Abstract
Injury to the bilateral internal branch of superior laryngeal nerve (ibSLN) brings on an impairment of the laryngeal cough reflex that could potentially result in aspiration pneumonia and other respiratory illnesses. We describe a patient with traumatic cervical injury who underwent bilateral ibSLN palsy after anterior cervical discectomy with fusion (ACDF). An 75-year-old man visited with cervical spine fracture and he underwent ACDF through a right side approach. During the post-operative days, he complained of high pitched tone defect, and occasional coughing during meals. With a suspicion of SLN injury and for the work up for the cause of aspiration, we performed several studies. According to the study results, he was diagnosed as right SLN and left ibSLN palsy. We managed him for protecting from silent aspiration. Swallowing study was repeated and no evidence of aspiration was found. The patient was discharged with incomplete recovery of a high pitched tone and improved state of neurologic status. The SLN is an important structure; therefore, spine surgeons need to be concerned and be cautious about SLN injury during high cervical neck dissection, especially around the level of C3-C4 and a suspicious condition of a contralateral nerve injury.
Keywords: Superior laryngeal nerve, Cervical discectomy, Cough reflex
INTRODUCTION
The superior laryngeal nerve (SLN) originates from the vagus nerve and descends medially toward the thyroid membrane, then branches into internal branches (ib) and external branches (eb) deep into the internal carotid artery. The ibSLN traverses the inferior to the greater horn of the hyoid bone accompanied by the superior laryngeal artery5). The distal portion of the ibSLN is located between the C3-C4 levels and is responsible for a sensory branch of laryngeal mucosa that initiates a cough reflex4). An ebSLN supplies motor fibers to the cricothyroid muscle and accompanies the superior thyroid artery.
Injury to the unilateral SLN does not cause prompt, noticeable functional impairment of the vocal cords and dual innervation of laryngeal mucosa from the contralateral SLN prevents loss of laryngeal sensation4). Injury to the ebSLN incurs ipsilateral paralysis of the cricothyroidius, which results in loss of tension in the vocal cords, which is necessary for attainment of high pitched notes during singing.
Rarely, injury to the bilateral ibSLN brings on impairment of the laryngeal cough reflex8). Laryngeal cough reflex is a most important protective mechanism of the lung against aspiration of foreign material that could potentially result in aspiration pneumonia and other respiratory illnesses7). However, the importance of SLN has been overlooked and the morbidity caused by SLN injury has not been of concerned in surgical literature.
We report on a case of unexpected bilateral injury to the internal branch of the SLN in a patient with traumatic cervical injury who presented as loss of cough reflex after undergoing anterior cervical discectomy with fusion (ACDF).
CASE REPORT
A 75-year-old man visited with neck pain and paresthesia along the shoulder and lateral forearm after falling down during hiking. Magnetic resonance imaging (MRI) and computed tomography scans of the cervical spine showed fracture and subluxation at the C3-C4 level with a left vertebral artery injury (Fig. 1). His treatment was delayed due to his denial of surgical management. After 1 month of insult, his pain was worsened and he accepted the operation. He subsequently underwent ACDF through a right side approach using a cage with plating and posterior fusion using a lateral mass screw at C3-C4 (Fig. 2). Posterior fusion was performed on the right unilateral side due to the left lateral mass fracture.
Fig. 1.
Imaging of preoperative evaluation, including plain X-ray, computed tomography (CT) scan, magnetic resonance imaging (MRI), and CT angiogram. A : Simple lateral cervical plain X-ray shows subluxation of C3-C4. B : Preoperative sagittal CT scan shows a left lateral mass fracture of the C3 level. C : T2 weighted image of MRI reveals disrupted disc material on C3-C4 with signal change of the cervical cord. D : CT angiogram indicates compromised left vertebral artery flow.
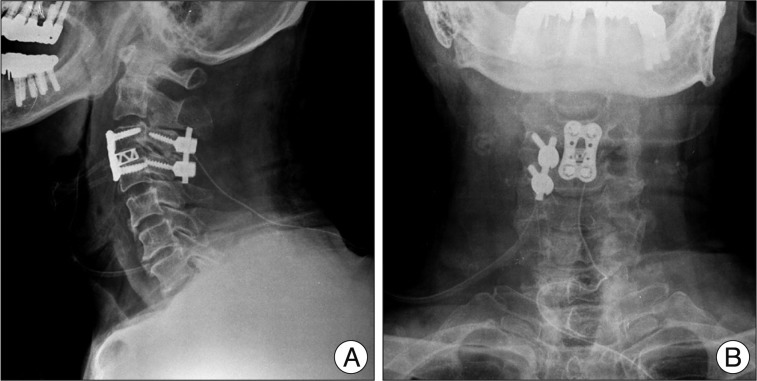
Fig. 2.
Post-operative plain X-ray imaging shows anterior and posterior (right unilateral) fusion using a cage with a plate and lateral mass screws in lateral (A) and AP (B) view images.
On the day after the operation, he expressed satisfaction with his improvement from pain and had no specific complaint, except for mild dysphagia. Immediate post-operative plain X-ray revealed mild soft tissue swelling in the neck. On day 2 post-operation, he complained of a defect in the high pitched tone of his voice and mentioned in passing an occasional cough during meals. We suspected a right SLN injury and felt the need to perform an evaluation for pulmonary aspiration. Then, we consulted him to be evaluated by a video fluoroscopic swallowing study (VFSS) and the result showed occurrence of silent aspiration on 3 cc of thin and thick liquid (Fig. 3). We undertook studies to find the cause of the silent aspiration after ACDF. Thus, brain MRI, laryngoscopy, and laryngeal electromyography (EMG) were performed for the work up of aspiration. Brain MRI showed negative results. Laryngeal EMG revealed that the left cricothyroid muscle and both thyroarytenoid muscles impulsed normal motor unit action potential (MUAP); however, no MUAP was observed in the right cricothyroid muscle (Fig. 4). In addition, the video laryngoscopic examination reported slight bowing of the right vocal cord and decreased laryngeal mucosa sensation when touching the mucosa using an air pulse sensory stimulator (absence of cough reflex on the right side and decreased on left side) (Fig. 5). According to these results, he was diagnosed as right SLN and left ibSLN palsy. Therefore, we performed L-tube insertion in order to protect him from silent aspiration.
Fig. 3.
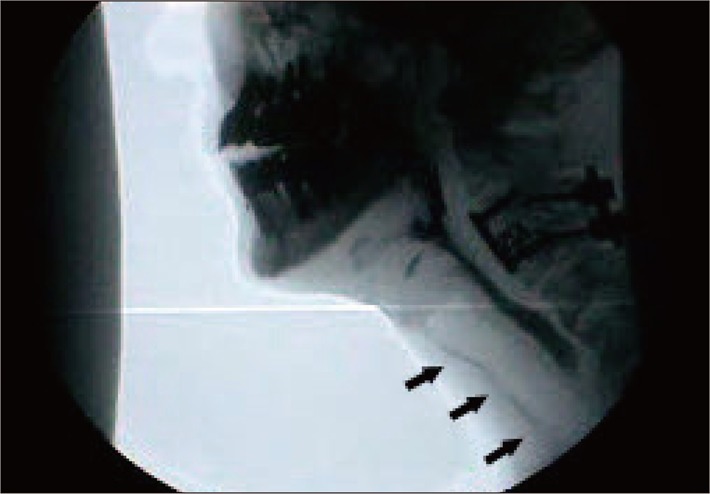
Initial video fluoroscopic swallowing study shows aspiration of thin and thick fluid. Arrows indicates aspiration materials under vocal cords.
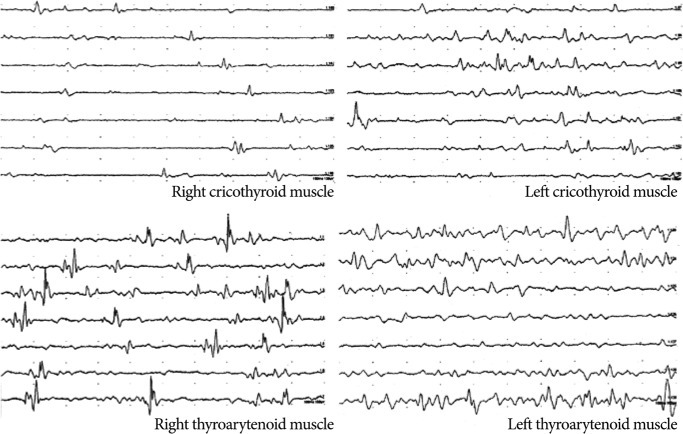
Fig. 4.
Laryngeal eletromyography reveals that there is no motor unit action potential (MUAP) in the right cricothyroid muscle. And, normal MUAPs were identified in the left cricothyroid muscle and both thyroarytenoid muscles.
Fig. 5.
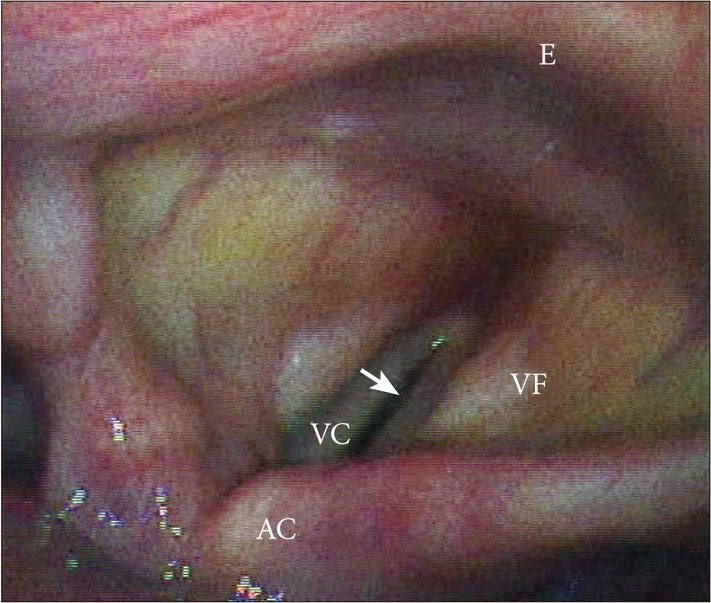
Video-laryngoscopy shows slight bowing of the right vocal cord (white arrow). E : epiglottis, VF : vestibular fold, VC : vocal cord, AC : arytenoid cartilage.
After 2 weeks of insertion, his VFSS was repeated and the result showed reduced aspiration. Therefore, we removed the L-tube and he carefully started soft meals. His chest X-ray was also followed weekly and no pneumonic evidence was seen. He underwent repeated VFSS at 2 weeks after removal of the L-tube and no evidence of aspiration was found. He was discharged with incomplete recovery of the high pitched tone and improved state of neurologic status.
DISCUSSION
Evaluation of the true incidence of SLN palsy is difficult due to diagnostic difficulties; therefore, few reports on the prevalence of SLN palsy have been published6). In a retrospective study of the anterior cervical approach, Bulger et al.1) reported an incidence rate of 1% for permanent SLN palsy. Dual innervation of laryngeal mucosa would explain the relatively low incidence of aspiration after high cervical dissections despite the high possibility of at least transient SLN palsy4). The optimal tool for diagnosis of SLN injury is use of laryngoscopy and laryngeal EMG. In particular, laryngeal EMG is also used for monitoring of the nerve's recovery2).
The distal portions of both SLN branches are prone to injury in the anterior upper cervical approach. These include, but are not limited to, accidental direct nerve injury, postoperative hematoma or edema, and inordinate traction during placement of self-retaining retractor blades3). For prevention of injury to the nerves, the most important point is that the retractor blades be secured under the medial edge of the longus colli muscle in order to avoid malpositioning laterally over the muscle. And, surgeons can reduce direct injury to these nerves by limiting all dissections to the medial edge of the blades.
In our case, we encountered an unexpected bilateral ibSLN injury. Perhaps the left ibSLN was injured at the time of the accident and the injury was not recognized. Through the operation, right side iatrogenic SLN injury has occurred; therefore, we supposed that noticeable clinical symptoms had developed. If we had missed or delayed diagnosis of his silent aspiration, it might have given rise to a desperate result.
CONCLUSION
The SLN is an important structure that could potentially result in aspiration pneumonia and other respiratory illnesses; therefore, spine surgeons need to be concerned and cautious of the SLN during high cervical neck dissection, especially around the level of C3-C4 and a suspicious condition of a contralateral nerve injury. Preoperative evaluations are suggested to include formal laryngeal EMG and laryngoscopic evaluation for SLN injury in suspicious patients who are planned for anterior cervical approach. If injury of the SLN was identified, more caution in dissection with retraction should be given to prevent nerve injury of contra-lateral side.
References
- 1.Bulger RF, Rejowski JE, Beatty RA. Vocal cord paralysis associated with anterior cervical fusion : considerations for prevention and treatment. J Neurosurg. 1985;62:657–661. doi: 10.3171/jns.1985.62.5.0657. [DOI] [PubMed] [Google Scholar]
- 2.Dursun G, Sataloff RT, Spiegel JR, Mandel S, Heuer RJ, Rosen DC. Superior laryngeal nerve paresis and paralysis. J Voice. 1996;10:206–211. doi: 10.1016/s0892-1997(96)80048-8. [DOI] [PubMed] [Google Scholar]
- 3.Lu J, Ebraheim NA, Nadim Y, Huntoon M. Anterior approach to the cervical spine : surgical anatomy. Orthopedics. 2000;23:841–845. doi: 10.3928/0147-7447-20000801-19. [DOI] [PubMed] [Google Scholar]
- 4.Melamed H, Harris MB, Awasthi D. Anatomic considerations of superior laryngeal nerve during anterior cervical spine procedures. Spine (Phila Pa 1976) 2002;27:E83–E86. doi: 10.1097/00007632-200202150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Monfared A, Kim D, Jaikumar S, Gorti G, Kam A. Microsurgical anatomy of the superior and recurrent laryngeal nerves. Neurosurgery. 2001;49:925–932. doi: 10.1097/00006123-200110000-00026. discussion 932-933. [DOI] [PubMed] [Google Scholar]
- 6.Schauber MD, Fontenelle LJ, Solomon JW, Hanson TL. Cranial/cervical nerve dysfunction after carotid endarterectomy. J Vasc Surg. 1997;25:481–487. doi: 10.1016/s0741-5214(97)70258-1. [DOI] [PubMed] [Google Scholar]
- 7.Stephens RE, Wendel KH, Addington WR. Anatomy of the internal branch of the superior laryngeal nerve. Clin Anat. 1999;12:79–83. doi: 10.1002/(SICI)1098-2353(1999)12:2<79::AID-CA1>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 8.Widdicombe JG, Tatar M. Upper airway reflex control. Ann N Y Acad Sci. 1988;533:252–256. doi: 10.1111/j.1749-6632.1988.tb37254.x. [DOI] [PubMed] [Google Scholar]