Abstract
A 31-year-old man was admitted to our hospital due to hydrocephalus with neurosarcoidosis. Ventriculo-peritoneal shunting was performed in the right lateral ventricle with intravenous methylprednisolone. Subsequently, after 4 months, additional ventriculo-peritoneal shunting in the left lateral ventricle was performed due to the enlarged left lateral ventricle and slit-like right lateral ventricle. After 6 months, he was re-admitted due to upward gaze palsy, and magnetic resonance image showed an isolated fourth ventricle with both the inlet and outlet of fourth ventricle obstructed by recurrent neurosarcoidosis. Owing to the difficulty of using an endoscope, we performed neuronavigator-guided ventriculo-peritoneal shunting via the left lateral transcerebellar approach for the treatment of the isolated fourth ventricle with intravenous methyl prednisolone. The patient was discharged with improved neurological status.
Keywords: Neurosarcoidosis, Hydrocephalus, Ventriculoperitoneal shunt
INTRODUCTION
Sarcoidosis is a very rare disease in Korea with an incidence of 59 cases in 1998 (0.125 cases/100000 people)11). Neurosarcoidosis makes up 5-15% of sarcoidosis cases10). Hydrocephalus is a rare clinical feature with a prevalence of 6% among patients with neurosarcoidosis, as reported by a prospective study2). Delaney6) reported that granulomatous meningitis is the main cause of hydrocephalus in neurosarcoidosis. Secondary hydrocephalus following meningitis, ventriculitis, or hemorrhage may be complicated by septum formation in the ventricular system2). Benzagmout et al.14) reported that after the treatment of ventricular shunt and corticosteroid therapy, acute hydrocephalus by neurosarcoidosis was resolved. We report the case of a 31-year-old man who developed multi-septated hydrocephalus from neurosarcoidosis and was treated with multiple shunt placements.
CASE REPORT
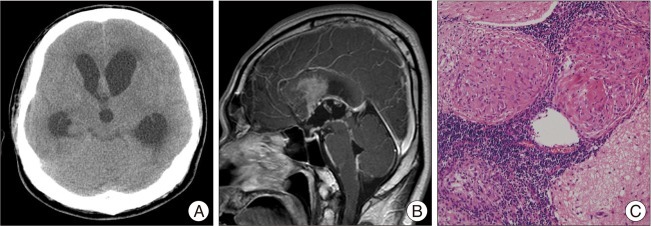
A 31-year-old man complained of a mild headache in the frontal area without nausea or vomiting for 7 days. On admission, he was confused and disoriented with time and space. The patient had no fever, and his complete blood count, serum biochemistry profiles and autoimmune antibody screening results were normal. Computed tomography (CT) revealed enlarged ventricles with periventricular interstitial edema (Fig. 1A). Cerebrospinal fluid (CSF) analysis revealed leukocytosis (53 leukocytes/mm3) with a mononuclear preponderance and markedly increased protein to 2.64 g/L. The microbiological examination of CSF was negative for bacteria, fungi, and mycobacterium. Chest radiograph and chest CT scan showed bilateral symmetric hilar and mediastinal lymphadenopathy suggesting sarcoidosis. Gadolinium-enhanced magnetic resonance image (MRI) of brain revealed hydrocephalus and enhanced lesions in septum pellucidum, infundibulum, aqueduct, corpus callosum, and leptomeninges (Fig. 1B). We performed neuroendoscopic biopsy of the enhanced lesions in the septum pellucidum through the standard right precoronal approach. Histopathological results showed non-caseating granuloma and biopsy specimens were all negative for bacteria, fungi and acid-fast bacilli, which were consistent with neurosarcoidosis (Fig. 1C). Ventriculo-peritoneal shunting (Strata valve; Medtronic, CA, USA) through the right parieto-occipital approach was performed, and intravenous methyl prednisolone was then started at 20 mg/kg/day for 3 consecutive days; this was followed by prednisolone (1 mg/kg/day) for 4 weeks. On post-operative day 5, the patient showed progressive improvement of confusion and disorientation, and at 3 weeks post-operation, he was discharged without any neurological deficit.
Fig. 1.
Non enhanced computed tomography showing enlarged ventricles with periventricular edema (A) and Gadolinium-enhanced magnetic resonance image showing enhanced lesions in septum pellucidum, infundibulum, aqueduct, corpus callosum, leptomeninges (B). Biopsy specimen shows noncaseating granulomas (H&E, ×200) (C).
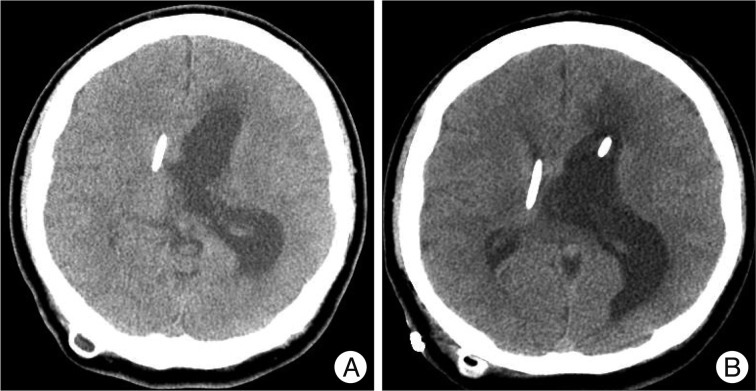
Four months after discharge, the patient was re-admitted due to headache, and gait disturbance. Brain CT revealed an enlarged left lateral ventricle with periventricular edema and a collapsed right ventricle, at which a ventricular catheter was inserted (Fig. 2A). Additional ventriculo-peritoneal shunting was performed through left Kocher's point (Fig. 2B). On post-operative day 5, gait disturbance including headache improved gradually, and in post-operative week 4, he was discharged without any neurological deficit.
Fig. 2.
Non enhanced computed tomography showing enlarged left lateral ventricle with decreased size of right ventricle inserted by catheter (A) and additional shunt catheter in left ventricle (B).
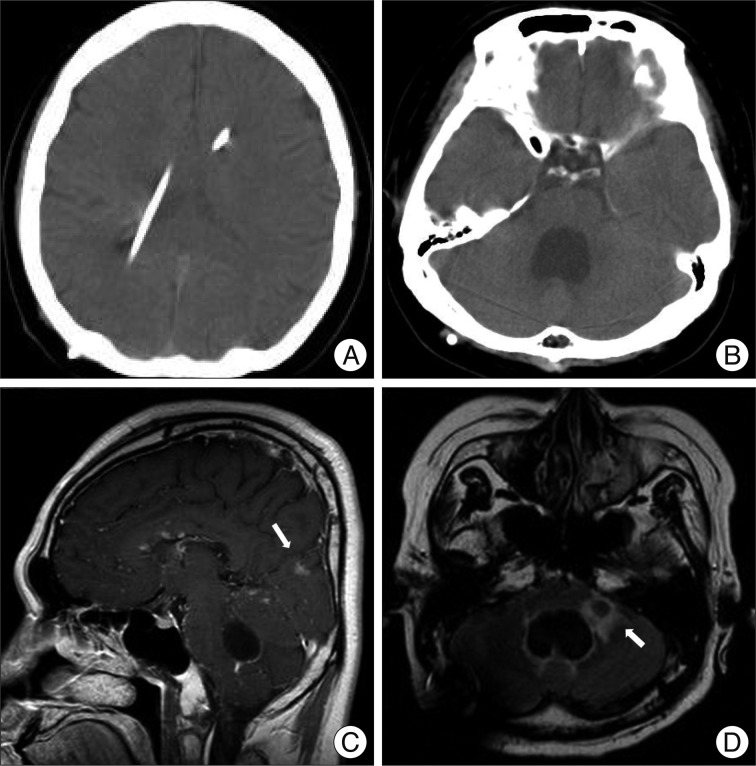
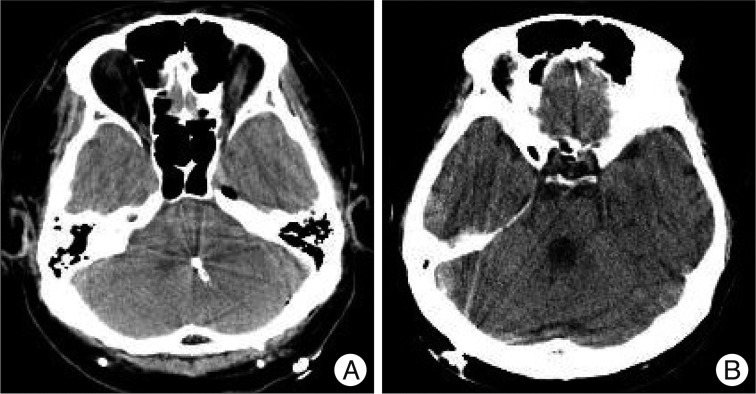
Six months after second shunt operation, he complained of upward gaze palsy, and gait disturbance. Brain CT showed an increased fourth ventricle with periventricular edema and both lateral ventricles were well-collapsed with ventricular catheter in situ (Fig. 3A, B). Gadolinium-enhanced MRI of the brain revealed an enlarged fourth ventricle with other enhanced lesions in the left occipital lobe, left cerebellar peduncle (Fig. 3C, D). Therefore, we planned ventriculo-peritoneal shunting for the isolated fourth ventricle by neuronavigation with intravenous methyl prednisolone. Neuronavigator-guided fourth ventriculo-peritoneal shunting was performed via the left lateral transcerebellar approach with neuronavigation (In2vision; Cybermed, Seoul, Korea). The fourth ventriculo-peritoneal shunt was not connected to the previous shunt. The CSF profile collected at the operative field revealed severe leukocytosis (121 leukocytes/mm3) and an increase in the level of protein to 2.03 g/L. After 2 weeks of steroid treatment, CSF collected at the valve dome was normalized (6 leukocytes/mm3 and 0.62 g/L protein). On post-operative day 10, upward gaze palsy and gait disturbance gradually disappeared, and the patient was discharged 4 weeks post-operatively with mild neurological deficit. Four months later, the patient's previous upward gaze palsy and gait disturbance was resolved and CT at follow-up showed a reduction in the size of the fourth ventricle compared to the previous pre-operative CT scan (Fig. 4).
Fig. 3.
Non enhanced computed tomography and showing both collapsed lateral ventricles following shunting (A), enlarged fourth ventricle with periventricular edema (B). Gadolinium-enhanced magnetic resonance image showing another enhanced lesions in the left occipital lobe (arrow) (C) and left cerebellar peduncle (arrow) (D).
Fig. 4.
Follow-up non-enhanced computed tomography scan showing catheter in the fourth ventricle (A) and decreased size of the fourth ventricle (B).
DISCUSSION
Sarcoidosis is a very rare granulomatous disease in Korea, and its cause remains unknown. Neurosarcoidosis most often presents with cranial nerve palsies, predominantly affecting the optic and facial nerves, reflecting its predilection for the base of the brain. The diagnosis of neurosarcoidosis is confirmed by biopsy showing noncaseating granulomas in the absence of organisms or other potential causes. In patients with hydrocephalus, the treatment depends upon the clinical status. In the case of asymptomatic hydrocephalus, treatment is not required4). However, ventricular drainage is usually lifesaving in symptomatic hydrocephalus1). Secondary hydrocephalus following meningitis may be complicated by septum formation in the ventricular system, resulting in complex manifestation of CSF circulation disturbance7). Even though the prognosis for neurosarcoidosis itself is good, hydrocephalus associated with neurosarcoidosis has poor long-term prognosis with a mortality rate of 75%1). Benzagmout et al.3) reported that after the treatment with ventricular shunt and corticosteroid therapy, acute hydrocephalus associated with neurosarcoidosis was resolved. In the present case, we first performed ventriculo-peritoneal shunt in the right lateral ventricle for hydrocephalus in neurosarcoidosis, and observed the slit-like right lateral ventricle 4 months after discharge. Hamada et al.8) reported that endoscopic treatment was effective for the treatment of obstructive ventricles in neurosarcoidosis. Further, they suggested that loculated hydrocephalus, which was often treated by placement of an additional shunt, can be better treated with neuroendoscopy since multiple shunt placement was complicated and often results in shunt malfunction8). It was necessary to perform endoscopic plasty of the occluded right foramen of Monro and fenestration of the septum pellucidum for the treatment of hydrocephalus during endoscopic biopsy.
Isolated fourth ventricle requires neurosurgical intervention, because impairment of brain stem functions may lead to sudden death12,13). Shin et al.14) reported that in the presence of a functioning shunt in the lateral ventricle, treatment options for the isolated fourth ventricle include the placement of an additional fourth ventricular catheter, via a variety of trajectories or endoscopic approaches to open the cerebral aqueduct. An endoscopic approach can only be performed if a membranous occlusion of the aqueduct is present on preoperative MRI. Further, the standard precoronal approach can be used only in cases with a dilated supratentorial ventricular system5). In the present case, because the supratentorial ventricular system was markedly collapsed and both the inlet and the outlet of the fourth ventricle were obstructed by enhanced lesions, the endoscopic procedure was not considered as an appropriate treatment option. Therefore, to minimize the complications related to fourth ventricular shunt insertion, we performed ventriculo-peritoneal shunting via the left lateral transcerebellar approach using a neuronavigator. The risks of this procedure included brain stem penetration by the ventricular catheter, with focal neurological deficit because of the compressed cerebellum and brain stem expansion by decompressing the isolated fourth ventricle following ventriculo-peritoneal shunting9). However, in the present case, there were no complications caused by the catheter during follow-up.
CONCLUSION
We report a case of hydrocephalus associated with neurosarcoidosis treated by multiple shunt placement with clinical features and a review of literature.
References
- 1.Akhondi H, Barochia S, Holmström B, Williams MJ. Hydrocephalus as a presenting manifestation of neurosarcoidosis. South Med J. 2003;96:403–406. doi: 10.1097/01.SMJ.0000056648.43258.C0. [DOI] [PubMed] [Google Scholar]
- 2.Allen RK, Sellars RE, Sandstrom PA. A prospective study of 32 patients with neurosarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2003;20:118–125. [PubMed] [Google Scholar]
- 3.Benzagmout M, Boujraf S, Góngora-Rivera F, Bresson D, Van-Effenterre R. Neurosarcoidosis which manifested as acute hydrocephalus : diagnosis and treatment. Intern Med. 2007;46:1601–1604. doi: 10.2169/internalmedicine.46.0126. [DOI] [PubMed] [Google Scholar]
- 4.Burns TM. Neurosarcoidosis. Arch Neurol. 2003;60:1166–1168. doi: 10.1001/archneur.60.8.1166. [DOI] [PubMed] [Google Scholar]
- 5.Cinalli G, Spennato P, Savarese L, Ruggiero C, Aliberti F, Cuomo L, et al. Endoscopic aqueductoplasty and placement of a stent in the cerebral aqueduct in the management of isolated fourth ventricle in children. J Neurosurg. 2006;104:21–27. doi: 10.3171/ped.2006.104.1.21. [DOI] [PubMed] [Google Scholar]
- 6.Delaney P. Neurologic manifestations in sarcoidosis : review of the literature, with a report of 23 cases. Ann Intern Med. 1977;87:336–345. doi: 10.7326/0003-4819-87-3-336. [DOI] [PubMed] [Google Scholar]
- 7.Eller TW, Pasternak JF. Isolated ventricles following intraventricular hemorrhage. J Neurosurg. 1985;62:357–362. doi: 10.3171/jns.1985.62.3.0357. [DOI] [PubMed] [Google Scholar]
- 8.Hamada H, Hayashi N, Kurimoto M, Umemura K, Hirashima Y, Endo S. Isolated third and fourth ventricles associated with neurosarcoidosis successfully treated by neuroendoscopy--case report. Neurol Med Chir (Tokyo) 2004;44:435–437. doi: 10.2176/nmc.44.435. [DOI] [PubMed] [Google Scholar]
- 9.Harter DH. Management strategies for treatment of the trapped fourth ventricle. Childs Nerv Syst. 2004;20:710–716. doi: 10.1007/s00381-004-1004-5. [DOI] [PubMed] [Google Scholar]
- 10.Jarnier D, Seriès C. [Neurosarcoidosis. Review of the literature] Neurochirurgie. 1999;45:214–218. [PubMed] [Google Scholar]
- 11.Kim DS. Sarcoidosis in Korea : report of the Second Nationwide Survey. Sarcoidosis Vasc Diffuse Lung Dis. 2001;18:176–180. [PubMed] [Google Scholar]
- 12.Kiwak KJ. Trapped fourth ventricle. Surg Neurol. 1988;29:247. doi: 10.1016/0090-3019(88)90017-1. [DOI] [PubMed] [Google Scholar]
- 13.Rosenfeld DL, Lis E, DeMarco K. Transtentorial herniation of the fourth ventricle. Pediatr Radiol. 1995;25:436–439. doi: 10.1007/BF02019057. [DOI] [PubMed] [Google Scholar]
- 14.Shin M, Morita A, Asano S, Ueki K, Kirino T. Neuroendoscopic aqueductal stent placement procedure for isolated fourth ventricle after ventricular shunt placement. Case report. J Neurosurg. 2000;92:1036–1039. doi: 10.3171/jns.2000.92.6.1036. [DOI] [PubMed] [Google Scholar]