Abstract
Objective
To determine whether the image quality (IQ) is improved with iterative reconstruction in image space (IRIS), and whether IRIS can be used for radiation reduction in chest CT.
Materials and Methods
Standard dose chest CT (SDCT) in 50 patients and low dose chest CT (LDCT) in another 50 patients were performed, using a dual-source CT, with 120 kVp and same reference mAs (50 mAs for SDCT and 25 mAs for LDCT) employed to both tubes by modifying a dual-energy scan mode. Full-dose data were obtained by combining the data from both tubes and half-dose data were separated from a single tube. These were reconstructed by using a filtered back projection (FBP) and IRIS: full-dose FBP (F-FBP); full-dose IRIS (F-IRIS); half-dose FBP (H-FBP) and half-dose IRIS (H-IRIS). Objective noise was measured. The subjective IQ was evaluated by radiologists for the followings: noise, contrast and sharpness of mediastinum and lung.
Results
Objective noise was significantly lower in H-IRIS than in F-FBP (p < 0.01). In both SDCT and LDCT, the IQ scores were highest in F-IRIS, followed by F-FBP, H-IRIS and H-FBP, except those for sharpness of mediastinum, which tended to be higher in FBP. When comparing CT images between the same dose and different reconstruction (F-IRIS/F-FBP and H-IRIS/H-FBP) algorithms, scores tended to be higher in IRIS than in FBP, being more distinct in half-dose images. However, despite the use of IRIS, the scores were lower in H-IRIS than in F-FBP.
Conclusion
IRIS generally helps improve the IQ, being more distinct at the reduced radiation. However, reduced radiation by half results in IQ decrease even when using IRIS in chest CT.
Keywords: Iterative reconstruction in image space, Chest CT, Radiation dose reduction, Image quality
INTRODUCTION
The high contrast between air and pulmonary parenchyma makes the lungs suitable for the assessment by a reduced dose CT. Although the various methods have been developed and used to reduce the radiation dose and improve image quality for a CT, lowering the tube current manually and dynamic adjustment of the tube current, during scanning at a fixed peak tube voltage, are the most practical ways of achieving radiation dose reduction (1-9). However, the use of low mAs in filtered back projection (FBP), the current CT image reconstruction technique, unavoidably increases the image noise, which is inversely proportional to the square root of mAs (3). This is a major limitation of FBP in radiation dose reduction, and most studies have shown that perceived image quality (IQ) is lower in the reduced-dose than in the standard-dose chest CT (10-14).
Currently, the iterative reconstruction techniques have been proposed as one approach to improving the IQ and reducing the radiation dose in a CT (15-17). In the iterative reconstruction, once CT image has been reconstructed from the projected raw data using the FBP, and new forward projected raw data, which exactly represent the CT image, are obtained using mathematical calculations. However, the new projected raw data is not identical to the original scanner-acquired raw data. Therefore, the difference between these two raw data is used to derive the corrected projections, reconstruct a corrected image and update the corrected CT image. Then this circuit starts again, and it is continued until the deviation between the measured and calculated projections is smaller than a preset limit. This method, however, takes a much longer time than FBP because of the intense computations required for a single iteration. Iterative reconstruction in image space (IRIS), by using a master raw data reconstruction, and the iterative image correction with this master reconstruction, rather than the original raw data in image space, enables the image reconstruction in a clinically acceptable time. Additionally, decoupling of the spatial resolution and image noise may be allowed that the image noise can be reduced without degradation of the detail resolution.
To our knowledge, the comparison of the IQ of a chest CT, reconstructed with IRIS and FBP technique, in an intraindividual and intraexam comparison by a dual-source CT and the investigation of the usefulness of IRIS technique for the radiation dose reduction have not been performed. In this two-part study, we investigated whether the IQ is improved with IRIS in a chest CT, and we assessed the influence of the IRIS technique on the radiologist's preference. Then we tried to know whether IRIS can be used for the reduction of the radiation dose by half in a chest CT. In part 1 of this study, we evaluated the IQ.
MATERIALS AND METHODS
Patients
This prospective study was approved by our institutional review board. Informed consent was obtained from all participating patients.
From March to April 2010, 50 patients (30 men, 20 women; mean age, 56.4 ± 14.9 years; range, 18-79 years, mean BMI, 23.0 ± 3.0 kg/m2) underwent standard dose chest CT (SDCT) and another 50 patients (31 men, 19 women; mean age, 57.2 ± 11.9 years; range, 27-76 years, BMI, 24.0 ± 3.0 kg/m2) underwent low dose chest CT (LDCT). All patients were evaluated for the check-up or for known abnormalities.
CT Examination and Reconstruction
All CT scans were performed with a dual-source CT scanner (Somatom Definition; Siemens Medical Solutions, Erlangen, Germany). A saline bag was placed on the upper anterior chest wall of the patient, during CT scanning, for a quantitative measurement of the image noise. To acquire both the full radiation dose data and half radiation dose data, without additional CT scanning, we performed CT scanning using a modifying dual energy CT scan mode employing the same voltage and the same mAs to both X-ray tubes. The reference values applied to both tubes were 50 mAs at 120 kVp for SDCT and 25 mAs at 120 kVp for LDCT. Automated dose modulation (CARE Dose 4D, Siemens Healthcare, Erlangen, Germany) was used in all cases. The central 14 rows of detectors with 1.2 mm collimation were used to improve a scatter-correction. The craniocaudal direction was used for all scans. Each subject was administered 100 mL of iomeprol (Iomeron 300; Bracco, Milan, Italy) at a rate of 3.0 mL/s, using a power injector for SDCT, and CT scanning was performed at a fixed scan delay of 50 seconds. No contrast material was used for LDCT. CT data, at full radiation dose (100 effective mAs for SDCT and 50 effective mAs for LDCT), were obtained by combining the data from both tubes. Half radiation dose CT data was separated from the detector A alone (50 effective mAs for SDCT and 25 effective mAs for LDCT).
Both full-radiation dose data and half-radiation dose data, from one SDCT scan, were reconstructed using the standard FBP algorithm and the IRIS algorithm. Therefore 4 CT image sets from one SDCT scan were obtained: 1) FBP images at full radiation dose (F-FBP), 2) IRIS images at full radiation dose (F-IRIS), 3) FBP images at half radiation dose (H-FBP), and 4) IRIS images at half radiation dose (H-IRIS). In FBP images, the CT images were reconstructed in 5 mm thickness at 5 mm intervals with the B30f kernel for the evaluation of mediastinal structures, and the CT images were reconstructed at 5 mm thickness at 5-mm intervals, and 1 mm thickness at 1 mm intervals with B70f kernel for the evaluation of the lung parenchyma. For IRIS, we used the I30f (5 mm thickness at 5 mm intervals) for the mediastinum and the I70f (5 mm thickness at 5 mm intervals and 1 mm thickness at 1 mm intervals) for the lung parenchyma. Finally, total of 200 CT image sets from 50 SDCT scan, were prepared for review: 1) F-FBP (B30f 5 mm/B70f 5 mm/B70f 1 mm), 2) F-IRIS (B30f 5 mm/B70f 5 mm/B70f 1 mm), 3) H-FBP (B30f 5 mm/B70f 5 mm/B70f 1 mm), and 4) H-IRIS (B30f 5 mm/B70f 5 mm/B70f 1 mm), 4 image sets from one CT scan. We also performed the image reconstruction in the same way for LDCT images, and we prepared 200 CT image sets of LDCT for review. Consecutive CT examinations were dicomized and sent to our picture archiving and communication system (Petavision; Asan Medical Center, Seoul, Korea). For the evaluations of the mediastinum, the CT images with 5 mm slice thickness and B30f kernel or I30f were preset at the window level of 35 H and window width of 350 H. For the evaluations of lung parenchyma, the appropriate CT images were preset at the lung window setting (window level of -700 H and a window width of 1500 H). The radiologists were asked not to change the preset window levels and widths during the evaluation of IQ.
Image Quality
Objective Analysis
One research worker who was not involved in the subjective IQ analysis made quantitative noise measurements on CT images with B50f/5 mm thickness and I50f/5 mm thickness. Image noise measurement was made by recording the standard deviation of CT attenuation in an identically sized circular region of interest (ROI) on a saline bag at the level of the carina. The ROIs, as large as the saline bag, were used for these measurements, and care was given to the position of the ROI in the inner portion of the saline bag. The field of view (FOV) of the dual source CT was limited to 260 mm because of the smaller detector width of the one tube. ROIs for the noise measurement were placed only inside these FOVs. The size, shape, and position of the ROIs were kept constant among the 4 image sets by applying a copy and paste function at the workstation (MultiModality Workplace, Siemens Healthcare, Erlanger, Germany).
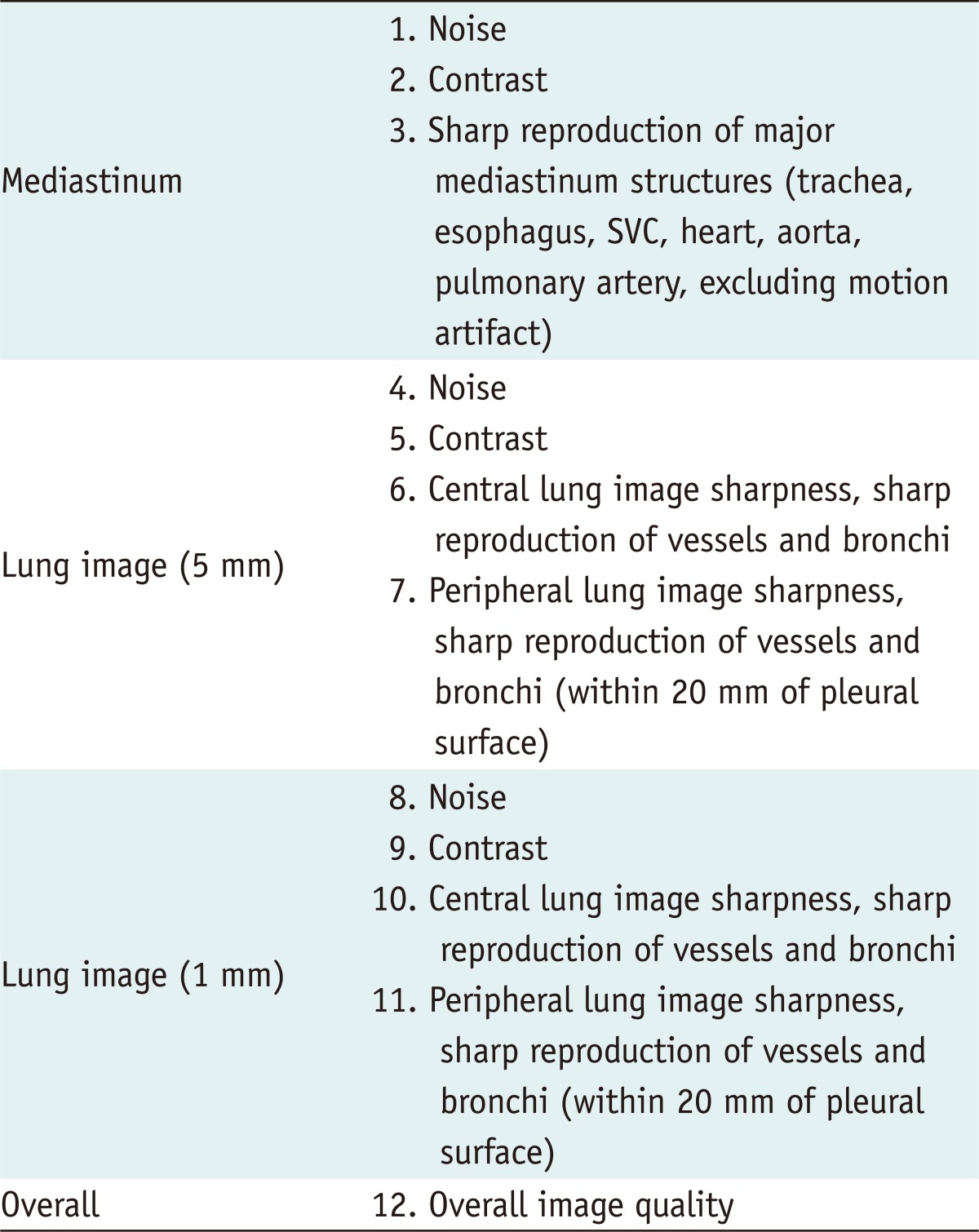
Subjective Analysis
Each 200 CT image sets of SDCT and LDCT were respectively randomized and these randomized SDCT and LDCT image sets were analyzed in different sessions by two thoracic radiologists (reader 1, with 10 years of experience and reader 2, with 5 years of experience), independently, both of who were unaware of the reconstruction methods and the radiation dose. The radiologists were asked to evaluate the noise and contrast of the mediastinum, and the sharpness of the mediastinal structures, according to a five-point scale (1, poor; 2, suboptimal; 3, adequate; 4, very good; 5, excellent). Similarly, the noise, contrast and sharpness of the central and peripheral lungs, in both 5 mm and 1 mm thickness CT images, were assessed. Finally, the overall IQ of each CT image was evaluated on a five-point scale (Table 1). Image noise was defined as the overall graininess or mottle, and image contrast was defined as the ability to differentiate between the object and its background noise.
Table 1.
Categories for Image Quality Assessment
Note.- SVC = suerior vena cava
Statistical Analysis
All statistical analyses were performed with SAS, version 9.1.3, statistical software (SAS, Cary, NC, USA). The subjective IQ scores for each category in each CT image, scored by two radiologists, were added together, resulting in the total score (2-10). In addition, for the evaluation of the differences in the total scores of subjective IQ between the 4 image sets (F-FBP, F-IRIS, H-FBP and H-IRIS), the Friedman test was used. Whenever the Friedman test revealed a significant effect of the current (p < 0.05), post hoc comparisons were performed and the difference was considered statistically significant at p < 0.001. t tests were used to compare the quantitative image noise in the half dose IRIS and the full dose FBP images.
RESULTS
Radiation Dose
CT examination and acquisition of the half dose images from the detector A were performed successfully for all subjects. The mean dose-length product (DLP) were 202.8 ± 45.6 mGy·cm for SDCT, and 127.2 ± 13.8 mGy·cm for LDCT, and the mean estimated effective doses were 2.84 ± 0.64 mSv and 1.78 ± 0.19 mSv, respectively, using a conversion factor of 0.014 mSv/mGy/cm (18). The radiation dose of the half dose images were assumed to be half of the full dataset.
Image Quality
Objective Analysis
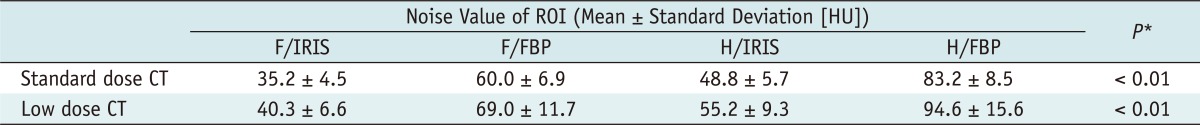
The mean quantitative ROI noise values (hounsfield unit [HU]) are summarized in Table 2. The mean noise values were significantly lower in IRIS images even with the half radiation dose than that of F-FBP, in both SDCT and LDCT (p < 0.01). Figures 1-4 shows the reduction of the image noise obtained with iterative reconstructions.
Table 2.
Quantitative Assessment of Image Noise
Note.- *Comparison between F/FBP and H/IRIS. F/FBP = full dose image with filtered back projection, F/IRIS = full dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen, Germany), H/FBP = half dose image with filtered back projection, H/IRIS = half dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen, Germany), HU = Hounsfield unit, ROI = region of interest
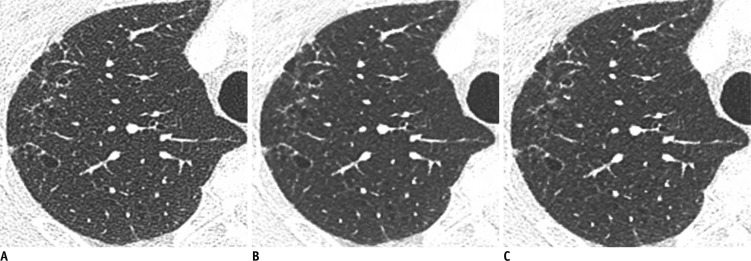
Fig. 1.
Standard dose contrast enhanced-chest CT in 48-year-old woman (BMI: 23 kg/m2) with lung cancer in left upper lobe.
A-C. Transverse CT images with (A) full radiation dose FBP in B70f kernel and 5 mm slice thickness, (B) full radiation dose IRIS in I70f kernel and 5 mm slice thickness, and (C) half radiation dose IRIS in I70f kernel and 5 mm slice thickness. Objective noise measured in saline bag was 66.1 HU, 37.5 HU and 53.8 HU, respectively (not shown). BMI = body mass index, HU = Hounsfield unit, FBP = filtered back projection, IRIS = iterative reconstruction in image space
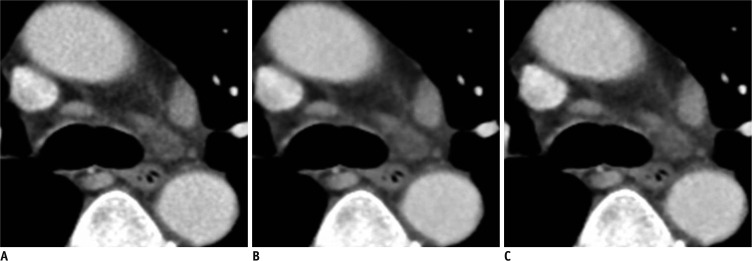
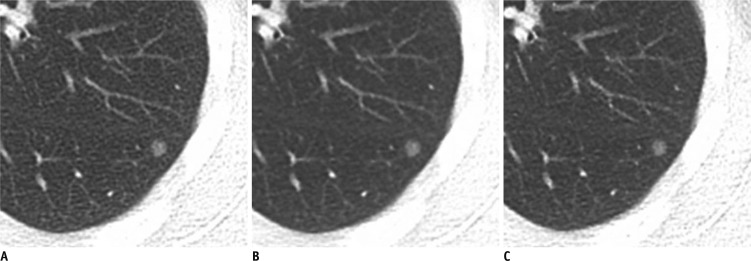
Fig. 4.
Standard dose chest CT with enhancement in 75-year-old man (BMI: 21 kg/m2) with small lymph nodes in mediastinum.
A-C. Transverse CT images with (A) full radiation dose FBP in B30f kernel and 5 mm slice thickness, (B) full radiation dose IRIS in I30f kernel and 5 mm slice thickness, and (C) half radiation dose IRIS in I30f kernel and 5 mm slice thickness. Objective noise measured in saline bag was 59.7 HU, 34.5 HU and 48.5 HU, respectively (not shown). Margins of mediastinal structures were slightly more blurred in (B) and (C) than in (A) due to excessive smoothing effect of IRIS image. BMI = body mass index, HU = Hounsfield unit, FBP = filtered back projection, IRIS = iterative reconstruction in image space
Subjective Analysis
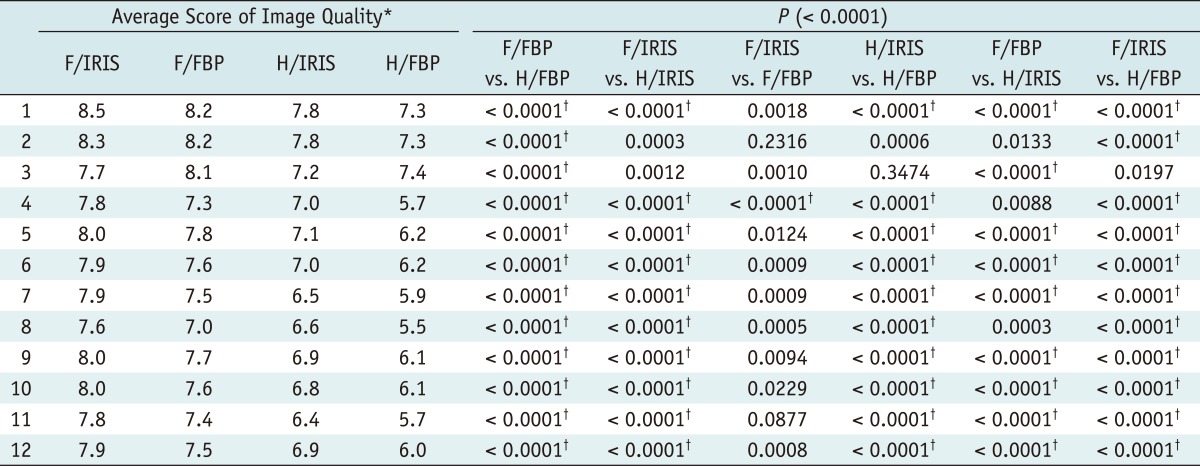
In both SDCT and LDCT, the mean total IQ scores of the F-IRIS images were highest, followed by the F-FBP, H-IRIS and H-FBP images in most assessed categories. However, the mean total IQ scores for the sharpness of mediastinal structures were highest in the F-FBP images, followed by the F-IRIS, H-IRIS and H-FBP images (Tables 3, 4) (Fig. 4). None of the mean total IQ scores of the F-IRIS, F-FBP and H-IRIS images was below 6, indicating that all of these images had adequate IQ, whereas, some H-FBP images in several categories (noise and peripheral lung image sharpness in both 5 mm and 1 mm slice thickness SDCT and LDCT for the lung evaluation and overall IQ in LDCT) were rated below 6, which indicated an inadequate IQ.
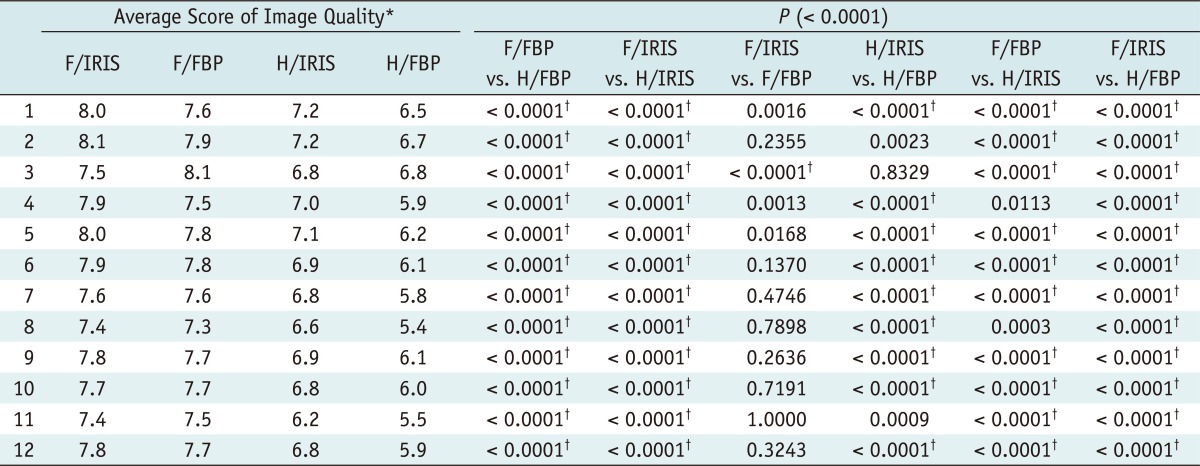
Table 3.
Scores of Image Quality in Standard Dose Chest CT
Note.- Numbers in first column is related to Table 1. Numbers of 'average score of image quality' are means of total scores resulting from sum of subjective image quality scores by two radiologists. *Friedman test showed significant results in all assessed categories, †In post hoc comparisons, p value of < 0.0001 (adjusted by Bonferroni correction) indicates significant difference. F/FBP = full dose image with filtered back projection, F/IRIS = full dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen, Germany), H/FBP = half dose image with filtered back projection, H/IRIS = half dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen, Germany)
Table 4.
Scores of Image Quality in Low Dose Chest CT
Note.- Numbers in first column is related to Table 1. Numbers of 'average score of image quality' are means of total scores resulting from sum of subjective image quality scores by two radiologists. *Friedman test showed significant results in all assessed categories, †In post hoc comparisons, p value of < 0.0001 (adjusted by Bonferroni correction) indicates significant difference. F/FBP = full dose image with filtered back projection, F/IRIS = full dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen Germany), H/FBP = half dose image with filtered back projection, H/IRIS = half dose image with iterative reconstruction in image space (Siemens Healthcare, Erlangen, Germany)
The Friedman test showed a significant difference in all the assessed categories. Post-hoc comparisons of the full dose and half dose CT images with the same reconstruction algorithm showed that the mean of total IQ scores were significantly higher for the full dose images than for the half dose images in the most assessed categories (p < 0.0001) in both SDCT and LDCT. When we compared the CT images at the same radiation dose with different reconstruction methods, the mean of total IQ scores of the IRIS images and the FBP images were not significantly different in the full dose CT images, except for image noise in lung 5 mm slice thickness image in SDCT, in which the mean total score of F-IRIS images was significantly higher than that of the F-FBP images. Otherwise, when we assessed half dose images, we found that the mean total scores were significantly higher for IRIS than for FBP images in most assessed categories (p < 0.0001), in both SDCT and LDCT. However, in the evaluations of image contrast of mediastinum and the sharpness of mediastinal structure in both SDCT and LDCT, and the peripheral lung sharpness in LDCT, the mean total IQ scores of H-IRIS images were not significantly higher than those of the H-FBP images. Comparing the F-FBP images and H-IRIS images, we found that the mean total scores were significantly higher in the full dose images with FBP than in the half dose images, even with IRIS in most categories, whereas, they did not differ significantly when assessing the image noise in lung 5 mm and 1 mm slice SDCT and LDCT, and image contrast of the mediastinum in SDCT (Tables 3, 4). Figures 1, 2 and 3 illustrate the lung parenchyma in F-FBP, F-IRIS and H-IRIS images of the SDCT and LDCT.
Fig. 2.
Standard dose contrast enhanced-chest CT in 69-year-old man (BMI: 24 kg/m2) with mild emphysema.
A-C. Transverse CT images with (A) full radiation dose FBP in B70f kernel and 1 mm slice thickness, (B) full radiation dose IRIS in I70f kernel and 1 mm slice thickness, and (C) half radiation dose with IRIS in I70f kernel and 1 mm slice thickness. Objective noise measured in saline bag was 59.9 HU, 35.7 HU and 47.6 HU, respectively (not shown). BMI = body mass index, HU = Hounsfield unit, FBP = filtered back projection, IRIS = iterative reconstruction in image space
Fig. 3.
Low dose chest CT without enhancement in 37-year-old woman (BMI: 23 kg/m2) with small ground glass nodules.
A-C. Transverse CT images with (A) full radiation dose FBP in B70f kernel and 5 mm slice thickness, (B) full radiation dose IRIS in I70f kernel and 5 mm slice thickness, and (C) half radiation dose IRIS in I70f kernel and 5 mm slice thickness. Objective noise measured in saline bag was 67.8 HU, 41.5 HU and 58.2 HU, respectively (not shown). BMI = body mass index, HU = Hounsfield unit, FBP = filtered back projection, IRIS = iterative reconstruction in image space
DISCUSSION
We have shown here that the use of IRIS technique generally improved the subjective IQ of the images obtained at the same radiation dose, and that this improvement was more distinct and statistically significant in the images obtained at the reduced radiation dose. However, subjective IQ scores for the evaluation of the sharpness of the mediastinum were higher in FBP than in IRIS images, at the same radiation dose, especially, in LDCT, due to blurred margin of the mediastinal structures in IRIS images (Fig. 4). Even with the IRIS technique, decreased radiation dose resulted in decreased subjective IQ, except for noise of lung images, in which the subjective IQ scores of IRIS images at the half radiation dose were comparable to those of FBP images at the full radiation dose.
The noise reduction effect of the IRIS was distinct, and the objective image noise was significantly lower in IRIS images, even at the half radiation dose, than in FBP images at the full radiation dose. However, this does not mean that the noise reduction effect in IRIS technique is equal in every part of these images. In each loop of the iteration steps in IRIS, the local characteristics of every part of the images is evaluated, and the non-linear image processing algorithm, which is called "regularization", is used to enhance the spatial resolution at higher object contrasts and to reduce the image noise in low contrast areas. Therefore, we performed the overall subjective IQ evaluation by the reader study in our study, beside the objective image noise evaluation.
Generally, IRIS technique could significantly reduce the objective image noise of chest CT and improve the subjective IQ. Although IRIS improved the IQ in full dose images, this improvement was not remarkable and not statistically significant, compared with the images obtained with the FBP technique. In contrast, the improvement of the IQ with IRIS in the half dose images was more distinct and statistically significant. Our explanation is that the degree of image mottling may depend on the total photon numbers used of the image, which is proportional to the selected mAs (19). The full dose images are obtained at relatively high current, which results in excellent IQ and a relatively low level of image noise. In half dose images, however, photon starvation and beam hardening artifacts contribute to the greater image noise, and the additional value of IRIS is likely to be beneficial under these circumstances. Our results, therefore, suggest that IRIS may be more beneficial in CT protocols that use lower radiation dose.
In our study, the average IQ scores of the full dose image in LDCT tended to be higher than those of the half dose image in SDCT, even though those two images sets were acquired using the same effective mAs value. However, the measured mean DLP in LDCT was higher than half of that in SDCT, which means that the actual radiation dose used for the half dose images of SDCT was lower. In addition, photon attenuation or deprivation may be greater in the SDCT than in LDCT, due to photon absorption and attenuation by the contrast medium, thus, reducing the number of photons that reach the detector in SDCT. These explanations are supported by the fact that the quantitatively assessed noise was higher in the half dose SDCT than in the full dose LDCT images. These differences also explain why IRIS improved the IQ significantly in the half dose image of SDCT, while it had little effect on the full dose images of LDCT.
A recent study reported that IRIS technique significantly reduced the image noise, in both lung and mediastinal images (20, 21). Those studies, however, did not separately evaluate the effect of IRIS on the sharpness of the mediastinal and lung structures. In the study with the adaptive statistical iterative reconstruction technique, by the Prakash et al. (22), they evaluated the visual sharpness of the thoracic structures and all the chest CT exams were rated as acceptable for the visual sharpness of the thoracic structures, regardless of their location in the mediastinum or lungs. In our study, comparing the images with the different reconstruction method and the same radiation dose, we found that, although the subjective IQ scores of the sharpness of mediastinal structures in IRIS images were rated as above acceptable, their sharpness tended to be lower in IRIS than in FBP images, due to the excessive smoothing effect of the IRIS algorithm. In contrast, IRIS images for the evaluation of the lung parenchyma showed comparable or better IQ in the evaluation of the sharpness of lung structures, as well as the image noise reduction, compared with that of the FBP images. This tendency was observed in both SDCT and LDCT. It appears to be due to that the reducing image noise process in the "regularization" step in the I30f kernel for the mediastinal image is too excessive, and this problem should be solved in the future.
According to the result of our study, for the evaluation of the subjective IQ, reducing radiation dose by 50%, using IRIS, is doubtful. But the subjective IQ for the CT image noise for the lung parenchyma, the IRIS images with reduced radiation dose by 50% were comparable with that of the FBP images, with the full radiation dose. And another study, in which we performed the radiologists' preference study with the same image data, produced different results. Moreover, radiologists preferred IRIS images for the evaluation of the lung parenchyma, even at the reduced radiation dose by 50% (23).
Although iterative reconstruction techniques have many advantages, and the IRIS technique has made possible for the actual clinical application of iterative reconstruction, the current computation processing takes more time for CT reconstruction with IRIS technique than the FBP technique. Generally CT images are reconstructed at 20 images per second, as for IRIS technique, and while for the FBP technique, they are reconstructed at 40 to 50 images per second.
This study had several limitations. Firstly, we did not evaluate the diagnostic acceptability and lesion conspicuity of the IRIS images. Although the subjective IQ of 50% reduced dose CT images, with the IRIS technique, was acceptable for the evaluation of anatomic structures and radiologists preferred IRIS images at half dose compared with that of the full dose FBP images, the diagnostic performance of the IRIS technique in the evaluation of abnormal lesions remains to be investigated. Secondly, although the radiologists who evaluated the CT images were blinded to the reconstruction method, complete blinding was not possible because the visual appearance of IRIS images was somewhat unique, especially, in the lung 1 mm thickness images. In our study, however, even though the readers might acknowledge the reconstruction method, the radiation dose of each image set was totally blinded. There was no way for the readers to know whether the images were full-dose or half-dose image. Thirdly, BMI of our patients is relatively low, due to the natural characteristics of the Asian population; thus, it is uncertain if our results can be generalized to encompass more adipose patients. Finally, we used DSCT scanners in modified dual energy mode to evaluate the half dose CT images without additional CT scanning. However, the two X-ray tubes and two detector arrays result in a cross scattering radiation (i.e., the scattering of X-ray photons from one source to the detector array of the other source). Accordingly, the effect of cross scattering radiation may have affected the image quality. However, this effect might have been negligible because the current DSCT scanners employ scatter correction algorithms to minimize the cross scattering effect (24).
In conclusion, we found that the IRIS algorithm generally improved the IQ and this improvement is more distinct and significant in the chest CT with reduced radiation dose. The 50% reduction of radiation in clinical practice is doubtful even reducing image noise significantly in chest CT with IRIS technique.
Footnotes
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A111599).
References
- 1.Kalra MK, Maher MM, Toth TL, Schmidt B, Westerman BL, Morgan HT, et al. Techniques and applications of automatic tube current modulation for CT. Radiology. 2004;233:649–657. doi: 10.1148/radiol.2333031150. [DOI] [PubMed] [Google Scholar]
- 2.Lell MM, May M, Deak P, Alibek S, Kuefner M, Kuettner A, et al. High-pitch spiral computed tomography: effect on image quality and radiation dose in pediatric chest computed tomography. Invest Radiol. 2011;46:116–123. doi: 10.1097/RLI.0b013e3181f33b1d. [DOI] [PubMed] [Google Scholar]
- 3.McNitt-Gray MF. AAPM/RSNA Physics Tutorial for Residents: topics in CT. Radiation dose in CT. Radiographics. 2002;22:1541–1553. doi: 10.1148/rg.226025128. [DOI] [PubMed] [Google Scholar]
- 4.Mulkens TH, Bellinck P, Baeyaert M, Ghysen D, Van Dijck X, Mussen E, et al. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation. Radiology. 2005;237:213–223. doi: 10.1148/radiol.2363041220. [DOI] [PubMed] [Google Scholar]
- 5.Prasad SR, Wittram C, Shepard JA, McLoud T, Rhea J. Standard-dose and 50%-reduced-dose chest CT: comparing the effect on image quality. AJR Am J Roentgenol. 2002;179:461–465. doi: 10.2214/ajr.179.2.1790461. [DOI] [PubMed] [Google Scholar]
- 6.Rothenberg LN, Pentlow KS. Radiation dose in CT. Radiographics. 1992;12:1225–1243. doi: 10.1148/radiographics.12.6.1439023. [DOI] [PubMed] [Google Scholar]
- 7.Schenzle JC, Sommer WH, Neumaier K, Michalski G, Lechel U, Nikolaou K, et al. Dual energy CT of the chest: how about the dose? Invest Radiol. 2010;45:347–353. doi: 10.1097/RLI.0b013e3181df901d. [DOI] [PubMed] [Google Scholar]
- 8.Wildberger JE, Mahnken AH, Schmitz-Rode T, Flohr T, Stargardt A, Haage P, et al. Individually adapted examination protocols for reduction of radiation exposure in chest CT. Invest Radiol. 2001;36:604–611. doi: 10.1097/00004424-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Yu L, Li H, Fletcher JG, McCollough CH. Automatic selection of tube potential for radiation dose reduction in CT: a general strategy. Med Phys. 2010;37:234–243. doi: 10.1118/1.3264614. [DOI] [PubMed] [Google Scholar]
- 10.Dinkel HP, Sonnenschein M, Hoppe H, Vock P. Low-dose multislice CT of the thorax in follow-up of malignant lymphoma and extrapulmonary primary tumors. Eur Radiol. 2003;13:1241–1249. doi: 10.1007/s00330-002-1647-0. [DOI] [PubMed] [Google Scholar]
- 11.Mayo JR, Hartman TE, Lee KS, Primack SL, Vedal S, Müller NL. CT of the chest: minimal tube current required for good image quality with the least radiation dose. AJR Am J Roentgenol. 1995;164:603–607. doi: 10.2214/ajr.164.3.7863879. [DOI] [PubMed] [Google Scholar]
- 12.Mayo JR, Kim KI, MacDonald SL, Johkoh T, Kavanagh P, Coxson HO, et al. Reduced radiation dose helical chest CT: effect on reader evaluation of structures and lung findings. Radiology. 2004;232:749–756. doi: 10.1148/radiol.2323030899. [DOI] [PubMed] [Google Scholar]
- 13.Takahashi M, Maguire WM, Ashtari M, Khan A, Papp Z, Alberico R, et al. Low-dose spiral computed tomography of the thorax: comparison with the standard-dose technique. Invest Radiol. 1998;33:68–73. doi: 10.1097/00004424-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Yamada T, Ono S, Tsuboi M, Saito H, Sato A, Matsuhashi T, et al. Low-dose CT of the thorax in cancer follow-up. Eur J Radiol. 2004;51:169–174. doi: 10.1016/j.ejrad.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 15.Gregor J, Benson T. Computational analysis and improvement of SIRT. IEEE Trans Med Imaging. 2008;27:918–924. doi: 10.1109/TMI.2008.923696. [DOI] [PubMed] [Google Scholar]
- 16.Lasio GM, Whiting BR, Williamson JF. Statistical reconstruction for x-ray computed tomography using energy-integrating detectors. Phys Med Biol. 2007;52:2247–2266. doi: 10.1088/0031-9155/52/8/014. [DOI] [PubMed] [Google Scholar]
- 17.Xu J, Tsui BM. Electronic noise modeling in statistical iterative reconstruction. IEEE Trans Image Process. 2009;18:1228–1238. doi: 10.1109/TIP.2009.2017139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.AAPM. AAPM Report No. 96: the Measurement, Reporting, and Management of Radiation Dose in CT. College Park: American Association of Physicists in Medicine; 2008. [Google Scholar]
- 19.Ravenel JG, Scalzetti EM, Huda W, Garrisi W. Radiation exposure and image quality in chest CT examinations. AJR Am J Roentgenol. 2001;177:279–284. doi: 10.2214/ajr.177.2.1770279. [DOI] [PubMed] [Google Scholar]
- 20.Pontana F, Duhamel A, Pagniez J, Flohr T, Faivre JB, Hachulla AL, et al. Chest computed tomography using iterative reconstruction vs filtered back projection (Part 2): image quality of low-dose CT examinations in 80 patients. Eur Radiol. 2011;21:636–643. doi: 10.1007/s00330-010-1991-4. [DOI] [PubMed] [Google Scholar]
- 21.Pontana F, Pagniez J, Flohr T, Faivre JB, Duhamel A, Remy J, et al. Chest computed tomography using iterative reconstruction vs filtered back projection (Part 1): evaluation of image noise reduction in 32 patients. Eur Radiol. 2011;21:627–635. doi: 10.1007/s00330-010-1990-5. [DOI] [PubMed] [Google Scholar]
- 22.Prakash P, Kalra MK, Digumarthy SR, Hsieh J, Pien H, Singh S, et al. Radiation dose reduction with chest computed tomography using adaptive statistical iterative reconstruction technique: initial experience. J Comput Assist Tomogr. 2010;34:40–45. doi: 10.1097/RCT.0b013e3181b26c67. [DOI] [PubMed] [Google Scholar]
- 23.Hwang HJ, Seo JB, Lee JS, Song JW, Kim SS, Lee HJ, et al. Radiation dose reduction of chest CT with iterative reconstruction in image space - Part II: assessment of radiologists' preferences using dual source CT. Korean J Radiol. 2012;13:720–727. doi: 10.3348/kjr.2012.13.6.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kyriakou Y, Kalender WA. Intensity distribution and impact of scatter for dual-source CT. Phys Med Biol. 2007;52:6969–6989. doi: 10.1088/0031-9155/52/23/014. [DOI] [PubMed] [Google Scholar]