Abstract
Ovarian endometriosis can transform into malignant tumors, and ovarian carcinomas relatively frequently contain foci of endometriosis. In this study, the author reviewed 15 cases of endometrioid adenocarcinoma of the ovary in the last 15 years of our pathology laboratory in search for the presence of endometriosis within the tumor. Six (40%) of the 15 endometrioid adenocarcinoma were found to have endometriosis in the tumor. All of the endometriosis were atypical. The age of the 6 patients ranged from 44 year to 78 year with a median of 59 years. Grossly, the endometrial adenocarcinomas with endometriosis were characterized by unilocular cystic tumors in 5 cases and multilocular cystic tumor in one case. Histologically, the grade of endometrioid carcinoma was grade I in 3 cases, grade II in 2 cases and grade III in 1 case. Endometriosis was mixed with the tumors or was present adjacent to the tumor. The endometriosis was composed of a layer of atypical epithelium (atypical endometriosis), and gradual merges between endometriosis and carcinoma were present in 3 cases. These findings suggest that atypical endometriosis can transform into endometrioid carcinoma.
Keywords: Endometrioid adenocarcinoma, ovary, atypical endometriosis, transform
Introduction
It is well recognized that malignant transformation can occur in ovarian endometriosis [1,2]. Nishida et al. [2] reported that one case of ovarian carcinoma was recognized in the 147 cases of the ovarian endometriosis; thus the incidence of malignancy in ovarian endometriosis is 0.7%. Two of the most common malignant tumors of such a situation were clear cell adenocarcinoma and endometrioid adenocarcinoma [3]. A few studies showed that endometriosis was seen within endometrioid adenocarcinoma in 14% [4], 26% [5], 39% [6], and 43% [7]. The author herein reports 6 cases of endometrioid adenocarcinoma arising from endometriosis.
Materials and methods
The author reviewed 15 cases of endometrioid adenocarcinoma of the ovary in the last 15 years of our pathology laboratory for the presence of endometriosis within the tumor.
Results
Six (40%) of the 15 endometrioid adenocarcinoma were found to have endometriosis in the tumor. All of the endometriosis was atypical endometriosis. The age of the five patients ranged from 44 year to 78 year with a median of 59 years.
Grossly, the endometrial adenocarcinomas with endometriosis were characterized by unilocular cystic tumors (Figure 1) in 5 cases and a multilocular cystic tumor in one case. Within the cysts, single or multiple nodules were noted in the inner surfaces (Figure 1). The remaining is smooth flat lesions. The outer surface is smooth and free from tumors. Histologically, the nodules within the cystic tumors were endometrioid adenocarcinomas. The grade of endometrioid carcinoma was grade I in 3 cases, grade II in 2 cases (Figure 2) and grade III in 1 case. In the inner flat lesion consisted of atypical endometriosis (Figure 3). Endometriosis was mixed with the tumors or was present adjacent to the tumor (Figure 4). The atypical endometriosis was composed of a layer of atypical epithelium not regarded as malignant (Figure 5), and gradual merges between the endometriosis and carcinoma were present in 3 cases (Figure 6). In one case, the endometriosis was also present in the outer surface (Figure 7).
Figure 1.
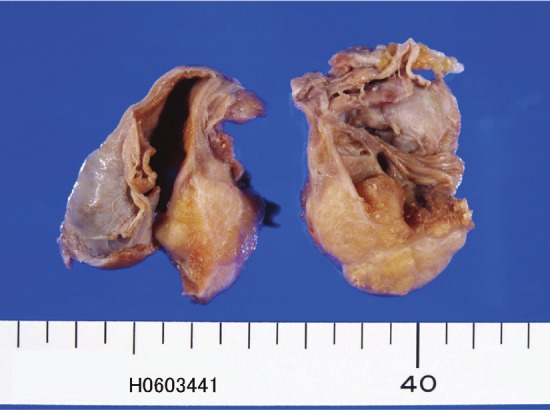
Gross features of endometrioid adenocarcinoma associated with endometriosis of the ovary. A unilocular cyst contain inner nodules (carcinoma) is seen. The inner flat areas are also recognized (endometriosis).
Figure 2.
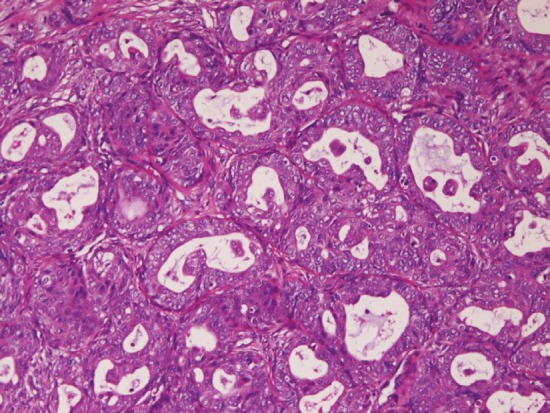
Histopathology of endometrioid adenocarcinomaassociated with endometriosis. HE, x100.
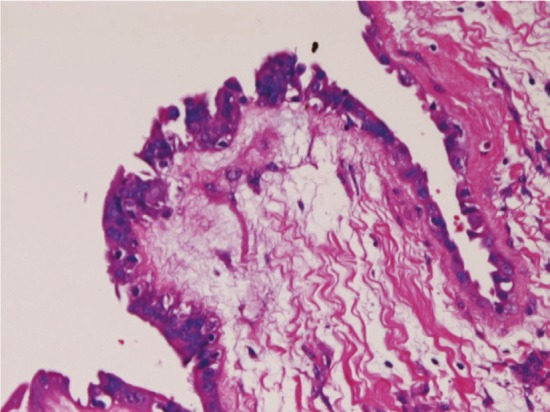
Figure 3.
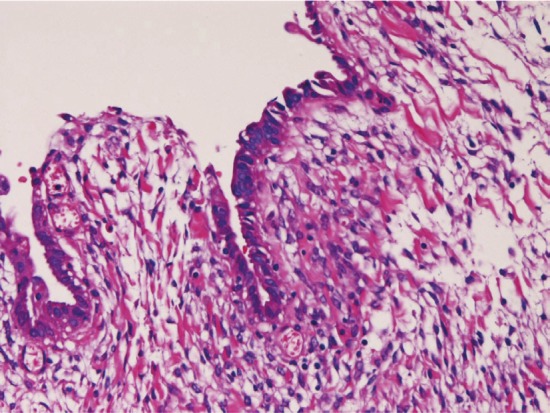
An area of atypical endometriosis. It is composedof a layer of atypical epithelium not regardedas malignancy. HE, x100.
Figure 4.
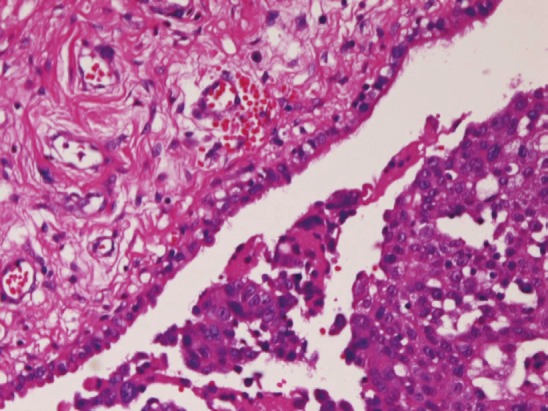
Atypical endometriosis (left) is seen nearthe inner endometrioid adenocarcinoma cells. HE,x100.
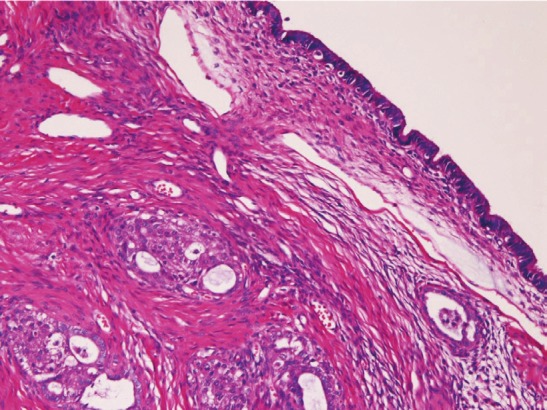
Figure 5.
Atypical endometriosis. The cell showsatypia not regarded as carcinoma. HE, x100.
Figure 6.
There is a gradual merge between atypicalendometriosis (upper) and carcinoma cells (lower).HE, x100.
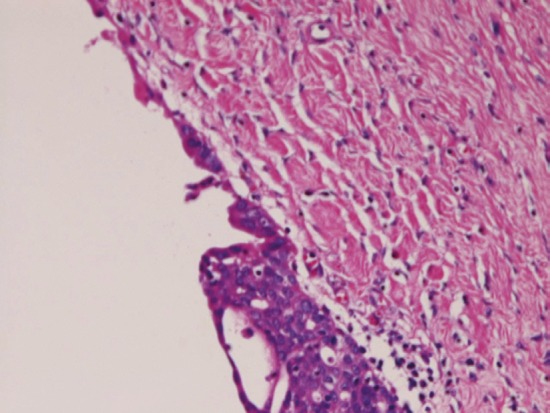
Figure 7.
In this case, endometriosis is present in theouter surface. HE, x100.
Discussion
Malignant transformation of endometriosis is rare but occurs in 0.7%, according to the data of Nishida et al [2]. They found 1 case of ovarian malignancy of the 147 cases of ovarian endometriosis. On the other hand, Stern et al [8] showed that the incidence of endometriosis was 5% of ovarian malignancies associated with ovarian endometriosis. The most common malignancies arising in endometriosis of the ovary is endometrioid adenocarcinoma and clear cell adenocarcinoma. According to Yoshikawa et al [3], malignancies in endometriosis are clear cell (39.2%), endometrioid (21.2%), serous (3.3%), and mucinous type (3.0%). In endometrioid adenocarcinoma, the frequency of endometriosis is reported to be 3/22, 14% [4], 11/42, 26% [5], 9/23 39% [6], and 3/7, 43% [7]. In the present study, the incidence was 6/15 (40%).
The ovarian endometriosis is classified into typical and atypical endometriosis based on the cellular atypia. The atypical endometriosis has a close association with ovarian epithelial malignancies [9]. Ogawa et al [7] reported that endometriosis associated with ovarian malignancies was typical endometriosis in 35 cases and atypical endometriosis in 29 cases. In the present 6 cases, all the 6 cases were of atypical endometriosis, suggesting that atypical endometriosis is closely associated with the development of endometrioid adenocarcinoma. In the present study, gradual merges between atypical endometriosis and carcinoma cells were recognized, suggesting that the atypical endometriosis develop into endometrioid carcinoma after initiation and promotion. The author speculates that an endometrial cyst develops in the ovary. Its epithelium undergoes initiation, thus giving rise to atypical endometriosis consisting of dysplastic or intraepithelial neoplastic epithelium. The atypical epithelium ultimately leads to endometrioid adenocarcinoma showing an unilocular cyst or multilocular cyst with foci of atypical endometriosis.
The pathogenesis of endometriosis-associated ovarian malignancies is unknown. Recent studies have suggested the role of PTEN and hepatocyte nuclear factor-1β [10,11]. P53, bcl-2, cyclin D-1, c-erbB2, and chromosomal genetic alterations may play a role in the development of ovarial carcinomas from endometriosis [12].
In summary, the present findings suggest that atypical endometriosis transforms into endometrioid carcinoma.
Conflict of interest statement
The author has no conflict of interest.
References
- 1.Scully RE, Richardson GS, Barlow JF. The development of malignancy in endometriosis. Clin Obstet Gynecol. 1966;9:384–411. doi: 10.1097/00003081-196606000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Nishida M, Watanabe K, Sato N, Ichikawa Y. Malignant transformation of ovarian endometroosis. Gynecol Obstet Invest. 2000;50(Suppl 1):18–25. doi: 10.1159/000052874. [DOI] [PubMed] [Google Scholar]
- 3.Yoshikawa H, Jimbo H, Okada S, Matsumoto K, Onda T, Yasugi T, Taketani Y. Prevalence of endometriosis in ovarian cancer. Gynecol Obstet Invest. 2000;50(supple 1):11–17. doi: 10.1159/000052873. [DOI] [PubMed] [Google Scholar]
- 4.Valezuela P, Ramos P, Redondo S, Cabrera Y, Alvarez I, Ruiz A. Endometrioid adenocarcinoma of the ovary and endometriosis. Eur J Obstet Gynecol Reprod Biol. 2007;134:83–86. doi: 10.1016/j.ejogrb.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 5.DePriest PD, Banks ER, Powell DE, van Nagell JR, Gallion HH, Puls LE, Hunter JE, Kryscio RJ, Royalty MB. Endometrioid adenocarcinoma of the ovary and endometriosis: the association in postmenopausal women. Gynecol Oncol. 1992;47:71–75. doi: 10.1016/0090-8258(92)90079-x. [DOI] [PubMed] [Google Scholar]
- 6.Sainz de la Cuesta R, Eichhorn JH, Rice LW, Fuller AF, Nikrui N, Goff BA. Histological transformation of benign endometriosis to early epithelial ovarian cancer. Gynecol Oncol. 1996;60:238–244. doi: 10.1006/gyno.1996.0032. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa S, Kaku T, Amada S, Kobayashi H, Hirakawa T, Ariyoshi K, Kamura T, Nakano H. Ovarian endometoriosis associated with ovarian carcinoma: a clinicopathologic and immunohistochemical study. Gynecol Oncol. 2000;77:298–304. doi: 10.1006/gyno.2000.5765. [DOI] [PubMed] [Google Scholar]
- 8.Stern RC, Dash R, Bentley RC, Snyder MJ, Haney AF, Robboy SJ. Malignancy in endometriosis: frequency and comparison of ovarian and extraovarian types. Int J Gynecol Pathol. 2001;20:133–139. doi: 10.1097/00004347-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Fukunaga M, Nomura K, Ishikawa E, Ushigome S. Ovarian atypical endometriosis; its close association with malignant epithelial tumours. Histopathology. 1997;30:248–255. doi: 10.1046/j.1365-2559.1997.d01-592.x. [DOI] [PubMed] [Google Scholar]
- 10.Obata K, Hoshian H. Common genetic change between endometriosis and ovarian cancer. Gynecol Obstet Invest. 2000;50(Suppl 1):39–43. doi: 10.1159/000052877. [DOI] [PubMed] [Google Scholar]
- 11.Kato N, Sasou S, Motoyama T. Expression of hepatocyte nuclear factor-1beta (HNF-1beta) in clear cell tumors and endometriosis of the ovary. Mod Pathol. 2006;19:83–89. doi: 10.1038/modpathol.3800492. [DOI] [PubMed] [Google Scholar]
- 12.Mhawech P, Kinkel K, Viastos G, Pelte MF. Ovarian carcinomas in endometriosis: an immunohistochemical and comparative genomic hydridization study. Int J Gynecol Pathol. 2002;21:401–406. doi: 10.1097/00004347-200210000-00010. [DOI] [PubMed] [Google Scholar]


