Abstract
Aims
This study examines the preliminary outcomes of an intervention targeting service providers in methadone maintenance therapy clinics in China. The intervention effects on both service providers and clients are reported.
Design
The MMT CARE intervention pilot was developed and implemented collaboratively with local health educators. After three group intervention sessions, trained providers in intervention clinics delivered two individual motivational interviewing sessions with their clients.
Settings
Six clinics in Sichuan, China, were randomized to either the MMT CARE intervention condition or a standard care condition.
Participants
A total of 41 providers and 179 clients were sampled from the six clinics.
Measurements
At baseline and 3-, 6-, and 9-month assessments, providers completed self-administrated paper/pencil questionnaires regarding provider-client interaction, methadone maintenance therapy knowledge, perceived job-related stigma, and clinic support. Clients completed a face-to-face survey about their concurrent drug use and drug avoidance self-efficacy. Mixed-effects regression models with clinic-level random effect were used to assess the intervention effects.
Findings
Significant intervention effects for providers were found in improved methadone maintenance therapy knowledge, provider-client interaction, and perceived clinic support. For clients, better improvements in drug avoidance self-efficacy and reduced concurrent drug use were observed for the intervention compared to the standard care group.
Conclusions
The methadone maintenance therapy CARE intervention targeting providers in methadone maintenance clinics can improve providers’ treatment knowledge and their interaction with clients. The intervention can also reduce clients’ drug using behavior through motivational interviewing sessions conducted by trained providers.
Keywords: Methadone maintenance therapy, providers, intervention pilot, China
INTRODUCTION
The first methadone maintenance therapy (MMT) clinic in China was established in 2004 [1]. By the end of September 2011, 716 clinics serving nearly 333,000 clients were operating in the country [2]. This rapid scale-up of MMT programs has decreased drug use, criminality, and increased quality of life and employment among drug users [3,4]. Despite the progress, MMT programs are encountering challenges including high dropout rates (about 50%) and concurrent heroin use (about one-third) [5–9]. Effective interventions are urgently needed to sustain the effectiveness of MMT.
Internationally there has been a great deal of effort to reduce concurrent drug use and increase MMT treatment adherence, with most efforts targeted clients directly [10–12]. However, providers play an important role in the success of MMT. Positive interactions between providers and clients improved treatment outcomes by increasing mutual understanding, empathy, trust, and shared decision making [13–16]. The rapid scale-up of MMT programs in China, however, has been associated with limited training and support for providers [17]. Normally, no more than two providers per clinic can receive formal national MMT training. Many providers do not have a clear understanding of the client needs, treatment dosages and risk management [18,19]. Most MMT clinics lack of the capacity to deliver psychosocial interventions and other services [17,20–22]. Moreover, difficulties in pursuing a professional career can affect a provider’s morale [17] and internalized shame associated with working with a drug-using population can negatively impact interaction with clients [6].
This study was the first study to assess outcomes of an intervention targeting providers working at MMT clinics in China. Instead of directly delivering program activities to clients, we trained providers to conduct individual sessions with their clients. With the assumption that provider support and communications with clients can serve as an important contextual factor impacting client behaviors, we hypothesized that improved provider outcomes would be correlated with positive outcomes for clients.
The two specific aims of the intervention were to examine:
Whether providers in the intervention, compared to providers in the standard care, demonstrated improved provider-client interactions, MMT knowledge, better perceived support from clinic, and reduced perceived stigma associated with working in a drug-related field.
Whether MMT clients in the intervention, compared to clients in the standard care, reported increased self-efficacy to avoid drug and reduced concurrent illicit drug use.
METHODS
Study Design and Participants
This study was conducted from March 2009 to February 2011 in Sichuan, China. In 2009, Sichuan was ranked number four among provinces with the most drug users in China [23]. HIV prevalence was more than 15% among drug users [24].
The study utilized a two-armed design. Six MMT clinics were randomly selected out of 32 MMT clinics in Sichuan, and matched into three pairs based on number of clients and average retention rates. After baseline, the two clinics in each pair were randomized to MMT CARE intervention or standard care condition. The distance between the intervention and standard care clinics was far enough to avoid contamination.
The study participants included providers and clients from the selected MMT clinics. To be eligible for the study, providers had to be 18 years or older and working at the participating clinics, and clients had to be at least 18 years old and receiving MMT at the clinics. The study was approved by the Institutional Review Boards of the University of California, Los Angeles, and the Chinese Center for Disease Control and Prevention.
All providers who provided direct services to clients, including doctors, nurses, and pharmacists, were invited to participate in the study. The research staff waited for potential client participants near the entry hall of each clinic, and approached them randomly in a predetermined interval. During the recruitment of both providers and clients, research staff followed standardized scripts to introduce the study purpose, procedures, the voluntary nature, potential risks, and benefits in detail. Written informed consents were obtained. A total of 41 providers and 179 clients were recruited from the six clinics. The refusal rate was zero for providers and less than 10% for clients.
Intervention
The MMT CARE intervention consisted of two linked components: 1) group sessions with service providers, and 2) individual sessions delivered by trained providers to clients. The intervention was implemented by health educators from provincial and district-level CDCs to ensure regional relevancy and sustainability.
Service providers recruited from the intervention clinics received three group sessions in three consecutive weeks. Each session was about 90 minutes and was conducted with a group of 5 to 7 providers at each clinic. The themes of the three sessions were: MMT protocol and procedures, understanding stigma and its impact, effective communication with clients and motivational interviewing concepts and skills. The contents reflected the challenges faced by MMT providers that were identified from our earlier formative studies [6,7]. The sessions incorporated interactive activities such as games, pair-share, and role-play to encourage participants’ full involvement.
The second component of the intervention required trained providers to deliver two brief motivational interviewing sessions in a one-on-one format to three to six clients in promoting positive behavior changes and treatment adherence. Each session lasted about one hour and was conducted in a private room. The providers were encouraged to apply the skills, tools, and strategies learned from the provider training to assist clients in treatment adherence by enhancing their motivation and commitment to positive behavior changes. In order to ensure the fidelity of individual sessions, clients were given a journal to document their experience, including date, time, what they liked or disliked about the contents and formats of each session. We also conducted brief interviews to seek clients’ opinions about the sessions and areas to be improved.
After the individual sessions with clients, there were two booster sessions for providers, each lasting about 75 minutes. The booster sessions focused on sharing experiences in working with clients and continued skill building and problem solving through a new set of interactive games and activities. The participation rate for these activities was higher than 95%.
Standard Care
The providers in the standard care clinics continued to receive regular training on MMT related policies, procedures, and side-effect management. Such training was provided by the National MMT Training Center in a didactic lecturing format. No intervention activity or additional services were delivered to the clients in the standard care clinics.
Data Collection
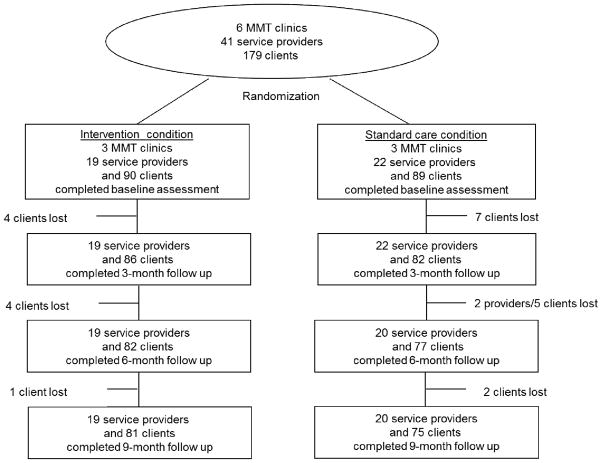
The intervention outcomes were evaluated with data collected at baseline (before randomization and intervention delivery) and 3-, 6-, and 9-month assessments after baseline. At each assessment, provider participants completed self-administrated paper/pencil questionnaires independently in a private room, which took approximately 25 minutes to complete. A trained interviewer was available to answer questions during the assessment. Client data collection was conducted in a one-on-one, face-to-face format by trained interviewers in a private room. After the assessment, the client participants were asked to provide a urine specimen for urine morphine test. Assessments lasted an average of 30 to 45 minutes. All participants were compensated 50 yuan (U.S. $7.70) for each assessment. Figure 1 shows the follow-up rates for providers and clients at each follow-up point.
Figure 1.
Flow of Study Participants
Provider Outcome Measures
Provider-client interaction was measured with 12 questions specifically designed for this study. Sample questions included, “Do you ask clients questions about their concerns?” and “Do you find out the reason if your client is missing a dose?” Each question was measured on a 5-point scale with 1=not at all and 5=very much likely (range=12–60). A higher score indicates better client-provider interaction (α=0.82).
MMT knowledge was measured with 18 true-or-false questions adapted from the Methadone Knowledge Questionnaire [25] and the MMT Clinical Guidance Handbook [26]. The answers to these questions were confirmed by MMT experts in China. The measure encompassed various topics on MMT eligibility, treatment goal, dosage, potential side effects and management. Sample items included: “Purpose of current MMT program is to achieve abstinence” and “MMT increases the severity of preexisting depression.” Participants scored one for each correct answer (range=0–18).
Perceived stigma was used to measure providers’ perceived stigma associated with working in a drug-related locale. The scale was originally developed and tested in other studies among providers in China [27]. The scale included nine items such as “You suffer discrimination or stigma from other providers due to the field in which you work,” and “You feel shame to work with drug users compared with professionals in other medical fields.” Each item scored from 1=strongly disagree to 5=strongly agree (range=9–45). A higher score indicates a higher level of perceived stigma (α=0.93).
Perceived clinic support was measured by responses to eight statements that had been validated in previous studies in China [28]. Sample statements included “My institute has enough equipments and medicine for occupational exposure protection,” and “If I work hard, I will have opportunities to be promoted.” The original responses for each statement were 1=yes, 2=not sure, or 3=no and were further dichotomized as 1=yes and 0=no/not sure. The positive answers (1=yes) were summed so that higher numbers indicating higher levels of perceived institutional support from the clinic (range=0–6; α=0.68).
Client Outcome Measures
Drug avoidance self-efficacy was measured with selected questions of the Drug-Avoidance Self-efficacy Scale (DASES) [29]. We chose 8 out of 16 questions that were considered to be relevant to the target population. Some questions were modified to fit Chinese culture. For example, “Imagine it is Chinese New Year and you plan to do something special to celebrate. Would you use drugs?” All the questions were answered with a 5-point Likert scale from 1=definitely to 5=definitely not. Some questions were reversed so that a higher score indicated higher self-efficacy to avoid drug use (range=8–40; α =0.77).
Concurrent drug use was determined using self-report of drug use in combination with urine morphine test, as suggested by Ciesla and Spear in 2001 [30]. Frequency and severity of heroin use in the past 30 days were self-reported by using the drug use section of the Addiction Severity Index (ASI) [31]. Urine specimen collection was collected and tested for morphine. Concurrent drug use was defined if a client either self-reported the use of heroin at least one day in the prior 30 days or had a positive morphine urine result.
Statistical Analysis
We used an intention-to-treat approach to estimate intervention effects. Baseline differences between intervention and standard care samples were tested using chi-square and t tests (or Wilcoxon rank tests) for categorical and continuous variables, respectively. The data for providers and clients were analyzed separately. Mixed-effects regression models with clinic-level random effect were used to assess the intervention effects on the positive change of providers’ outcomes or the positive change of clients’ outcomes. Covariates included preselected provider’s or client’s characteristics, group (standard care vs. intervention), visit (baseline, 3-, 6-, or 9-month follow-up), and group-by-visit interaction. The pre-selected provider’s characteristics included age, gender, profession (doctor vs. other), and working at MMT clinic (month), and the pre-selected client’s characteristics included age, gender, marital status (married/living as married vs. other), education (no schooling, primary school, and at least junior high), income in past month (yuan), methadone dose at enrollment (ml). The visit variable in these models was treated as a categorical variable in order to relax the linearity assumption. The model included a clinic-level random effect to account for dependence within clinics and a first-order autoregressive (AR1) covariance structure to account for repeated observations for each study participant. The primary interest in this study was to examine whether the changes (improvement or reduction) in outcome measure are different between intervention and standard care at the follow-up, which we refer to as an “intervention effect” at the follow-up. Thus, we present the comparison of interest through model contrasts, i.e., the estimated baseline differences and intervention effects at each follow-up after adjusting for provider’s or client’s characteristics. We also present the results from F-tests for the main effects (group and visit effects) and the interaction term. Lastly, we explored whether, in the intervention group, the characteristics of providers or clients influenced a client’s level of drug avoidance using a mixed-effects regression model. This model included the same random-effect and covariance structure as that used for clients. Additional covariates of interest were provider characteristics (years working in the medical field and service provider’s profession) and provider time-varying covariates (provider-client interaction, MMT knowledge, perceived stigma, and clinical support). All statistical analyses were conducted using SAS for Windows (Version 9.2).
RESULTS
Baseline demographic characteristics
Of the 41 providers, 19 were recruited from the intervention clinics and 22 were recruited from the standard care clinics. About 61% of the providers were women, and around 50% were doctors. Nearly 32% of the providers in the standard care and 47% of the providers in the intervention were 46 years or older. In the standard care, about 59% reported having been working in the medical field at least 15 years, compared to 63% in the intervention. At baseline, no significant differences were observed for gender, age, profession, or years working in the medical field. Significant differences in duration working at MMT clinics were found between the intervention and standard care groups (mean: 22.5 vs. 33.4 months, respectively, P =0.021). The average score of the provider-client interaction measure at baseline in the standard care was significantly lower than that for the intervention (mean: 34.1 vs. 37.8, respectively; P=0.028). Comparable levels of provider reports on MMT knowledge, perceived stigma, and perceived clinic support at baseline were observed across the two intervention conditions (Table 1).
Table 1.
Demographic and Background Characteristics by Group Service Providers
| Characteristics | Standard Care | Intervention | P |
|---|---|---|---|
|
| |||
| N (%) | N (%) | ||
| Number of Participants | 22 | 19 | |
| Gender | 0.7071 | ||
| Male | 8 (36.4) | 8 (42.1) | |
| Age (Year) (Mean ± SD) | 39.2 ± 10.8 | 45.3 ± 12.2 | 0.0972 |
| 35 or younger | 9 (40.9) | 3 (15.8) | |
| 36–45 | 6 (27.3) | 7 (36.8) | |
| 46 or older | 7 (31.8) | 9 (47.4) | |
| Profession | 0.6131 | ||
| Doctor | 11 (50.0) | 8 (42.1) | |
| Nurse/Pharmacist/Other | 11 (50.0) | 11 (58.9) | |
| Years Working at Medical Field | 15.5 ± 10.1 | 20.8 ± 13.8 | 0.1682 |
| 5 or less | 6 (27.3) | 4 (21.1) | |
| 6–15 | 3 (13.6) | 3 (15.8) | |
| 16–25 | 9 (40.9) | 5 (26.3) | |
| 26 or more | 4 (18.2) | 7 (36.8) | |
| Working at MMT Clinic (Months) (Mean ± SD) | 22.5 ± 15.8 | 33.4 ± 12.5 | 0.0212 |
| 12 or Less | 5 (22.7) | 2 (10.5) | |
| 13–24 | 11 (50.0) | 1 (5.26) | |
| 25–36 | 1 (4.55) | 10 (52.6) | |
| 37 or More | 5 (22.7) | 6 (31.6) | |
| Baseline | |||
| Provider-Client Interaction | |||
| Mean ± SD | 34.1 ± 4.26 | 37.8 ± 6.18 | 0.0282 |
| Perceived Stigma | |||
| Mean ± SD | 21.4 ± 6.04 | 18.4 ± 8.05 | 0.1902 |
| MMT Knowledge | |||
| Mean ± SD | 14.7 ± 1.42 | 15.1 ±0.97 | 0.4052 |
| Perceived Clinic Support | |||
| Mean ± SD | 2.41 ± 1.68 | 1.74 ±1.41 | 0.1772 |
Chi-square test;
t-test or Wilcoxon test
As shown in Table 2, there were 89 clients in the standard care group and 90 in the intervention. About 65% of the clients were men; at least 50% of the sample reported being married or living as married; and more than 62% of the client sample reported junior high school or above in education. At baseline, no significant differences between the intervention and standard care were observed for age, gender, marital status, education, or annual income. Standard care clients reported higher average methadone dose (59.6) than intervention (50.9) clients (P =0.042). One-third of the client participants self-reported heroin use in the previous 30 days, and 33.1% had a positive urine morphine test. The agreement of these two measurements was moderate (Kappa=0.47). Altogether 39.3% of clients in the standard care and 50.0% in the intervention either reported concurrent heroin drug use or had a positive urine test, and were thus considered concurrent heroin users in this study. The drug avoidance self-efficacy, heroin use during past month, and positive urine results of clients at baseline across the two intervention conditions were comparable.
Table 2.
Demographic and Background Characteristics by Group Clients
| Characteristics | Standard Care | Intervention | P |
|---|---|---|---|
|
| |||
| N (%) | N (%) | ||
| Number of Participants | 89 | 90 | |
| Gender | 0.7951 | ||
| Male | 59 (66.3) | 58 (64.4) | |
| Age (Year) (Mean ± SD) | 36.4 ± 5.6 | 38.4 ± 5.4 | 0.0212 |
| 35 or younger | 36 (40.5) | 23 (25.6) | |
| 36–40 | 32 (36.0) | 43 (47.8) | |
| 41 or older | 21 (23.6) | 24 (26.7) | |
| Marital status | 0.1121 | ||
| Married/living as married | 55 (61.8) | 45 (50.0) | |
| Other | 34 (38.2) | 45 (50.0) | |
| Education | 0.4951 | ||
| No schooling | 16 (18.0) | 16 (17.8) | |
| Primary school | 12 (13.5) | 18 (20.0) | |
| Junior high or higher | 61 (68.5) | 56 (62.2) | |
| Income in Past Month (Yuan) (Mean ± SD) | 792 ± 1382 | 1128 ± 2421 | 0.2572 |
| 100 or Less | 33 (37.1) | 37 (41.1) | |
| 101 – 600 | 24(27.0) | 16 (17.8) | |
| 601 or more | 32 (36.0) | 37 (41.1) | |
| Methadone Dose at enrollment (Mean ± SD) | 59.6 ± 26.3 | 50.9 ± 29.7 | 0.0422 |
| Baseline | |||
| Drug Avoidance Self-Efficacy | |||
| Mean ± SD | 26.4 ± 6.87 | 24.9 ± 5.41 | 0.1052 |
| Heroin Use Past Month or Positive Urine | |||
| Results (%) | 35 (39.3) | 45 (50.0) | 0.1511 |
Chi-square test;
t-test or Wilcoxon test
Intervention effects on service providers
Table 3 presents the estimated intervention effects, differences in improvement or reduction of outcome measures between intervention and standard care, from the mixed-effect regression models for providers. We found that doctors reported significantly higher level of perceived stigma (P =0.011) and lower level of clinic support (P =0.014) as compared to the other profession. At 6-month, significant intervention effects on provider-client interaction (estimated difference=4.84, 95% CI: 0.71–8.97; P=0.023) and MMT knowledge (estimated difference=1.97, 95% CI: 0.71–3.22; P=0.003), after adjusting for provider’s characteristics, were observed. At 9-month, the intervention effect on provider-client interaction remained (estimated difference=4.82, 95% CI: 0.44–9.19; P =0.033), and the providers in the intervention group reported a significant increase in perceived clinic support (estimated difference=1.82, 95% CI: 0.55–3.09; P=0.006). The average estimated intra-class correlation was about 0.05 (range: 0.027–0.095), and the AR1 correlation parameters were all significantly positive (range: 0.23–0.60). Since a significant difference in provider-client interaction at baseline was observed, we performed a sensitivity analysis by including the provider-client interaction measurement at baseline in the model. The results were very similar to those discussed above.
Table 3.
Results (Estimate and 95% CI) from Mixed-Effects Regression Models - Service Providers
| Parameter | Provider-Client Interaction | MMT Knowledge | Perceived Stigma | Clinic Support | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Est. | 95% CI | P | Est. | 95% CI | P | Est. | 95% CI | P | Est. | 95% CI | P | |
| Provider’s Characteristics | ||||||||||||
| Male (vs. Female) | −1.977 | (−4.621, 0.667) | 0.145 | −0.115 | (−0.825, 0.595) | 0.751 | 2.911 | (−0.441, 6.263) | 0.091 | 0.319 | (−0.353, 0.991) | 0.354 |
| Age | −0.051 | (−0.173, 0.071) | 0.410 | −0.031 | (−0.064, 0.002) | 0.062 | −0.034 | (−0.189, 0.121) | 0.668 | −0.011 | (−0.042, 0.020) | 0.508 |
| Doctor (vs. Others) | −0.462 | (−2.888, 1.964) | 0.710 | 0.403 | (−0.250, 1.056) | 0.228 | 4.051 | (0.988, 7.114) | 0.011 | −0.785 | (−1.404, −0.166) | 0.014 |
| Months at MMT | −0.032 | (−0.116, 0.052) | 0.452 | 0.023 | (0.001, 0.045) | 0.050 | −0.037 | (−0.143, 0.069) | 0.492 | −0.013 | (−0.035, 0.009) | 0.246 |
| Main effect1 | ||||||||||||
| Group | <0.001 | 0.014 | 0.053 | 0.502 | ||||||||
| Visit | 0.148 | 0.846 | 0.009 | 0.315 | ||||||||
| Interaction1 | ||||||||||||
| Group × Visit | 0.111 | 0.001 | 0.414 | 0.038 | ||||||||
|
| ||||||||||||
| Comparison of Interest | ||||||||||||
| Baseline comparison2 | 4.502 | (0.735, 8.269) | 0.021 | 0.334 | (−0.742, 1.410) | 0.544 | −2.479 | (−6.813, 1.855) | 0.264 | −0.524 | (−1.718, 0.670) | 0.391 |
| Intervention Effect3 | ||||||||||||
| 3-Month | 2.002 | (−1.432, 5.436) | 0.255 | 1.002 | (−0.086, 2.090) | 0.073 | −0.175 | (−3.360, 3.010) | 0.915 | 0.387 | (−0.720, 1.494) | 0.494 |
| 6-Month | 4.837 | (0.705, 8.969) | 0.023 | 1.966 | (0.714, 3.218) | 0.003 | −2.876 | (−6.959, 1.207) | 0.170 | 1.218 | (−0.029, 2.465) | 0.057 |
| 9-Month | 4.815 | (0.438, 9.192) | 0.033 | −0.144 | (−1.440, 1.152) | 0.828 | −1.866 | (−6.394, 2.662) | 0.421 | 1.819 | (0.545, 3.093) | 0.006 |
P-value from F-test. The significances of the main effects were not of interest.
Estimated difference in provider’s outcome measure at baseline between Intervention and Standard Care through model contrasts.
Intervention effect = Estimated difference in changes from baseline between Intervention and Standard Care through model contrasts.
Intervention effects on clients
Results from mixed-effect regression models for clients are shown in Table 4. Age and marital status were found to be positively associated with level of drug avoidance self-efficacy (P=0.036 and 0.013, respectively). At 3-month, a significant intervention effect on the level of drug avoidance self-efficacy (estimated difference=2.93, 95% CI: 0.94–4.92; P=0.004) was observed (i.e., the clients in the intervention had a significantly better improvement in drug avoidance self-efficacy). We also found that the clients in the intervention had significantly lower odds of concurrent heroin use (i.e., heroin use in the past month or positive urine results) as compared to those in the standard care (OR=0.26, 95% CI: 0.08–0.79; P=0.018).
Table 4.
Results (Estimate and 95% CI) from Mixed-Effects Regression Model - Clients
| Drug Avoidance Self-Efficacy | Heroin Use Past Month or Positive Urine Results | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Parameter | Estimate | 95% CI | P | OR | 95% CI | P |
| Client’s Characteristics | ||||||
| Male (vs. Female) | −1.167 | (−2.386, 0.052) | 0.061 | 1.215 | (0.588, 2.510) | 0.598 |
| Age | 0.114 | (0.008, 0.220) | 0.036 | 0.948 | (0.891, 1.010) | 0.099 |
| Married/Living as Married (vs. Other) | 1.481 | (0.321, 2.641) | 0.013 | 0.845 | (0.423, 1.689) | 0.633 |
| Education (Ref=At least Junior High) | ||||||
| No Schooling | 1.405 | (−0.143, 2.953) | 0.076 | 0.827 | (0.329, 2.078) | 0.685 |
| Primary School | 0.011 | (−1.510, 1.532) | 0.989 | 2.038 | (0.811, 5.120) | 0.131 |
| Income in Past Month (in 10 yuan) | 3.996 | (−2.566, 10.56) | 0.233 | 2.519 | (0.052, 122.3) | 0.641 |
| Methadone Dose at Enrollment | −0.010 | (−0.032, 0.012) | 0.358 | 1.007 | (0.993, 1.021) | 0.353 |
| Main Effect1 | ||||||
| Group | 0.796 | 0.816 | ||||
| Visit | 0.012 | 0.424 | ||||
| Interaction1 | ||||||
| Group Visit | 0.037 | 0.065 | ||||
|
| ||||||
| Comparison of Interest | ||||||
| BaselineComparison2 | 1.689 | (−0.630, 4.008) | 0.155 | 2.354 | (0.384, 14.426) | 0.355 |
| Intervention Effect3 | ||||||
| 3-Month | 2.929 | (0.942, 4.916) | 0.004 | 0.255 | (0.083, 0.786) | 0.018 |
| 6-Month | 1.535 | (−0.784, 3.854) | 0.195 | 0.789 | (0.252, 2.469) | 0.684 |
| 9-Month | 1.252 | (−1.173, 3.677) | 0.312 | 0.362 | (0.115, 1.144) | 0.084 |
P-value from F-test. The significances of the main effects were not of interest.
Estimated difference in provider’s outcome measure at baseline between Intervention and Standard Care through model contrasts.
Intervention effect = Estimated difference in changes from baseline between Intervention and Standard Care through model contrasts.
Linking drug avoidance self-efficacy to providers’ and clients’ characteristics
In an effort to explore associations between intervention effects on providers and clients, we conducted further analyses within the intervention group. Table 5 presents the selected characteristics of clients or their providers that were associated with client drug avoidance self-efficacy in the intervention. Male clients reported a significantly lower level of drug avoidance self-efficacy as compared to female clients (P=0.024). Providers’ years of working in the medical field was also positively associated with drug avoidance self-efficacy (P=0.036). A lower level of perceived stigma from providers was significantly associated with a higher client drug avoidance self-efficacy (P=0.017). Unexpectedly, increasing providers’ MMT knowledge was significantly associated with a lower level of drug avoidance (P=0.010).
Table 5.
Results from Model on Linked Provider and Client Data within Intervention Group
|
Outcome: Drug Avoidance Self-Efficacy
|
|||
|---|---|---|---|
| Estimate | 95% CI | P | |
| Client’s Characteristics | |||
| Male | −1.81 | (−3.358, −0.262) | 0.024 |
| Age | 0.13 | (−0.007, 0.267) | 0.057 |
| Visit (Ref=Baseline) | |||
| 3-month | 2.52 | (1.070, 3.970) | 0.001 |
| 6-Month | 2.19 | (0.544, 3.836) | 0.010 |
| 9-Month | 2.73 | (1.025, 4.435) | 0.002 |
| Providers’ Characteristics | |||
| Years working at medical field | 0.14 | (0.003, 0.227) | 0.036 |
| Profession (Ref=Doctor) | |||
| Nurse | 3.06 | (0.159, 5.961) | 0.041 |
| Other | 2.07 | (−1.732, 5.872) | 0.288 |
| Provider’s Time-Varying Covariate | |||
| Provider-Client Interaction | −0.09 | (−0.227, 0.047) | 0.222 |
| MMT Knowledge | −0.71 | (−1.239, −0.181) | 0.010 |
| Perceived Stigma | −0.14 | (−0.258, −0.022) | 0.017 |
| Clinic Support | 0.14 | (−0.291, 0.571) | 0.537 |
DISCUSSION
Compared to Western nations, MMT programs in China are still at an early stage of development. Although previous work using strategies such as contingency management has shown promising results in enhancing retention among clients, efficacy is not likely to be sustainable if providers are not adequately trained [10–12,21]. There is an urgent need to broaden the focus from solely on individual clients to their treatment provision [32,33]. The current study takes an important step in this direction.
Preliminary outcomes of the MMT CARE intervention are promising. For providers, we observed significant intervention effects on improved MMT knowledge and provider-client interaction at the 6-month follow-up, and elevated perceived clinic support reported at both the 6- and 9-month. Our program evaluation showed that the intervention was well received by providers. The vast majority of them completed the assignment - 73% conducted individual sessions with five or more clients. It is likely and hopeful that trained providers will incorporate the knowledge and communication skills they learned into their routine practice.
This study also evaluated potential connections between client outcomes and sessions delivered by trained providers. Although clients did not participate in the group intervention activities, they showed evident improvement in drug avoidance self-efficacy and a reduction in concurrent drug use at 3-month. In this study, the effort to link provider and client outcomes was exploratory. It is important to establish the connections between providers and clients in future efficacy studies of interventions targeting both providers and clients.
This study identified a provider’s years working in the medical field and occupation as a nurse was significantly associated with clients’ drug avoidance self-efficacy. These findings can inform program improvements. For example, training could be individualized based on occupation or the provider’s work experience. Also, the negative association between stigma perceived by providers and client’s drug avoidance self-efficacy implies the importance of reducing internalized shame among providers in the role of achieving positive client outcomes. It is difficult to explain the unexpected findings in provider MMT knowledge and client drug avoidance self-efficacy; this may be due to the small sample size and the pilot nature of the study. Another explanation could lead to the role of MMT knowledge in treatment services. In a previous study, MMT knowledge was not found to be related to a provider’s willingness to interact with clients or their negative attitude toward drug users, suggesting that information alone is not sufficient to change provider attitudes or their behaviors toward MMT clients [6].
This study offers further evidence of the usefulness of motivational interviewing at MMT clinics [34]. Although MMT clients come to clinics every day for a routine procedure, unless special sessions are scheduled, providers normally interact only briefly with clients. This can become a barrier to effective provider-client communication. In this study, trained providers conducted brief motivational interview sessions with their clients, which could enhance provider-client interaction. Previous studies demonstrated that relationships between providers and clients could be positively associated with treatment outcomes [14,35–38]. Findings from this study further support the importance of the interaction between providers and clients in the context of MMT clinics.
There are limitations to this study. Foremost, data were collected from six clinics in one province of China so caution must be used in generalizing the findings to other geographic areas. Second, issues related to social-desirability bias could be raised because the measures mostly relied on self-reported data. Third, the small sample size and short follow-up period could not provide conclusive evidence of intervention efficacy. Also, some imbalances in background characteristics were observed between intervention and standard care such as clients’ methadone dosage, possibly due to the small sample size. Nonetheless, this study reported important data for future programs targeting MMT providers, including how to localize intervention contents and core messages, how to use tools and participatory activities in implementation, and how to link provider and client outcomes in data analysis.
Acknowledgments
This study was supported by the National Institute of Mental Health (NIMH) Grant R34-MH083512. We thank project team members in Sichuan, Beijing, and Los Angeles for their contributions to this study.
Footnotes
Declaration of Interest: All authors have no conflict declared
Clinical Trial Registration: NCT01532609
References
- 1.Wu ZY, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369(9562):679–90. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.China Ministry of Health, Joint United Nations Programme on HIV/AIDS, World Health Organization. 2011 Estimates for the HIV/AIDS Epidemic in China. 2007 [cited 2012 Feb 13]. Available from: http://news.sciencenet.cn/upload/news/file/2012/1/20121291555312820.pdf.
- 3.Pang L, Hao Y, Mi GD, Wang CH, Luo W, Rou KM, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS. 2007;21(Suppl 8):S103–7. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan GS, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy. 2007;18:118–28. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Cao XB, Pang L, Rou KM, Yin WY, Wang CH, Luo W, et al. Five-year follow-up study of the retention rate and its risk factors for the first 1057 methadone maintenance treatment patients in China. Chinese Journal of AIDS/STD. 2010;16(3):211–4. [Google Scholar]
- 6.Li L, Wu ZY, Cao XB, Zhang LL. Provider-Client Interaction in Methadone Treatment Clinics in China. J Drug Issues. doi: 10.1177/0022042612446593. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin C, Wu ZY, Rou KM, Yin WY, Wang CH, Shoptaw S, et al. Structural-level factors affecting implementation of the methadone maintenance therapy program in China. J Subst Abuse Treat. 2010a;38:119–27. doi: 10.1016/j.jsat.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu EW, Liang T, Shen LM, Wang B, Wu Z, Detels R. Correlates of methadone client retention: A prospective cohort study in Guizhou province, China. Int J Drug Policy. 2009;20(4):304–3. doi: 10.1016/j.drugpo.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin WY, Hao Y, Sun XH, Li F, Li JH, Rou KM, et al. Scaling up the national methadone maintenance treatment program in China: achievements and challenges. Int J Epidemiol. 2010;39(Suppl 2):ii29–37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Darker CD, Sweeney BP, El Hassan HO, Smyth BP, Ivers JH, Barry JM. Brief interventions are effective in reducing alcohol consumption in opiate-dependent methadone-maintained patients: Results from an implementation study. Drug Alcohol Rev. 2011 Sep 15; doi: 10.1111/j.1465–3362.2011.00349.x. [DOI] [PubMed] [Google Scholar]
- 11.DeFulio A, Silverman K. Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: post-intervention outcomes. Addiction. 2011 May;106(5):960–7. doi: 10.1111/j.1360-0443.2011.03364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nyamathi AM, Nandy K, Greengold B, Marfisee M, Khalilifard F, Cohen A, et al. Effectiveness of intervention on improvement of drug use among methadone maintained adults. J Addict Dis. 2011 Jan;30(1):6–16. doi: 10.1080/10550887.2010.531669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heritage J, Maynard DW. Problems and prospects in the study of physician-patient interaction: 30 years o research. Annu Rev Sociol. 2006;32:351–74. [Google Scholar]
- 14.Jackson TR. Treatment practice and research issues in improving opioid treatment outcomes. Science & Practice Perspective. 2002;1(1):22–8. doi: 10.1151/spp021122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthias MS, Parpart AL, Nyland KA, Huffman MA, Stubbs DL, Sargent C, et al. The patient-provider relationship in chronic pain care: providers’ perspectives. Pain Med. 2010 Nov;11(11):1688–97. doi: 10.1111/j.1526-4637.2010.00980.x. [DOI] [PubMed] [Google Scholar]
- 16.Neumann M, Edelhauser F, Kreps GL, Scheffer C, Lutz G, Tauschel D, et al. Can patient-provider interaction increase the effectiveness of medical treatment or even substitute it?--an exploration on why and how to study the specific effect of the provider. Patient Educ Couns. 2010;80:307–14. doi: 10.1016/j.pec.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 17.Lin C, Wu ZY, Rou KM, Pang L, Cao XB, Shoptaw S, et al. Challenges in providing service in methadone maintenance therapy clinics in China: Service providers’ perceptions. Int J Drug Policy. 2010b;21(3):173–8. doi: 10.1016/j.drugpo.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han L, Ling L, Xia Y, Chen W, Chen A, Chen J, et al. Status quo and policy recommendations of methadone maintenance treatment clinics in Guangdong Province. Chinese Journal of Health Policy. 2010;3(3):34–38. [Google Scholar]
- 19.Lin C, Detels R. A qualitative study exploring the reason for low dosage of methadone prescribed in the MMT clinics in China. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chawarski MC, Zhou W, Schottenfeld RS. Behavioral drug and HIV risk reduction counseling (BDRC) in MMT programs in Wuhan, China: A pilot randomized clinical trial. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2010.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hser YI, Li J, Jiang H, Zhang R, Du J, Zhang C, et al. Effects of a randomized contingency management intervention on opiate abstinence and retention in methadone maintenance treatment in China. Addiction. 2011 Oct;106(10):1801–9. doi: 10.1111/j.1360-0443.2011.03490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang YC, Duan S, Xiang LF, Ye RH, Gao J, Yang SS, et al. Adherence and related determinants on methadone maintenance treatment among heroin addicts in Dehong prefecture, Yunnan province. Zhonghua Liu Xing Bing Xue Za Zhi. 2011 Feb;32(2):125–9. [PubMed] [Google Scholar]
- 23.Ministry of Health, China, Joint United Nations Programme on HIV/AIDS, World Health Organization. 2009 Estimates for the HIV/AIDS Epidemic in China. 2010 [cited 2012 Feb 13]. Available from: www.unaids.org.cn/.../2009%20China%20Estimation%20Report-En.pdf.
- 24.Bao YP, Liu ZM. Systematic review of HIV and HCV infection among drug users in China. Int J STD AIDS. 2009 Jun;20(6):399–405. doi: 10.1258/ijsa.2008.008362. [DOI] [PubMed] [Google Scholar]
- 25.Caplehorn J, Irwig L, Saunders JB. Attitudes and beliefs of staff working in methadone maintenance clinics. Subst Use Misuse. 1996;31:437–52. doi: 10.3109/10826089609045820. [DOI] [PubMed] [Google Scholar]
- 26.National MMT working group. Methadone Maintenance Therapy clinical guidance handbook. 2005 [cited 2012 Feb 13]. Available from: http://www.chinaaids.cn/chinammt/download/support/guide2006.pdf.
- 27.Li L, Lin C, Wu ZY, Wu S, Rotheram-Borus MJ, Detels R, et al. Stigmatization and shame: Consequences of caring for HIV/AIDS patients in China. AIDS Care. 2007a;19:258–63. doi: 10.1080/09540120600828473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li L, Liang LJ, Wu ZY, Lin C, Wu S. Institutional Support for HIV/AIDS Care in China: A Multilevel Analysis. AIDS Care. 2008;20(10):1190–6. doi: 10.1080/09540120801919394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin GW, Wilkinson DA, Poulos CX. The drug avoidance self-efficacy scale. J Subst Abuse. 1995;7:151–63. doi: 10.1016/0899-3289(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 30.Ciesla JR, Spear SF. Concordance of Self-Reported Drug Use and Qualitative Urinalysis in Adolescents Treated for Substance Abuse. Clin Drug Invest. 2001;21 (11):789–95. [Google Scholar]
- 31.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 32.Deering DE, Sheridan J, Sellman JD, Adamson SJ, Pooley S, Robertson R, et al. Consumer and treatment provider perspectives on reducing barriers to opioid substitution treatment and improving treatment attractiveness. Addict Behav. 2011 Jun;36(6):636–42. doi: 10.1016/j.addbeh.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present and future. Lancet. 2010;376:268–84. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–61. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 35.Joe GW, Simpon DD, Dansereau DF, Rowan-Szal GA. Relationships between counseling rapport and drug abuse treatment outcomes. Psychiatr Serv. 2001;52:1223–9. doi: 10.1176/appi.ps.52.9.1223. [DOI] [PubMed] [Google Scholar]
- 36.Magura S, Nwakeze PC, Kang SY, Demsky S. Program quality effects on patient outcomes during methadone maintenace: A study of 17 clinics. Subst Use Misuse. 1999;34(9):1299–324. doi: 10.3109/10826089909039410. [DOI] [PubMed] [Google Scholar]
- 37.Simpson DD, Joe GW, Rowan-Szal GA, Greener JM. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997;14(6):565–72. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- 38.Blaney T, Craig RJ. Methadone maintenance. Does dose determine differences in outcome? J Subst Abuse Treat. 1999;16(3):221–8. doi: 10.1016/s0740-5472(98)00031-2. [DOI] [PubMed] [Google Scholar]