0b013e3181568656. [DOI] [PubMed] [Google Scholar]
- 25.Singer CM, Baraff LJ, Benedict SH, Weiss EL, Singer BD. Exposure of emergency medicine personnel to ionizing radiation during cervical spine radiography. Ann Emerg Med. 1989;18:822–825. doi: 10.1016/s0196-0644(89)80204-5. [DOI] [PubMed] [Google Scholar]
- 26.Tian NF, Xu HZ. Image-guided pedicle screw insertion accuracy : a meta-analysis. Int Orthop. 2009;33:895–903. doi: 10.1007/s00264-009-0792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES, et al. Image-guided spine surgery : state of the art and future directions. Eur Spine J. 2010;19:25–45. doi: 10.1007/s00586-009-1091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van de Kraats EB, van Walsum T, Kendrick L, Noordhoek NJ, Niessen WJ. Accuracy evaluation of direct navigation with an isocentric 3D rotational X-ray system. Med Image Anal. 2006;10:113–124. doi: 10.1016/j.media.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S. Spinal pedicle fixation : reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 1988;13:1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Xu R, Ebraheim NA, Ou Y, Yeasting RA. Anatomic considerations of pedicle screw placement in the thoracic spine. Roy-Camille technique versus open-lamina technique. Spine (Phila Pa 1976) 1998;23:1065–1068. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 31.Yang YL, Zhou DS, He JL. Comparison of Isocentric C-Arm 3-Dimensional Navigation and Conventional Fluoroscopy for C1 Lateral Mass and C2 Pedicle Screw Placement for Atlantoaxial Instability. J Spinal Disord Tech. 2011 doi: 10.1097/BSD.0b013e31823d36b6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]