Abstract
Jejunal diverticulosis is uncommon and often asymptomatic. It can produce significant complications, and some complications are potentially life threatening and require early surgical treatment, such as obstruction, hemorrhage and perforation. There is no consensus on the management of this disease. Only a few cases of jejunal diverticulosis with midgut volvulus have been reported. We herein report a case of 57-year-old woman with jejunal diverticulosis causing small bowel volvulus who complained of intermittent upper abdominal pin-prick for 5 years that eventually progressed to a complete obstruction. The computed tomography scans revealed a mesenteric vessel "whirlpool" and laparotomy showed midgut volvulus secondary to jejunal diverticula. This case highlights jejunal diverticulosis causing small bowel volvulus as an uncommon mechanism of small bowel obstruction, which should be included in the differential diagnosis of small bowel obstruction.
Keywords: Jejunal diverticulosis, Midgut volvulus, Intestinal obstruction, Computed tomography, Surgery
INTRODUCTION
Although jejunal diverticulosis is rare and often asymptomatic[1], it can produce severe complications, such as obstruction, diverticulitis, hemorrhage and perforation. Obstruction can be caused by inflammatory stenosis, jejuna stones of the small bowel or small bowel volvulus. Most of the patients with gastrointestinal obstruction may require surgical intervention. Here we describe a patient with midgut volvulus due to jejunal diverticula. The computed tomography (CT) scans revealed a mesenteric vessel "whirlpool" and laparotomy showed midgut volvulus secondary to jejunal diverticula.
CASE REPORT
A 57-year old woman presented to our department with a 5-year history of increasingly intermittent upper abdominal pin-prick pain, which would occur after meals and eased in the right lateral decubitus. She denied any change in bowel or bladder habits, or presence of other gastrointestinal symptoms. There was no other relevant past medical, family or surgical histories. Left upper quadrant tenderness was found on physical examination.
The initial contrast-enhanced CT scan of the abdomen showed mesentery and superior mesenteric artery with "whirlpool" signs (Figure 1). However, most whirl signs exhibited on CT suggest but not prove to be indicative of small bowel volvulus[2]. Therefore, the patient was referred for an angiography due to the suspicion of a vascular variation as a reason to explain her intermittent upper abdominal pain. On the angiography, the superior mesenteric artery appeared twisted. Subsequent contrast barium study was performed with the suspicion of intestinal volvulus. The upper gastrointestinal barium study showed a diverticulum of duodenum, multiple giant jejunal diverticula and certified midgut volvulus (Figures 2 and 3).
Figure 1.
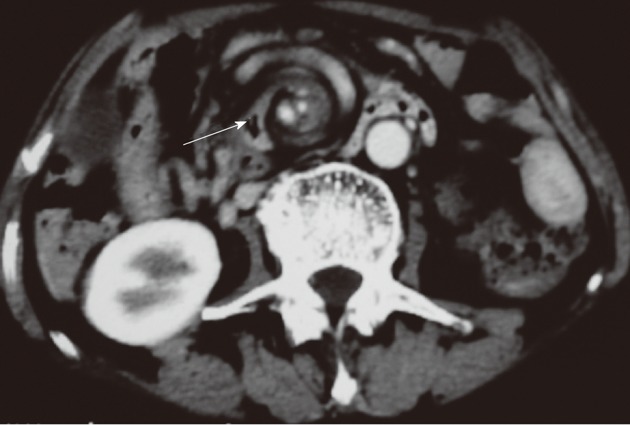
Initial contrast-enhanced computed tomography scan of the abdomen showed mesentery and superior mesenteric artery with "whirlpool" signs (arrow).
Figure 2.
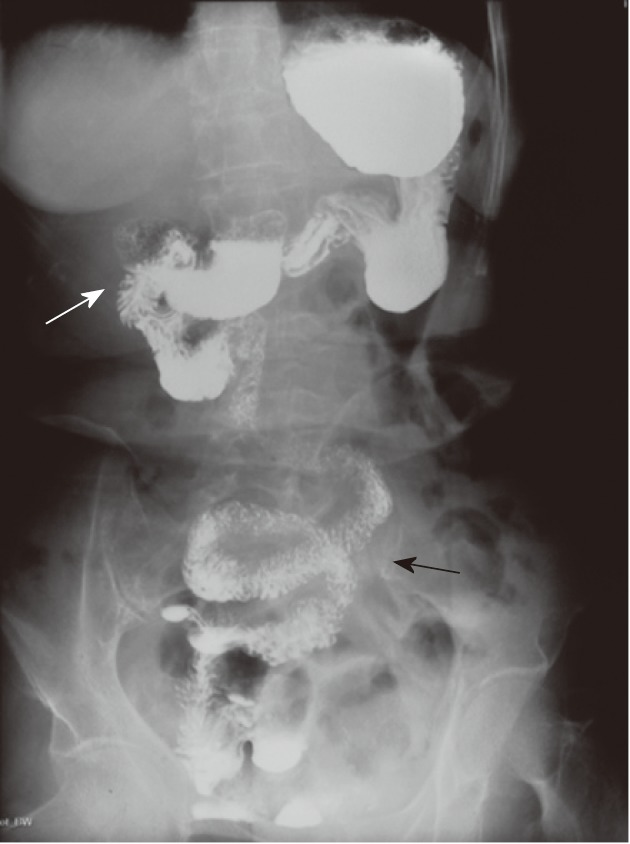
Upper gastrointestinal barium studies demonstrated duodenal diverticulum (white arrow) and "corkscrew" configuration (black arrow) of proximal small bowel.
Figure 3.
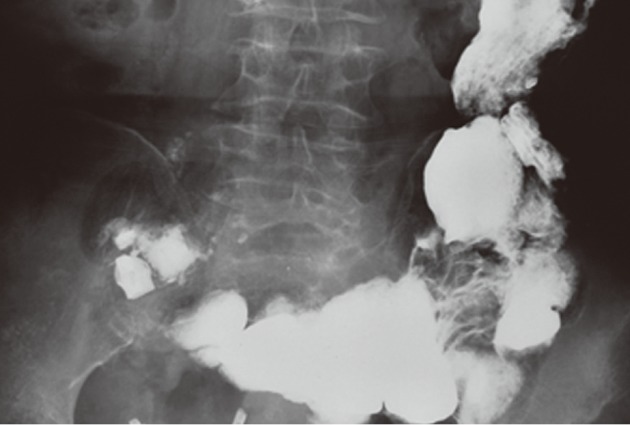
Upper gastrointestinal barium study showed multiple giant jejunal diverticula.
On the fourth day of hospitalization, the patient experienced a worsening of pain. Physical examination revealed tenderness in the whole abdomen, with tinkling bowel sounds. Abdominal X-ray showed dilated bowel loops and air-fluid levels. Surgery was indicated based on the clinical manifestations, the symptoms of obstruction and the examination results.
She underwent an emergency laparotomy which revealed diffuse giant jejunal diverticulosis and midgut volvulus. The diameters of these diverticula ranged between 3.5 cm and 8 cm. The whole jejuna and its mesentery were found twisted clockwise by 540-degree at the root of mesentery. The proximal half of the small bowel was dilated, congested, and oedematous (Figure 4). Excision of the small bowel containing multiple jejunal diverticula and an end-to-end anastomosis of the jejuna were performed. The patient had an uneventful postoperative recovery and was discharged on the 12th post-operative day.
Figure 4.

Extremely enlarged jejuna were seen after distortion. Enlargement starts 20 cm distal to the ligament of Treitz and extends to 120 cm.
DISCUSSION
Jejunal diverticulosis is a rare entity with an incidence rate ranging from 0.3%-1.3% in autopsy series to 2.3% in radiographic findings[1]. Etiology of jejunal diverticulosis is still uncertain. Increased intraluminal pressure may play an important role. The mean age of symptomatic patients is up to 60 years in all reported studies. It is reported that jejunal diverticulosis associated with visceral neuropathies can lead to an increased intraluminal pressure, and it is commonly seen in connective tissue diseases, such as systemic lupus erythematosus[3-6].
About 80% of the jejunal diverticulosis cases present with no symptoms, and chronic clinical manifestations may be misdiagnosed as dyspepsia and irritable bowel syndrome, which delayed the correct diagnosis in its early phase.
A few symptomatic patients may explain of chronic post-prandial abdominal pain, nausea and vomiting, borborygmi, alternating diarrhea and constipation, weight loss, anemia, steatorrhea, tenderness and fever[7]. We should pay attention to these symptoms which reflect inflammation, malabsorption, hemorrhage or mechanical obstruction.
Mechanical intestinal obstruction occurs in 2.3%- 4.6% of cases of jejuno-ileal diverticulosis[8]. Obstruction can be caused by inflammatory stenosis, intussusceptions and voluminous jejuna stones. Besides, in jejuno-ileal diverticulosis, volvulus of the diverticula-containing segment is a cause of intestinal obstruction. The involved segment, which is filled with fluid and is heavier than the non-involved part, might be responsible for initiating the volvulus[8]. It is reported that a large small-bowel diverticulum was much more frequently seen in patients with volvulus (35%) than in those with small bowel volvulus (1%) (P < 0.001)[9].
The diagnostic work-up in asymptomatic patients can start with plain abdominal X-ray or CT. But in some cases, these modalities fail to show typical jejunal diverticula. Since they are situated along the mesenteric border, it makes the diagnosis difficult. The specific diagnosis of small bowel diverticula is possible by radiologic contrast studies using various forms of barium[10,11]. The radiologic technique of enteroclysis is specific for the jejuna and the ileum, and the barium meal for the duodenum[12]. Similar to the diverticulitis of the large intestine, perforation is the most common complication in diverticulitis of the small intestine[13]. Perforation is associated with peritonitis in most cases. Thus, we should choose iodine contrast instead of barium if perforation is suspected, considering the high mortality of barium solution peritonitis. Enteroscopy may be another feasible method for diagnosing small bowel diverticulosis[10,14]. In recent years, endoscopy has replaced enteroclysis and has become the most widespread technique for the diagnosis of small bowel diverticula[15].
In case of acute abdomen pain due to small bowel volvulus, repeated physical examinations and X-ray films are recommended. Besides, CT examination and angiographic study are helpful in diagnosis. The "whirl sign" on abdominal CT refers to a whirling or spiral shape of the mesenteric vessels, which may accompany the intestinal loops and their feeding vessels[2,16]. Fisher first described it as a CT finding suggestive of midgut volvulus[17]. It is a sensitive marker of volvulus with a sensitivity of 60% and an odds ratio of 25.3 in predicting the presence of small bowel obstruction necessitating surgery[18]. Awareness of the CT whirl sign is important in the triage of patients who need emergency surgical intervention[19]. Although angiography is not feasible for all the suspected cases of intestinal volvulus due to its invasive nature and high cost, it is still a good method for preoperative evaluation of the "whirlpool" and "barber's pole"[16].
Usually uncomplicated jejunal diverticulosis does not require operative management. However, surgical intervention is mandatory in patients with complications of jejunal diverticulosis. Surgical therapy of jejunal diverticulosis with small bowel volvulus consists of untwisting or resecting the involved segment. A mortality rate of 25% was reported[8].
In our case, the main clinical symptom in the patient's history was increasingly intermittent upper abdominal pin-prick pain with vomiting. It was caused by hyperdistention of the voluminous diverticula. The thickened and enlarged small bowel found at laparotomy would suggest that partial obstruction was present for some time before the acute episode.
In summary, we present a case of a midgut volvulus which was induced by jejunal diverticula. Jejunal diverticulosis remains asymptomatic in about 80% of cases, making the diagnosis both delayed and difficult. Diagnosis is often initiated in cases with related complications, such as hemorrhage, perforation or obstruction. Intestinal obstruction can be caused by inflammatory stenosis, jejunal stones, intussusception or volvulus. It is suggested that a large small-bowel diverticulum might play a contributing role in the occurrence of small bowel volvulus in adults. Enteroclysis is probably the most reliable method for diagnosing small bowel diverticulosis. In case of acute abdomen pain due to small bowel volvulus, CT examination shows typical signs of this disorder. The whirl signs detected on CT have a high specificity for small bowel volvulus. Surgical excision of the affected jejuna segment with primary end-to-end anastomosis is the treatment of choice.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Qing-Ping Cai from the Department of General Surgery, Changzheng Hospital, for providing the surgical information and photographs of the patient.
Footnotes
Peer reviewer: Dr. José Liberato Ferreira Caboclo, Professor, Rua Antônio de Godoy, São José do Rio Preto 4120, Brazil
S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13:2240–2242. doi: 10.3748/wjg.v13.i15.2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gollub MJ, Yoon S, Smith LM, Moskowitz CS. Does the CT whirl sign really predict small bowel volvulus?: Experience in an oncologic population. J Comput Assist Tomogr. 2006;30:25–32. doi: 10.1097/01.rct.0000191680.28344.f0. [DOI] [PubMed] [Google Scholar]
- 3.Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983;85:538–547. [PubMed] [Google Scholar]
- 4.Machin GA, Walther GL, Fraser VM. Autopsy findings in two adult siblings with Coffin-Lowry syndrome. Am J Med Genet Suppl. 1987;3:303–309. doi: 10.1002/ajmg.1320280536. [DOI] [PubMed] [Google Scholar]
- 5.Milanes-Gonzalez A, Herrera-Esparza R, Arguelles R. Multiple duodenum-jejunal diverticula in a case of scleroderma. Clin Exp Rheumatol. 1986;4:289–290. [PubMed] [Google Scholar]
- 6.Yağmur Y, Aldemir M, Büyükbayram H, Taçyildiz I. Multiple jejunal diverticulitis with perforation in a patient with systemic lupus erythematosus: report of a case. Surg Today. 2004;34:163–166. doi: 10.1007/s00595-003-2653-9. [DOI] [PubMed] [Google Scholar]
- 7.Lempinen M, Salmela K, Kemppainen E. Jejunal diverticulosis: a potentially dangerous entity. Scand J Gastroenterol. 2004;39:905–909. doi: 10.1080/00365520410006288. [DOI] [PubMed] [Google Scholar]
- 8.de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523–2528. doi: 10.1111/j.1572-0241.1998.00605.x. [DOI] [PubMed] [Google Scholar]
- 9.Chou CK, Mark CW, Wu RH, Chang JM. Large diverticulum and volvulus of the small bowel in adults. World J Surg. 2005;29:80–82. doi: 10.1007/s00268-004-7454-9. [DOI] [PubMed] [Google Scholar]
- 10.Maglinte DD, Chernish SM, DeWeese R, Kelvin FM, Brunelle RL. Acquired jejunoileal diverticular disease: subject review. Radiology. 1986;158:577–580. doi: 10.1148/radiology.158.3.3080802. [DOI] [PubMed] [Google Scholar]
- 11.Salomonowitz E, Wittich G, Hajek P, Jantsch H, Czembirek H. Detection of intestinal diverticula by double-contrast small bowel enema: differentiation from other intestinal diverticula. Gastrointest Radiol. 1983;8:271–278. doi: 10.1007/BF01948132. [DOI] [PubMed] [Google Scholar]
- 12.Maglinte DD, Hall R, Miller RE, Chernish SM, Rosenak B, Elmore M, Burney BT. Detection of surgical lesions of the small bowel by enteroclysis. Am J Surg. 1984;147:225–229. doi: 10.1016/0002-9610(84)90094-1. [DOI] [PubMed] [Google Scholar]
- 13.Makris K, Tsiotos GG, Stafyla V, Sakorafas GH. Small intestinal nonmeckelian diverticulosis. J Clin Gastroenterol. 2009;43:201–207. doi: 10.1097/MCG.0b013e3181919261. [DOI] [PubMed] [Google Scholar]
- 14.Hortling N, Vahlensieck M, Schweikert HU, Vetter H, Schild HH. [Clinical aspects and diagnosis of jejunal diverticulosis] Aktuelle Radiol. 1995;5:367–369. [PubMed] [Google Scholar]
- 15.Bach AG, Lübbert C, Behrmann C, Surov A. [Small bowel diverticula - diagnosis and complications] Dtsch Med Wochenschr. 2011;136:140–144. doi: 10.1055/s-0031-1272497. [DOI] [PubMed] [Google Scholar]
- 16.Bozlar U, Ugurel MS, Ustunsoz B, Coskun U. CT angiographic demonstration of a mesenteric vessel “whirlpool” in intestinal malrotation and midgut volvulus: a case report. Korean J Radiol. 2008;9:466–469. doi: 10.3348/kjr.2008.9.5.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher JK. Computed tomographic diagnosis of volvulus in intestinal malrotation. Radiology. 1981;140:145–146. doi: 10.1148/radiology.140.1.7244217. [DOI] [PubMed] [Google Scholar]
- 18.Duda JB, Bhatt S, Dogra VS. Utility of CT whirl sign in guiding management of small-bowel obstruction. AJR Am J Roentgenol. 2008;191:743–747. doi: 10.2214/AJR.07.3386. [DOI] [PubMed] [Google Scholar]
- 19.Chen HL, Bair MJ, Lin IT, Wu CH. Whirl sign. Am J Med Sci. 2011;342:423. doi: 10.1097/MAJ.0b013e318228c2e6. [DOI] [PubMed] [Google Scholar]


