Abstract
Background:
Idiopathic cutaneous hyperchromia at the orbital region (ICHOR) is a cutaneous hyperchromia characterised by bilateral darkening of the eyelid and orbital skin that contrasts with the adjoining facial skin. ICHOR is frequent in dark skin. It interferes with the face appearance which often causes difficulties in societal acceptance and may impact quality of life.
Objective:
The aim of this investigation was to study the epidemiology, clinical features and risk factors associated with ICHOR in Indian patients and also to study the distribution of melanin and haemoglobin in ICHOR patients. This study also assessed the relevance of SIAscopy technique (spectrophotometric intracutaneous analysis (SIA)), a new objective non-invasive method to measure melanin and haemoglobin concentration in vivo.
Materials and Methods:
Thirty-three patients diagnosed with ICHOR at the All India Institute of Medical Sciences, New Dehli, India, were included in the study. Epidemiological data were collected through a self-administrated questionnaire. Standard photographs were taken from each patient and SIAscopy measurements were done on dark circles and normal skin.
Results:
Surprisingly our study showed no significant correlation between ICHOR prevalence and family history, atopic and contact dermatitis, contemporaneous melasma and hormonal factors. The study confirms that sun exposure is a risk factor of dark circles aggravation. Indeed patients tend to reduce sun exposure after the onset of dark circles. SIAscopy analysis reveals significant differences in the concentration of total melanin, of dermal melanin and of haemoglobin between ICHOR skin and normal skin of the same patient.
Conclusion:
This study confirms that melanin deposits and blood stasis in dark circles may play a role in ICHOR pathogenesis and cause the darkening of skin under eyes. SIAscopy provides objective diagnostic information about ICHOR.
KEYWORDS: Idiopathic cutaneous hyperchromia of the orbital region, periorbital pigmentation, dark circles around the eyes
INTRODUCTION
Cutaneous hyperchromia of the orbital region is characterised by bilateral darkening of the eyelid and orbital skin that contrasts with the adjoining facial skin. It is also known as periorbital melanosis, dark circles, infraorbital pigmentation, idiopathic cutaneous hyperchromia at the orbital region (ICHOR). Hyperchromia of the orbital region can be subdivided into primary and secondary types. The first type is ICHOR, which is characterised by bilateral darkening of the eyelid and orbital skin that is not secondary to systemic or local diseases.[1] The second type is hyperchromia associated with systemic or local diseases of a known cause. It affects individuals of any age, both genders and all races. The condition worsens with skin sagging and abnormal lipid deposits that appear later in life.[2] It is aesthetically very annoying. Dark circles interfere with the face appearance, giving the patient a tired, sad, or hangover look, which often causes difficulties in societal acceptance and may impact quality of life.
Little is known regarding the epidemiological characteristics of ICHOR. Periorbital hyperpigmentation is characterised by dark circles around the eyes, which are not uncommon, often familial, and frequently found in individuals with dark pigmentation or Mediterranean ancestry.[3] Under-eye circles are common complaint by both men and women. ICHOR may extend from the eye to the cheekbone and halfway down the sides of the nose root. The medial region of the eyelids is usually darker than other areas.[4] Some studies indicated a greater incidence of ICHOR complaint among individuals with darker hair, eyes and skin.[4,5] In 1965, Winkelmann[6] suggested that the darkening of the periorbital and eyelid regions associated with severe diseases was a consequence of dehydration in an area with little subcutaneous tissue. The effect of light on this tissue would favour a faint bluish colouration. In 1966, Marks[7] made an association between hyperchromia of the skin in the orbital region and allergic rhinitis in children. The pathogenesis of such discolouration would come from venous stasis. It was reported to be more commonly found in women[4] but other authors related a male to female ratio of 1:1.[2] ICHOR is rare in infancy and does not occur in newborns. It seems to be more common among adults but may be present in individuals from childhood onwards. It appears to be more prevalent among people of mixed race and Jewish origin. Unfortunately most of these observations come from case reports. No appropriate epidemiologic studies exist up to date.[4,8]
ICHOR does not have a clear etiopathogenesis. Several aetiological factors have been suggested: genetic transmission, excessive sun exposure, endogenous or exogenous estrogens and progestagens, pregnancy, post-inflammatory hyperpigmentation, excessive subcutaneous vascularisation and hypertransparency of the skin, periorbital oedema and herniation of the eyelid skin fat.
The most common primary cause of ICHOR is hyperpigmentation of the skin, which results from melanin deposits in the dermis. Melanin deposits in the dermis may be congenital (primary) or secondary to environmental factors such as: excessive exposure to the sun, endogenous or use of exogenous estrogens and progestagens,[9] pregnancy and breast-feeding. Another possible cause of dark circles is the presence of prominent superficial vasculature, visible on the lower eyelid. The hypervascular appearance is due to the combination of excess subcutaneous vascularisation and hypertransparency of the skin.[10,11] In 1937, Touraine[12] noticed that the vessels became more visible because of loss of subcutaneous fat and muscle tonus in the region. More recently Ohshima confirmed the importance of dermal thickness in the appearance of dark circles.[13] Any inflammation or vasodilation in this area may manifest as darkening. The presence of a shadow due to periorbital oedema, eyelid skin slackness,[10] “excess” of skin[14] or herniation of the eyelid skin fat[15] may also contribute towards hyperchromia of the orbital region. The worsening of the darkened region of lower eyelid with time appears to be due to gravitational effect and actinic damage. Force of gravity acting on an area with little subcutaneous tissue and little support causes the skin to move downward, thereby becoming stretched and thinned and allowing the underlying vessels and orbicular musculature to become more apparent.[16] Exposure to ultraviolet radiation causes skin thinning and increases melanin and vessel content, thus favouring the darkening of this region.[11] The degree of hyperchromia appears to vary with some factors such as fatigue, the menstrual cycle, bouts of flu and other situations of physical and mental stress.[17] This indicates that a dynamic factor may be present. There is probably greater dermal vessel clogging during such periods. However, the histology of dark circles has been scarcely performed and in most studies, the presence of melanin inside dermal macrophages was shown as a consequence of pigmentary incontinence.[5,10,14,18–21]
Evaluating the concentration of melanin and haemoglobin in dark circles is important to better understand ICHOR. Objective and non-invasive methods are needed to measure melanin concentration in vivo in human skin. The current methods are limited by lack of specificity and inability to resolve spatial distribution of the perplexing chromophore, haemoglobin. A new device, SIAscopy (spectrophotometric intracutaneous analysis (SIA)),[22–25] has been developed by Cotton and Claridge[22] then Astron Clinica (Cambridge, UK), providing an objective non-invasive method to measure melanin concentration in vivo. It allows the concentration and distribution of eumelanin, oxyhaemoglobin and dermal collagen to be measured in vivo.
The aim of this investigation was to study the epidemiology, clinical features and risk factors associated with ICHOR in Indian patients and also to study the distribution of melanin and haemoglobin in ICHOR patients with SIAscopy technique.
MATERIALS AND METHODS
Patients
Patients with dark circles were recruited at the Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. A total of 33 patients (11 males, 22 females) with ICHOR diagnosed by clinical examination were included in the study. Patients suffering from pigmentary dermacations lines were excluded from the study. Mean age was 28 years (range 14–48 years). Among the study patients, 18 had previously experienced treatments of dark circles. All patients were of phototype ≥ IV. All patients gave written informed consent. The study was approved by the Institute's ethics committee.
Epidemiological analysis
Epidemiological data were investigated through a self-administrated questionnaire. Information regarding the duration of outdoor activities and sun exposure before and after onset of ICHOR, the extension of ICHOR lesions and the co-morbidity of ICHOR with other disease such as melasma was collected.
Photographs
Full face standardised photos of all patients were taken with Canfield VISIA CR® device (Canfield Imaging Systems, Fairfield, USA). Three types of photographs were systematically made: Standard flash, Cross Polarised and Ultra violet-A (UVA) lightening. Those three types of photograph allow skin pigmentation to be examined. The standard flash type is close to clinical observation; the cross polarised type allows the effects of surface such as brightness to be suppressed and skin pigmentation to be more precisely visualised; the UVA lighting allows superficial melanin to be brought out.
Spectometric analysis: SIAscopy technique
Spectrophotometric intracutaneous analysis (SIAscopy) is a method of analysing pigmented skin lesions non-invasively. Compared with dermoscopy which highly depends on the skills and experience of the examiner, SIAscopy is based on objective features such as the presence of dermal pigment, vascularity of the lesion and the integrity of collagen.
The SIAscopy technique was used to study melanin and haemoglobin distribution within the skin.The technique is based on a unique combination of dermatoscopy, contact remittance spectrophotometry and hyperspectral imaging. SIA analysis arose from research undertaken at the University of Birmingham in the UK where the colours arising from skin lesions were being investigated with the aim of identifying objective diagnostic information.
The SIAscope operates by probing the skin spectrally over a 24 × 24 mm or 12 × 12 mm area with radiation ranging from 400 to 1000 nm. Eight narrow-band spectrally filtered images of the skin are recorded, calibrated and used as inputs to a series of complicated computer algorithms that extract information regarding the microarchitecture of the skin. The wavelengths of the wavebands are chosen to interact preferentially with skin constituents.[22,23,25] The SIA algorithm first utilises the infrared wavebands to ascertain the amount of collagen within the papillary dermis at every point over the skin lesion. This is a crucial step for this technique since it provides a necessary transformation on the wavebands for accurate extraction of total melanin and haemoglobin. The total melanin, collagen and haemoglobin SIAgraphs can now be displayed. The effect of these chromophores on the wavebands is then removed, allowing a key piece of diagnostic information, the presence of melanin below the dermal epidermal junction, to be identified. It is made possible because the spectral remittance of melanin changes with regard to its position in the superficial anatomical layers of the skin, namely the epidermis and the papillary dermis. Using SIAscopy the accuracy of this identification is extremely high and gives the dermal melanin SIAgraph.[23]
In short, the SIAscope is able to obtain a high resolution composite white-light image of the skin over a defined area and provides four additional, mutually exclusive chromophore maps that show the concentration of melanin in epidermis and haemoglobin, collagen and melanin in the papillary dermis, pixel by pixel [Figure 1].
Figure 1.
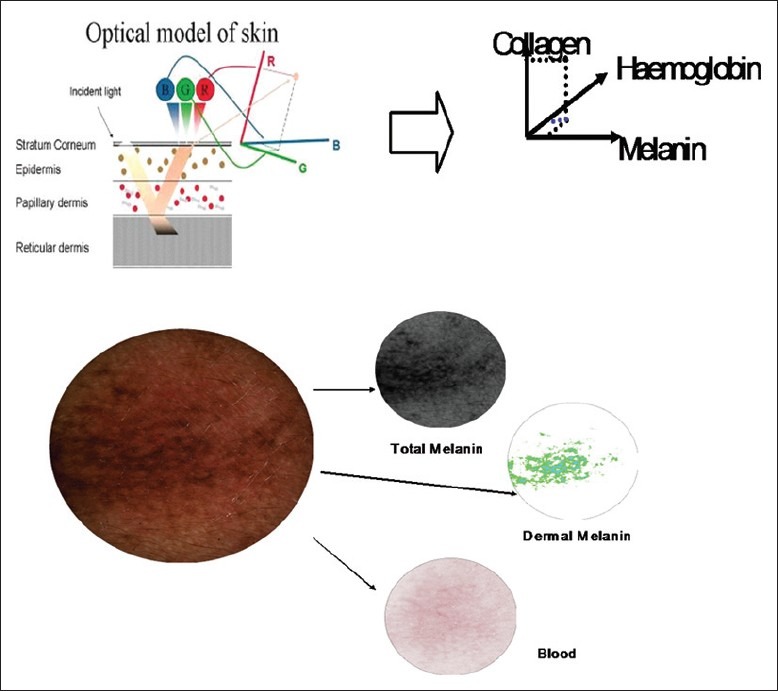
Schema representing the SIAscopy technique
In our study SIAscopy measurements were done on dark circles (left and right side), and normal skin on the cheek of each patient.
RESULTS
Epidemiological results
Onset and duration
The mean length of ICHOR in the 33 study patients was 13 years (range 2–48 years). Seventeen patients had dark circles for less than 10 years, nine patients for a time length between 10 and 20 years and seven patients for more than 20 years. The latter showed dark circles with the largest surface area.
Risks factors
Family history was also recorded. Among 33 patients 7 had family history of ICHOR. The extension of dark circles to the cheekbone and sides of the face was not linked to family history of dark circles.
Patients were also questioned and examined for personal history of contact dermatitis and atopic dermatitis. Out of 33 patients, 7 patients had contact dermatitis of the eyelids, 5 had atopic dermatitis and 1 patient had both contact and atopic dermatitis. Contact dermatitis and atopic dermatitis were not correlated with ICHOR extension. It was striking that none of the patients with atopic background showed extensive dark circles.
We found no correlation with hormonal factors: pregnancies, menstruation, contraception and menopause and no correlation with drug intake.
Regarding UV light exposure, on average the patients had been exposed for more than 22 hours per week before the onset of dark circles. The majority of patients reduced the number of hours of outdoor sun exposure after the onset of dark circles. The mean time of sun exposure was dropped to 14.3 hours per week. Dark circles could be graded according to four severity grades (1 to 4) and it was found that the mean average sun exposure for patients with grade 3–4 was 16.5 hours per week (18 patients) whereas it was 20.5 hours per week for patients with grades 1 and 2 (n = 13).
Among the explored risk factors, Melasma co-morbidity was checked. In fact, among 33 patients with dark circles, only 9 patients had a concomitant melasma.
Photographs
Typical photographs were obtained with the Canfield VISIA CR® device. Dark circles are well visible.
For darker skin types, UVA light does not distinguish DC from the rest of the face since melanin is highly present across the face [Figures 2 and 3].
Figure 2.

Typical photographs obtained with the Canfield VISIA CR® device (Canfield Imaging Systems, Fairfield, USA); From left to right, Skin VISIA standard flash, Cross Polarised and c-Ultra violet-A (UVA) lightening, respectively
Figure 3.
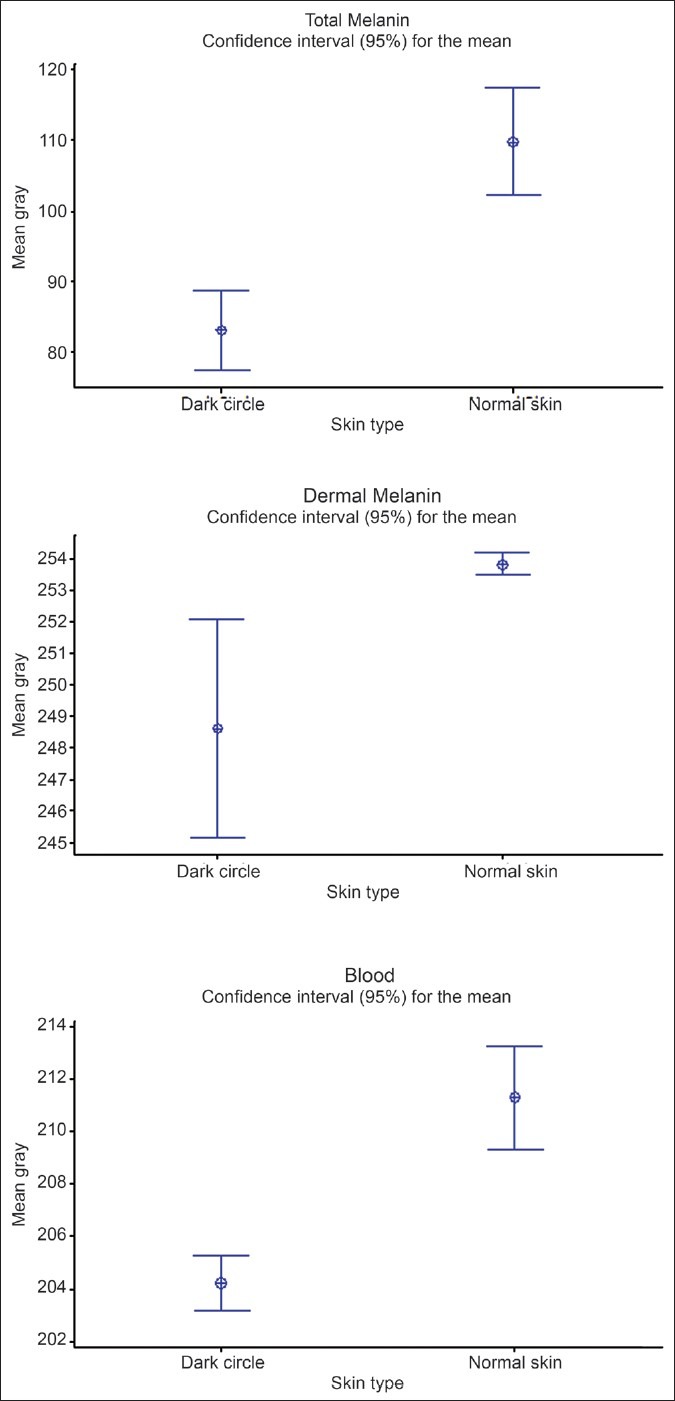
Graphic representation of SIAscopy results: Total melanin, Dermal melanin and haemoglobin content in dark circle versus normal skin
SIAscopy results
Each SIAscan (haemoglobin, total melanin and dermal melanin; collagen was not analysed) was converted into grey levels and the mean of grey levels is calculated. The mean of Grey levels is inversely proportional to the concentration of each component.
The results of SIAscan allowed us to compare the content of epidermal melanin, total melanin and haemoglobin in dark circles and in normal skin (cheeks) [Table 1].
Table 1.
Results of SIAscan
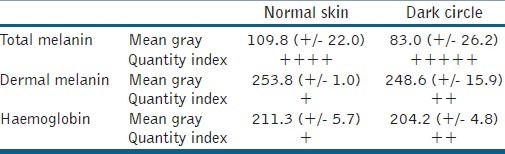
The SIAscopy results show that total melanin and dermal melanin contents are higher in dark circles than in normal skin. The content of dermal melanin is particularly low in normal skin. It is higher in dark circle skin, but a high variability is noted [Figure 3]. As regards haemoglobin content, it is also higher in DC skin than in normal skin.
DISCUSSION
Although ICHOR is considered as a disorder within the limit of physiology, patients, especially women, are really bothered and concerned about it, even relating a significant impairment on their quality of life owing to the presence of dark circles.
Our study shows surprising epidemiological results compared with the literature. They have to be confirmed in a larger study. No significant correlation between ICHOR prevalence and family history has been found, and the extension of lesions does not appear to be linked to a family history. In contrast, there are studies showing the evidence of a family character, with dominant autosomal inheritance and variable expression of the genes involved.[5,18,19] In 1962, Hunzinker[19] described a family whose 10 members were affected by ICHOR, including an 8-year-old girl. Goodman and Belcher[18] reported 22 individuals with ICHOR affecting six generations of a single family. Subsequently, they described three other families, one included 11 members with ICHOR over two generations. In 1969, Maruri and Diaz[5] described 20 affected individuals over three generations of another family. Nevertheless, there is no concrete evidence that might confirm genetic transmission, and it does not emerge from our study. Whereas post-inflammatory hyperpigmentation is believed to be secondary to atopic or allergic contact dermatitis,[10,15] we have not found here any correlation between extension of dark circles and atopic and contact dermatitis. Our study also does not give evidence of any correlation with contemporaneous melasma as only 9 patients out of 33 had melasma. No involvement of ICHOR with hormonal factors, such as pregnancies, menstruation, contraception, menopause, etc., has been identified. Nevertheless this study confirms that sun exposure is a risk factor of dark circles aggravation. Indeed patients tend to reduce sun exposure after the onset of dark circles. This is confirmed by correlating the severity grade with current time of solar exposure: the more severe dark circles are, the shorter current sun exposure time is.
SIAscopy analysis reveals significant differences in the content of total melanin, of dermal melanin and of haemoglobin between ICHOR skin and normal skin of the same patient. This confirms that melanin deposits and the presence of blood in dark circles may play a role in ICHOR pathogenesis and cause the darkening of skin under eyes. The majority of the histological studies on ICHOR have shown the presence of melanin inside dermal macrophages which seems to be an important factor in hyperchromia genesis of the periorbital skin.[5,10,14,18] The disorder seems to consist of pigment incontinence.[19–21] Histological characteristics of infraorbital darkening suggest that they are caused by multiple etiologic factors that include dermal melanin deposits, post-inflammatory hyperpigmentation secondary to atopic or allergic contact dermatitis, periorbital oedema, superficial location of vasculature and shadowing due to skin laxity.[10] Watanabe et al.[26] studied periorbital biopsies of 12 Japanese patients with DC and showed that all of them had dermal melanosis revealed by histology. According to the authors, melanosis could be interpreted as dermal melanocytosis based on the findings of the anti-S100 protein and Masson–Fontana silver staining. However, if melanocytosis is a fixed finding, what could explain the daily fluctuation in these patients’ condition? The authors speculated that thickening of the dermis, caused by oedema, led to an enhanced incidence of diffused light reflection from the pigments resulting in increased darkness of the skin. They came to this conclusion based on the works by West et al.[27] who successfully treated infraorbital pigmentation using carbon dioxide (CO2) laser, without any corresponding improvement in melanin spectrometric readings. The latter authors speculated that the efficacy of CO2 laser depended on the tightening of dermal tissues and improvement in the skin surface texture, which caused the Tyndall effect. Therapeutic options are still limited and most of the time unsatisfactory. The presence of dermal melanin could explain the difficulties to obtain good results. However a study by Elson[11] that evaluated the use of vitamin K combined with retinol 0.15% for the treatment of periorbital hyperpigmentation demonstrated that this preparation was effective in improving under-eye circle in 93% of the patients. For now, it seems certain that the best treatment options at patients’ disposal are sunscreens and increased rest.
SIA provides objective information regarding skin colour. Indeed when we assess skin pigmentation subjectively by eye it is always confounded by the presence of haemoglobin. In simple terms, while the human eye has superb contrast sensitivity[28] (down to only 2% of full brightness) and can distinguish adjacent browns and reds with ease, it becomes virtually impossible to separate visually and/or communicate reliably the relative contributions of melanin and haemoglobin when they overlay one another, as is the case both in young or photoprotected skin (very homogeneous distribution of each chromophore) and in older photodamaged skin (e.g. co-location of telangiectasia and lentigos or diffuse hyperpigmentation). Visual assessment, therefore, is at best semiquantitative and certainly not linear. Objective approaches to determining skin colour in vivo centre on spectrophotometric or colorimetric ones and the use of derived colour coordinates, various digital imaging and image analysis techniques, reviewed in full by Pierard.[29] SIA provides objective diagnostic information with the investigation of colours arising from skin lesions.[22,23,25] It has become apparent that analysis of purely visual colour information is insufficient to extract reliable diagnostic information relating to the lesion's internal structure and that it is necessary to extend the analysis into the infrared to extract such information. The result of this research is a technique capable of rapidly imaging a skin lesion in vivo and allowing the distribution, location and quantity of a range of chromophores, including melanin, blood and collagen within the papillary dermis and the location of melanin relative to the dermal epidermal junction to be examined. The clinical device based on this technique is termed a SIAscope and it returns SIAgraphs showing those constituents for interpretation and for ICHOR diagnosis. Astron Clinica has developed Non contact SIAscopy™ (NCS) that overcomes the limitations of a skin contact probe. NCS is implemented[30] using an essentially conventional (although finely calibrated) digital camera and lighting system and may be used to acquire large-field eumelanin and oxyhaemoglobin chromophore maps.
CONCLUSION
In conclusion, our results show that SIAscopy can be used as a useful tool to provide diagnostic information about ICHOR. The accuracy of identification of the chromophores melanin, haemoglobin and collagen using SIAscopy is extremely high. The presence of melanin deposits and presence of blood stasis in dark circles may play a role in its pathogenesis and cause the darkening of skin under eyes. SIAscopy is of major help in providing objective diagnostic information about dark circles. Despite their prevalence and cosmetic importance, there are few reported studies in the scientific literature about dark circles. Even a good definition of this condition is lacking. As there is neither a general understanding about dark circle pathogenesis nor a consensus about the major responsible features, treatments are chosen in a simplified way, thus giving suboptimal results most of the time. It is important to identify the specific anatomic problem of each patient in order to individualise treatment. No study has ever investigated the levels of melanin, haemoglobin and collagen using SIAscopy. This is the maiden attempt on the status of melanin, haemoglobin and collagen in ICHOR patients using SIAscopy. This study may add some insight in explaining the role of melanin and blood in the pathophysiology of ICHOR. Further studies in a larger patient cohort might verify whether investigation of these chromophores using SIAscopy may help in identifying objective diagnostic information in patients with ICHOR.
ACKNOWLEDGEMENT
We would like to thank Laurent Petit from Galderma Recherche for his help regarding SIAscopy measurements and statistical analysis.
Footnotes
Source of Support: University of Nice, France.
Conflict of Interest: None declared.
REFERENCES
- 1.Graziosi AC, Quaresma MR, Ferreira LM, Michalany NS. Histopathologic study of cutaneous idiopathic hyperchromia of the orbital region. Dermatol Surg. doi: 10.1007/s00266-012-0048-2. [in press] [DOI] [PubMed] [Google Scholar]
- 2.Yaar M, Gilchrest BA. Skin aging: Postulated mechanisms and consequent changes in structure and function. Clin Geriatr Med. 2001;17:617–30. doi: 10.1016/s0749-0690(05)70089-6. [DOI] [PubMed] [Google Scholar]
- 3.William J, Berger T, Elston D. Andrews’ diseases of the skin: Clinical dermatology. 10th ed. Philadelphia: Saunders; 2005. [Google Scholar]
- 4.Aguilera Díaz L. Pathology and genetics of bipalperbral hyperpigmentation. Actas Dermosifiliogr. 1971;62:397–410. [PubMed] [Google Scholar]
- 5.Maruri CA, Diaz LA. Dark circles around the eyes. Cutis. 1969;5:979–82. [Google Scholar]
- 6.Winkelmann RK. Dark circles under the eyes. JAMA. 1965;193:161. [Google Scholar]
- 7.Marks MB. Allergic shiners. Dark circles under the eyes in children. Clin Pediatr (Phila) 1966;5:655–8. doi: 10.1177/000992286600501106. [DOI] [PubMed] [Google Scholar]
- 8.Bingel A. Heritability. Eugenics and population policy. Münch Med Wschr. 1937;84:1531–2. [Google Scholar]
- 9.Garcia A, Fulton JE., Jr The combination of glycolic acid and hydroquinone or kojic acid for the treatment of melasma and related conditions. Dermatol Surg. 1996;22:443–7. doi: 10.1111/j.1524-4725.1996.tb00345.x. [DOI] [PubMed] [Google Scholar]
- 10.Lowe NJ, Wieder JM, Shorr N, Boxrud C, Saucer D, Chalet M. Infraorbital pigmented skin. Preliminary observations of laser therapy. Dermatol Surg. 1995;21:767–70. [PubMed] [Google Scholar]
- 11.Elson ML, Nacht S. Treatment of periorbital hyperpigmentation with topical vitamin K/vitamin A. Cosm Dermatol. 1999;12:32–4. [Google Scholar]
- 12.Touraine A. Dermatoses: Symptomatic visceral lesions. Surgical Medical Encyclopedia, Dermatology. 1937;2:14. [Google Scholar]
- 13.Ohshima H, Takiwaki H. Evaluation of dark circles of the lower eyelid: Comparison between reflectance meters and image processing and involvement of dermal thickness in appearance. Skin Res Technol. 2008;14:135–41. doi: 10.1111/j.1600-0846.2007.00277.x. [DOI] [PubMed] [Google Scholar]
- 14.Boxrud C, Shorr N, Stensapir K. American Society of Ophthalmologic Plastic and Reconstructive Surgeons. Chicago: 1993. Management of dark circles around the eyes; p. 129. [Google Scholar]
- 15.Epstein JS. Management of infraorbital dark circles. A significant cosmetic concern. Arch Facial Plast Surg. 1999;1:303–7. doi: 10.1001/archfaci.1.4.303. [DOI] [PubMed] [Google Scholar]
- 16.Elson ML. Evaluation and treatment of the aging face. New York: Springer-Verlag; 1994. pp. 1–8. [Google Scholar]
- 17.Duke-Elder S. The eyelids. The ocular adnexae. In: Duke-Elder S, editor. Text of ophtalmology. St Louis: Mosby; 1952. pp. 364–71. [Google Scholar]
- 18.Goodman RM, Belcher RW. Periorbital hyperpigmentation. An overlooked genetic disorder of pigmentation. Arch Dermatol. 1969;100:169–74. doi: 10.1001/archderm.100.2.169. [DOI] [PubMed] [Google Scholar]
- 19.Hunzinker N. About familial hyperpigmentation of eyelids. J Génét Hum. 1962;11:16–21. [PubMed] [Google Scholar]
- 20.Miescher G, Stork H. Pigment incontinence of xanthoma palpebrarum. Dermatologica. 1951;102:366. [Google Scholar]
- 21.Jadassohn W, Franceschetti A, Golay M. Clinical comments on skin pigmentation. Dermatologica. 1954;108:225–34. [PubMed] [Google Scholar]
- 22.Cotton SD, Claridge E. Developing a predictive model of human skin colouring. Proc SPIE. 1996;2708:814–25. [Google Scholar]
- 23.Cotton SD, Claridge E, Hall PN. Non-invasive skin imaging. In: Duncan J, Gindi G, editors. Proceedings of Information Processing in Medical Imaging. London: Springer-Verlag; 1997. pp. 501–6. [Google Scholar]
- 24.Moncrieff M, Cotton SD, Claridge E, Hall PN. Spectrophotometric intracutaneous analysis-a new technique for imaging pigmented skin lesions. Br J Dermatol. 2002;146:448–57. doi: 10.1046/j.1365-2133.2002.04569.x. [DOI] [PubMed] [Google Scholar]
- 25.Cotton SD. A non-invasive imaging system for assisting in the diagnosis of malignant melanoma. PhD thesis. UK: Birmingham University; 1988. [Google Scholar]
- 26.Watanabe S, Nakai K, Ohnishi T. Condition known as “dark rings under the eyes” in the Japanese population is a kind of dermal melanocytosis which can be successfully treated by Q-switched ruby laser. Dermatol Surg. 2006;32:785–9. doi: 10.1111/j.1524-4725.2006.32161.x. [DOI] [PubMed] [Google Scholar]
- 27.West TB, Alster TS. Improvement of infraorbital hyperpigmentation following carbon dioxide laser resurfacing. Dermatol Surg. 1998;24:615–6. doi: 10.1111/j.1524-4725.1998.tb04216.x. [DOI] [PubMed] [Google Scholar]
- 28.Campbell FW, Robson JG. Application of fourier analysis to the visibility of gratings. J Physiol. 1968;197:551–66. doi: 10.1113/jphysiol.1968.sp008574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pierard GE. EEMCO guidance for the assessment of skin colour. J Eur Acad Dermatol Venereol. 1998;10:1–11. doi: 10.1016/s0926-9959(97)00183-9. [DOI] [PubMed] [Google Scholar]
- 30.Preece S, Cotton SD, Claridge E. Imaging the pigments of skin with a technique which is invariant to changes in surface geometry and intensity of illuminating light. In: Barber D, editor. Proceedings of Medical Image Understanding and Analysis. Malvern: British Machine Vision Association; 2003. p. 145. [Google Scholar]


