Abstract
To enhance the accuracy of radioactive seed implants in the head and neck, a digital model individual template, containing information simultaneously on needle pathway and facial features, was designed to guide implantation with CT imaging. Thirty-one patients with recurrent and local advanced malignant tumors of head and neck after prior surgery and radiotherapy were involved in this study. Before 125I implants, patients received CT scans based on 0.75mm thickness. And the brachytherapy treatment planning system (BTPS) software was used to make the implantation plan based on the CT images. Mimics software and Geomagic software were used to read the data containing CT images and implantation plan, and to design the individual template. Then the individual template containing the information of needle pathway and face features simultaneously was made through rapid prototyping (RP) technique. All patients received 125I seeds interstitial implantation under the guide of the individual template and CT. The individual templates were positioned easily and accurately, and were stable. After implants, treatment quality evaluation was made by CT and TPS. The seeds and dosages distribution (D90,V100,V150) were well meet the treatment requirement. Clinical practice confirms that this approach can facilitate easier and more accurate implantation.
Keywords: Digital model, individual template, radioactive seeds, head and neck
INTRODUCTION
Radioactive seed brachytherapy has been used in radiotherapy for many years [1, 2]. Today, permanent radioactive seed implantation is used for the treatment of prostate cancer, breast cancer and cancer of the head and neck [2–8]. Many radioactive isotopes have been used, including 198Au, 192Ir, 125I, and 103Pb [7–10].
One of the advantages of brachytherapy is that it allows delivery of a higher radiation dose to the tumor while at the same time sparing the surrounding normal tissue [7]. In general, a treatment plan containing information on the position and direction of the implantation needles, and the expected distribution of seeds and dosages is required pre-treatment to ensure that an adequate dose is delivered to the target volume, and that a relatively low dose is delivered to adjacent normal tissue. Needles and seeds thus need to be arranged according to the treatment plan during the implantation process. Many techniques have been developed to improve the accuracy of implantation. Modern imaging techniques, such as ultrasound, CT and MRI, play an important role in improving visibility during implantation [6, 11, 12]. Template guidance is used to enhance accuracy and efficiency of the procedure [13].
Traditionally, interstitial implantation for prostate cancer is performed using transperineal template and transrectal ultrasound guidance [2, 13]. The accuracy of implantation for the treatment of malignant tumors of the head and neck has not been fully explored to date. As a result of complex anatomy in this region, implantation is more difficult and the application of ultrasound is limited. Furthermore, as a result of head and neck flexibility and posture changes between planning and treatment, the use of conventional template products can lead to error in terms of patient positioning, as well as direction errors, which may influence treatment accuracy. In addition, it may result in a decrease in the dose delivered to the target volume and increase the dose delivered to adjacent normal tissue, both of which may influence the effectiveness of treatment and the occurrence and severity of complications. These disadvantages limit the application of conventional template products when implanting radioactive seeds in the head and neck region.
In order to enhance the accuracy of interstitial implantation, we designed an individual template using a computer aid design (CAD) and rapid prototyping (RP) technique, and implanted radioactive seeds using this individual template and CT guidance.
MATERIALS AND METHODS
Thirty-one patients (17 males and 14 females) aged between 2 and 86 years (median, 68 years) received permanent implantation of 125I seeds (model 6711, 4.5 mm long and 0.8 mm in diameter, China Institute of Atomic Energy) between August 2010 and November 2011, for recurrent and locally advanced malignant tumors of the head and neck. The tumor site included the parotid and buccal areas, the upper neck, the mouth floor, the base of the tongue, the paranasal sinus, the nasal cavity, the skull base (infratemporal fossa) and the periorbital area. The prescription dose (peripheral matching dose) was 80 to 120 Gy for recurrent tumors in areas that had previously received radiotherapy and 120 to 160 Gy for tumors without prior radiotherapy. This study was approved by the Ethics Committee of Peking University, and all patients gave their informed consent for use of their data.
The protocol for 125I interstitial implantation brachytherapy was as follows:
Preparation
Before implantation, patients underwent CT scanning based on a thickness of 0.75 mm. Data was saved in DICOM format. Patient posture during CT examination was the same as the predicted posture during implantation.
Implantation plan
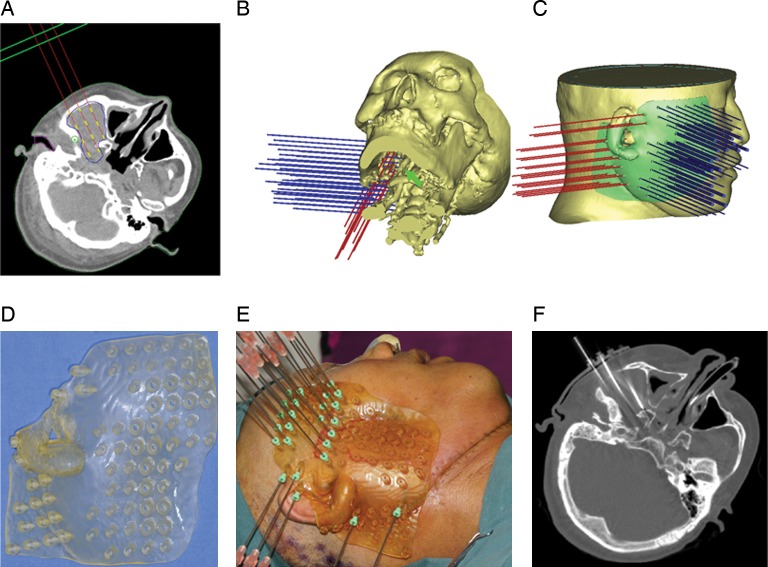
The brachytherapy treatment planning system (BTPS, Beijing Atom and High Technique Industries Inc., Beijing, China) software for Windows XP was used to read information from CT images and to construct the implantation plan (Fig. 1A). In the plan, needles were implanted from different directions to avoid bone, major blood vessels and important organs (Fig. 1B). The CT images, including planned information on number, position, and direction of the implant needles, were then exported and saved in DICOM format.
Fig. 1.
(A) BTPS was used to construct the treatment plan (the red line represents the implant needle, and the yellow line represents the 125I seeds); (B) the treatment plan in three-dimensional (3-D) images, showing how the mandibular ramus and major blood vessels (green arrow) were avoided; the needles are implanted in two directions; (C) the individual template was designed according to the 3-D appearance of the skin in the head and neck region and from information on the implantation needles; (D) an individual template of the parotid, infratemporal fossa and mandibular ramus region; (E) interstitial implantation guided by the individual template; (F) CT image showing the implant needles at the expected site under individual template guidance.
Design and production of the individual template
The Mimics 10.01 for windows (Materialise, Belgium) was used initially to read CT and needle information, and then used to reconstruct the three-dimensional (3-D) appearance of the head and neck region and implantation needles in the correct positions (Fig. 1C). The 3-D data was then exported to software Geomagic 8.0 (Geomagic Company, USA) in an STL format. The individual template was designed according to the 3-D appearance of the skin using Geomagic software, and ideally covering a marking point, such as the nose, the lower border of mandible, the zygoma or the ear, which could facilitate placement of the template in the correct position (Fig. 1C). The thickness of the template (6 mm in our study) and the diameter of the implantation needles (18G interstitial needles in our treatment) were then determined, and the Boolean minus operation was applied to obtain an image of the individual template that contained the needle information. According to the digital model, the individual template was constructed from the medial light-cured resin using the rapid forming machine Eden250 (Objet Company, Israel). An individual template of the parotid, infratemporal fossa and mandibular ramus regions can be seen in Fig. 1D.
Interstitial implantation
Under general anesthesia, the needles were implanted using the individual template and CT guidance, to ensure that all needles were in the expected position and depth, which was calculated in BTPS (Fig. 1E, 1F). Following this, 125I seeds were implanted in the tissues via the needles, in accordance with the implantation plan. Finally, a further CT examination was performed to verify and guarantee that the seeds were distributed in the correct position.
Verification and quality assurance of treatment
CT images of the seeds were used to calculate the D90, V100, V150 and dosages at organs at risk after treatment by BTPS.
RESULTS
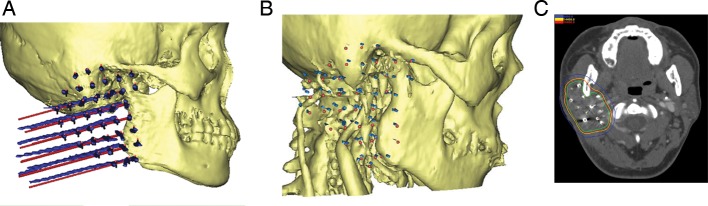
All digital model individual templates at the different sites, containing information on the position, direction and diameter of the implantation needles, were successfully produced. And the templates were well fitted and stable in the designed position. The implantations were performed in strictly accordance with the implantation plan under individual template and CT guide (Fig. 1E and 1F). All needles were in the designed position, and the seeds achieved an acceptable distribution (Fig. 2A and 2B).
Fig. 2.
(A) Actual needles implanted in the planned site. The blue line or dot represents the actual needles, and the red line or dot represents the planned needles; (B) the implanted seeds achieving the expected distribution. (The blue dots represent the actual seed distribution, and the red dots represent the planned seed distribution); (C) this CT image shows the isodose curve after seed implantation (The green curve represents the target area, and the red, yellow and blue curves represent the 160 Gy, 144 Gy and 80 Gy isodose curves, respectively.)
In this study, the D100 was 134.5 ± 22.4 Gy in mean (range from 89 Gy to 178 Gy),and it was larger than the prescription dose in 90.3% (28/31) patients; the D90 was 173.6 ± 24.5 Gy in mean(range from 127 Gy to 225 Gy) and it was larger than the prescription dose in every patient. The V100 was 99.7 ± 0.9% in mean (range from 96% to 100%), and the V150 was 29.9 ± 7.1% in mean (range from 18% to 41%). In this series, the D90, V100 and V150 achieved met the treatment plan requirements in every case (Fig. 2C), and dosages delivered to organs at risk were within acceptable limits of tolerance.
DISCUSSION
With current developments in the application of the template and the transrectal ultrasound guidance technique, brachytherapy plays an increasingly important role in the treatment of prostate cancer, and the template guidance technique has now become standard treatment [13, 14]. As imaging techniques develop, CT and MRI technology, which can enhance visibility during treatment, are also used to guide radioactive seed implantation. Owing to the complexity of the structure of the head and neck, use of ultrasound is limited. Therefore, CT-guided 125I implantation has been increasingly used in the head and neck region [6].
However, the template guidance technique, which can enhance the accuracy of implantation and can simplify operation procedures, has developed slowly for the treatment of malignant head and neck tumors. The anatomical structure of this area is complex, with many vital organs, all of which make implantation more challenging. Thus, it is difficult to identify a fixed site for a template when treating malignant tumors in different sites in the head and neck region. Furthermore, as the head and neck moves, there can be an associated patient and/or template set-up error, which may significantly influence the accuracy of implantation. For these reasons, we designed an individual template, which has many advantages. Firstly, it contains information on local facial features of each patient, which can decrease the set-up error and can remain stable in the right position (Fig. 1E). Secondly, it contains information on the position and direction of the implantation needles, which can decrease position and direction error and thereby enhance implantation accuracy (Fig. 1A, 1E and 1F). Thirdly, adjusting the direction of the needles during implantation can usually be undertaken without damage to bones, major vessels and organs at risk (Fig. 1B and Fig. 3). On the other hand, when using conventional templates, a change in needle direction is associated with a change in the template direction and frequently changing the template may lead to increased operation time, as well as errors in position and/or direction. Using the individual technique, one can collect information from several conventional templates in one individual template (Fig. 1D and 1E), which enhances efficiency and accuracy. In our series, one individual template contained the information of between two and six conventional templates (mean, 3). Finally, the size of the conventional template cannot be changed with the target area, unlike the individual template products, which can thus guarantee that the target area can be covered by one template. And the diameter of needle pathway in the digital modal individual template can be adjusted to fit needles with different diameters.
Fig. 3.
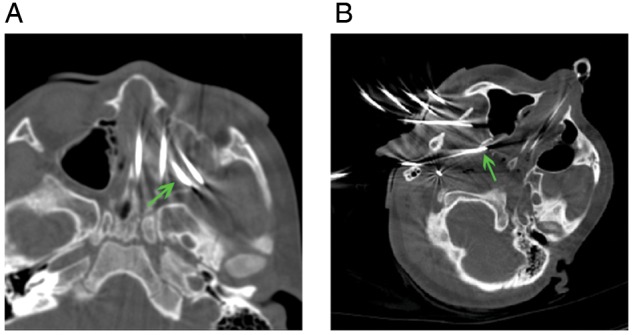
(A) The needles (green arrow) were implanted in different directions to avoid the damage to the left eyeball; (B) the needle (green arrow) was implanted in different directions to avoid the bones (mandible, mastoid process and pterygoid process of sphenoid bone).
This digital model of an individual template is suitable for radioactive seed interstitial implantation in the head and neck region and can enhance implantation accuracy, as well as simplifying the procedure. The use of individual templates and CT guidance for radioactive seed implantation in this area is feasible, and permits the delivery of highly localized brachytherapy.
ACKNOWLEDGMENTS
This study was partially supported by the new technique and new treatment modality fund of Peking University School and Hospital of Stomatology (2010). The authors would like to thank Hua-Qiu Guo and Ming-Hui Mao (Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology) for their valuable discussions.
REFERENCES
- 1.Mazeron JJ, Noel G, Simon JM. Head and neck brachytherapy. Semin Radiat Oncol. 2002;12:95–108. doi: 10.1053/srao.2002.28668. [DOI] [PubMed] [Google Scholar]
- 2.Sylvester J, Blasko J, Grimm P, et al. Interstitial implantation techniques in prostate cancer. J Surg Oncol. 1997;66:65–75. doi: 10.1002/(sici)1096-9098(199709)66:1<65::aid-jso13>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 3.Keller B, Sankreacha R, Rakovitch E, et al. A permanent breast seed implant as partial breast radiation therapy for early-stage patients: a comparison of palladium-103 and iodine-125 isotopes based on radiation safety considerations. Int J Radiat Oncol Biol Phys. 2005;62:358–65. doi: 10.1016/j.ijrobp.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Pignol JP, Rakovitch E, Keller BM, et al. Tolerance and acceptance results of a palladium-103 permanent breast seed implant phase I/II study. Int J Radiat Oncol Biol Phys. 2009;73:1482–8. doi: 10.1016/j.ijrobp.2008.06.1945. [DOI] [PubMed] [Google Scholar]
- 5.Zhang J, Zhang JG, Song TL, et al. 125I seed implant brachytherapy-assisted surgery with preservation of facial nerve for treatment of malignant parotid gland tumors. Int J Oral Maxillofac Surg. 2008;37:515–20. doi: 10.1016/j.ijom.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Jiang YL, Meng N, Wang JJ, et al. CT-guided iodine-125 seed permanent implantation for recurrent head and neck cancers. Radiat Oncol. 2010;5:68. doi: 10.1186/1748-717X-5-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ashamalla H, Rafla S, Zaki B, et al. Radioactive gold grain implants in recurrent and locally advanced head-and-neck cancers. Brachytherapy. 2002;1:161–6. doi: 10.1016/s1538-4721(02)00054-5. [DOI] [PubMed] [Google Scholar]
- 8.Glaser MG, Leslie MD, Coles I, et al. Iodine seeds in the treatment of slowly proliferating tumors in the head and neck region. Clin Oncol. 1995;7:106–9. doi: 10.1016/s0936-6555(05)80811-8. [DOI] [PubMed] [Google Scholar]
- 9.Stannard CE, Hering E, Hough J, et al. Post-operative treatment of malignant salivary gland tumors of the palate with iodine-125 brachytherapy. Radiother Oncol. 2004;73:307–11. doi: 10.1016/j.radonc.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Emami B, Marks JE. Re-irradiation of recurrent carcinoma of the head and neck by afterloading interstitial 192Ir implant. Laryngoscope. 1983;93:1345–7. doi: 10.1002/lary.1983.93.10.1345. [DOI] [PubMed] [Google Scholar]
- 11.Holm HH, Torp-Pederson S, Rasmussen F, et al. Ultrasound guided implantation of radioactive seeds. Prog Clin Biol Res. 1987;237:143–52. [PubMed] [Google Scholar]
- 12.Nguyen PL, Chen MH, D'Amico Av, et al. Magnetic resonance image-guided salvage brachytherapy after radiation in select men who initially presented with favorable-risk prostate cancer: a prospective phase 2 study. Cancer. 2007;110:1485–92. doi: 10.1002/cncr.22934. [DOI] [PubMed] [Google Scholar]
- 13.Blasko JC, Ragde H, Schumacher D. Transperineal percutaneous iodine-125 implantation from prostatic carcinoma using transrectal ultrasound and template guidance. Endocurietherapy Hyperthermia Oncol. 1987;3:131–9. [Google Scholar]
- 14.Nath R, Bice WS, Jr, Butler WM, et al. AAPM recommendations on dose prescription and reporting methods for permanent interstitial brachytherapy for prostate cancer: report of Task Group 137. Med Phys. 2009;36:5310–22. doi: 10.1118/1.3246613. [DOI] [PMC free article] [PubMed] [Google Scholar]