Abstract
Although endoplasmic reticulum (ER) stress is a pathologic mechanism in a variety of chronic diseases, it is unclear what role it plays in chronic hypertension (HTN). Dysregulation of brain mechanisms controlling arterial pressure is strongly implicated in HTN, particularly in models involving angiotensin II (Ang II). We tested the hypothesis that ER stress in the brain is causally linked to Ang II–dependent HTN. Chronic systemic infusion of low-dose Ang II in C57BL/6 mice induced slowly developing HTN, which was abolished by co-infusion of the ER stress inhibitor tauroursodeoxycholic acid (TUDCA) into the lateral cerebroventricle. Investigations of the brain regions involved revealed robust increases in ER stress biomarkers and profound ER morphological abnormalities in the circumventricular subfornical organ (SFO), a region outside the blood-brain barrier and replete with Ang II receptors. Ang II–induced HTN could be prevented in this model by selective genetic supplementation of the ER chaperone 78-kDa glucose-regulated protein (GRP78) in the SFO. These data demonstrate that Ang II–dependent HTN is mediated by ER stress in the brain, particularly the SFO. To our knowledge, this is the first report that ER stress, notably brain ER stress, plays a key role in chronic HTN. Taken together, these findings may have broad implications for the pathophysiology of this disease.
Introduction
ER stress has emerged as a major pathophysiological mechanism of various chronic diseases. The ER, the cellular organelle responsible for protein synthesis, folding, and trafficking, is also recognized as a primary sensor of cellular stress. Perturbations that challenge normal ER function, such as increased protein synthesis, alterations in cellular redox status, and disturbances in intracellular Ca2+ levels, trigger ER stress and lead to activation of a conserved set of intracellular signaling cascades called the unfolded protein response (UPR) (1–3). The UPR facilitates adaptation to acute cellular perturbations and reestablishes ER homeostasis. However, long-term UPR activation can disrupt cellular function and lead to chronic disease (2–4).
Essential hypertension (HTN) affects nearly 1 billion people worldwide, increasing the risk for diseases of the heart, kidneys, and brain (5). Interestingly, cellular perturbations known to cause ER stress, including oxidative stress and alterations in intracellular Ca2+, are prevalent in HTN (6). Whether ER stress plays a role in HTN is largely unknown.
There is compelling evidence that alterations in CNS circuits involved in cardiovascular regulation are a key mechanism of HTN (6, 7). ER stress in the CNS leads to long-term changes in neural function through alterations in molecules known to be involved in CNS-driven HTN, including Ca2+, ROS and transcription factors such as NF-κB and AP-1 (1, 6, 7).
The circumventricular subfornical organ (SFO), a tiny forebrain structure sitting outside the BBB, has emerged as pivotal in certain forms of HTN, especially those involving Ang II (6–8). The SFO serves as a “gateway” for circulating factors such as Ang II that are too large to cross the BBB and access key CNS cardiovascular centers (8). This is interesting in the context of ER stress, since UPR activation is particularly relevant in cells exposed to chronic environmental stimuli or insults (3). Because the SFO is perpetually exposed to changing levels of circulating hormones, electrolytes, and metabolites, neurons in this brain region may be especially susceptible to perturbations of ER homeostasis. Furthermore, alterations in Ca2+ and redox signaling in the SFO, two key ER modulators, are strongly implicated in Ang II–dependent HTN (6, 7).
Here we tested the hypothesis that ER stress in the brain, particularly the SFO, mediates Ang II–dependent HTN. Our findings provide the first evidence to our knowledge that elevated circulating levels of Ang II in mice induce robust ER stress in the SFO and that this is causally linked to the rise in arterial pressure (AP) in this model of HTN.
Results and Discussion
Induction of brain ER stress causes sympathetic nervous system activation and elevations in AP.
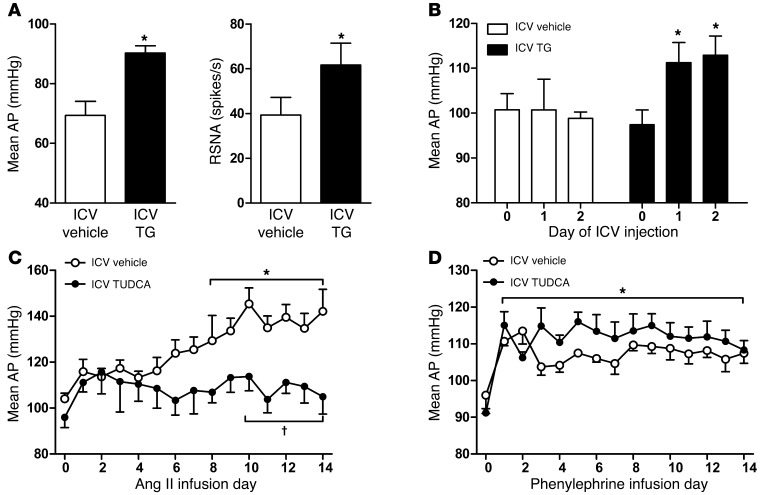
The UPR consists of complex intracellular signaling cascades, including 3 ER stress transduction branches: protein kinase R–like ER kinase (PERK), activating transcription factor–6 (ATF-6), and inositol-requiring enzyme 1 (IRE-1) (1–3). Due to this complexity, one method of evoking generalized ER stress in cells and tissues, including the brain, is via the chemical agent thapsigargin (TG) (9). We tested whether ER stress in the brain is causally linked to cardiovascular and autonomic regulation by directly injecting TG via an indwelling lateral ventricle (ICV) cannula in adult male C57BL/6 mice and measuring AP and renal sympathetic nerve activity (RSNA) under anesthesia 24 hours later. Mice treated with a single brain injection of TG showed elevated mean AP and RSNA a day later compared with vehicle controls (Figure 1A). These findings were extended using radiotelemetric recordings of AP in conscious mice. Induction of ER stress in the brain via ICV TG injections over a 2-day period resulted in a significant elevation in AP by the first day, and this was sustained through the second day (Figure 1B). No changes in AP were observed in mice that received brain injections of vehicle over the same time period. The data corroborate those of Purkayastha et al., which showed that TG injections into the ventral third ventricle of the brain resulted in a significant short-term elevation in AP (9). These findings provide strong evidence that acute induction of ER stress in the brain activates the sympathetic nervous system and elevates AP.
Figure 1. ER stress in the brain increases AP and RSNA and mediates systemic Ang II–induced HTN.
The chemical ER stress inducer TG or vehicle was injected via an ICV cannula in male C57BL/6 mice. (A) Mean AP and RSNA in anesthetized mice 24 hours after brain injections (n = 7–8). (B) Mean AP in conscious mice over 2 days of brain TG or vehicle injections (n = 4–5); *P < 0.05 versus ICV vehicle or day 0. In separate experiments, chronic HTN was induced over 2 weeks with systemic infusion of Ang II (600 ng/kg/min) or phenylephrine (30 μg/kg/min) in conjunction with brain infusion of the ER stress inhibitor TUDCA or vehicle via an ICV cannula. AP recorded by radiotelemetry in conscious mice during (C) Ang II or (D) phenylephrine infusion in combination with brain delivery of TUDCA or vehicle (n = 3–5). *P < 0.05 versus day 0; †P < 0.05 versus ICV vehicle.
ER stress in the CNS mediates chronic Ang II HTN.
To determine whether ER stress in the brain contributes to the development of chronic HTN, we utilized an experimental mouse model in which long-term systemic infusion of low-dose Ang II causes slowly developing yet persistent elevations in AP that are dependent on CNS mechanisms (7). This model of Ang II HTN is thought to recapitulate key features of human essential HTN, including central neural dysregulation (10). We tested whether brain infusion of tauroursodeoxycholic acid (TUDCA), a chemical ER chaperone that relieves ER stress in vivo (11, 12), would ameliorate Ang II HTN as measured by radiotelemetry in conscious mice. Mice that were administered vehicle ICV exhibited the classic, steadily increasing and sustained HTN produced by systemic Ang II infusions over 2 weeks (Figure 1C). In contrast, mice that received ICV TUDCA showed no change in AP over the 2-week Ang II infusion period. In another hypertensive model in which the α1 adrenergic receptor agonist phenylephrine was infused systemically over the same period of time, the rise in AP was unaffected by delivery of TUDCA to the brain (Figure 1D). These data suggest that ER stress in the brain is causally linked to Ang II–induced HTN, and elevated AP itself is not sensitive to inhibition of brain ER stress.
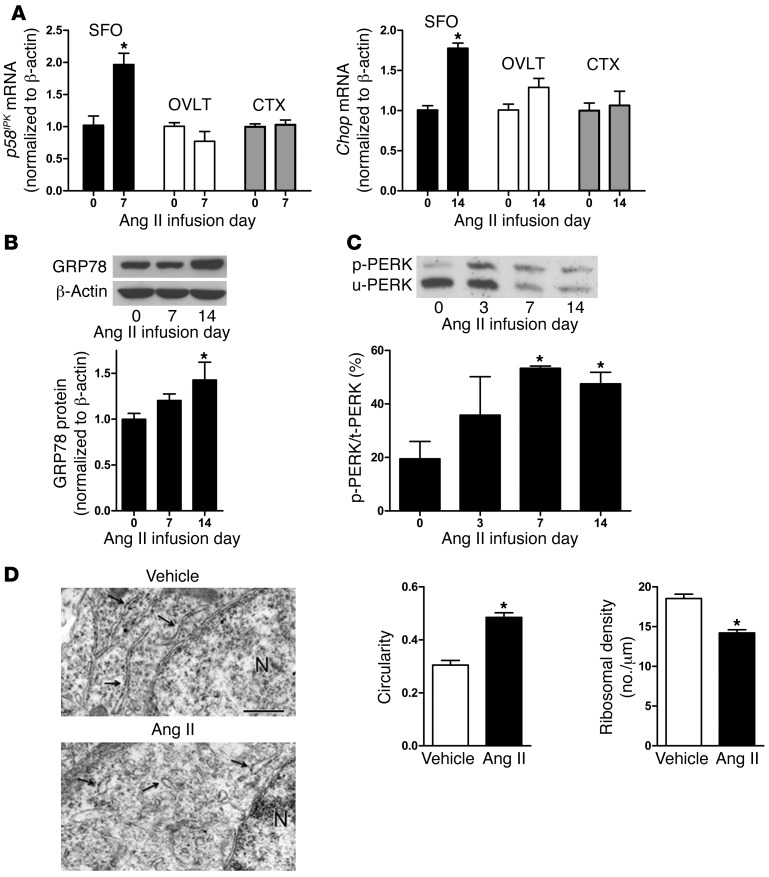
Elevated circulating Ang II induces ER stress biomarker expression in the SFO.
The findings presented in Figure 1 suggest that increased levels of circulating Ang II result in ER stress in the brain, which is functionally linked to the development of HTN. A key question is what CNS regions undergo ER stress during Ang II HTN. Since circulating Ang II does not cross the BBB but gains access to cardiovascular regulatory centers of the brain parenchyma through sites such as the SFO (8), we first profiled key ER stress biomarkers in this region and in the other forebrain circumventricular region known for mediating the central actions of Ang II, the organum vasculosum lamina terminalis (OVLT). Real-time PCR revealed a doubling of p58IPK mRNA, an ER molecule induced during the early adaptive phase of the UPR (2, 3), in micropunches obtained from SFO at a pre-hypertensive time point (day 7) (Figure 2A). In addition, mRNA levels of Chop, a major downstream effector of the UPR that signals long-term ER stress (2, 3), were significantly elevated in the SFO at 14 days of Ang II infusion when HTN was maximal (Figure 2A). Neither of these markers was altered in the OVLT or the cerebral cortex (CTX), a control brain region inside the BBB (Figure 2A). Furthermore, no changes in ER stress marker expression were observed in any of the regions during systemic vehicle infusion (data not shown).
Figure 2. Increased circulating Ang II induces ER stress in the SFO.
(A) Real-time PCR measurements of ER stress biomarkers p58IPK and Chop from micropunches of the SFO, OVLT, and CTX at key time points during systemic Ang II infusions (n = 3–4). (B) Representative Western blot and quantitative summary of the ER chaperone GRP78 in SFO homogenates at select time points during Ang II–induced HTN (n = 3–5). (C) Representative Phos-tag gel (upper panel) showing phosphorylated (p-PERK) and un-phosphorylated (u-PERK) PERK in SFO homogenates harvested at key time points during Ang II infusions. Data are summarized (lower panel) and expressed as a percentage of p-PERK relative to total PERK (n = 3). (D) Representative electron micrographs (left panels) of RER (arrows) in SFO neurons at day 14 of vehicle or Ang II infusions (N, nucleus). Quantification (right panels) of RER profile circularity (4π × area/ perimeter2) and ribosome density (n = 105–121 RER profiles/group, n = 3 mice/group). Scale bar: 500 nm. *P < 0.05 versus day 0 or vehicle.
These findings suggest that the SFO may be particularly susceptible to systemic Ang II–induced ER stress during the development of HTN in this model. Thus, further ER stress biomarker profiling studies were carried out, focusing specifically on this brain region. A key response to ER perturbation is induction of the ER-resident chaperone 78-kDa glucose-regulated protein (GRP78), which facilitates UPR activation (1, 2). GRP78 is upregulated in a variety of animal models of disease and in patients (13). Protein levels of this ER chaperone showed a trend toward being increased in SFO micropunches harvested prior to an increase in AP (day 7, Figure 2B, P = 0.07) and were significantly elevated during peak Ang II–induced HTN (day 14, P < 0.05, Figure 2B). In contrast, GRP78 was not altered in SFO during HTN induced by systemic infusion of phenylephrine (data not shown), indicating that ER chaperone upregulation in this brain region was Ang II dependent and not due to an increase in AP per se. Finally, given the emerging role of the PERK pathway in cardiovascular and neural diseases (14), we utilized a Phos-tag–based system (15) to investigate whether elevated levels of circulating Ang II cause activation, i.e., phosphorylation of PERK, in SFO (1). Ang II infusion caused a significant increase in the percentage of p-PERK (relative to total PERK) in SFO at both pre-hypertensive (day 7) and peak hypertensive (day 14) phases, with approximately 50% of PERK undergoing phosphorylation at these time points compared with baseline (Figure 2C). No increases in p-PERK were observed in SFO of vehicle-infused mice (data not shown). These data suggest that increased circulating Ang II causes robust UPR activation in the SFO.
Increased systemic Ang II causes ultrastructural abnormalities in the ER of SFO neurons.
In addition to changes in UPR molecules, ultrastructural abnormalities of the rough ER (RER) are another classic hallmark of ER stress (1, 14). Using electron microscopic analysis of SFO tissue harvested during peak Ang II HTN (day 14), we observed distended and disorganized ER cisternae with ribosomal detachment in SFO neurons (Figure 2D). In contrast, the RER of SFO neurons from vehicle-infused mice at this time point exhibited the normal parallel “stacked” arrangement, with attached ribosomes covering the exterior surface. Quantitative analysis revealed significant increases in circularity, i.e., distension, and reductions in ribosomal density of the RER profiles in SFO neurons of Ang II hypertensive mice (Figure 2D). These data demonstrate that systemic infusion of Ang II causes abnormal RER morphology in SFO neurons, further confirming that Ang II HTN is characterized by robust ER stress in the SFO.
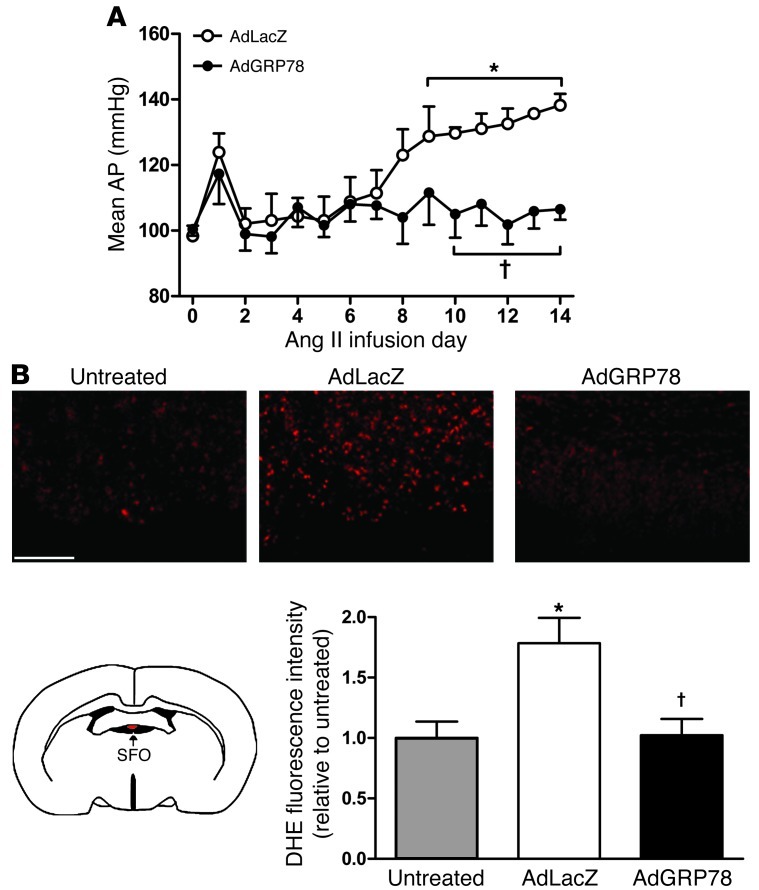
Ang II–induced ER stress in the SFO is functionally linked to HTN.
The data in Figures 1 and 2 demonstrate that ER stress in the brain is functionally linked to elevations in AP and RSNA and that increases in circulating Ang II cause ER stress in the SFO. To determine whether Ang II–induced ER stress in the SFO plays a causal role in the development of HTN, we utilized a genetic approach to relieve ER stress selectively in SFO. Supplementation of ER chaperones such as GRP78 is an effective way to abrogate ER stress in vivo (16). Accordingly, we developed an adenoviral vector expressing the full-length cDNA of mouse GRP78, including its ER retention signal (AdGRP78; Supplemental Figure 1A; supplemental material available online with this article; doi: 10.1172/JCI64583DS1). Infection of Neuro2A cells with AdGRP78 increased Grp78 mRNA in a concentration-dependent manner, and double immunocytochemistry confirmed GRP78 localization to the ER of these cells (Supplemental Figure 1, B and C). Infection of Neuro2A cells with AdGRP78 also prevented TG-induced increases in p58IPK mRNA compared with control virus–treated cells (Supplemental Figure 1D). Finally, targeting of AdGRP78 to the SFO in vivo prevented the increase in Chop mRNA in this brain region caused by ICV injection of TG (Supplemental Figure 1D).
Having established the potency and efficacy of AdGRP78 in reducing ER stress in vitro and in vivo, we tested whether SFO-specific supplementation of GRP78 with AdGRP78 prior to Ang II infusions would prevent the development of HTN. Mice underwent implantation of radiotelemeters and SFO-targeted microinjection of AdGRP78 or a control vector (AdLacZ) (7, 17). One week was allowed for recovery and maximal transgene expression before systemic infusions of Ang II began. As shown in Figure 3A, mice with SFO-targeted AdLacZ demonstrated the typical progressive and robust increase in AP over 2 weeks as reported previously (7) and shown in Figure 1C. In contrast, SFO-targeted AdGRP78 prevented the development of Ang II–induced HTN (Figure 3A). Immunocytochemistry and real-time PCR confirmed robust expression of GRP78 in SFO (Supplemental Figure 2). In addition, AdGRP78 prevented upregulation of ER stress biomarkers in SFO at day 7 (p58IPK fold-day 0: 1.46 ± 0.19 vs. 0.44 ± 0.07; AdLacZ vs. AdGRP78, P < 0.05, n = 4) and day 14 (Chop fold-day 0: 1.67 ± 0.16 vs. 1.11 ± 0.16; AdLacZ vs. AdGRP78, P < 0.05, n = 4) of Ang II infusion. Furthermore, as demonstrated previously using this SFO-targeted gene transfer approach (7), GRP78 expression was absent or negligible in all other brain regions (Supplemental Figure 2B). This demonstrates that ER stress in the SFO is a key underlying mechanism of Ang II–dependent HTN.
Figure 3. Genetic relief of ER stress selectively in the SFO prevents Ang II–induced HTN and ROS production.
An adenovirus encoding the ER molecular chaperone GRP78 was targeted to SFO 1 week prior to the start of systemic Ang II infusions. (A) Mean AP measured by radiotelemetry during Ang II infusions in conscious mice with SFO-targeted AdGRP78 or control vector AdLacZ (n = 4–5). (B) Schematic of a coronal brain section containing the SFO (lower left) and representative DHE fluorescence images of SFO from untreated mice or from mice with SFO-targeted injections of AdLacZ or AdGRP78. Summary data are shown on the bottom right (n = 4). Scale bar: 50 μm. *P < 0.05 versus day 0 or untreated; †P < 0.05 versus AdLacZ.
Ang II–induced oxidant stress in the SFO is linked to ER stress.
Redox signaling in the SFO mediates Ang II HTN (7), and ER stress and oxidant stress are tightly coupled mechanisms (18). Thus, we examined whether ER stress is linked to oxidative stress in the SFO during Ang II HTN. Ang II caused a significant increase in ROS production in freshly dissociated murine SFO cells when dihydroethidium (DHE) was used as an indicator (7), and this was prevented by pretreatment with TUDCA (Supplemental Figure 3). Furthermore, in situ DHE microfluorography in brain sections revealed that SFO-targeted AdGRP78 abolished the approximately 2-fold increase in DHE fluorescence intensity in SFO induced by 2 weeks systemic Ang II infusion observed in AdLacZ-treated mice (Figure 3B). These findings suggest that Ang II–induced ER stress is a source of SFO oxidative stress in this model of HTN.
Summary.
We provide the first evidence to our knowlege that ER stress, notably brain ER stress, plays a key causative role in the pathogenesis of chronic HTN. Our data point to the importance of ER stress in the circumventricular SFO in the Ang II infusion HTN model. However, these findings could have broad implications for understanding the mechanisms of different forms of HTN, including spontaneous and genetic forms of the disease.
Methods
Detailed Supplemental Methods are available online with this article.
Statistics.
Data are expressed as mean ± SEM and analyzed by 2-tailed unpaired t test or ANOVA. Post-hoc comparisons were performed using Tukey’s test. The α level was set at P < 0.05.
Study approval.
Care of the mice met standards set forth by the NIH Guide for the Care and Use of Laboratory Animals (publication no. 85-23. Revised 1985). All procedures were approved by the IACUC of Cornell University and the University of Iowa.
Supplementary Material
Acknowledgments
This work was supported by NIH grants HL63887, HL84624, HL96571, and HL84207 and an American Physiological Society Fellowship (to C.N. Young); and an American Heart Association Fellowship (10POST3450044) (to X. Cao).
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2012;122(11):3960–3964. doi:10.1172/JCI64583.
See the related Commentary beginning on page 3859.
References
- 1.Ron D, Walter P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat Rev Mol Cell Biol. 2007;8(7):519–529. doi: 10.1038/nrm2199. [DOI] [PubMed] [Google Scholar]
- 2.Schroder M, Kaufman RJ. The mammalian unfolded protein response. Annu Rev Biochem. 2005;74:739–789. doi: 10.1146/annurev.biochem.73.011303.074134. [DOI] [PubMed] [Google Scholar]
- 3.Scheuner D, Kaufman RJ. The unfolded protein response: a pathway that links insulin demand with beta-cell failure and diabetes. Endocr Rev. 2008;29(3):317–333. doi: 10.1210/er.2007-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hotamisligil GS. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell. 2010;140(6):900–917. doi: 10.1016/j.cell.2010.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman MC, Davisson RL. Redox signaling in central neural regulation of cardiovascular function. Prog Biophys Mol Biol. 2004;84(2–3):125–149. doi: 10.1016/j.pbiomolbio.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman MC, Lazartigues E, Sharma RV, Davisson RL. Hypertension caused by angiotensin II infusion involves increased superoxide production in the central nervous system. Circ Res. 2004;95(2):210–216. doi: 10.1161/01.RES.0000135483.12297.e4. [DOI] [PubMed] [Google Scholar]
- 8.Ferguson AV. Angiotensinergic regulation of autonomic and neuroendocrine outputs: critical roles for the subfornical organ and paraventricular nucleus. Neuroendocrinology. 2009;89(4):370–376. doi: 10.1159/000211202. [DOI] [PubMed] [Google Scholar]
- 9.Purkayastha S, Zhang H, Zhang G, Ahmed Z, Wang Y, Cai D. Neural dysregulation of peripheral insulin action and blood pressure by brain endoplasmic reticulum stress. Proc Natl Acad Sci U S A. 2011;108(7):2939–2944. doi: 10.1073/pnas.1006875108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simon G, Abraham G, Cserep G. Pressor and subpressor angiotensin II administration. Two experimental models of hypertension. Am J Hypertens. 1995;8(6):645–650. doi: 10.1016/0895-7061(95)00047-S. [DOI] [PubMed] [Google Scholar]
- 11.Ozcan U, et al. Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science. 2006;313(5790):1137–1140. doi: 10.1126/science.1128294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ozcan L, et al. Endoplasmic reticulum stress plays a central role in development of leptin resistance. Cell Metab. 2009;9(1):35–51. doi: 10.1016/j.cmet.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Zhang LH, Yang XL, Zhang X, Cheng JX, Zhang W. Association of elevated GRP78 expression with increased astrocytoma malignancy via Akt and ERK pathways. Brain Res. 2011;1371:23–31. doi: 10.1016/j.brainres.2010.11.063. [DOI] [PubMed] [Google Scholar]
- 14.Back SH, et al. Translation attenuation through eIF2alpha phosphorylation prevents oxidative stress and maintains the differentiated state in beta cells. Cell Metab. 2009;10(1):13–26. doi: 10.1016/j.cmet.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang L, Xue Z, He Y, Sun S, Chen H, Qi L. A Phos-tag-based approach reveals the extent of physiological endoplasmic reticulum stress. PLoS One. 2010;5(7):e11621. doi: 10.1371/journal.pone.0011621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kammoun HL, et al. GRP78 expression inhibits insulin and ER stress-induced SREBP-1c activation and reduces hepatic steatosis in mice. J Clin Invest. 2009;119(5):1201–1215. doi: 10.1172/JCI37007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butz GM, Davisson RL. Long-term telemetric measurement of cardiovascular parameters in awake mice: a physiological genomics tool. Physiol Genomics. 2001;5(2):89–97. doi: 10.1152/physiolgenomics.2001.5.2.89. [DOI] [PubMed] [Google Scholar]
- 18.Malhotra JD, Kaufman RJ. Endoplasmic reticulum stress and oxidative stress: a vicious cycle or a double-edged sword? Antioxid Redox Signal. 2007;9(12):2277–2293. doi: 10.1089/ars.2007.1782. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.