Abstract
Post-discharge outcomes following percutaneous coronary intervention (PCI) are important measures of quality of care and complement in-hospital measures. We sought to assess in-hospital and post-discharge PCI outcomes to 1) better understand the relationship between acute and 30 day outcomes, 2) identify predictors of 30-day hospital re-admission, and 3) determine the prognostic significance of 30-day hospital readmission. We analyzed in-hospital death and length of stay (LOS) and non-elective cardiac-related re-hospitalization following discharge in 10,965 patients following PCI in the Dynamic Registry. From 1999–2006, in-hospital death rate and LOS declined. The 30-day cardiac re-admission rate was 4.6%, with considerable variability over time and among hospitals. The risk of re-hospitalization was greater in women, those with CHF, unstable angina, multiple lesions and emergency PCI. Conversely, a lower risk of re-hospitalization was associated with a higher number of treated lesions. Patients re-admitted within 30 days had higher one-year mortality than those free from hospital readmission. In conclusion, while in-hospital mortality and LOS following PCI have decreased over time, the observed 30 day cardiac re-admission rate was highly variable and the risk of re-admission was more closely associated with underlying patient characteristics than procedural characteristics.
Keywords: percutaneous coronary intervention, outcomes, re-admission
Introduction
Hospital length of stay (LOS) and in-hospital mortality following percutaneous coronary intervention (PCI) represent acute process and quality of care measures, respectively (1,2). Important and complementary measures of overall PCI quality are those that occur after hospital discharge (1,3). In fact, in-hospital and post-discharge metrics may be discordant as improvements in acute in-hospital process of care metrics may not translate to improvements in subsequent clinical events (2, 4–6). In addition, the introduction of new technologies may impact acute process and 30 day outcomes differently. As such, there has been a renewed focus not only on LOS (2) but post discharge mortality and re-admission rates following PCI. The latter was addressed in recently published data that suggested substantial and widely variable re-admission rates among hospitals (7). While the study of re-admission rates likely provides an avenue for improving care, this metric leaves much to be desired as the nature of re-admission is complex (8–10). Using a database designed specifically to prospectively assess PCI outcomes, we sought to assess in-hospital and post-discharge PCI outcomes, specifically the 30 day rate of hospital re-admission following PCI. In addition, we examined predictors of re-admission at 30 days and the impact of hospital readmission on one year mortality.
Methods
Details of the purpose, structure, and function of the National Heart, Lung and Blood Institute (NHLBI) sponsored Dynamic Registry have been previously described (11). A total of 10,965 patients undergoing PCI were consecutively enrolled in five recruitment waves between 1997 and 2006: 2,524 patients were recruited from 1997 to 1998, 2,105 patients were recruited in 1999, 2,047 patients were recruited from 2001 to 2002, 2,112 patients were recruited in 2004, and 2,177 patients were recruited in 2006. Patient- and lesion-level data were collected and component and composite rates recorded. Outcomes considered for this analysis included LOS as an acute process measure, as well as rates of in-hospital major adverse cardiac events (MACE) including in hospital death, myocardial infarction (MI), and any repeat target vessel revascularization procedure (acute quality measures). For those patients discharged alive, 30 day cardiovascular re-admission rates, and 30 day and one year mortality were determined. Cardiovascular re-admission was defined as non-elective repeat hospitalization by 30 days in all patients alive at discharge for one or more of the following: angina, MI, coronary artery bypass graft surgery (CABG), non-staged/non-index artery PCI, heart failure or stroke.
Patients participating in the Dynamic Registry consented to the collection of in-hospital and post-discharge data after the index procedure. Study coordinators at each site contacted patients multiple times in the first year and at 1 year to obtain vital status and information regarding intercurrent hospitalizations, cardiovascular events, or procedures. Dates corresponding to all reported outcomes were recorded and confirmed by requesting relevant records. Whenever possible, angiographic data pertaining to repeat PCI were collected and reviewed to determine target-vessel revascularization. Post-discharge follow-up data was available for 97.5%, 94.9%, 90.2%, 99%, and 99% of patients for waves 1–5, respectively. The study protocol was approved by the Institutional Review Boards of the coordinating center (University of Pittsburgh) and all the clinical sites involved.
Statistical analysis
Patients were stratified by 30 day re-admission status. Continuous data were summarized as means ± 1 standard deviation (SD). Categorical variables are summarized as counts or percentages. Overall differences between proportions were assessed by the chi-square test and continuous variables were compared by the Kruskal-Wallis test while the test for trend was assessed with the Mantel-Haenszel test for categorical variables and the ordered Jonckherre-Terpstra test for continuous variables. Similar methods were used for lesion-level analyses. Cumulative event rates at 30d and one year were calculated by the Kaplan–Meier method and compared using the log rank statistic. Patients who did not experience the outcome of interest were censored at the last known date of contact or at thirty days or one-year if contact extended beyond that point. All rates are reported as point estimates. Rates were also adjusted for imbalances in important covariates among waves using general linear modeling methods. In order to examine risk factors associated with a cardiovascular re-admission within 30 days of PCI, a model was built using important clinical, demographic, and procedural factors via Cox proportional hazards methodology. Hazard ratios and their corresponding 95% confidence intervals are reported. All statistical analyses were performed with the use of SAS software, version 9.2, and a two-sided p-value of 0.05 or less was considered to indicate statistical significance.
Results
Over successive periods between 1997 and 2006, there were significant increases in patient age, body mass index, prior revascularization, percent with concomitant non-cardiac disease, diabetes mellitus, hyperlipidemia, heart failure, and hypertension; and a decrease in percent with prior MI (Table 1). Overall stent use increased over time. No drug eluting stents were used prior to 2004 whereas a preponderance were used in the 2004 and 2006 recruitment periods. Procedural success remained unchanged (see Table 2). Radial artery access was used in 3.1% overall, with a trend toward increasing use that peaked at 6.6% in the final 2006 recruitment wave (p<0.0001).
Table 1.
Demographic Characteristics
| Characteristic | 1997–98 (N=2483) |
1999 (N=2077) |
2001–02 (N=2026) |
2004 (N=2083) |
2006 (N=2161) |
P value* |
|---|---|---|---|---|---|---|
| Age, mean, median (years) | 62.5, 63 | 62.9, 63 | 64.3, 65 | 63.6, 64 | 63.9, 64 | <0.001 |
| Age over 65 | 44.1% | 45.2% | 48.8% | 46.3% | 46.5% | 0.066 |
| Women | 35.2% | 36.1% | 36.0% | 32.6% | 32.9% | 0.013 |
| Race | ||||||
| White | 80.0% | 78.1% | 79.1% | 76.9% | 75.1% | 0.982 |
| Black | 7.8% | 12.1% | 12.9% | 14.7% | 16.2% | |
| Asian | 4.8% | 3.9% | 3.8% | 3.0% | 2.1% | |
| Hispanic | 7.2% | 5.7% | 4.1% | 5.3% | 5.8% | |
| Other | 0.2% | 0.2% | 0.1% | 0.0% | 0.7% | |
| Body Mass Index (kg/m2) mean, median |
28.2, 28 | 28.8, 28 | 29.3, 28 | 29.2, 28 | 29.7, 29 | <0.001 |
| Prior Percutaneous Coronary Intervention |
28.2% | 30.7% | 33.2% | 31.9% | 35.4% | <0.001 |
| Prior Coronary Artery Bypass Surgery |
16.4% | 17.0% | 19.6% | 19.9% | 17.8% | 0.147 |
| Prior Myocardial Infarction Severe Non-Cardiac |
39.1% | 32.5% | 27.6% | 26.2% | 22.6% | <0.001 |
| Concomitant Disease | 29.4% | 33.6% | 38.4% | 36.7% | 36.0% | <0.001 |
| Cerebrovascular | 6.0% | 6.4% | 6.8% | 8.0% | 6.8% | 0.042 |
| Renal | 3.3% | 4.8% | 7.1% | 8.3% | 8.7% | <0.001 |
| Peripheral Vascular | 7.1% | 7.1% | 9.0% | 8.7% | 7.4% | 0.176 |
| Pulmonary | 6.8% | 8.8% | 8.2% | 7.6% | 7.7% | 0.613 |
| Cancer | 5.6% | 6.7% | 7.6% | 7.7% | 7.4% | 0.006 |
| Other | 8.4% | 10.6% | 15.4% | 14.5% | 11.2% | <0.001 |
| Diabetes Mellitus | 27.5% | 28.5% | 30.2% | 33.2% | 34.2% | <0.001 |
| Congestive Heart Failure | 9.7% | 9.3% | 12.4% | 9.2% | 10.1% | 0.694 |
| Hypertension | 59.2% | 64.4% | 74.7% | 77.1% | 78.2% | <0.001 |
| Hyperlipidemia | 61.3% | 63.6% | 71.7% | 75.2% | 79.2% | <0.001 |
| Smoking | ||||||
| Never | 34.4% | 32.1% | 33.3% | 37.5% | 36.0% | 0.041 |
| Current | 25.4% | 27.1% | 24.0% | 22.6% | 25.6% | |
| Former | 40.1% | 40.8% | 42.7% | 39.9% | 38.4% |
Test for trend patients from successive recruitment periods discharged alive.
Table 2.
Angiographic / Procedural Characteristics
| Characteristic | 1997–98 (N=2483) |
1999 (N=2077) |
2001–02 (N=2026) |
2004 (N=2083) |
2006 (N=2161) |
P value* |
|---|---|---|---|---|---|---|
| Abnormal Left Ventricular Ejection Fraction | 26.8% | 27.1% | 31.1% | 30.7% | 28.7% | 0.044 |
| Left Ventricular Ejection Fraction, mean, median | 55.2, 56 | 53.3, 55 | 51.6, 55 | 51.8, 55 | 52.7, 55 | <0.001 |
| Number Significant Lesions, mean, median | 2.9, 2 | 2.9, 2 | 3.1, 3 | 3.1, 3 | 3.1, 3 | <0.001 |
| Amenable to Complete Coronary Artery Bypass Surgery Revascularization |
87.4% | 85.4% | 82.6% | 76.0% | 72.1% | <0.001 |
| Amenable to Complete Percutaneous Coronary Intervention Revascularization |
81.4% | 81.2% | 81.8% | 87.0% | 90.2% | <0.001 |
| Revascularization reason | ||||||
| Asymptomatic | 2.2% | 4.7% | 8.5% | 10.1% | 14.5% | <0.001 |
| Stable Angina Pectoris | 25.1% | 20.6% | 20.0% | 23.0% | 18.8% | <0.001 |
| Unstable Angina Pectoris | 47.3% | 45.8% | 41.9% | 34.9% | 32.7% | <0.001 |
| Acute Myocardial Infarction | 18.5% | 25.7% | 27.8% | 27.8% | 28.8% | <0.001 |
| Other | 6.9% | 2.7% | 1.4% | 1.7% | 1.8% | <0.001 |
| Cardiogenic shock | 1.1% | 1.4% | 1.6% | 0.7% | 1.1% | 0.282 |
| Circumstances of Procedure | ||||||
| Elective | 66.7% | 51.7% | 51.9% | 77.8% | 65.9% | 0.001 |
| Urgent | 16.2% | 41.7% | 27.8% | 15.9% | 25.9% | |
| Emergent | 17.2% | 6.7% | 20.4% | 6.3% | 8.2% | |
| Lesion ACC/AHA Classification | ||||||
| A | 10.0% | 13.1% | 16.2% | 10.6% | 11.6% | 0.013 |
| B1 | 29.3% | 32.8% | 34.2% | 35.9% | 29.7% | |
| B2 | 39.8% | 38.2% | 30.3% | 32.3% | 29.5% | |
| C | 20.9% | 15.9% | 19.3% | 21.1% | 29.2% | |
| Treatment strategy | ||||||
| Stent use (overall) | 67.6% | 79.2% | 86.1% | 93.3% | 95.6% | <0.001 |
| Eluting Stent use (overall) | 0% | 0% | 0% | 65.2% | 82.8% | <0.001 |
| In hospital Myocardial Infarction | 2.6% | 2.7% | 1.8% | 2.4% | 1.7% | 0.0919 |
| In hospital Q-wave MI/Emergency Coronary Artery Bypass Surgery |
0.7% | 0.5% | 0.2% | 0.2% | 0.1% | <0.001 |
| Overall Angiographic Success | ||||||
| None | 3.3% | 2.7% | 2.2% | 2.2% | 2.1% | <0.001 |
| Partial | 4.2% | 4.2% | 3.2% | 2.3% | 1.6% | |
| Total | 92.5% | 93.1% | 94.7% | 95.5% | 96.3% | |
| Procedure Success (angiographic, without death /Q wave Myocardial Infarctions/ Emergent Coronary Artery Bypass Surgery) |
96.3% | 97.0% | 97.6% | 97.6% | 97.8% | 0.0069 |
Test for trend in patients from successive recruitment periods discharged alive
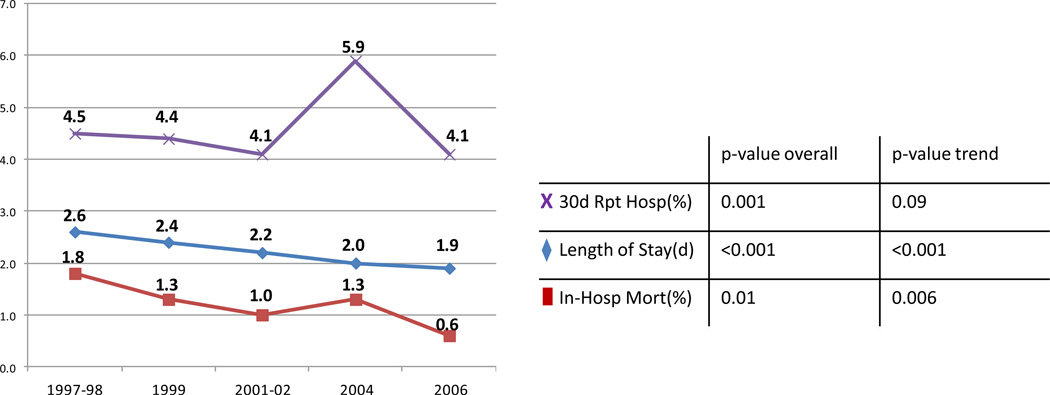
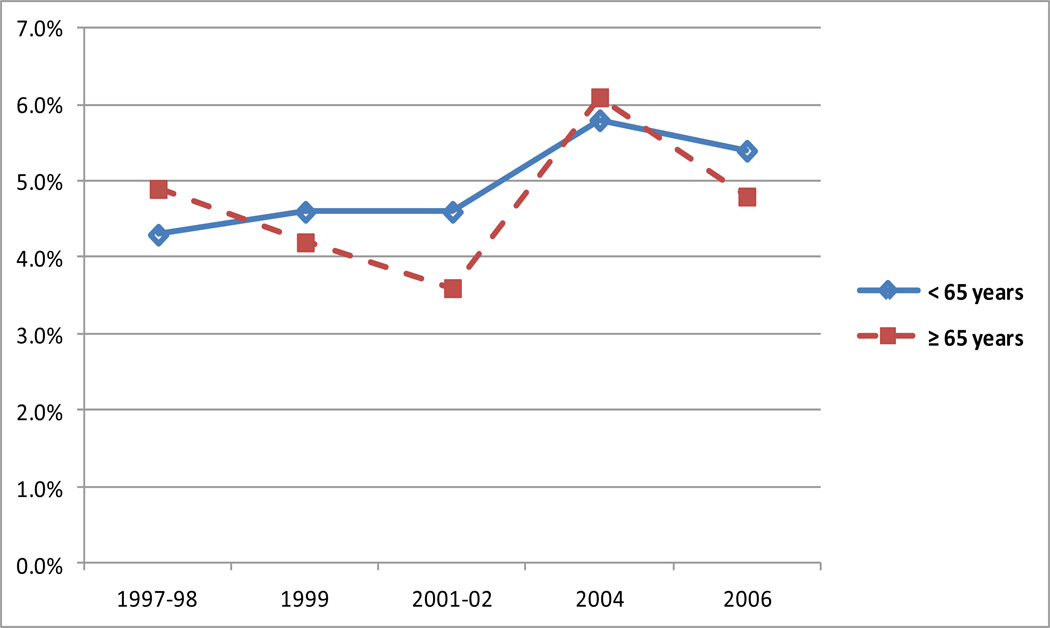
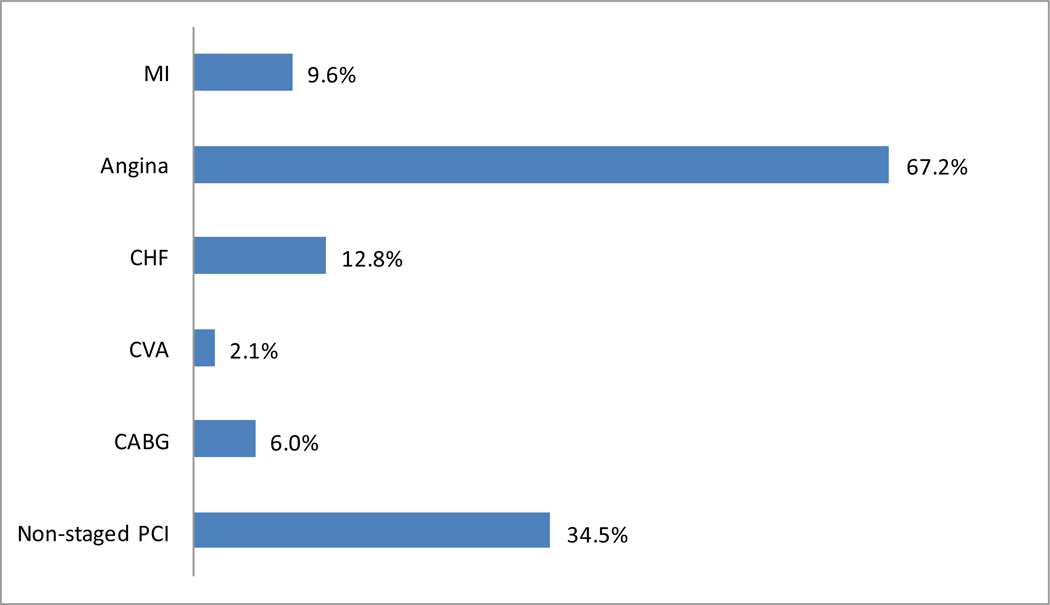
Over time, in-hospital mortality improved significantly and LOS shortened. Over the same time period, there was considerable variability in 30 day cardiac re-admission rates (Figure 1). The cardiac-related re-admission rate among those discharged alive was 4.6% (95% CI 3.5–5.7) and ranged from 0 to 14.3% across the 27 sites. The cardiac re-admission rate for the period 2001–02 (where only 90.2% follow up was achieved compared to the 95–99% follow up rates for the rest of the recruitment periods), was estimated by imputation to be between 4.9% and 5.2%. Cardiac readmission rates for those < 65 years (n=5835) and those ≥ 65 years (n=4985) were similar (Figure 2). The distribution of cardiac-related reasons for re-admission is shown in Figure 3.
Figure 1. Trends in In-Hospital and 30 Day Outcomes Following PCI.
X shows the 30-day repeat hospitalization rates;◊ shows the length of hospital stay in days;□ shows the in-hospital mortality rate.
Figure 2. Re-Hospitalization Rate by Age.
Cardiac Readmission Rates Over Successive Periods For Patient Age Less Than 65 And 65 Years And Older. The average readmission rate for the entire cohort less than 65 years was 4.9% and 4.7% for those 65 years or older.
Figure 3. Cardiovascular-Related Reasons For Readmission.
For those discharged alive and re-hospitalized within 30 days of discharge. Hospitalization can be for more than one reason. MI = myocardial infarction, CHF = congestive heart failure, CVA = cerebrovascular accident, CABG = coronary artery bypass graft surgery.
Tables 3 and 4 show demographic, angiographic, and procedural characteristics for those patients discharged alive according to 30 day re-admission status. Those characteristics independently associated with re-hospitalization by 30 days of discharge are shown in Table 5. As demonstrated, there were no procedural predictors, but several patient-related variables associated with the risk of re-hospitalization. While female sex, CHF, acute coronary syndromes, co-morbid conditions, a larger number of significant lesions, and emergent PCI were associated with a greater risk of re-hospitalization, increasing numbers of lesions treated by PCI was associated with a lower risk of readmission.
Table 3.
Demographic Characteristics Stratified by Re-hospitalization Status
| Rehospitalization | ||||
|---|---|---|---|---|
| Characteristic | Total (n=10,829) |
No (n=10,345) |
Yes (n=484) |
P value* |
| Age, mean, median (years) | 63.4, 64 | 63.4, 64 | 63.2, 63 | 0.9147 |
| Age over 65 | 46.1% | 46.1% | 45.5% | 0.7803 |
| Women | 34.6% | 34.2% | 41.5% | 0.0010 |
| Race | ||||
| White | 77.9% | 78.0% | 77.1% | 0.8037 |
| Black | 12.6% | 12.6% | 12.0% | |
| Asian | 3.5% | 3.5% | 4.3% | |
| Hispanic | 5.7% | 5.6% | 6.4% | |
| Other | 0.2% | 0.3% | 0.2% | |
| Body Mass Index (kg/m2), mean, median | 29.0, 28 | 29.0, 28 | 28.7, 28 | 0.1814 |
| Prior Percutaneous Coronary Intervention | 31.7% | 31.6% | 35.2% | 0.1218 |
| Prior Coronary Artery Bypass Surgery | 17.9% | 17.7% | 20.9% | 0.1299 |
| Prior Myocardial Infarction | 29.9% | 29.9% | 30.5% | 0.7865 |
| Severe Non-Cardiac | ||||
| Concomitant Disease | 34.6% | 34.2% | 42.3% | 0.0003 |
| Cerebrovascular | 6.8% | 6.7% | 9.1% | |
| Renal | 6.4% | 6.4% | 6.2% | 0.8750 |
| Peripheral Vascular | 7.8% | 7.8% | 9.5% | 0.1525 |
| Pulmonary | 7.9% | 7.8% | 10.0% | 0.0892 |
| Cancer | 7.0% | 7.0% | 6.4% | 0.6461 |
| Other | 11.8% | 11.6% | 17.0% | 0.0003 |
| Diabetes Mellitus | 30.6% | 30.5% | 34.0% | 0.1039 |
| Congestive Heart Failure | 10.1% | 9.9% | 14.3% | 0.0019 |
| Hypertension | 70.3% | 70.2% | 73.5% | 0.1222 |
| Hyperlipidemia | 70.1% | 70.0% | 71.2% | 0.5830 |
| Smoking | ||||
| Never | 34.7% | 34.5% | 38.2% | 0.0518 |
| Current | 25.0% | 24.9% | 27.0% | |
| Former | 40.3% | 40.6% | 34.9% | |
Stratification variable is re-hospitalizations for cardiac reasons within 30 days of discharge from index PCI
For patients discharged alive
Table 4.
Angiographic / Procedural Characteristics Stratified by Re-hospitalization Status
| Re-hospitalization | ||||
|---|---|---|---|---|
| Characteristic | Total (n=10,829) |
No (n=10,345) |
Yes (n=484) |
P value* |
| Abnormal Left Ventricular Ejection Fraction | 28.9% | 28.7% | 33.5% | 0.0479 |
| Left Ventricular Ejection Fraction, mean, median | 52.9, 55% | 52.9%, 55% | 52.0%, 55% | 0.1985 |
| Number Significant Lesions, mean, median Amenable to Complete Coronary Artery | 3.0, 2 | 3.0, 2 | 3.4, 3 | <.0001 |
| Bypass Surgery Revascularization Revascularization | 80.6% | 80.7% | 79.5% | 0.5443 |
| Amenable to Complete Percutaneous Coronary Intervention Revascularization | 84.4% | 84.5% | 81.7% | 0.1103 |
| Revascularization reason | ||||
| Asymptomatic | 8.0% | 8.1% | 6.0% | 0.1011 |
| Stable Angina Pectoris | 21.6% | 21.9% | 15.3% | 0.0005 |
| Unstable Angina Pectoris | 40.7% | 40.5% | 45.0% | 0.0480 |
| Acute Myocardial Infarction | 25.5% | 25.2% | 31.6% | 0.0017 |
| Other | 2.8% | 2.9% | 1.7% | 0.1131 |
| Cardiogenic shock | 1.2% | 1.1% | 2.7% | 0.0017 |
| Circumstances of Procedure | ||||
| Elective | 58.3% | 58.8% | 49.6% | <.0001 |
| Urgent | 31.0% | 30.9% | 34.5% | |
| Emergent | 10.6% | 10.4% | 15.9% | |
| Lesion ACC/AHA Classification | ||||
| A | 12.2% | 12.2% | 13.4% | 0.2813 |
| B1 | 32.2% | 32.4% | 29.1% | |
| B2 | 34.2% | 34.1% | 36.3% | |
| C | 21.3% | 21.3% | 21.2% | |
| Treatment strategy | ||||
| Stent use (overall) | 77.8% | 77.8% | 78.3% | 0.7552 |
| Eluting Stent use (overall) | 28.2% | 28.0% | 32.5% | 0.0123 |
| In hospital Myocardial Infarction | 2.3% | 2.2% | 3.3% | 0.1106 |
| In hospital Q-wave MI/Emergency | ||||
| Coronary Artery Bypass Surgery | 0.4% | 0.4% | 0.4% | 0.8991 |
| Overall Angiographic Success | ||||
| None | 2.5% | 2.4% | 3.9% | 0.0733 |
| Partial | 3.1% | 3.1% | 2.3% | |
| Total | 94.4% | 94.4% | 93.8% | |
| Procedure Success (angiographic, without death/Q wave MI / Emergent CABG), % | 97.2% | 97.3% | 95.7% | 0.0289 |
Stratification variable is re-hospitalizations for cardiac reasons within 30 days of discharge from index PCI.
For patients discharged alive
Table 5.
Predictors of Rehospitalization Within 30 Days Of Discharge From Index PCI
| Hazard Ratio | 95% CI | p-value | |
|---|---|---|---|
| Age | 0.99 | 0.98–1.00 | 0.02 |
| Women | 1.39 | 1.14–1.68 | <0.001 |
| Body Mass Index | 0.98 | 0.96–1.00 | 0.03 |
| Congestive Heart Failure | 1.41 | 1.07–1.87 | 0.02 |
| Co-morbid condition | 1.31 | 1.08–1.59 | 0.006 |
| Reason for revascularization (versus other) | |||
| Stable Angina Pectoris | 1.12 | 0.75–1.67 | 0.57 |
| Unstable Angina Pectoris | 1.66 | 1.16–2.37 | 0.006 |
| Acute Myocardial Infarction | 1.52 | 1.02–2.26 | 0.04 |
| Number significant lesions | 1.15 | 1.08–1.22 | <0.001 |
| Number lesions treated | 0.84 | 0.73–0.98 | 0.03 |
| Acuity (versus elective) | |||
| Urgent | 1.15 | 0.92–1.44 | 0.21 |
| Emergent | 1.53 | 1.11–2.12 | 0.01 |
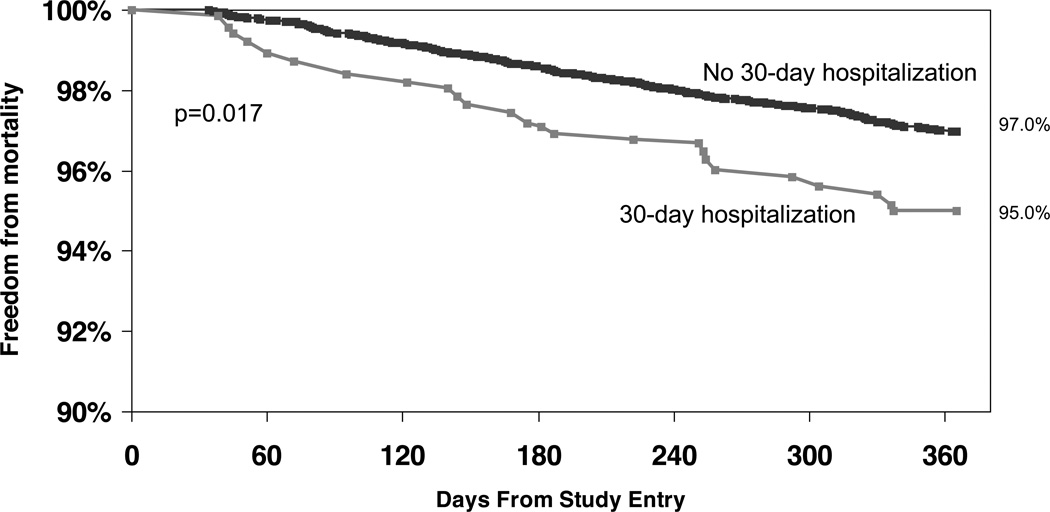
After adjusting for baseline differences between groups, the risk for mortality by 1 year for the non re-hospitalized group compared to those hospitalized at least once in the first 30 days after index PCI is shown in Figure 4 and suggests that re-admitted patients are at higher risk for death at one year. Even after accounting for baseline differences, 30-day cardiac hospitalization was an independent predictor for mortality at one year (Table 6).
Figure 4. Adjusted Freedom From Mortality By 30-Day Cardiac Re-Hospitalization Status.
Adjusted one year survival curves using the inverse probability weight method for those who experienced a 30-day re-hospitalization compared to those who did not are shown. Those who died in the 30-day period from discharge were excluded. The solid line represents the non-hospitalized group (n=10328), the dashed line represents the group that had been hospitalized at least once in the first 30-days (n=455).
Table 6.
Adjusted Hazard Ratios and 95% CIs for Mortality From Day 31-365
| Cox Proportional Hazards | |||
|---|---|---|---|
| Hazard Ratio | 95% CI | p-value | |
| 30-day hospitalization | 1.56 | 1.03–2.36 | 0.035 |
| Age | 1.03 | 1.02–1.05 | <0.001 |
| Race | |||
| Black | 1.32 | 0.97–1.81 | 0.08 |
| Asian | 1.42 | 0.79–2.56 | 0.205 |
| Hispanic | 1.25 | 0.75–2.10 | 0.40 |
| Body mass index (versus <25) | |||
| 25.0–29.9 | 0.55 | 0.42–0.72 | <0.001 |
| ≥30 | 0.54 | 0.40–0.73 | <0.001 |
| Diabetes Mellitus | 1.67 | 1.30–2.14 | <0.001 |
| Congestive Heart Failure | 2.14 | 1.64–2.79 | <0.001 |
| Double Vessel Coronary Disease | 1.13 | 0.82–1.56 | 0.46 |
| Triple Vessel Coronary Disease | 1.34 | 0.96–1.87 | 0.09 |
| Cardiogenic shock | 2.05 | 0.96–4.36 | 0.06 |
| Co-morbid conditions | |||
| Chronic Kidney Disease | 2.34 | 1.75–3.13 | <0.001 |
| Peripheral Vascular Disease | 1.37 | 1.01–1.85 | 0.04 |
| Chronic Lung Disease | 1.66 | 1.23–2.25 | <0.001 |
| Cancer | 1.67 | 1.22–2.28 | 0.001 |
Discussion
In this analysis of PCI outcomes over time, we observed stable and high procedural success rates, decreasing in-hospital mortality, and decreasing LOS. Notwithstanding these improvements in acute care outcomes and processes of care, there was discordance with, and variability in, the 30 day cardiac re-hospitalization rate over time. There was increased mortality risk at one year for re-admitted patients. While several patient-level characteristics were associated with a greater risk of re-hospitalization at 30 days, there was no such association with any procedure-related variables. These findings highlight the complex nature of assessing PCI quality and provide further insight into cardiac readmission rate following PCI and its clinical significance.
In the current era of public reporting and linking of payment to patient outcomes (12–16), it behooves us to critically assess PCI quality metrics such as rates of repeat hospitalization following PCI. With procedures like PCI, where low event rates may coexist with inconsistent data collection mechanisms, the link between specific outcomes and operator or hospital performance is problematic (17, 18), even with adjudication (19). In addition, there may be poor correlation between risk-adjusted outcomes and preventable outcomes (20). The present analysis corroborates others that suggest that PCI outcomes may not be directly related to the procedure itself but to patient-specific and/or health care system factors (21–23).
Metrics such as 30 day re-admission rate do not lend themselves to explicit implications and are the product of a complex set of incentives and external regulatory forces (24). Two recent retrospective analyses, one from a Medicare database (7) and the other from 22 Massachusetts hospitals (25), reported all cause post- PCI re-admission rates of 1 in 7 (14%) and 1 in 8 (12.5%) following PCI, respectively. Our prospective analysis revealed a cardiac re-admission rate of 1 in 22 PCI procedures (4.6%) and no significant difference between those 65 or older and those under 65 years of age. A third retrospective analysis from a single center reported a 9.4% all cause (and 6.5% cardiac) re-admission rate following PCI (26).
The complex nature of readmission following PCI is further demonstrated in this analysis by the potential way in which new technology and new innovation with device therapy may confound attempts to measure post-procedural quality. As noted in Figure 1, re-admission rates increased during the 2004 recruitment period despite contemporaneous decreases in mortality and LOS. This recruitment period spanned the time of the FDA public health notification of adverse events associated with the Cordis CYPHER™ Coronary Stent (27). Secular changes in PCI practice may also confound interpretation of re-admission rates via temporal changes in procedural and patient selection criteria and may explain, in part, the apparent increase in PCI in the “asymptomatic” subgroup in the registry. Many of the latter patients were previously symptomatic but were asymptomatic at the time of PCI. In addition, a substantial fraction of patients were undergoing the second of a planned staged PCI for multivessel revascularization.
Our detailed prospective analysis suggests that patient characteristics (namely female gender, heart failure, acute coronary syndromes, multiple significant lesions, emergent procedures and the presence of non-cardiac co-morbid conditions) more strongly predict 30 day cardiac re-admission than procedural characteristics. Further evidence for this is supported by our observation that more extensive PCI (greater number of lesions treated) was associated with a lower 30 day re-admission rate. Importantly, we note lower one year survival for those readmitted within 30 days after index PCI. Increased efforts to target this group of patients at discharge are warranted and are an important part of the “transition of care” process. (28–30)
This analysis is limited by the fact that there have been many secular changes in reimbursement and hospital discharge policies over the time period studied. Because of this, it is difficult to draw convincing conclusions regarding cause and effect relationships. The Dynamic Registry collected all data prospectively. Follow-up rates consistently exceeded 90% and were carefully documented and substantiated.
References
- 1.The Centers for Medicare & Medicaid Services (CMS) Hospital Quality Initiatives; Outcome Measures. https://www.cms.gov/HospitalQualityInits/20_OutcomeMeasures.asp.
- 2.Chambers CE, Dehmer GJ, Cox DA, Harrington RA, Babb JD, Popma JJ, Turco MA, Weiner BH, Tommaso CL. Defining the Length of Stay Following Percutaneous Coronary Intervention: An Expert Consensus Document From the Society for Cardiovascular Angiography and Interventions. Catheterization and Cardiovascular Interventions. 2009;73:847–858. doi: 10.1002/ccd.22100. [DOI] [PubMed] [Google Scholar]
- 3.Laskey WK, Selzer F, Jacobs AK, Cohen HA, Holmes DR, Jr, Wilensky RL, Detre KM, Williams DO. NHLBI Dynamic Registry Investigators. Importance of the Postdischarge Interval in Assessing Major Adverse Clinical Event Rates Following Percutaneous Coronary Intervention. American Journal of Cardiology. 2005;95:1135–1139. doi: 10.1016/j.amjcard.2005.01.038. [DOI] [PubMed] [Google Scholar]
- 4.Rosen CA. Length of stay. How short should hospital care be? European Journal of Public Health. 2001;11:166–170. doi: 10.1093/eurpub/11.2.166. [DOI] [PubMed] [Google Scholar]
- 5.Hernandez AF, Fonarow GC, Liang L, Heidenreich PA, Yancy C, Peterson ED. The Need for Multiple Measures of Hospital Quality. Results from the Get With The Guidelines–Heart Failure Registry of the American Heart Association. Circulation. 2011;124:712–719. doi: 10.1161/CIRCULATIONAHA.111.026088. [DOI] [PubMed] [Google Scholar]
- 6.Hernandez AF, Curtis LH. Minding the gap between efforts to reduce re-admissions and disparities. JAMA. 2011;305:715–716. doi: 10.1001/jama.2011.167. [DOI] [PubMed] [Google Scholar]
- 7.Curtis JP, Schreiner G, Wang Y, Chen J, Spertus JA, Rumsfeld JS, Brindis RG, Krumholz HM. All-cause re-admission and repeat revascularization after percutaneous coronary intervention in a cohort of Medicare patients. Journal of the American College of Cardiology. 2009;54:903–907. doi: 10.1016/j.jacc.2009.04.076. [DOI] [PubMed] [Google Scholar]
- 8.Kereiakes DJ. Return to Sender: Hospital Re-admission After Percutaneous Coronary Intervention. Journal of the American College of Cardiology. 2009;54:908–910. doi: 10.1016/j.jacc.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 9.Jencks SF, Williams MV, Coleman EA. Re-hospitalizations among patients in the Medicare Fee-for-Service Program. New Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 10.Epstein AM. Revisiting Re-admissions – Changing the Incentives for Shared Accountability. New Engl J Med. 2009;360:1457–1459. doi: 10.1056/NEJMe0901006. [DOI] [PubMed] [Google Scholar]
- 11.Williams DO, Holubkov R, Yeh W, Bourassa MG, Al-Bassam M, Block PC, Coady P, Cohen H, Cowley M, Dorros G, Faxon D, Holmes DR, Jacobs A, Kelsey SF, King SB, 3rd, Myler R, Slater J, Stanek V, Vlachos HA, Detre KM. Percutaneous coronary intervention in the current era compared with 1985–86. The National Heart, Lung and Blood Institute Registries. Circulation. 2000;102:2945–2951. doi: 10.1161/01.cir.102.24.2945. [DOI] [PubMed] [Google Scholar]
- 12.Secretarial review and publication of the annual report to congress submitted by the contracted consensus-based entity regarding performance measurement. Fed Regist. 2009;74:46594–46603. [Google Scholar]
- 13.Bernheim SM, Grady JN, Lin Z, Wang Y, Wang Y, Savage SV, Bhat KR, Ross JS, Desai MM, Merrill AR, Han LF, Rapp MT, Drye EE, Normand ST, Krumholz HM. National Patterns of Risk-Standardized Mortality and Re-admission for Acute Myocardial Infarction and Heart Failure: Update on Publicly Reported Outcomes Measures Based on the 2010 Release. Circulation: Cardiovascular Quality and Outcomes. 2010;3:459–467. doi: 10.1161/CIRCOUTCOMES.110.957613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 15.Orszag PR, Emanuel EJ. Health care reform and cost control. New Engl J of Med. 2010;363:601–603. doi: 10.1056/NEJMp1006571. [DOI] [PubMed] [Google Scholar]
- 16.Patient protection and affordable care act. [Accessed May 1, 2010]; Public Law No: 111-148. Available at: http://thomas.loc.gov/cgi-bin/thomas.
- 17.Thomas JW, Hofer TP. Accuracy of risk-adjusted mortality rate as a measure of hospital quality of care. Medical Care. 1999:83–92. doi: 10.1097/00005650-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Kuntz RE, Normand ST. Measuring Percutaneous Coronary Intervention Quality by Simple Case Volume. Circulation. 2005;112:1088–1091. doi: 10.1161/CIRCULATIONAHA.105.561126. [DOI] [PubMed] [Google Scholar]
- 19.Barringhaus KG, Zelevinsky K, Lovett A, Normand ST, Ho KK. Impact of Independent Data Adjudication on Hospital-Specific Estimates of Risk-Adjusted Mortality Following Percutaneous Coronary Interventions in Massachusetts. Circulation: Cardiovascular Quality and Outcomes. 2011;4:92–98. doi: 10.1161/CIRCOUTCOMES.110.957597. [DOI] [PubMed] [Google Scholar]
- 20.Guru V, Tu JV, Etchells E, Anderson GM, Naylor CD, Novick RJ, Feindel CM, Rubens FD, Teoh K, Mathur A, Hamilton A, Bonneau D, Cutrara C, Austin PC, Fremes SE. Relationship between preventability of death after coronary artery bypass graft surgery and all-cause risk adjusted mortality rates. Circulation. 2008;117:2969–2976. doi: 10.1161/CIRCULATIONAHA.107.722249. [DOI] [PubMed] [Google Scholar]
- 21.Resnic FS, Welt FGP. The public health hazards of risk avoidance associated with public reporting of risk-adjusted outcomes in coronary intervention. Journal of the American College of Cardiology. 2009;53:825–830. doi: 10.1016/j.jacc.2008.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Califf RM, Peterson ED. Public Reporting of Quality Measures. What Are We Trying to Accomplish? Journal of the American College of Cardiology. 2009;53:831–833. doi: 10.1016/j.jacc.2008.10.056. [DOI] [PubMed] [Google Scholar]
- 23.Yeh RW, Rosenfield K, Zelevinsky K, Mauri L, Sakhuja R, Shivapour DM, Lovett A, Weiner BH, Jacobs AK, Normand SL. Circulation: Cardiovascular Interventions. 2012;5:227–236. doi: 10.1161/CIRCINTERVENTIONS.111.967638. [DOI] [PubMed] [Google Scholar]
- 24.Joynt KE, Jha AK. Thirty-Day Readmissions–Truth of Consequences. New Engl J Med. 2012;366:1366–1368. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 25.Yeh RW, Zelevinsky K, Normand SLT, Sakhuja R, Lovett A, Weiner BH, Rosenfield KA. 30-Day All-Cause Re-admission After Percutaneous Coronary Intervention in Massachusetts: Clinical Predictors and Hospital-Variation of a New Quality Metric. Circulation. 2010;122:A18716. [Google Scholar]
- 26.Khawaja FJ, Shah ND, Lennon RJ, Slusser JP, Alkatib AA, Rihal CS, Gersh BJ, Montori VM, Holmes DR, Bell MR, Curtis JP, Krumholz HM, Ting HH. Factors Associated With 30-Day Readmission Rates After Percutaneous Coronary Intervention. Archives of Internal Medicine. 2011;172:112–117. doi: 10.1001/archinternmed.2011.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.FDA Public Health Notification of Adverse Events Associated with the Cordis CYPHER™ Coronary Stent. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm064528.htm.
- 28.Coleman EA, Parry C, Chalmers S, Min SJ. The Care Transitions Intervention: results of a randomized controlled trial. Archives of Internal Medicine. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 29.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O'Donnell JK, Paasche-Orlow MK, Manasseh C, Martin S, Culpepper L. A reengineered hospital discharge program to decrease re-hospitalization: a randomized trial. Annals of Internal Medicine. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stauffer Brett D, Fullerton Cliff, Fleming Neil, Ogola Gerald, Herrin Jeph, Stafford Pamala Martin, Ballard David J. Effectiveness and Cost of a Transitional Care Program for Heart Failure: A Prospective Study With Concurrent Controls. Archives of Internal Medicine. 2011;171:1238–1243. doi: 10.1001/archinternmed.2011.274. [DOI] [PubMed] [Google Scholar]