Abstract
OBJECTIVE:
To examine the rates and predictors of mental health services use for a nationally representative cohort of youths who had been investigated for alleged maltreatment.
METHODS:
Data came from caregiver and caseworker baseline and 18-month interviews in the second National Survey of Child and Adolescent Well-being. These interviews took place from March 2008 to September 2008 and September 2010 to March 2011. Data on family and child characteristics and service use were gathered and examined by using weighted univariate and multivariate analyses.
RESULTS:
Children had numerous challenges: 61.8% had a previous report of maltreatment, 46.3% had poor socialization skills, and 23.9% had a mental health problem measured by the Child Behavior Checklist (CBCL). At baseline, 33.3% received some mental health service and this varied by age, with younger children receiving fewer services. This percentage decreased to 30.9% at the 18-month follow-up, although the youngest children had increases in services use. For younger children, race/ethnicity, out-of-home placement, chronic physical health problems, low adaptive behaviors, and CBCL scores in the clinical range were related to use. For children ≥11, out-of-home placement, high CBCL scores, and family risk factors predicted services use at 18 months.
CONCLUSIONS:
Mental health services utilization increases as young children come into contact with schools and medical providers or have more intensive involvement with child welfare. Minority children receive fewer services adjusting for need. Over the 18-month follow-up, there was a decrease in service use that may be a result of the tremendous financial challenges taking place in the United States.
KEY WORDS: child mental health problems, child welfare, mental health services use
What’s Known on This Subject:
Children investigated for alleged maltreatment have considerable physical, mental health (MH), developmental, and educational needs and often do not receive services to address these needs. The prevalence/correlates of MH services use in the current challenging financial environment is unknown.
What This Study Adds:
This study demonstrates the importance of medical providers and schools for receipt of MH services for these children, but shows disparities in MH service use between white and nonwhite children. Unlike earlier findings, MH service use declined over the follow-up.
Since the 1970s, providers and researchers have documented high levels of unmet health needs among the 6 million children referred to child welfare agencies annually.1–17 Mental health (MH) problems are identified in 23% to 80% of children, chronic health problems in 35% to 80%, growth abnormalities in up to 43%, and educational challenges in 31% to 67%.2,3,9,11–13,15 Although these problems have long been recognized, the documentation of their MH service use and its predictors is relatively recent.18
Early information about service use came from multiple sources.18 Medicaid analyses showed that children in foster care had higher MH services use compared with other Medicaid-supported children and that usage was related to sociodemographic characteristics and physical health status.19–24 Single-site studies demonstrated that age, race/ethnicity, and need were usually positively associated with use.25–27 San Diego–based studies found that abuse type, race/ethnicity, age, and need were related to services use.28–31 These studies documented that need and non-need factors are related to use.
The National Survey of Child and Adolescent Well-being (NSCAW I) allowed the first examination of need for and use of MH services in a nationally representative sample of children investigated by child welfare agencies. Analyses showed high MH need at entrance into child welfare (47.9%) but less service use (24.4%).32 Longitudinal analyses established that age, race/ethnicity, placement type, and consistency of service use are all positively related to continued service use. Being reported to child welfare greatly increased the likelihood of receiving some type of MH services, although these services may be suboptimal.18,26,33–37
Much has changed since NSCAW I began in 1999. Professional groups concerned with the needs of vulnerable children and multidisciplinary groups of experts have continued to advocate quality standards for screening, assessment, and treatment.38 The Council on Accreditation and the Child and Family Services Reviews have mandated attention to child well-being, including assessments and services.39–41 Advocacy groups have brought class action lawsuits against child welfare systems in more than 32 states with settlements requiring that states implement actions in 30. Approximately 70% of the settlements require provision of services, including MH services.42 These pushes for additional services occurred during a period of deep economic recession. Unemployment more than doubled nationally from a low of 4.6% in 2007 to 9% in 2011, diminishing states’ tax revenues.43 States cut budgets by an average of 4% in 2009 and almost 7% in 2010.44 Since 2008, more than 45 states have reduced services including health care programs like Medicaid (31 states) and services to the disabled (29 states).45
It is unclear what the current MH services use is for children investigated by child welfare agencies, how use is related to MH needs, and whether factors previously related to use remain important. The analyses reported in this article address these issues and compare predictors of MH services use and rates of use at 18 months post baseline between NSCAW I and the second National Survey of Child and Adolescent Well-being (NSCAW II).
Methods
Design and Analytic Sample
Data came from NSCAW II, a longitudinal study of 5872 youth ages 0 to 17.5 years referred to US child welfare agencies for whom an investigation of maltreatment was completed between February 2008 and April 2009. Excluded from the study were agencies in states that required first contact of caregivers by agency staff rather than study staff.46 Initial interviews were collected within ∼4 months of completed investigations. NSCAW II, like its predecessor NSCAW I, used a national probability sampling strategy to select primary sampling units (PSUs), typically counties, from which the sample was drawn. NSCAW II used NSCAW I PSUs whenever possible. Of the 92 PSUs in NSCAW I, 71 agreed to participate in NSCAW II, and 10 additional PSUs were added to replace those not participating.
Data come from the baseline interviews completed March 2008 to September 2009 and the 18-month follow-up interviews completed September 2010 to March 2011. Analyses used data from interviews with caregivers and child welfare workers about children ≥18 months of age (n = 3084). Services use data were also gathered at the 18-month follow-up from children ≥11 years of age. NSCAW II was approved by the Research Triangle Institute’s institutional review board; present analyses of the NSCAW II de-identified data were approved by the Rady Children’s Hospital San Diego institutional review board.
Survey Design and Assessment Procedures
Analysis Weights
Analysis weights were constructed in stages corresponding to the stage of the sample design, accounting for the probability of county selection and of each child’s selection within a county. Weights were further adjusted for more or fewer population members than expected in the sampling frame, small deviations from the original plan that occurred during sampling, nonresponse patterns, and replacement PSUs. All analyses use weighting, and weighted estimates (ie, means, percentages) represent the US child welfare population.
Measures
Sociodemographics included child’s age, sex, race/ethnicity, insurance status, and placement-related information.
The Vineland Adaptive Behavior Scale Screener measures personal and social skills with 4 age-specific versions consisting of 15 items in each domain. NSCAW II includes daily living skills and socialization domains.47
Chronic conditions is a dichotomous measure indicating whether caregivers endorsed any of 9 chronic physical health problems (ie, AIDS, asthma, autism, Down syndrome, developmental delay, diabetes, cystic fibrosis, cerebral palsy, and muscular dystrophy).
Family Risk Score is constructed from caseworkers’ interviews at baseline. A cumulative risk score was based on the sum of 14 risk assessment items (scored 1 if present, 0 otherwise) that were part of the NSCAW I risk assessment.
Child Behavior Checklist (CBCL) version 1.5-5 was administered to caregivers of young children and the CBCL 6-18 was administered to caregivers of older children. The CBCL was “designed to provide standardized descriptions of behaviors rather than diagnostic inferences.” A score of ≥64 is considered clinically significant.48,49
Outcome Variable: Use of MH Services
Current caregivers detailed children’s MH services by using an adapted version of the Child and Adolescent Services Assessment,50 focusing on 3 classes of services: Specialty MH services (outpatient and inpatient), school-based services, and medical MH services.18
Children were characterized with regard to whether they had received any MH service at the time of investigation and between the baseline and 18-month interviews. At baseline, caregivers who lived with the child since birth were asked about services received “ever” and “in the last 12 months,” whereas those who lived with the child for 12 months were asked about services in the last 12 months. Caregivers who lived with a child for <12 months or those of infants <12 months of age were asked about services “since start of living arrangements” or “since birth.” The services data were augmented with reports of MH services from caseworker interviews and, at the 18-month follow-up, from interviews with children ≥11 years old. Changes in the structure of questions about services occurred in response to concerns that NSCAW I caregivers were asked to report on services use for periods when they had not been living with the child. Given differences in the services questions between NSCAW I and NSCAW II, rates of services use at baseline are not directly comparable.
Analyses
Descriptive statistics summarize key variables. Models predicting MH service use employ logistic regression and were tested in stages. Except where noted, significant bivariate predictors (P < .05) were included in multivariate models. Model stages included variables related to the child and the type of maltreatment, and then the family risk score. All analyses were conducted by using SAS-Callable SUDAAN version 10.0.1 (SAS Institute Inc, Cary, NC).
Results
One-third of the sample was 2 to 5 years old (33.7%), half was female (50.2%), just over 50% was either black (21.8%) or Hispanic (29.3%), and 72.7% was insured by Medicaid (Table 1). Most children were in their biological homes with (22.5%) or without child welfare services (64%). Only 13.5% lived in an out-of-home placement. Many lived in families experiencing considerable psychosocial risk (33.2%, 2–3 risks; 28.4%, 4 or more risks). Children were most often placed out-of-home for supervisory neglect (25%) or other types of maltreatment (35.5%), and 61.8% of these children had a previous maltreatment report. More than 20% had one of the chronic physical conditions; 36.2% scored in the moderate to severe problem range on the Vineland Daily Living Skills and 46.3% in this range for the Vineland Socialization Scale. Prevalence of elevated CBCL scores varied by age: 13.5% of 1.5- to 2-year-olds, 15.3% of >2- to 5-year-olds, 26.7% of 6- to 10-year-olds, 32.9% of 11- to 15-year-olds, and 25.5% of those ≥16 years. Overall, 23.9% of children had a CBCL score indicating a need for MH services.
TABLE 1.
Characteristics at Study Entry of the 3084 of children ≥1.5 y of Age Investigated by Child Welfare Agencies for Alleged Maltreatment
| Characteristic | %(SE) |
|---|---|
| Age | |
| 1.5–2 | 3.1(0.5) |
| >2–5 | 33.7(1.4) |
| 6–10 | 30.7(1.2) |
| 11–15 | 25.8(1.4) |
| ≥16 | 6.6(0.9) |
| Gender: Male | 49.8(1.5) |
| Race/Ethnicity | |
| Black | 21.8(2.6) |
| White | 42.1(4.0) |
| Hispanic | 29.3(3.8) |
| Other | 6.8(1.1) |
| Insurance type | |
| Federal | 72.7(1.7) |
| State | 4.6(0.9) |
| Private/Other | 12.7(1.3) |
| No insurance | 10.0(1.0) |
| Current placement | |
| Home, no child welfare services | 64.0(3.1) |
| Home, with child welfare services | 22.5(2.9) |
| Nonrelative foster care | 3.2(0.4) |
| Relative foster care | 9.5(1.0) |
| Group home/Residential treatment | 0.6(0.2) |
| Other | 0.2(0.1) |
| Family Risk Score | |
| 0–1 | 38.4(2.5) |
| 2–3 | 33.2(1.7) |
| 4+ | 28.4(1.8) |
| Primary maltreatment type at baseline | |
| Physical abuse | 22.6(1.4) |
| Sexual abuse | 8.1(1.1) |
| Physical neglect/Failure to provide | 8.8(1.1) |
| Supervisory neglect | 25.0(1.6) |
| Other | 35.5(2.1) |
| Any prior reports of maltreatment: Yes | 61.8(2.1) |
| Chronic condition | 22.7(1.4) |
| Vineland daily living skills: severe/moderate | 36.2(1.6) |
| 46.3(1.7) | |
| CBCL (Total ≥64) | 23.9(1.3) |
| 1.5–2 | 13.5(5.5) |
| >2–5 | 15.3(2.0) |
| 6–10 | 26.7(2.3) |
| 11–15 | 32.9(3.5) |
| ≥16 | 25.5(4.5) |
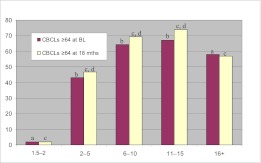
At baseline, services use increased with age from 1.9% of 1.5- to 2-year-olds to 45.9% of those ≥16 years (Table 2). The increase in use for children ≥6 years was largely driven by school-based services. At the 18-month interview, use increased for the youngest children in the study population (1–5 years), but decreased for those children ≥6 years largely owing to decreases in school-based services. A lower percentage of children 1.5 to 2 years with elevated CBCL scores received services at 18 months, compared with older children, although within age groups there were no statistically significant differences between services receipt at baseline and 18 months for children with elevated CBCL scores (Fig 1).
TABLE 2.
Proportion of Children Receiving Any MH Service at Baseline and 18 mo by Age
| Totmh_w1 | Totmh_w2 | |
|---|---|---|
| Baseline | 18 mo | |
| %(SE) | %(SE) | |
| Total | 33.3(1.6) | 30.9(1.5) |
| SPMH | 24.7(1.6 | 23.6(1.4) |
| Inpatient | 4.7(0.7) | 3.4(0.5) |
| School | 17.9(1.4) | 14.3(1.1) |
| Medical | 11.4(1.3) | 9.2(0.9) |
| 1.5–2 y | 1.9(0.8) | 3.2(1.4) |
| SPMH | 1.3(0.7) | 2.9(1.3) |
| Inpatient | 0.0(0.0) | 0.0(0.0) |
| School | 0.1(0.1) | 0.1(0.1) |
| Medical | 0.5(0.3) | 0.4(0.3) |
| >2–5 y | 12.5(2.0) | 20.6(2.6) |
| SPMH | 10.1(1.9) | 15.2(2.1) |
| Inpatient | 0.4(0.3) | 0.0(0.0) |
| School | 4.0(0.9) | 7.7(1.4) |
| Medical | 5.4(1.9) | 5.2(1.3) |
| 6–10 y | 43.4(2.7) | 36.7(2.9) |
| SPMH | 31.3(2.8) | 28.1(2.8) |
| Inpatient | 5.2(1.1) | 3.8(1.4) |
| School | 22.4(2.7) | 18.6(2.0) |
| Medical | 17.9(2.7) | 13.8(2.4) |
| 11–15 y | 49.5(3.3) | 39.6(3.7) |
| SPMH | 37.1(3.1) | 31.7(3.3) |
| Inpatient | 9.5(1.9) | 6.9(1.4) |
| School | 31.6(3.1) | 20.5(2.6) |
| Medical | 13.0(1.8) | 9.1(1.6) |
| ≥16 y | 45.9(6.4) | 34.4(5.3) |
| SPMH | 31.8(5.1) | 23.0(3.5) |
| Inpatient | 7.8(2.8) | 6.2(2.2) |
| School | 25.3(4.5) | 10.3(2.9) |
| Medical | 10.7(4.2) | 13.5(5.2) |
SPMH, Specialty Mental Health Service; Totmh_1, Any Mental Health Service at Baseline; Totmh_2, Any Mental Health Service at 18 months.
FIGURE 1.
Mental Health Service use for children with CBCL scores ≥64 at study entry and at 18 months by age group. a: CBCL ≥64 receiving services at baseline for children 1.5 to 2 years is statistically significantly different compared with those 16 years and older (P ≤ .05); b, CBCL ≥64 receiving services at baseline for children >2 to 5 years is statistically significantly different compared with those 6 to 10 and 11 to 15 years (P ≤ .05); c, CBCL ≥64 receiving services at 18 months for children 1.5 to 2 years is statistically significantly different compared with all other ages (P ≤ .05); d, CBCL ≥64 receiving services at 18 months for children >2 to 5 years is statistically significantly different compared with children ages 6 to 10 and 11 to 15 (P ≤ .05).
Characteristics related to any MH services use at 18 months by age are shown in Table 3. For the youngest children, no variable was related to use. Among >2- to 5-year-olds, use was related to race/ethnicity, placement, previous reports of maltreatment, chronic physical conditions, delays on the Vineland Daily Living Skills, and elevated CBCL scores. Children with CBCL scores in the clinical range were more than twice as likely to receive an MH service (43.2% vs 16.5%, P < .01). For 6- to 10-year-olds, MH service correlates included gender, race/ethnicity, placement, maltreatment type, chronic physical conditions, delays on either Vineland domain, and elevated CBCL scores. Children with CBCL scores in the clinical range were more than twice as likely to receive an MH service (64.2% vs 26.8%, P < .001). Among 11- to 15-year-olds, MH services use was related to 4 factors: current placement, higher family risk, delays on Vineland Socialization domain, and an elevated CBCL score. Nonrelative out-of-home placement virtually ensured the receipt of MH services. For the oldest children, placement, a family with multiple psychosocial risks, and an elevated CBCL score all were related to MH service use.
TABLE 3.
Percentage of Children Using any MH Service at 18 mo as a Function of Child/Family Characteristics
| 1.5–2 y % | >2–5 y % | 6–10 y % | 11–15 y | 16+ y | |
|---|---|---|---|---|---|
| Total | 3.2 | 20.6 | 36.7 | 39.6 | 34.4 |
| Gender | ** | ||||
| Male | 3.2 | 24.3 | 44.0 | 40.1 | 32.6 |
| Female | 3.2 | 16.4 | 27.2 | 39.4 | 35.7 |
| Race/Ethnicity | * | ** | |||
| Black | 3.8 | 12.5 | 32.2 | 43.2 | 39.4 |
| White | 5.4 | 30.0 | 50.2 | 43.1 | 32.9 |
| Hispanic | 0.6 | 15.9 | 21.6 | 32.1 | 23.4 |
| Other | 0.0 | 14.4 | 25.9 | 41.5 | 66.3 |
| Insurance type | |||||
| Federal | 3.7 | 19.5 | 40.7 | 44.2 | 29.3 |
| State | 0.0 | 17.9 | 24.4 | 17.8 | 35.5 |
| Private/Other | 0.0 | 36.7 | 33.2 | 31.0 | 50.4 |
| No insurance | 0.0 | 16.5 | 23.2 | 30.9 | 44.5 |
| Current placement | *** | *** | ** | * | |
| Home, no child welfare services | 2.4 | 19.3 | 33.3 | 33.6 | 24.6 |
| Home, with child welfare services | 0.8 | 17.7 | 36.6 | 42.8 | 35.4 |
| Nonrelative foster care | 21.1 | 45.7 | 78.9 | 93.3 | 64.2 |
| Relative foster care | 6.6 | 31.0 | 48.1 | 47.1 | 43.6 |
| Group home/Residential treatment | 60.6 | 100 | 94.5 | 88.7 | |
| Other Out of Home Placement | 0.0 | 0.0 | 5.0 | 91.1 | 51.3 |
| Primary maltreatment | * | ||||
| Physical abuse | 0.9 | 22.1 | 49.6 | 42.6 | 47.3 |
| Sexual abuse | 0.0 | 18.3 | 56.1 | 35.1 | 57.7 |
| Physical neglect/Failure to provide | 12.2 | 13.6 | 23.2 | 31.9 | 85.8 |
| Supervision neglect | 2.2 | 24.9 | 33.3 | 37.7 | 19.3 |
| Other | 4.1 | 17.8 | 30.7 | 43.4 | 26.5 |
| Any prior reports of maltreatment | * | ||||
| Yes | 5.4 | 24.8 | 38.3 | 44.6 | 37.4 |
| No | 1.8 | 15.7 | 35.1 | 33.7 | 23.8 |
| Family risk score | *** | * | |||
| 0–1 | 0.7 | 12.6 | 32.2 | 27.1 | 19.1 |
| 2–3 | 9.6 | 24.3 | 39.0 | 40.6 | 25.9 |
| 4+ | 3.6 | 26.3 | 44.3 | 57.6 | 52.0 |
| Chronic condition | ** | ** | |||
| Yes | 4.1 | 38.9 | 53.6 | 44.9 | 31.6 |
| No | 3.1 | 17.0 | 31.1 | 37.4 | 36.4 |
| Vineland Daily Living Skills | ** | ** | |||
| Severe/Moderate | 4.5 | 27.9 | 59.0 | 46.7 | 28.8 |
| Normal | 1.9 | 14.7 | 29.3 | 35.9 | 40.2 |
| Vineland Socialization | *** | ** | |||
| Severe/Moderate | 2.3 | 24.2 | 50.3 | 46.7 | 31.9 |
| Normal | 3.4 | 19.4 | 24.7 | 24.0 | 47.7 |
| CBCL baseline | ** | *** | *** | * | |
| Total ≥64 | 2.0 | 43.2 | 64.2 | 67.1 | 58.1 |
| Total <64 | 3.5 | 16.5 | 26.8 | 25.3 | 26.9 |
P < .05; ** P < .01; *** P < .001.
Multivariable logistic regression results showed that no characteristic was associated with use in 1.5- to 2-year-olds. For children >2 to 5 years, 4 baseline factors were related to use at 18 months (Table 4): black and Hispanic children were less likely to receive services (odds ratio [OR] = 0.31; 95% confidence interval [CI] 0.14, 0.66 and OR = 0.32; 95% CI 0.12, 0.89 respectively); those placed out-of-home at baseline were more likely (OR = 1.84; 95% CI 1.07, 3.16) to receive services compared with those in home with or without child welfare services; those with chronic physical conditions were more likely to receive services (OR = 2.52; 95% CI 1.31, 4.83) and those with elevated CBCL scores were more likely to receive services (OR = 2.97; 95% CI 1.49, 5.91). Children 6 to 10 years were more likely to receive services if they were white, placed out-of-home at baseline, were originally investigated for physical or sexual abuse rather than neglect or another form of maltreatment (OR = 0.43; 95% CI 0.23,0.82 and OR = 0.43; 95% CI 0.21, 0.90 respectively), had a chronic physical condition, or an elevated CBCL score. For those 11 to 15 years, 4 characteristics were related to service use: being placed out-of-home (OR = 2.75, 95% CI 1.11, 6.83), a moderate/severe Vineland Socialization score, an elevated CBCL score (OR = 4.69; 95% CI 2.75, 7.98), and a high family risk score (risk score ≥4: OR = 2.41; 95% CI 1.31, 4.43). For children ≥16 years, placement out-of-home (OR = 3.83; 95% CI 1.10, 13.31) and high family risk were related to receipt of MH services.
TABLE 4.
Multivariable Logistic Regression Models Predicting MH Services Use at the 18-mo Follow-up by Age Category
| Characteristic | 2–5 y (n = 862) | 6–10 y (n = 774) | 11–15 y (n = 585) | ≥16 y (n = 148) | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Child: | ||||||||
| Gender | ||||||||
| Male | — | — | 1.59 | 0.94, 2.70 | — | — | — | — |
| Female | — | — | 1.00 | 1.00, 1.00 | — | — | — | — |
| Race/Ethnicity | ||||||||
| Black | 0.31 | 0.14, 0.66*** | 0.41 | 0.19, 0.87* | — | — | — | — |
| White | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | — | — | — | — |
| Hispanic | 0.32 | 0.12, 0.89* | 0.22 | 0.10, 0.46*** | — | — | — | — |
| Other | 0.42 | 0.15, 1.18 | 0.27 | 0.08, 0.89* | — | — | — | — |
| Placement at entry | ||||||||
| In home, no child welfare services | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 |
| In home, no child welfare services | 0.97 | 0.56, 1.69 | 1.56 | 0.83, 2.92 | 1.30 | 0.65, 2.62 | 0.79 | 0.22, 2.92 |
| Out of home | 1.84 | 1.07, 3.16* | 3.05 | 1.44, 6.46** | 2.75 | 1.11, 6.83* | 3.83 | 1.10, 13.31* |
| Type of maltreatment | ||||||||
| Physical/sexual abuse | — | — | 1.00 | 1.00, 1.00 | — | — | — | — |
| Neglect | — | — | 0.43 | 0.23, 0.82* | — | — | — | — |
| Other | — | — | 0.43 | 0.21, 0.90* | — | — | — | — |
| Previous reports of maltreatment | ||||||||
| Yes | 1.93 | 1.06, 3.51* | — | — | — | — | — | — |
| No | 1.00 | 1.00, 1.00 | — | — | — | — | — | — |
| Chronic health problem | ||||||||
| Yes | 2.52 | 1.31, 4.83** | 1.93 | 1.02, 3.66* | — | — | — | — |
| No | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | — | — | — | — |
| Vineland Daily Living Skills | ||||||||
| Severe/Moderate | 1.88 | 0.90, 3.92 | 1.62 | 0.70, 3.71 | — | — | — | — |
| Normal | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | — | — | — | — |
| Vineland socialization | ||||||||
| Severe/Moderate | — | — | 1.52 | 0.82, 2.84 | 2.14 | 1.13, 4.04* | — | — |
| Normal | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | — | — | ||
| CBCL | ||||||||
| ≥64 | 2.97 | 1.49, 5.91** | 4.08 | 2.06, 8.08*** | 4.69 | 2.75, 7.98*** | 2.27 | 0.74, 6.94 |
| <64 | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 |
| Family Risk Score | ||||||||
| 0–1 | — | — | — | — | 1.00 | 1.00, 1.00 | 1.00 | 1.00, 1.00 |
| 2–3 | — | — | — | — | 1.38 | 0.80, 2.37 | 1.45 | 0.30, 7.01 |
| ≥4 | — | — | — | — | 2.41 | 1.31, 4.43** | 6.06 | 1.17, 31.30* |
P < .05; ** P < .01; *** P < .001. —, not a significant variable in the age specific model.
Discussion
The children investigated for maltreatment in the NSCAW II sample, like those in NSCAW I, face considerable challenges. Most children have had a previous report of maltreatment, and most families face multiple social stressors. Children largely remain in their homes, usually with no follow-up services. More than 20% of children in this sample have ≥1 chronic physical health condition, 36% face moderate/severe developmental challenges, and 24% may need MH services based on CBCL scores. Generally, these levels of need are similar to NSCAW I, although the lower level of MH service need as measured by the CBCL is a surprising difference from NSCAW I, the reasons for which are not entirely clear.18
As in NSCAW I, the rates of service use were largely consistent with levels of need; however, rates of service use were considerably lower than need among the youngest children51 and increased substantially between baseline and 18 months for children ages 2 to 5 years old. We suspect that involvement in other service sectors (eg, school, primary care) contributes to the substantial increases in service use rates among these children as their needs come to the attention of other care providers.18 Support for the role of alternate care providers in recognizing need is provided by the relationship of chronic physical conditions and service use among young children. The increased likelihood of contact with medical care providers because of a chronic physical condition may increase the identification of and referral for emotional and behavioral concerns. Similar identification and referral may happen as children enter school.18
For children ≥6 years, overall rates of MH services use decreased between baseline and 18 months, although more children with elevated CBCL scores at 18 months received services compared with those at study entry, suggesting better targeting of services to children with MH needs. This decrease in service use at 18 months contrasts with the NSCAW I data, where services use increased largely owing to increases in school services.18 In NSCAW I, any MH service use at 18 months by age category was as follows: 2- to 5-year-olds 28.9%, 6- to 10-year-olds 49.5%, 11+ 64.1%. It is unknown whether decreased service use at 18 months in NSCAW II is a result of changes in the services questions, differences in the services questions time frames, or the known decrease in social and medical services by states since the 2008 recession. When we examined NSCAW I school services without the 2 questions unavailable in NSCAW II, the percentage of children receiving an MH service dropped 7%, putting it closer to the rate in NSCAW II. If it is changes in the time frames for the services questions, the NSCAW I increase in service use may be a result of overreporting by caregivers who were asked to report on time periods when they were not living with the child and had no knowledge of service use. Conversely, the NSCAW II time frame changes may produce gaps in reporting periods, and social service records are often not detailed enough for caseworkers to fill in those gaps. It is also possible that the decrease in service use is real and is related to states’ curtailment of services because of budget challenges. Certainly there are data to suggest that schools underserve children with severe MH issues.52,53 Unfortunately, evaluating these possible explanations is not currently possible with NSCAW data but should be a future research focus.
Children placed out-of-home had a higher probability of use of MH services than those remaining at home. These results are consistent with analyses of NSCAW I, which established that child welfare contact acts as a gateway to MH services for children placed out-of-home, but not as strongly for the many children who remain in their homes subsequent to a maltreatment investigation.
The high rates of socialization difficulties among children in NSCAW II suggest that children from families at risk for child welfare involvement often experience emotional/behavioral and relational difficulties. Among adolescents, use of MH services is also driven by multiple family risk factors. These associations might be a result of adolescents more actively seeking to address issues that affect their own MH in complex family environments, or a result of increased help-seeking among families with more risks. Whatever the reasons, NSCAW II clearly shows an increase in the connection between MH service use and the complexity of family issues as children age.
One important non–need-related finding, also observed in NSCAW I, is the lower rate of service use among nonwhite children. Among 2- to 10-year-old children, rates of service use by children from other race/ethnic groups is significantly lower than among white children. Previous studies have documented low rates of MH and developmental service use among nonwhite children, especially during early childhood.18,29,30 Results suggest that minority group families with high risk for child welfare involvement are less likely to receive beneficial MH services during important early developmental stages.51 Whether the failure to ensure that children who need MH services get them is because of agencies not pursuing services rigorously for nonwhite children, because of nonwhite caregivers being more reluctant to seek or accept services, or because minority children are disproportionately found on child welfare caseloads and, thus, may have relatively fewer problems/require less service is unknown.51 However, that this finding has not changed since NSCAW I suggests that agencies have not attended to this well-documented issue.18 Work by Hurlburt and colleagues35 suggests that service systems can play a substantial role in minimizing such disparities, but results from NSCAW II indicate that much more remains to be done. Given the policy implications of this finding, it should be thoroughly investigated to inform the development of incentives to minimize disparities.
Conclusions
Results from NSCAW II highlight system-level issues related to service use. Service use for MH problems increases as young children enter school, have additional contact with medical care providers, or have more intense involvement with child welfare. Earlier work from NSCAW I identified that how service systems relate to one another is instrumental in reducing disparities in service use among minority children,35 but the finding in NSCAW II that minority children continue to receive fewer services controlling for need suggests that these service systems may not have addressed issues important for alleviating disparities. A disturbing finding is the decrease in service use at 18-month follow-up in children 6 years and older. This decrease may be a result of the tremendous financial challenges currently facing most states and warrants careful monitoring to ensure that critically needed services remain available for children at high risk.
Glossary
- CBCL
Child Behavior Checklist
- CI
confidence interval
- MH
mental health
- NSCAW I
National Survey of Child and Adolescent Well-Being I
- NSCAW II
National Survey of Child and Adolescent Well-Being II
- OR
odds ratio
- PSU
primary sampling unit
Footnotes
Dr Horwitz conceptualized the study, constructed the analysis and interpreted the data, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final manuscript as submitted; Dr Hurlburt conceptualized the study, assisted with the analysis and interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted; Dr Goldhaber-Fiebert interpreted the data, drafted portions of the initial manuscript, reviewed and revised the manuscript, and approved the final manuscript as submitted; Dr Heneghan interpreted the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted; Ms Zhang analyzed and interpreted the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted; Ms Rolls-Reutz interpreted the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted; Ms Fisher interpreted the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted; Dr. Landsverk conceptualized the study, critically revised the manuscript for important intellectual content, and approved the final manuscript as submitted; and Dr Stein interpreted the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
This document includes data from the NSCAW, developed under contract with the Administration on Children, Youth, and Families, US Department of Health and Human Services and the National Data Archive on Child Abuse and Neglect. We thank the National Institute of Mental Health for the support but acknowledge that the findings and conclusions presented are those of the authors and do not necessarily reflect the opinions of the National Institute of Mental Health, or the endorsement of its content by Administration on Children, Youth and Families, US Department of Health and Human Services.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was supported by the National Institute of Mental Health award P30-MH074678; PI: J Landsverk. Funded by the National Institutes of Health (NIH).
References
- 1.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000;106(4 suppl):909–918 [PubMed] [Google Scholar]
- 2.Chernoff R, Combs-Orme T, Risley-Curtiss C, Heisler A. Assessing the health status of children entering foster care. Pediatrics. 1994;93(4):594–601 [PubMed] [Google Scholar]
- 3.Clausen JM, Landsverk J, Ganger W, Chadwick D, Litrownik A. Mental health problems of children in foster care. J Child Fam Stud. 1998;7:283–296 [Google Scholar]
- 4.Combs-Orme T, Chernoff RG, Kager VA. Utilization of health care by foster children: application of a theoretical model. Child Youth Serv Rev. 1991;3:113–129 [Google Scholar]
- 5.Halfon N, Mendonca A, Berkowitz G. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Arch Pediatr Adolesc Med. 1995;149(4):386–392 [DOI] [PubMed] [Google Scholar]
- 6.Hochstadt NJ, Jaudes PK, Zimo DA, Schachter J. The medical and psychosocial needs of children entering foster care. Child Abuse Negl. 1987;11(1):53–62 [DOI] [PubMed] [Google Scholar]
- 7.Klee L, Halfon N. Mental health care for foster children in California. Child Abuse Negl. 1987;11(1):63–74 [DOI] [PubMed] [Google Scholar]
- 8.McIntyre A, Keesler TY. Psychological disorders among foster children. J Clin Child Psychol. 1986;15:297–303 [Google Scholar]
- 9.Pilowsky D. Psychopathology among children placed in family foster care. Psychiatr Serv. 1995;46(9):906–910 [DOI] [PubMed] [Google Scholar]
- 10.Schor EL. The foster care system and health status of foster children. Pediatrics. 1982;69(5):521–528 [PubMed] [Google Scholar]
- 11.Schor EL. Foster care. Pediatr Rev. 1989;10(7):209–216 [DOI] [PubMed] [Google Scholar]
- 12.Simms MD. The foster care clinic: a community program to identify treatment needs of children in foster care. J Dev Behav Pediatr. 1989;10(3):121–128 [PubMed] [Google Scholar]
- 13.Stein E, Evans B, Mazumdar R, Rae-Grant N. The mental health of children in foster care: a comparison with community and clinical samples. Can J Psychiatry. 1996;41(6):385–391 [DOI] [PubMed] [Google Scholar]
- 14.Swire MR, Kavaler F. The health status of foster children. Child Welfare. 1977;56(10):635–653 [PubMed] [Google Scholar]
- 15.Szilagyi M. The pediatrician and the child in foster care. Pediatr Rev. 1998;19(2):39–50 [DOI] [PubMed] [Google Scholar]
- 16.US General Accounting Office Foster Care: Health Needs of Many Young Children Are Unknown and Unmet. Washington, DC: US Government Printing Office; 1995 [Google Scholar]
- 17.Administration for Children and Families Child Maltreatment 2005. Washington, DC: Administration for Children and Families; 2007 [Google Scholar]
- 18.Horwitz SM, Hurlburt MS, Zhang J. Patterns and predictors of mental health services use by children in contact with the child welfare system. In: Webb MB, Dowd K, Harden BJ, Landsverk J, Testa M, eds. Child Welfare and Child Well-Being: New Perspectives from the National Survey of Child and Adolescent Well-Being. New York, NY: Oxford University Press; 2009:279–329 [Google Scholar]
- 19.dosReis S, Zito JM, Safer DJ, Soeken KL. Mental health services for youths in foster care and disabled youths. Am J Public Health. 2001;91(7):1094–1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halfon N, Berkowitz G, Klee L. Mental health service utilization by children in foster care in California. Pediatrics. 1992;89(6 pt 2):1238–1244 [PubMed] [Google Scholar]
- 21.Harman JS, Childs GE, Kelleher KJ. Mental health care utilization and expenditures by children in foster care. Arch Pediatr Adolesc Med. 2000;154(11):1114–1117 [DOI] [PubMed] [Google Scholar]
- 22.Rubin DM, Alessandrini EA, Feudtner C, Mandell DS, Localio AR, Hadley T. Placement stability and mental health costs for children in foster care. Pediatrics. 2004;113(5):1336–1341 [DOI] [PubMed] [Google Scholar]
- 23.Snowden LR, Cuellar AE, Libby AM. Minority youth in foster care: managed care and access to mental health treatment. Med Care. 2003;41(2):264–274 [DOI] [PubMed] [Google Scholar]
- 24.Takayama JI, Bergman AB, Connell FA. Children in foster care in the state of Washington. Health care utilization and expenditures. JAMA. 1994;271(23):1850–1855 [PubMed] [Google Scholar]
- 25.Zima BT, Bussing R, Yang X, Belin TR. Help-seeking steps and service use for children in foster care. J Behav Health Serv Res. 2000;27(3):271–285 [DOI] [PubMed] [Google Scholar]
- 26.Farmer EMZ, Mustillo SA, Wagner HR, et al. Services use and multi-sector use for mental health problems by youth in contact with child welfare. Child Youth Serv Rev. 2010;32(6):815–821 [Google Scholar]
- 27.McMillen JC, Scott LD, Zima BT, Ollie MT, Munson MR, Spitznagel E. Use of mental health services among older youths in foster care. Psychiatr Serv. 2004;55(7):811–817 [DOI] [PubMed] [Google Scholar]
- 28.Blumberg E, Landsverk J, Ellis-MacLeod E, Ganger W, Culver SC. Use of the public mental health system by children in foster care: client characteristics and service use patterns. J Ment Health Adm. 1996;23(4):389–405 [DOI] [PubMed] [Google Scholar]
- 29.Garland AF, Hough RL, Landsverk JA, et al. Racial and ethnic variations in mental health case utilization among children in foster care. Child Serv (Mahwah NJ). 2000;3:133–146 [Google Scholar]
- 30.Garland AF, Landsverk JA, Lau AS. Racial/ethnic disparities in mental health service use among children in foster care. Child Youth Serv Rev. 2003;25(5-6):491–507 [Google Scholar]
- 31.Leslie LK, Landsverk J, Ezzet-Lofstrom R, Tschann JM, Slymen DJ, Garland AF. Children in foster care: factors influencing outpatient mental health service use. Child Abuse Negl. 2000;24(4):465–476 [DOI] [PubMed] [Google Scholar]
- 32.Burns BJ, Phillips SD, Wagner HR, et al. Mental health need and access to mental health services by youths involved with child welfare: a national survey. J Am Acad Child Adolesc Psychiatry. 2004;43(8):960–970 [DOI] [PubMed] [Google Scholar]
- 33.Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang JJ. Relationship between entry into child welfare and mental health service use. Psychiatr Serv. 2005;56(8):981–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leslie LK, Hurlburt MS, Landsverk J, Rolls JA, Wood PA, Kelleher KJ. Comprehensive assessments for children entering foster care: a national perspective. Pediatrics. 2003;112(1 pt 1):134–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hurlburt MS, Leslie LK, Landsverk J, et al. Contextual predictors of mental health service use among children open to child welfare. Arch Gen Psychiatry. 2004;61(12):1217–1224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stahmer AC, Leslie LK, Hurlburt M, et al. Developmental and behavioral needs and service use for young children in child welfare. Pediatrics. 2005;116(4):891–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raghavan R, Inoue M, Ettner SL, Hamilton BH, Landsverk J. A preliminary analysis of the receipt of mental health services consistent with national standards among children in the child welfare system. Am J Public Health. 2010;100(4):742–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Romanelli LH, Hoagwood KE, Kaplan SJ, et al. Child Welfare-Mental Health Best Practices Group . Best practices for mental health in child welfare: parent support and youth empowerment guidelines. Child Welfare. 2009;88(1):189–212 [PubMed] [Google Scholar]
- 39.Council on Accreditation. Accreditation standards—public agencies. 8th ed. Available at: www.coastandards.org/standards.php?navView=public. Accessed November 10, 2011
- 40.Adoption and Safe Families Act PL 105-89. 111 S 2115, amending 42 USC §671-675, 1997
- 41.Administration for Children and Families, US Department of Health and Human Services. Procedures manual. Available at: www.acf.hhs.gov/programs/cb/cwmonitoring/tools_guide/proce_manual.htm. Accessed August 21, 2011
- 42.Kosanovich A, Joseph RM. Child welfare consent decrees: analysis of thirty-five court actions from 1995–2005. Child Welfare League of America. 2005. Available at: www.cwla.org/advocacy/consentdecrees.pdf. Accessed August 21, 2011
- 43.US Bureau of Labor Statistics. Table A-2. Employment status of the civilian noninstitutional population 16 years and over by sex, 2002 to date. Available at: www.bls.gov/web/empsit/cpseea02.pdf Accessed March 30, 2012
- 44.National Association of State Budget Officers. The fiscal survey of the states, spring 2011: a report by the National Governors Association and the National Association of State Budget Officers. Washington, DC. Available at: www.nasbo.org/sites/default/files/Spring-2011-Fiscal-Survey_0.pdf. Accessed March 30, 2012
- 45.Johnson N, Oliff P, William E. An update on state budget cuts. Washington, DC: Center on Budget and Policy Priorities. Available at: www.cbpp.org/files/3-13-08sfp.pdf. Accessed March 30, 2012
- 46.Dowd K, Donlan M, Wallin J, et al. National Survey of Child and Adolescent Well-Being II: Combined Values 1-2 Data User’s Manual Restricted Release Version. Ithaca, NY: Cornell University, National Data Archive on Child Abuse and Neglect; 2011.
- 47.Sparrow SS, Carter AS, Cicchetti D. The Vineland Screener. New Haven, CT: Yale University Child Study Center; 1993 [Google Scholar]
- 48.Achenbach TM, Rescorla AA. Manual for the ASEBA preschool forms and profiles. Available at: www.aseba.org/preschool.html. Accessed September 13, 2011
- 49.Administration for Children and Families Child Welfare Outcomes 2003: Annual Report to Congress. Washington, DC: U.S. Government Printing Office; 2005 [Google Scholar]
- 50.Ascher BH, Farmer EMR, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): description and psychometrics. J Emot Behav Disord. 1996;4:12–20 [Google Scholar]
- 51.Horwitz SM, Hurlburt MS, Heneghan A, et al. Mental health problems in young children investigated by US child welfare agencies. J Am Acad Child Adolesc Psychiatry. 2012;51(6):572–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nelson CM, Rutherford RB, Jr, Center DB, Walker HM. Do public schools have an obligation to serve troubled children and youth? Except Child. 1991;57(5):406–417 [DOI] [PubMed] [Google Scholar]
- 53.Walker HM, Nishioka VM, Zeller R, Severson HH, Feil EG. Causal factors and potential solutions for the persistent underidentification of students having emotional or behavioral disorders in the context of schooling. Assess Eff Interv. 2000;26(1):29–39 [Google Scholar]