Abstract
Objectives. We used individual participant data from multiple studies to conduct a comprehensive meta-analysis of mechanical exposures in the workplace and low back pain.
Methods. We conducted a systematic literature search and contacted an author of each study to request their individual participant data. Because outcome definitions and exposure measures were not uniform across studies, we conducted 2 substudies: (1) to identify sets of outcome definitions that could be combined in a meta-analysis and (2) to develop methods to translate mechanical exposure onto a common metric. We used generalized estimating equation regression to analyze the data.
Results. The odds ratios (ORs) for posture exposures ranged from 1.1 to 2.0. Force exposure ORs ranged from 1.4 to 2.1. The magnitudes of the ORs differed according to the definition of low back pain, and heterogeneity was associated with both study-level and individual-level characteristics.
Conclusions. We found small to moderate ORs for the association of mechanical exposures and low back pain, although the relationships were complex. The presence of individual-level OR modifiers in such an area can be best understood by conducting a meta-analysis of individual participant data.
In the past 4 decades there have been more than 30 systematic reviews of workplace biomechanical risk factors and low back pain (LBP).1–33 Although these reviews were rigorously done, controversy remains about the role of mechanical workplace exposures34 among other possible factors,35 and important gaps in our knowledge persist.36 To date, authors of comprehensive systematic reviews that include multiple definitions of LBP and mechanical exposures have not attempted to statistically combine data. This is likely attributable to the diversity of study designs, study populations, methods of exposure measurement, and assessments of LBP. Differences in the way mechanical exposure and LBP are reported make it difficult to comprehensively summarize this literature.
To overcome these problems we developed methods to categorize “like” definitions of LBP that could be combined in a homogeneous meta-analysis37 and to create combinable mechanical exposure measures.38 We also obtained individual participant data for LBP studies in workers. We used these components to conduct an individual participant data meta-analysis. Use of individual participant data allowed us to go beyond the typical meta-analysis and make full use of all data collected. For example, we were not restricted to definitions of LBP reported in the published literature; instead, we were able to explore all definitions of LBP collected within a study. Individual participant data also enabled us to consistently adjust for potential confounding factors and explore individual-level odds ratio (OR) modifiers.
METHODS
A research librarian conducted a comprehensive39 literature search in the following bibliographic databases: MEDLINE (1966 to March 2005), EMBASE (1988 to March 2005), CINAHL (1982 to March 2005), PsychINFO (1974 to March 2005), Safety Science and Risk Abstracts (1981 to March 2005), and the Institute for Work and Health (Toronto) database. The search strategy was based on one suggested by the Cochrane Back Pain group40 (see Appendix A, available as a supplement to the online version of this article at http://www.ajph.org).
Inclusion and Exclusion Criteria
Any cohort, case–control, or cross-sectional study that related workplace biomechanical risk factors to LBP and that was published in English was eligible. We included LBP definitions based on pathology, symptoms or signs of nonspecific LBP, self-reported LBP, or events such as time off work, medical consultation, or treatment and disability reported to be a consequence of LBP. Eligible exposures were physical load or trunk posture during work based on job title, self-report, direct observation, or technical assessment (e.g., electromyography). We excluded studies of LBP attributable to pathologies unrelated to mechanical exposures such as LBP because of cancer or during pregnancy. We also excluded studies focusing only on nonwork exposures or including a single work-related event that directly precipitated the back injury, studies in which groups differed only by their exposure to whole-body vibrations, studies including working children, and aviation studies examining g-force exposures.
Reviewing Process
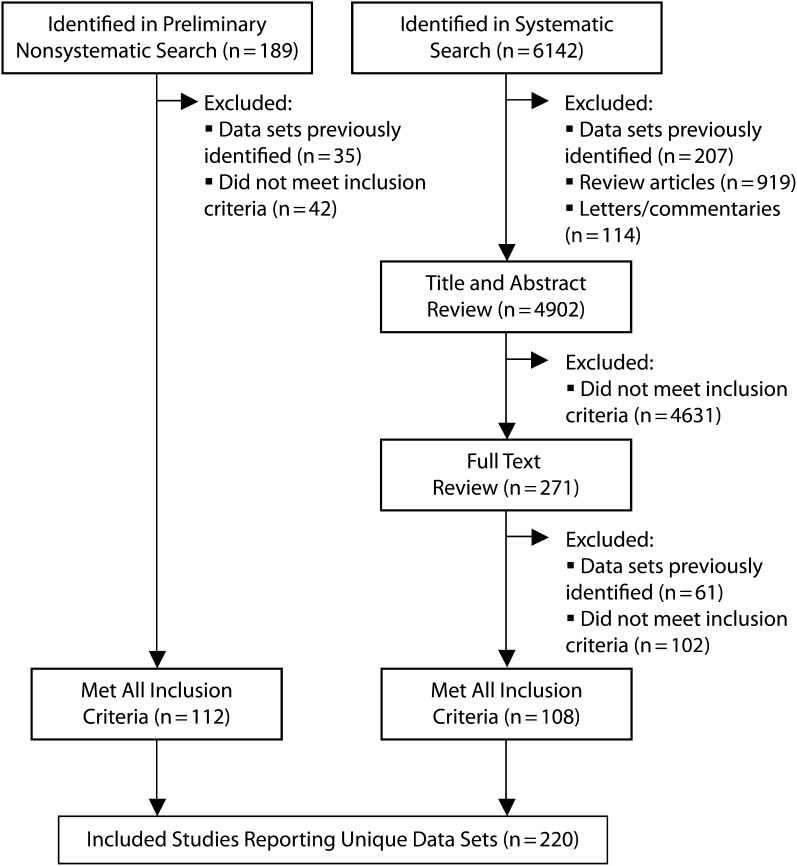
The literature search found 6142 unique articles that were eligible (Figure 1). After we excluded studies that contained data sets already identified from previous reviews (n = 207), review articles without primary data (n = 919), and letters and commentaries (n = 114), 4902 articles were left. We conducted title and abstract review of these 4902 articles to determine which studies to include and which to exclude.
FIGURE 1—
Results of reviewing process to identify studies of workplace mechanical exposures and low back pain.
Two raters (L. E. G. and H. S. S.) independently reviewed the titles and abstracts. Disagreements on inclusion and exclusion were resolved by consensus. This process continued until both raters felt that the application of inclusion and exclusion criteria was clear and that the full range of potential studies had been assessed (n = 333). Subsequently 1 rater (L. E. G.) reviewed the remaining 4569 studies twice on 2 separate occasions separated by at least 1 week. The second rater reviewed all studies not rated as definite exclusions (n = 379).
One rater (L. E. G.) reviewed all full-text articles. The other rater reviewed those categorized as either “probable” or “possible” exclusion. Any technical questions regarding exposure were addressed by a third reviewer trained in biomechanics (R. P. W.). Articles that referred to a data set already identified were excluded. In total, 220 articles reporting unique data sets were identified (Figure 1).
Contact information was available for authors of 95% (209 of 220) of the studies. Personalized e-mails were sent to each author explaining the study. If an author did not respond, at least 2 subsequent e-mail requests were sent. Ninety percent (189 of 209) of authors responded, and 51% (n = 97) indicated that their data would or might be available—26 cohort studies, 4 case–control studies, and 67 cross-sectional studies.
Because of limited resources, it was feasible to clean and process only a subset of the cross-sectional data sets. Therefore, we requested individual participant data for a random sample of 30 of the cross-sectional studies. If instruments were not in English, authors were asked to translate the key questions related to LBP, mechanical exposure, and potential confounders. This process yielded data sets from 48 primary studies (22 cohort, 4 case–control, and 22 cross-sectional).
Outcome Categorization
We had previously determined which definitions of LBP could be combined in an individual participant data meta-analysis via a Delphi consensus process.37 This resulted in 20 outcome sets grouped into 4 outcome types: pathology, symptoms, functional limitations, and participation or work indicators. There were 3 pathology outcome sets, 13 symptom sets, and 2 sets each for functional limitations and participation. We analyzed each outcome set separately.
There were 8 distinct exposure types reported: working situation (e.g., job title), qualitative descriptor (e.g., heavy work), named tasks (e.g., patient transfer), force (e.g., lifting), trunk postures (e.g., bending), gross postures (e.g,. kneeling), internal exposure (e.g., spinal load), and combinations (e.g., bending and lifting). A mapping of exposure measures suggested that trunk posture and force exposures were similar enough across studies to create algorithms to transform the exposures into common units. The algorithmic translations were developed by a biomechanist (R. P. W.) and are reported elsewhere.41
Briefly, for most studies, posture and force exposure data were collected in 1 of 3 ways. In the first way (the “time” exposure measures), studies recorded the duration of an average workday for which a worker was exposed to a specific posture or force, expressed as a percentage of an 8-hour workday. The second type of exposure measure, “task,” represented the percentage of time spent on the job that included the task entailing that posture. For example, all components of a person's job could involve trunk flexion, even if the person only spent some of the time in a flexed posture. Thus, the “task” exposure measure would be 100%, whereas the “time” exposure measure would be, say, 20%. Finally, we created a binary “any” measure on the basis of whether a person's job required any time in the particular posture or applying the force. We developed algorithmic translations for moderate trunk flexion (> 20°), large trunk flexion (> 60°), nonneutral trunk postures (trunk flexion, twisting, or other awkward postures), twisting, lifting, and heavy lifting (> 20 kg).
Data Extraction
Study-level characteristics were extracted in duplicate (L. E. G., L. E. L.), including outcome definition, type of exposure variable, and how exposure was measured. Other study-level variables extracted were population (workplace-based or population-based), whether the data were collected by the authors (primary) or by other users (secondary), and whether the primary objective of the study was to examine the relationship between mechanical exposure and LBP. We extracted unadjusted and adjusted estimates of effect and covariates included in adjusted models.
Two reviewers (L. E. G., L. E. L.) independently assessed methodologic quality–based standardized criteria developed from general42–44 and LBP-specific15 quality assessment tools. The criteria rated the study design, study population, exposure measurement, assessment of LBP, and analysis. The items varied depending on the study design. Disagreements between reviewers were resolved by consensus.
A priori, we identified 3 potential sources of heterogeneity: nonsystematic measurement error, bias, and OR modification. These could be related to several variables, both study-level and individual-level. For example, different exposure types are associated with differing degrees of measurement error.45,46 Studies using job title to infer posture exposures have greater risk of misclassification than do those using direct measures of posture. If random, misclassification would tend to attenuate an effect measure.47,48 Heterogeneity associated with the potential for bias could be related to the study design (cohort vs cross-sectional), the quality of the original studies, and differential adjustment for strong confounding variables among the studies.
Operationalization of Variables
If necessary, we transformed data from each study to create a common set of variables. We included age, body mass index (BMI, defined as weight in kilograms divided by the square of height in meters), psychological job demands, and job control as continuous variables. Job demand and control were on a linearly converted 100-point scale. All other variables were categorical. We considered smoking status in 2 ways: current smoking status (yes vs no) and ever smoked (yes vs no). We dichotomized alcohol use (yes vs no). We categorized marital status as married, single, or divorced, separated, or widowed. We dichotomized number of children into having any children (yes vs no). We categorized education as less than high-school education, high-school education, and more than high-school education. We dichotomized leisure activities into “low” (few or no leisure activities) and “high” (regular participation in leisure activities). Driving (yes vs no) included occupational or nonoccupational driving. If job satisfaction was measured with a scale, we considered “satisfied” and “very satisfied” to be “high”; we considered all other categories to be “low.”
All study-level variables in the OR modification analysis were categorical. Because no case–control study had the outcome–exposure combinations included in the analysis study design was either cross-sectional or cohort. We considered the cohort studies in 2 ways: first, we counted all LBP events regardless of baseline LBP status; second, we counted only incident LBP events. We used the time point closest to 1-year follow-up for all cohort studies, as 1 year was the most commonly used follow-up period. We considered 4 quality items individually (participation rate > 80%, reliability of exposure measure reported, reliability of outcome measure reported, dose–response analysis reported). The relationship between mechanical exposure and LBP with the entire set of quality items was reported by Langlois.49 Finally, “exposure method” reflected whether measurement used direct observation or self-report, and “study base” reflected whether the study was population-based or workplace-based.
Table 1 presents the number of studies with individual participant data available for each outcome and exposure combination. Twenty-seven50–76 of the 48 studies with individual participant data had exposure data amenable to exposure translation. We chose outcome–exposure combinations that maximized the number of studies included in the analyses and to reflect the different types of exposure (i.e., “time,” “task,” and “any”) and LBP definitions. We chose flexion greater than 30° and LBP in the last 6 to 24 months; nonneutral postures and current LBP, LBP over 6 to 24 months, and sick leave because of LBP; and lifting and heavy lifting and LBP over 6 to 24 months and sick leave because of LBP.
TABLE 1—
Number of Studies of Mechanical Workplace Risk Factors and Low Back Pain With Algorithmic Translation Exposure–Outcome Combinations
| Trunk Flexion |
Nonneutral Trunk |
Large Trunk Flexion |
Trunk Twisting |
Liftingb |
||||||||||||
| Outcomea | 1A | 1B | 1C | 2A | 2B | 2C | 3A | 3B | 3C | 4A | 4B | 4C | 1A | 1B | 1C | 2C |
| Abnormal back (n = 0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lumbar disc disease (n = 0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Herniated lumbar disc (n = 2) | 1 | 1 | 2 | 1 | 2 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | 2 |
| Current LBP (n = 9) | 2 | 2 | 4 | 2c | 4c | 8c | 2 | 0 | 2 | 1 | 1 | 2 | 1 | 2 | 9 | 8 |
| LBP 1–3 mo (n = 3) | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| LBP 6 mo–2 y (n = 17) | 4c | 3c | 7c | 5c | 5c | 14c | 2 | 0 | 2 | 2 | 3 | 5 | 2 | 3 | 14 | 11 |
| LBP > 2 y (n = 9) | 5 | 1 | 6 | 5 | 2 | 6 | 2 | 0 | 2 | 2 | 1 | 3 | 2 | 1 | 8 | 7 |
| Regular LBP (n = 1) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Lumbago in last 12 mo (n = 2) | 2 | 0 | 2 | 2 | 1 | 2 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 2 | 2 |
| Lumbago > 1 y (n = 3) | 2 | 1 | 3 | 2 | 2 | 3 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 3 | 3 |
| Sciatica in last 12 mo (n = 4) | 2 | 1 | 3 | 3 | 2 | 4 | 2 | 0 | 2 | 1 | 0 | 1 | 2 | 1 | 5 | 4 |
| Sciatica > 1 y (n = 1) | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 0 | 1 | 1 | 1 | 2 | 0 | 0 | 2 | 2 |
| Long lasting or frequent LBP (n = 6) | 3 | 2 | 5 | 4 | 3 | 7 | 2 | 0 | 2 | 1 | 2 | 3 | 2 | 2 | 7 | 6 |
| LBP reported (n = 2) | 1 | 0 | 1 | 1 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 |
| Seeking care for LBP (n = 4) | 3 | 2 | 5 | 3 | 3 | 5 | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 2 | 5 | 5 |
| Filing a disability claim for LBP (n = 0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mild functional limitations (n = 2) | 2 | 1 | 3 | 2 | 2 | 3 | 2 | 0 | 2 | 1 | 0 | 1 | 1 | 1 | 3 | 3 |
| Moderate to severe functional limitations (n = 0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sick leave (n = 10) | 2 | 2 | 4 | 3c | 5c | 9c | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 3 | 8c | 7c |
| Disability pension (n = 0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 8 | 3 | 12 | 9 | 6 | 19 | 2 | 0 | 2 | 3 | 3 | 6 | 5 | 4 | 26 | 14 |
Note. LBP = low back pain. “A” exposures represent the percentage of a workday spent in a nonneutral posture or exerting a force; “B” exposures represent the percentage of job tasks requiring a nonneutral posture or exerting a force; “C” exposures represent ever experiencing a nonneutral posture or exerting a force; force 1C = lifting; force 2C = heavy lifting (> 20 kg).
Two studies of patient handling in nurses contributed only to sensitivity analyses for lifting and heavy lifting and thus are not counted in the table for force exposures.
Outcome categories determined through a Delphi consensus process.37
The outcome–exposure combinations included in the individual participant data analysis.
Statistical Methods
We used regression analyses to examine the relationship between LBP and mechanical exposure. To account for the nesting of participants within studies, we used generalized estimating equation regression analysis with a logit link and an exchangeable correlation structure.77 We used the GENMOD procedure of SAS/STAT software version 9.1 (SAS Institute, Cary, NC) for all individual participant data analyses.78 We tested model fit by using an adaptation of an extension of the Hosmer-Lemeshow goodness-of-fit statistics proposed by Horton et al.79,80
Potential Strong Confounders and Effect Modifiers
For each potential confounder we ran 2 regression models. The first included only the mechanical exposure variable, and the second included mechanical exposure and the potential confounder. Both models included the same data, such that any individuals with missing data for that potential confounder were excluded from both models. If the adjusted OR changed by 20% or more from the unadjusted OR, then we considered the confounder “strong.” If the adjusted OR changed by less than 20% but at least by 10%, we considered the confounder “moderate.”
We also used generalized estimating equation regression models to determine whether individual- and study-level variables were OR modifiers. We considered a variable an OR modifier if the interaction coefficient was statistically significant at P < .05 and the subgroup-specific ORs differed by 10% or more when there were 2 subgroups, or if the largest difference between ORs was 20% or more when there were 3 subgroups.
Finally, to explore whether posture and force exposures were independently associated with LBP, we restricted the analysis to studies that collected both nonneutral posture and lifting exposures and LBP 6 to 24 months. We ran 1 model with the posture variable only, 1 with the force variable only, and 1 with both posture and force variables. We chose the exposure–outcome combinations to incorporate the most possible studies.
Aggregate Data Meta-analysis
Studies often did not report analyses using all LBP outcomes or exposures collected, so to maximize the number of outcome and exposures combinations we used individual participant data to create aggregate data. Creating aggregate data also allowed for consistent adjustment of potential confounders. We created both unadjusted and age- and sex-adjusted ORs and standard errors for each outcome–exposure combination. Odds ratios for “time” and “task” posture measures are for a difference of 20% in exposure (e.g., 1.6 hours for an 8-hour shift). Aggregate data meta-analysis can be based on either a fixed-effect model or a random-effects model. Under the fixed-effect model, one assumes that there is 1 true effect size that is being measured by all studies in the analysis. The random-effects model, in contrast, allows that the true effect could vary from study to study. Because we were particularly interested in examining components that could be associated with between- and within-study differences, we used both fixed- and random-effects models81,82 for the aggregate data meta-analyses. The Q test was the primary test for heterogeneity.83 We used the I2 statistic to examine the magnitude of heterogeneity; we considered a value greater than 50% “substantial heterogeneity.”84
Having access to individual participant data allowed further examination of relationships identified using between-study comparisons via within-study data. We used an analysis restricted to cohort studies to compare cross-sectional (baseline data) to follow-up data within each study. We also calculated ORs for follow-up data with and without prevalent LBP cases included.
RESULTS
Of the 21 individual participant data sets amenable to algorithmic translation of mechanical exposure, 18 studies50,51,53,54,56,58,61–63,65–69,73–76 representing 25 513 individuals included at least 1 outcome and exposure combination analyzed. The characteristics of the 18 studies are presented in Appendix B (available as a supplement to the online version of this article at http://www.ajph.org). Eight studies had current LBP data with 9550 observations, 17 studies with 25 051 observations had data for LBP 6 to 24 months, and 10 studies with 6157 observations had data for sick leave attributable to LBP. The sample size for studies ranged from 132 to 7204 (median = 570). All 18 studies had individual-level data for age. Most had data for sex (n = 17), BMI (n = 13), leisure activities (n = 12), and marital status (n = 10). The covariates least often available were driving (n = 4), alcohol consumption (n = 4), and job satisfaction (n = 5).
Table 2 presents the meta-analysis results with the algorithmic translation of mechanical exposure. The ORs for “time” exposures tended to be slightly higher than those for the “task” exposures. The ORs for “any” posture exposures were higher than both the “time” and “task” exposures. The ORs for sick leave attributable to LBP were mostly higher than those for current LBP or LBP 6 to 24 months. The greatest amount of heterogeneity was almost always associated with the “any” exposures. The I2 ranged from 0% to more than 80%, with 5 of the 16 having an I2 greater than 50%. (I2 is the percentage of the total variability in a set of effect sizes because of true heterogeneity)
TABLE 2—
Summary of Traditional Meta-Analyses of Studies of Mechanical Risk Factors in the Workplace and Low Back Pain for Unadjusted Odds Ratios for Each of the Selected Outcome–Exposure Combinations, Using the Algorithmic Translation of Exposure
| Outcome–Exposure Combinations | Studies, No. | Fixed Effects OR (95% CI) | Pfixed | Random Effects OR (95% CI) | Prandom | Qa | PQ | I2, %b |
| LBP in the past 6 mo to 2 y | ||||||||
| Posture 1A | 4 | 1.27 (1.16, 1.40) | <.001 | 1.27 (1.16, 1.40) | <.001 | 1.4 | .70 | 0.0 |
| Posture 1B | 3 | 1.14 (1.08, 1.21) | <.001 | 1.14 (1.08, 1.21) | <.001 | 1.7 | .43 | 0.0 |
| Posture 1C | 7 | 1.33 (1.19, 1.50) | <.001 | 1.36 (1.07, 1.73) | .01 | 16.2 | .01 | 62.9 |
| Posture 2A | 5 | 1.27 (1.16, 1.39) | <.001 | 1.27 (1.16, 1.39) | <.001 | 1.4 | .84 | 0.0 |
| Posture 2B | 5 | 1.18 (1.15, 1.21) | <.001 | 1.18 (1.15, 1.21) | <.001 | 3.8 | .43 | 0.0 |
| Posture 2C | 14 | 1.69 (1.56, 1.82) | <.001 | 1.68 (1.39, 2.04) | <.001 | 42.3 | <.001 | 69.3 |
| Force 1C | 14 | 1.61 (1.52, 1.71) | <.001 | 1.40 (1.20, 1.62) | <.001 | 58.3 | <.001 | 77.7 |
| Force 2C | 11 | 1.43 (1.32, 1.55) | <.001 | 1.42 (1.30, 1.55) | <.001 | 10.7 | .38 | 6.9 |
| Current LBP | ||||||||
| Posture 2A | 2 | 1.20 (0.96, 1.51) | .11 | 1.20 (0.96, 1.51) | .11 | 0.2 | .69 | 0.0 |
| Posture 2B | 4 | 1.20 (1.16, 1.24) | <.001 | 1.20 (1.16, 1.24) | <.001 | 2.3 | .51 | 0.0 |
| Posture 2C | 8 | 1.70 (1.52, 1.91) | <.001 | 1.84 (1.28, 2.63) | <.001 | 39.3 | <.001 | 82.2 |
| Sick leave attributable to LBP | ||||||||
| Posture 2A | 3 | 1.65 (1.23, 2.23) | <.001 | 1.47 (0.59, 3.66) | .4 | 12.1 | .002 | 83.5 |
| Posture 2B | 5 | 1.19 (1.09, 1.30) | <.001 | 1.19 (1.09, 1.30) | <.001 | 0.6 | .96 | 0.0 |
| Posture 2C | 8 | 2.26 (1.68, 3.03) | <.001 | 2.03 (1.26, 3.38) | .004 | 11.8 | .11 | 40.7 |
| Force 1C | 7 | 2.02 (1.66, 2.46) | <.001 | 1.95 (1.53, 2.49) | <.001 | 7.5 | .28 | 19.7 |
| Force 2C | 7 | 2.11 (1.73, 2.57) | <.001 | 2.11 (1.73, 2.57) | <.001 | 3.3 | .77 | 0.0 |
Note. CI = confidence interval; LBP = low back pain; OR = odds ratio. Posture 1 = trunk flexion; posture 2 = nonneutral posture; force 1 = lifting; force 2 = heavy lifting; “A” exposures represent the percentage of a workday spent in a nonneutral posture or exerting a force; “B” exposures represent the percentage of job tasks requiring a nonneutral posture or exerting a force; “C” exposures represent ever experiencing a nonneutral posture or exerting a force. ORs for “A” and “B” exposures represent the OR for a difference in exposure of 20% (approximately 1.6 hours in an 8-hour workday). ORs for “C” exposures represent the OR for any exposure compared with no exposure.
Q is the χ2 test for heterogeneity.
I2 is the percentage of the total variability in a set of effect sizes because of true heterogeneity.
When we restricted the analysis of LBP 6 to 24 months to studies collecting both nonneutral posture and lifting exposures, the OR for working in a job requiring a nonneutral posture was 1.7, and the OR for working in a job requiring lifting was 1.4. When we put both variables in the same model, the OR for nonneutral posture was 1.6 (P < .001), and the OR for lifting was 1.2 (P < .001).
Education was the only “strong” confounder in any exposure–outcome combination. Adding education to the model reduced the OR for nonneutral posture (“time”) and sick leave attributable to LBP from 2.7 (95% confidence interval [CI] = 1.9, 3.9) to 2.2 (95% CI = 1.6, 2.9). Education was a “moderate” confounder for “any” nonneutral posture (–11.3%), and “any” lifting (–10.7%) for sick leave attributable to LBP.
No factors were consistent OR modifiers for all outcome–exposure combinations (Tables 3 and 4). Of the individual-level factors, age and sex were most consistent, with older participants and men having higher ORs. “Ever having smoked” was associated with lower ORs, although the effect of current smoking status was inconsistent. For the study-level variables, exposure and population were most consistent. Direct observation and workplace-based studies were associated with lower ORs. The results for quality items and study design were inconsistent. In most cases, cross-sectional studies had higher ORs than did cohort studies. The differences tended to be greater when participants with prevalent LBP at baseline were excluded from analyses. In sensitivity analyses restricted to cohort studies, within-study results generally agreed with the meta-analysis results. There was no evidence for lack of fit in any of the final models (data not shown).
TABLE 3—
Summary of Individual Participant Data Odds Ratio Modification Analyses for Algorithmic Translation of Mechanical Exposure of Individual-Level Variables in Studies of Mechanical Workplace Risk Factors and Low Back Pain
| LBP in the Past 6 Months to 2 Years |
Current LBP |
Sick Leave Attributable to LBP |
||||||||||||||
| Variables | Posture 1A | Posture 1B | Posture 1C | Posture 2A | Posture 2B | Posture 2Ca | Force 1Ca | Force 2C | Posture 2A | Posture 2B | Posture 2Cab | Posture 2Aab | Posture 2B | Posture 2C | Force 1C | Force 2C |
| Studies, no.c | 4 | 3 | 7 | 5 | 5 | 14 | 14 | 11 | 2 | 4 | 8 | 3 | 5 | 7 | 7 | 7 |
| Age, y, OR | ||||||||||||||||
| < 30 | 1.08 | 0.97 | 1.09 | 1.21 | ||||||||||||
| 30–< 50 | 1.25 | 1.40 | 1.25 | 1.15 | ||||||||||||
| ≥50 | 1.48 | 1.64 | 1.47 | 1.51 | ||||||||||||
| Sex, OR | ||||||||||||||||
| Female | 1.09 | 1.09 | 1.56 | 1.60 | ||||||||||||
| Male | 1.40 | 1.38 | 1.89 | 2.17 | ||||||||||||
| Current smoker, OR | d | d | ||||||||||||||
| No | 1.33 | 1.09 | 1.90 | |||||||||||||
| Yes | 0.86 | 1.37 | 3.17 | |||||||||||||
| Ever smoker, OR | ||||||||||||||||
| No | 1.42 | 1.20 | ||||||||||||||
| Yes | 1.26 | 1.00 | ||||||||||||||
| BMI, OR | ||||||||||||||||
| < 30 | 1.49 | 1.19 | 1.12 | |||||||||||||
| ≥ 30 | 1.16 | 1.55 | 1.29 | |||||||||||||
| Height,e OR | ||||||||||||||||
| Low | 1.80 | 1.08 | ||||||||||||||
| High | 1.62 | 1.27 | ||||||||||||||
| Weightf | ||||||||||||||||
| Low | 1.46 | 1.13 | ||||||||||||||
| High | 0.94 | 1.38 | ||||||||||||||
| Job satisfaction,g OR | ||||||||||||||||
| Low | 1.14 | 1.14 | 1.04 | 4.64 | ||||||||||||
| High | 1.27 | 1.27 | 1.29 | 1.60 | ||||||||||||
| Psychological job demands,h OR | ||||||||||||||||
| Low | 0.88 | 1.08 | ||||||||||||||
| High | 1.27 | 1.28 | ||||||||||||||
| Job control,i OR | ||||||||||||||||
| Low | 1.37 | 1.82 | 1.11 | |||||||||||||
| High | 1.24 | 1.33 | 1.26 | |||||||||||||
Note. BMI = body mass index (defined as weight in kilograms divided by the square of height in meters); LBP = low back pain; OR = odds ratio. Posture 1 = trunk flexion; posture 2 = nonneutral posture; force 1 = lifting; force 2 = heavy lifting; “A” exposures represent the percentage of a workday spent in a nonneutral posture or exerting a force; “B” exposures represent the percentage of job tasks requiring a nonneutral posture or exerting a force; “C” exposures represent ever experiencing a nonneutral posture or exerting a force.
The outcome–exposure combinations with heterogeneity indicated in aggregate data analysis.
Meta-regression not done because the number of studies was < 10.
Analyses included all studies of the variable of interest. The total number of studies included in each analysis may vary.
A variable identified as an OR modifier in the aggregate data analysis but not in the individual participant data analysis.
Low < 160 cm for women or < 175 cm for men; high ≥ 160 cm for women or ≥ 175 cm for men.
Low < 69 kg for women or < 89 kg for men; high ≥ 69 kg for women or ≥ 89 kg for men.
Low = not satisfied or very dissatisfied; high = satisfied or very satisfied.
Low < 50% of possible score; high ≥ 50% of possible score.
Low < 50% of possible score; high ≥ 50% of possible score.
TABLE 4—
Summary of Individual Participant Data Odds Ratio Modification Analyses for Algorithmic Translation of Mechanical Exposure of Study-Level Variables in Studies of Mechanical Workplace Risk Factors and Low Back Pain
| LBP in the Past 6 Months to 2 Years |
Current LBP |
Sick Leave Attributable to LBP |
||||||||||||||
| Variables | Posture 1A | Posture 1B | Posture 1C | Posture 2A | Posture 2B | Posture 2Ca | Force 1Ca | Force 2C | Posture 2A | Posture 2B | Posture 2Cab | Posture 2Aab | Posture 2B | Posture 2C | Force 1C | Force 2C |
| Studies, no.c | 4 | 3 | 7 | 5 | 5 | 14 | 14 | 11 | 2 | 4 | 8 | 3 | 5 | 7 | 7 | 7 |
| Study design, OR | ||||||||||||||||
| Cross-sectional | 1.13 | 1.90d | 1.65d | 2.09 | 1.19 | |||||||||||
| Cohort | 1.25 | 1.44d | 1.27d | 0.96 | 2.74 | |||||||||||
| Study design,e OR | ||||||||||||||||
| Cross-sectional | 1.27 | 1.90d | 1.65d | 2.09 | 1.19 | |||||||||||
| Cohort | 1.14 | 1.33d | 1.17d | 0.69 | 2.76 | |||||||||||
| Participation rate > 80%,OR | ||||||||||||||||
| Not reported | 1.43d | 1.18 | 1.15 | 2.74 | ||||||||||||
| Reported | 1.89d | 1.49 | 2.08 | 1.19 | ||||||||||||
| Exposure reliability, OR | ||||||||||||||||
| Not reported | 1.13 | 1.30 | 1.57d | 1.66 | 3.20 | 2.42 | ||||||||||
| Reported | 1.25 | 1.94 | 1.10d | 2.77 | 1.13 | 1.94 | ||||||||||
| Outcome reliability, OR | ||||||||||||||||
| Not reported | 0.99 | 3.20 | 1.95 | |||||||||||||
| Reported | 1.57 | 1.13 | 2.15 | |||||||||||||
| Dose–response analysis,OR | ||||||||||||||||
| Not reported | 2.25 | |||||||||||||||
| Reported | 1.80 | |||||||||||||||
| Exposure type, OR | ||||||||||||||||
| Observation-based | 0.98 | 1.01d | 1.07d | 0.96 | 1.80 | |||||||||||
| Self-report | 1.50 | 1.82d | 1.59d | 2.09 | 2.25 | |||||||||||
| Population type, OR | ||||||||||||||||
| Workplace-based | 1.30 | 1.43d | 1.24d | 1.26 | ||||||||||||
| Population-based | 1.63 | 1.94d | 1.70d | 2.14 | ||||||||||||
Note. LBP = low back pain; OR = odds ratio. Posture 1 = trunk flexion; posture 2 = nonneutral posture; force 1 = lifting; force 2 = heavy lifting; “A” exposures represent the percentage of a workday spent in a nonneutral posture or exerting a force; “B” exposures represent the percentage of job tasks requiring a nonneutral posture or exerting a force; “C” exposures represent ever experiencing a nonneutral posture or exerting a force.
The outcome–exposure combinations with heterogeneity indicated in aggregate data analysis.
Meta-regression not done because the number of studies was < 10.
Analyses include all studies of the variable of interest. The total number of studies included in each analysis may vary.
Variable also identified as an odds ratio modifier in meta-regression.
Includes only incident cases for cohort studies.
DISCUSSION
Overall, the magnitudes of the pooled ORs between posture exposures and LBP (1.1–2.0) were similar to those between force exposures and LBP (1.4–2.1), but in some cases the summary estimates could be misleading because there was substantial heterogeneity. There was also evidence that posture and force were independently related to LBP. In the case of LBP 6 to 24 months, both working in a nonneutral posture and lifting were independently predictive (OR = 1.6 and 1.2, respectively), although this finding was based on the subset of studies in which both posture and force variables were measured. Odds ratios for sick leave attributable to LBP (1.2–2.1) were slightly higher than those for current LBP (1.2–1.8) and LBP 6 to 24 months (1.1–1.7).
There was little evidence of strong confounding. This implies that differential adjustment for such confounders among studies would likely not lead to substantial heterogeneity in a traditional meta-analysis. Individual participant data analyses indicated the most consistent sources of heterogeneity were age, sex, study design (cross-sectional vs cohort), type of exposure measurement (observation vs self-report), and study population (population-based vs workplace-based).
Two of the most striking findings were related to the type of exposure measurement. The first was that “any” exposures were typically associated with the most heterogeneity compared with the “time” and “task” exposures. The implication is that the never-or-ever coding of exposure may not be sufficient for meta-analyses, in that the “ever” group encompasses very different amounts of exposure depending on the study population, thus leading to differences among the study-specific ORs and heterogeneity in a meta-analysis. Although studies are grouped to look at similar exposures, it is likely that residual differences still exist.
The second finding was the attenuation of the relationship between mechanical exposure and LBP when we used methods less susceptible to exposure misclassification (direct observation). We found this attenuation across all outcomes but most often with the “any” never-or-ever exposures. One possible explanation is that participants who already had LBP may have attributed it to work and thus were more likely to overestimate their mechanical exposure. To test this, we restricted the analysis to prospective cohort studies and incident cases of LBP. The results were similar in cohort studies in which participants with LBP were included at baseline, but they weakened when we restricted the analysis to the inception cohort studies for all LBP outcomes except sick leave attributable to LBP, in which case the attenuation was the same for the cohort and inception cohort studies. Within-study comparisons were possible for studies in which both direct observation and self-report data were collected. These analyses also indicated some attenuation in the relationship between mechanical exposure and LBP with direct observation data compared with self-report. Even within direct observation, however, random error can also be introduced when systematic observations are too few or too short.48
The most consistent individual-level sources of heterogeneity identified in the individual participant data analysis were age and sex. Overall, older workers and men tended to have higher ORs for nonneutral posture, lifting, and LBP. The relationship between increasing LBP and age has been well studied.85 However, there is evidence that physical workload measured by the sum of heavy lifting, awkward postures, and whole-body vibrations is more likely to predict incident LBP in younger workers than in older workers, which is counter to our findings.86 If workers who experience LBP are self-selected out of physically demanding jobs, the healthy worker effect would tend to attenuate (or potentially reverse) a positive relationship between age and LBP. If this is the case, the actual effect of age may be even greater.
Our finding of higher ORs for men than women seems less intuitive. Because men are typically stronger, one would think they would be less prone to LBP attributable to workplace physical factors. In a systematic review of the literature, Hooftman et al.87 found evidence for men having a higher risk of back complaints for lifting. They postulated that the total weight lifted is affected by the weight of the torso, so men would on average be lifting more. In addition, Marras et al.88 reported that men experienced significantly greater compression forces than women had. Another possible explanation is a gender difference in the healthy worker effect— i.e., women with symptoms leave their jobs earlier than do men with symptoms; thus, women remaining in physical jobs may be more resistant to mechanical exposures than men are. There has recently been evidence of this in a population-based study of shoulder pain in Finland.89
We did not find consistent OR modification with any of the quality items that were assessed. In particular, lower participation rates, reporting of exposure and outcome reliability, and reporting a dose–response analysis were not consistently related to a higher or lower OR. This article includes only a subset of potentially important quality variables. A more comprehensive assessment of quality was completed by Langlois,49 who found a similar lack of consistency of OR modification for 50 quality items.
This study represents a methodologically rigorous meta-analysis meeting all recommended criteria.90 Great efforts were made to comprehensively review the LBP literature, and requests for raw data were generally positively received. Collaboration with the study authors allowed us to clarify data issues and obtain additional data. However, there might be selection bias. To better examine this possibility, when authors told us data could not be provided we asked them why. The most commonly cited reason was that the data were no longer available. The factors most strongly associated with the willingness to provide individual participant data were the year of publication and the study size; our results drew on larger and more recent studies.
To better understand the complex relationship between workplace mechanical risk factors and LBP, assessing the potential for confounding and OR modification of individual-level factors is essential. Examining individual-level OR modifiers, however, is not possible in aggregate data meta-analysis unless stratified results are consistently reported among studies. Although individual participant data meta-analysis cannot answer all questions, it provides a method to systematically examine these individual-level factors, which provides context when one is interpreting the entirety of evidence. Individual participant data analysis, however, is resource- and time-intensive and may be best suited to areas of public health importance where there is a lack of consensus in interpreting the current evidence.
Acknowledgments
This study was funded by the Canadian Institutes for Health Research (grants FRN-67042 and ICH-63069), part of the Interdisciplinary Capacity Enhancement Teams Grant Program, with support from the Centre of Research Expertise for the Prevention of Musculoskeletal Disorders.
The authors would like to thank the members of the MAPLE Collaborative Group for their continued support of our project, the participants in the Delphi process of outcome categorization (Paulien Bongers, Alex Burdorf, David Coggon, Jill Hayden, Niklas Krause, and Annette Leclerc), the expert mechanical exposure raters (Alex Burdorf, W. Monroe Keyserling, Robert Norman, Patrick Neumann, Jim Potvin, David Rempel, Allard van der Beek, Judy Village, and Richard Wells), and student mechanical exposure raters (Rebecca Brookham, Steve Brown, Nicholas Hogg, Kristen McFall, Kevin Perdeau, and Lindsay Slater) for their invaluable contributions.
Human Participant Protection
This study was approved by the McMaster University research ethics board.
References
- 1.Musculoskeletal Disorders and Workplace Factors. A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati, OH: National Institute for Occupational Safety and Health; 1997 [Google Scholar]
- 2.Andersson G. Low back pain in industry: epidemiologic aspects. Scand J Rehabil Med. 1979;11(4):163–168 [PubMed] [Google Scholar]
- 3.Andersson GB. Epidemiologic aspects on low-back pain in industry. Spine (Phila Pa 1976). 1981;6(1):53–60 [DOI] [PubMed] [Google Scholar]
- 4.Bakker EW, Verhagen AP, van Trijffel E, Lucas C, Koes BW. Spinal mechanical load as a risk factor for low back pain: a systematic review of prospective cohort studies. Spine. 2009;34(8):E281–E293 [DOI] [PubMed] [Google Scholar]
- 5.Bovenzi M, Hulshof CT. An updated review of epidemiologic studies on the relationship between exposure to whole-body vibration and low back pain (1986–1997). Int Arch Occup Environ Health. 1999;72(6):351–365 [DOI] [PubMed] [Google Scholar]
- 6.Burdorf A, Sorock G. Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health. 1997;23(4):243–256 [DOI] [PubMed] [Google Scholar]
- 7.Davis KG, Heaney CA. The relationship between psychosocial work characteristics and low back pain: underlying methodological issues. Clin Biomech (Bristol, Avon). 2000;15(6):389–406 [DOI] [PubMed] [Google Scholar]
- 8.Davis KG, Jorgensen MJ. Biomechanical modeling for understanding of low back injuries: a systematic review. Occup Ergon. 2005;5:57–76 [Google Scholar]
- 9.Frank JW, Brooker AS, DeMaio SEet al. Disability resulting from occupational low back pain. Part II: What do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine (Phila Pa 1976). 1996;21(24):2918–2929 [DOI] [PubMed] [Google Scholar]
- 10.Frank JW, Kerr MS, Brooker ASet al. Disability resulting from occupational low back pain. Part I: What do we know about primary prevention? A review of the scientific evidence on prevention before disability begins. Spine (Phila Pa 1976). 1996;21(24):2908–2917 [DOI] [PubMed] [Google Scholar]
- 11.Gallagher S. Physical limitations and musculoskeletal complaints associated with work in unusual or restricted postures: a literature review. J Safety Res. 2005;36(1):51–61 [DOI] [PubMed] [Google Scholar]
- 12.Garg A, Moore JS. Epidemiology of low-back pain in industry. Occup Med. 1992;7(4):593–608 [PubMed] [Google Scholar]
- 13.Hartvigsen J, Leboeuf-Yde C, Lings S, Corder EH. Is sitting-while-at-work associated with low back pain? A systematic, critical literature review. Scand J Public Health. 2000;28(3):230–239 [PubMed] [Google Scholar]
- 14.Hayes M, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7(3):159–165 [DOI] [PubMed] [Google Scholar]
- 15.Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Physical load during work and leisure time as risk factors for back pain. Scand J Work Environ Health. 1999;25(5):387–403 [DOI] [PubMed] [Google Scholar]
- 16.Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine (Phila Pa 1976). 2000;25(16):2114–2125 [DOI] [PubMed] [Google Scholar]
- 17.Hulshof C, van Zanten BV. Whole-body vibration and low-back pain. A review of epidemiologic studies. Int Arch Occup Environ Health. 1987;59(3):205–220 [DOI] [PubMed] [Google Scholar]
- 18.Jensen RC. Back injuries among nursing personnel related to exposure. Appl Occup Environ Hyg. 1990;5:38–45 [Google Scholar]
- 19.Kelsey JL, Golden AL. Occupational and workplace factors associated with low back pain. Occup Med. 1988;3(1):7–16 [PubMed] [Google Scholar]
- 20.Kuiper JI, Burdorf A, Verbeek JHAM, Frings-Dresen MHW, van der Beek AJ, Viikari-Juntura ERA. Epidemiologic evidence on manual materials handling as a risk factor for back disorders: a systematic review. Int J Ind Ergon. 1999;24:389–404 [Google Scholar]
- 21.Linton SJ. Occupational psychological factors increase the risk for back pain: a systematic review. J Occup Rehabil. 2001;11(1):53–66 [DOI] [PubMed] [Google Scholar]
- 22.Lötters F, Burdorf A, Kuiper J, Miedema H. Model for the work-relatedness of low-back pain. Scand J Work Environ Health. 2003;29(6):431–440 [DOI] [PubMed] [Google Scholar]
- 23.Pope MH. Risk indicators in low back pain. Ann Med. 1989;21(5):387–392 [DOI] [PubMed] [Google Scholar]
- 24.Pope MH, Goh KL, Magnusson ML. Spine ergonomics. Annu Rev Biomed Eng. 2002;4:49–68 [DOI] [PubMed] [Google Scholar]
- 25.Riihimäki H. Low-back pain, its origin and risk indicators. Scand J Work Environ Health. 1991;17(2):81–90 [PubMed] [Google Scholar]
- 26.Roffey DM, Wai EK, Bishop P, Kwon BK, Dagenais S. Causal assessment of awkward occupational postures and low back pain: results of a systematic review. Spine J. 2010;10(1):89–99 [DOI] [PubMed] [Google Scholar]
- 27.Roffey DM, Wai EK, Bishop P, Kwon BK, Dagenais S. Causal assessment of occupational sitting and low back pain: results of a systematic review. Spine J. 2010;10(3):252–261 [DOI] [PubMed] [Google Scholar]
- 28.Roffey DM, Wai EK, Bishop P, Kwon BK, Dagenais S. Causal assessment of occupational standing or walking and low back pain: results of a systematic review. Spine J. 2010;10(3):262–272 [DOI] [PubMed] [Google Scholar]
- 29.Troup JD. Causes, prediction and prevention of back pain at work. Scand J Work Environ Health. 1984;10(6 spec no):419–428 [DOI] [PubMed] [Google Scholar]
- 30.Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med (Lond). 2001;51(2):124–135 [DOI] [PubMed] [Google Scholar]
- 31.Wai EK, Roffey DM, Bishop P, Kwon BK, Dagenais S. Causal assessment of occupational bending or twisting and low back pain: results of a systematic review. Spine J. 2010;10(1):76–88 [DOI] [PubMed] [Google Scholar]
- 32.Waters T, Genaidy A, Barriera Viruet H, Makola M. The impact of operating heavy equipment vehicles on lower back disorders. Ergonomics. 2008;51(5):602–636 [DOI] [PubMed] [Google Scholar]
- 33.Waters T, Genaidy A, Deddens J, Barriera-Viruet H. Lower back disorders among forklift operators: an emerging occupational health problem? Am J Ind Med. 2005;47(4):333–340 [DOI] [PubMed] [Google Scholar]
- 34.Marras WS, Cutlip RG, Burt SE, Waters TR. National occupational research agenda (NORA) future directions in occupational musculoskeletal disorder health research. Appl Ergon. 2009;40(1):15–22 [DOI] [PubMed] [Google Scholar]
- 35.Borkan J, Van Tulder M, Reis S, Schoene ML, Croft P, Hermoni D. Advances in the field of low back pain in primary care: a report from the fourth international forum. Spine (Phila Pa 1976). 2002;27(5):E128–E132 [DOI] [PubMed] [Google Scholar]
- 36.Frank JW, Pulcins IR, Kerr MS, Shannon HS, Stansfeld SA. Occupational back pain—an unhelpful polemic. Scand J Work Environ Health. 1995;21(1):3–14 [DOI] [PubMed] [Google Scholar]
- 37.Griffith LE, Hogg-Johnson S, Cole DCet al. Low-back pain definitions in occupational studies were categorized for a meta-analysis using Delphi consensus methods. J Clin Epidemiol. 2007;60(6):625–633 [DOI] [PubMed] [Google Scholar]
- 38.Griffith LE, Wells RP, Shannon HS, Walter SD, Cole DC, Hogg-Johnson S; Meta-analysis of Pain in the Lower Back and Work Exposures Collaborative Group. Developing common metrics of mechanical exposures across aetiological studies of low back pain in working populations for use in meta-analysis. Occup Environ Med. 2008;65(7):467–481 [DOI] [PubMed] [Google Scholar]
- 39.Lemeshow AR, Blum RE, Berlin JA, Stoto MA, Colditz GA. Searching one or two databases was insufficient for meta-analysis of observational studies. J Clin Epidemiol. 2005;58(9):867–873 [DOI] [PubMed] [Google Scholar]
- 40.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine (Phila Pa 1976). 1997;22(20):2323–2330 [DOI] [PubMed] [Google Scholar]
- 41.Griffith L, Shannon H, Wells R, Cole D, Hogg-Johnson S, Walter S. The use of individual participant data (IPD) for examining heterogeneity in a meta-analysis of biomechanical workplace risk factors and low back pain. Presented as a poster and oral presentation at: Fifth International Scientific Conference on Prevention of Work-Related Musculoskeletal Disorders; July 14, 2004; Zurich, Switzerland: 337–338 [Google Scholar]
- 42.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khan KS, ter Riet G, Popay J, Nixon J, Kleijnen J. Study quality assessment. : Khan KS, ter Riet G, Glanville J, Sowden AJ, Kleijnen J, Undertaking Systematic Reviews of Research Effectiveness. CRD's Guidance for Carrying Out or Commissioning Reviews. York, England: NHS Centre for Reviews and Dissemination (CRD), University of York; 2001:1–20 [Google Scholar]
- 44.Wells GA, Shea B, O'Connell Det al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2000. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed May 31, 2010
- 45.Barrero LH, Katz JN, Perry MJ, Krishnan R, Ware JH, Dennerlein JT. Work pattern causes bias in self-reported activity duration: a randomised study of mechanisms and implications for exposure assessment and epidemiology. Occup Environ Med. 2009;66(1):38–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takala EP, Pehkonen I, Forsman Met al. Systematic evaluation of observational methods assessing biomechanical exposures at work. Scand J Work Environ Health. 2010;36(1):3–24 [DOI] [PubMed] [Google Scholar]
- 47.Armstrong BK, White E, Saracci R. Exposure measurement error and its effects. : Armstrong BK, White E, Saracci R. Principles of Exposure Measurement in Epidemiology. New York, NY: Oxford University Press; 2000:49–75 Monographs in Epidemiology and Biostatistics; vol 21 [Google Scholar]
- 48.Jansen JP, Burdorf A. Effects of measurement strategy and statistical analysis on dose–response relations between physical workload and low back pain. Occup Environ Med. 2003;60(12):942–947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Langlois LE. Quality Assessment of Observational Studies of Low Back Pain Among Workers [master's thesis] Hamilton, Ontario: McMaster University; 2008 [Google Scholar]
- 50.Barnekow-Bergkvist M, Hedberg GE, Janlert U, Jansson E. Determinants of self-reported neck-shoulder and low back symptoms in a general population. Spine (Phila Pa 1976). 1998;23(2):235–243 [DOI] [PubMed] [Google Scholar]
- 51.Burdorf A, van Riel M, Brand T. Physical load as risk factor for musculoskeletal complaints among tank terminal workers. Am Ind Hyg Assoc J. 1997;58(7):489–497 [DOI] [PubMed] [Google Scholar]
- 52.Byrns G, Reeder G, Jin G, Pachis K. Risk factors for work-related low back pain in registered nurses, and potential obstacles in using mechanical lifting devices. J Occup Environ Hyg. 2004;1(1):11–21 [DOI] [PubMed] [Google Scholar]
- 53.Elders LAM, Heinrich J, Burdorf A. Risk factors for sickness absence because of low back pain among scaffolders. Spine. 2003;28(12):1340–1346 [DOI] [PubMed] [Google Scholar]
- 54.Goldsheyder D, Nordin M, Weiner SS, Hiebert R. Musculoskeletal symptom survey among mason tenders. Am J Ind Med. 2002;42(5):384–396 [DOI] [PubMed] [Google Scholar]
- 55.Harkness EF, Macfarlane GJ, Nahit ES, Silman AJ, McBeth J. Risk factors for new-onset low back pain amongst cohorts of newly employed workers. Rheumatology (Oxford). 2003;42(8):959–968 [DOI] [PubMed] [Google Scholar]
- 56.Hoogendoorn WE, Bongers PM, de Vet HC, Ariens GA, van Mechelen W, Bouter LM. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med. 2002;59(5):323–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang GD, Feuerstein M, Kop WJ, Schor K, Arroyo F. Individual and combined impacts of biomechanical and work organization factors in work-related musculoskeletal symptoms. Am J Ind Med. 2003;43(5):495–506 [DOI] [PubMed] [Google Scholar]
- 58.Jansen JP, Morgenstern H, Burdorf A. Dose-response relations between occupational exposures to physical and psychosocial factors and the risk of low back pain. Occup Environ Med. 2004;61(12):972–979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kerr MS, Frank JW, Shannon HSet al. Biomechanical and psychosocial risk factors for low back pain at work. Am J Public Health. 2001;91(7):1069–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Korkmaz NC, Kirdi N. Pain and occupational risk factors in textile industry workers. Pain Clin. 2003;15:219–223 [Google Scholar]
- 61.Lee P, Helewa A, Goldsmith CH, Smythe HA, Stitt LW. Low back pain: prevalence and risk factors in an industrial setting. J Rheumatol. 2001;28(2):346–351 [PubMed] [Google Scholar]
- 62.Lei L, Dempsey PG, Xu J-G, Ge L-N, Liang Y- X. Risk factors for the prevalence of musculoskeletal disorders among Chinese foundry workers. Int J Ind Ergon. 2005;35:197–204 [Google Scholar]
- 63.Masset D, Malchaire J. Low back pain. Epidemiologic aspects and work-related factors in the steel industry. Spine. 1994;19(2):143–146 [PubMed] [Google Scholar]
- 64.Matsui H, Maeda A, Tsuji H, Naruse Y. Risk indicators of low back pain among workers in Japan. Association of familial and physical factors with low back pain. Spine (Phila Pa 1976). 1997;22(11):1242–1247 [DOI] [PubMed] [Google Scholar]
- 65.Maul I, Läubli T, Klipstein A, Krueger H. Course of low back pain among nurses: a longitudinal study across eight years. Occup Environ Med. 2003;60(7):497–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miranda H, Viikari-Juntura E, Martikainen R, Takala EP, Riihimäki H. Individual factors, occupational loading, and physical exercise as predictors of sciatic pain. Spine (Phila Pa 1976). 2002;27(10):1102–1109 [DOI] [PubMed] [Google Scholar]
- 67.Ozguler A, Leclerc A, Landre MF, Pietri-Taleb F, Niedhammer I. Individual and occupational determinants of low back pain according to various definitions of low back pain. J Epidemiol Community Health. 2000;54(3):215–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Palmer KT, Griffin MJ, Syddall HE, Pannett B, Cooper C, Coggon D. The relative importance of whole body vibration and occupational lifting as risk factors for low-back pain. Occup Environ Med. 2003;60(10):715–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smedley J, Egger P, Cooper C, Coggon D. Prospective cohort study of predictors of incident low back pain in nurses. BMJ. 1997;314(7089):1225–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sobti A, Cooper C, Inskip H, Searle S, Coggon D. Occupational physical activity and long-term risk of musculoskeletal symptoms: a national survey of post office pensioners. Am J Ind Med. 1997;32(1):76–83 [DOI] [PubMed] [Google Scholar]
- 71.Tousignant M, Tougas G, Rossignol M, Goulet L. Development of a systematic observation protocol of physical exposure of the back: a preliminary study. Ann Occup Hyg. 2002;46(3):317–327 [DOI] [PubMed] [Google Scholar]
- 72.Vingård E, Alfredsson L, Hagberg Met al. To what extent do current and past physical and psychosocial occupational factors explain care-seeking for low back pain in a working population? Results from the Musculoskeletal Intervention Center–Norrtalje Study. Spine (Phila Pa 1976). 2000;25(4):493–500 [DOI] [PubMed] [Google Scholar]
- 73.Walsh K, Cruddas M, Coggon D. Interaction of height and mechanical loading of the spine in the development of low-back pain. Scand J Work Environ Health. 1991;17(6):420–424 [DOI] [PubMed] [Google Scholar]
- 74.Wickström GJ, Pentti J. Occupational factors affecting sick leave attributed to low-back pain. Scand J Work Environ Health. 1998;24(2):145–152 [DOI] [PubMed] [Google Scholar]
- 75.Xu Y, Bach E, Orhede E. Work environment and low back pain: the influence of occupational activities. Occup Environ Med. 1997;54(10):741–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yip VY. New low back pain in nurses: work activities, work stress and sedentary lifestyle. J Adv Nurs. 2004;46(4):430–440 [DOI] [PubMed] [Google Scholar]
- 77.Diggle PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. Oxford, UK: Oxford Science Publication, Clarendon Press; 1994 [Google Scholar]
- 78.SAS/STAT User's Guide. Version 8 Cary, NC: SAS Institute Inc; 2003 [Google Scholar]
- 79.Evans S, Li LL. A comparison of goodness of fit tests for the logistic GEE model. Stat Med. 2005;24(8):1245–1261 [DOI] [PubMed] [Google Scholar]
- 80.Horton NJ, Bebchuk JD, Jones CL. Goodness-of-fit for GEE: an example with mental health service utilization. Stat Med. 1999;18(2):213–222 [DOI] [PubMed] [Google Scholar]
- 81.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188 [DOI] [PubMed] [Google Scholar]
- 82.Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2(2):121–145 [DOI] [PubMed] [Google Scholar]
- 83.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558 [DOI] [PubMed] [Google Scholar]
- 84.Deeks JJ, Higgins JPT, Altman DG. Analysing and presenting results. : Higgins JPT, Green S, Cochrane Handbook for Systemic Reviews of Interventions 4.2.6. Chichester, UK: John Wiley & Sons Ltd; 2006 [Google Scholar]
- 85.Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. 2006;35(3):229–234 [DOI] [PubMed] [Google Scholar]
- 86.Miranda H, Viikari-Juntura E, Punnett L, Riihimäki H. Occupational loading, health behavior and sleep disturbance as predictors of low-back pain. Scand J Work Environ Health. 2008;34(6):411–419 [DOI] [PubMed] [Google Scholar]
- 87.Hooftman WE, van Poppel MN, van der Beek AJ, Bongers PM, van Mechelen W. Gender differences in the relations between work-related physical and psychosocial risk factors and musculoskeletal complaints. Scand J Work Environ Health. 2004;30(4):261–278 [DOI] [PubMed] [Google Scholar]
- 88.Marras WS, Davis KG, Jorgensen M. Gender influences on spine loads during complex lifting. Spine J. 2003;3(2):93–99 [DOI] [PubMed] [Google Scholar]
- 89.Miranda H, Viikari-Juntura E, Heistaro S, Heliövaara M, Riihimäki H. A population study on differences in the determinants of a specific shoulder disorder versus nonspecific shoulder pain without clinical findings. Am J Epidemiol. 2005;161(9):847–855 [DOI] [PubMed] [Google Scholar]
- 90.Stroup DF, Berlin JA, Morton SCet al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012 [DOI] [PubMed] [Google Scholar]