Abstract
Oncocytic lipoadenoma is a rare salivary gland tumour composed of adipose tissue and oncocytic epithelial cells in varied proportions. This tumour is still not included in the current WHO classification of salivary gland neoplasms. We herein report a further case of oncocytic lipoadenoma originating in the parotid gland of a 55-year-old woman. The tumour presented as a slowly growing asymptomatic left-sided parotid gland mass. The resected tumour measured 2.7 cm in maximum diameter and was composed of oncocytoma-like epithelial component admixed with mature adipocytes that made up 10% of the whole mass. Foci of sebaceous differentiation were seen. This rare variant of lipomatous salivary gland tumours is in need of more recognition and should be distinguished from other fat-containing salivary gland lesions, particularly lipomatous pleomorphic adenoma and myoepithelioma.
Keywords: Salivary gland tumours, oncocytes, sialolipoma, lipoadenoma
Introduction
Sialolipoma is a relatively new and uncommon type of benign salivary gland tumours that found a place in the WHO classification of salivary gland tumours only in 2005 [1]. The term sialolipoma was suggested by Nagao [2] in 2001, who reported a series of 7 salivary gland tumours, well circumcised and comprised of mature adipose elements, as well as glandular tissue, which closely resembled the cellular and structural composition of normal salivary glands. Since the tumour’s original description, around 35 cases of sialolipoma have been reported in the English and German literature [2-22] (Table 1). However, the variant composed chiefly of oncocytic cells is quite rare and still is not included in the current WHO classification of salivary gland tumours. This variant has been most commonly referred to as oncocytic lipoadenoma. Here we present a case of oncocytic lipoadenoma of the parotid gland and attempt to review the relevant literature.
Table 1.
Summary of the reported cases of sialolipoma/lipoadenoma in the literature
| Case No | Author | Year | Age in years | Sex | Site | Size ( mm) | Fatty Tissue % | Oncocytic Metaplasia |
|---|---|---|---|---|---|---|---|---|
| 1 | Nagao | 2001 | 20 | M | Parotid | 35x30x22 | 90 | No |
| 2 | Nagao | 2001 | 45 | F | Parotid | 60x30x20 | 90 | No |
| 3 | Nagao | 2001 | 67 | M | Parotid | 17x17x17 | 90 | No |
| 4 | Nagao | 2001 | 66 | F | Parotid | max 60 | 90 | Yes |
| 5 | Nagao | 2001 | 42 | M | Parotid | max 60 | 90 | No |
| 6 | Nagao | 2001 | 66 | M | Soft Palate | 22x15x15 | 50 | No |
| 7 | Nagao | 2001 | 75 | M | Hard Palate | max 10 | 50 | No |
| 8 | Fregnani | 2003 | Tongue | No | ||||
| 9 | Fregnani | 2003 | Buccal Mucosa | No | ||||
| 10 | Hornigold | 2003 | 0 | F | Parotid | 35x26x17 | No | |
| 11 | Lin | 2004 | 67 | F | Floor of Mouth | 30x20 | No | |
| 12 | Michaelides | 2006 | 44 | M | Parotid | max 35 | No | |
| 13 | Sakai | 2006 | 60 | F | Hard Palate | 18x12x10 | No | |
| 14 | Kadivar | 2007 | 3 | F | Parotid | max 30 | No | |
| 15 | Bansal | 2007 | 11 | M | Parotid | max 70 | No | |
| 16 | Ramer | 2007 | 84 | F | Buccal Mucosa | 14x10x10 | No | |
| 17 | Ramer | 2007 | 43 | F | Soft Palate | 20x20x20 | No | |
| 18 | Ponniah | 2007 | 60 | M | Floor of Mouth | max 20 | No | |
| 19 | Parente | 2008 | 77 | F | Submandibular | 30x20x18 | 80 | Yes |
| 20 | Pusiol | 2009 | 73 | M | Submandibular | max 20 | 80 | Yes |
| 21 | Okada | 2009 | 66 | F | Hard Palate | 20x16x10 | 40 | Yes |
| 22 | Dogan | 2009 | 33 | M | Parotid | 26x21x17 | No | |
| 23 | Jang | 2009 | 62 | F | Submandibular | Yes | ||
| 24 | Fritzsche | 2009 | 43 | M | Parotid | 65x50x20 | Yes | |
| 25 | Sato | 2010 | 32 | M | Submandibular | 40x30 | No | |
| 26 | de Moraes | 2010 | 72 | F | Hard Palate | 17x13x6 | No | |
| 27 | Nonaka | 2011 | 27 | F | Tongue | max 10 | 50 | No |
| 28 | Nonaka | 2011 | 73 | F | Floor of Mouth | 40x10 | 60 | No |
| 29 | Nonaka | 2011 | 65 | F | Buccal Mucosa | max 20 | 60 | Yes |
| 30 | Nonaka | 2011 | 68 | F | Retromolar | max 9 | 60 | Yes |
| 31 | Akrish | 2011 | 52 | M | Submandibular | 35x20x15 | Yes | |
| 32 | Akrish | 2011 | 67 | F | Hard Palate | 50x40x40 | No | |
| 33 | Kidambi | 2012 | 0 | M | Parotid | 45x30x45 | 50 | No |
| 34 | This report | 2012 | 55 | F | Parotid | 27x24x18 | Yes |
Case report
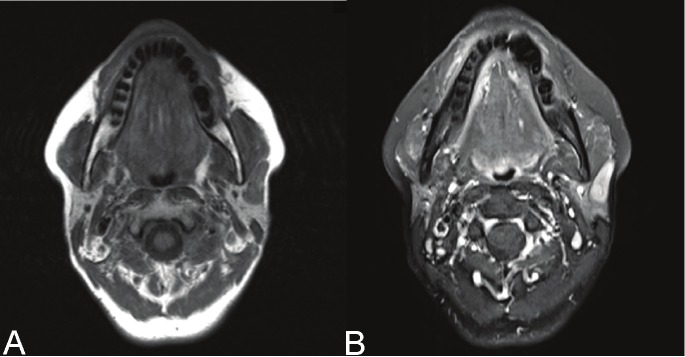
A 55-year old female patient presented to our Outpatient Department with a slowly progressing asymptomatic swelling of the left parotid region. The patient has noticed the swelling two months before and reported that it has gradually increased in size. The swelling did not fluctuate in size with eating. On examination, an approximately 20mm x 20mm round lesion was palpated in the left parotid region. The lesion was not mobile on palpation. There were no signs of inflammation. The salivary secretion from both the parotid glands was normal. A magnetic resonance tomography (MRT) was performed as the next step of the diagnostic procedure. A round, well defined, heterogeneous lesion with intermediate signal intensity in both T1 and T2 series was described (Figure 1A, B). The lesion was considered to be a parotid gland adenoma and a lateral parotidectomy was planned. The procedure was completed without any complications, fully preserving the function of the facial nerve. One year after the surgical removal of the tumour, there were no signs of recurrence.
Figure 1.
A, B : Magnetic Resonance Tomography imaging of the lesion: In both T1 and T2 a well defined, heterogeneous lesion with intermediate signal intensity could be depicted.
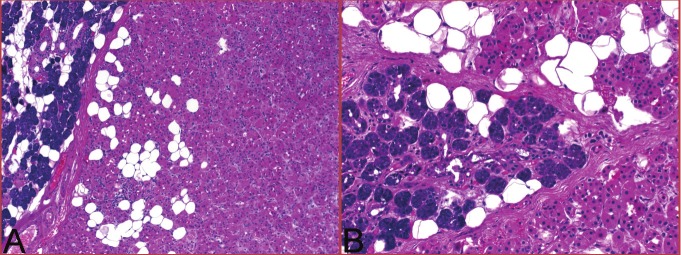
Pathological findings
The resected specimen contained an encapsulated tumour measuring 24 x 18 x 27 mm. Macroscopically the tumour was lobulated and whitish-brownish to yellow in appearance and was surrounded by a thin connective tissue capsule. Histological examination showed a predominance of large polygonal oncocytic cells arranged in large lobules separated by thin fibrous septa that occasionally contained residual normal serous acini (Figure 2A). The oncocytic component was associated with a variable fatty component that formed 10% of the tumor mass and occasionally predominated in small areas of the tumour (Figure 2B). Scattered small foci of sebaceous differentiation were seen between oncocytic cells and were commonly associated with ductal dilatation, chronic inflammation and periductal fibrosis. The tumour cells were monomorphic without evidence of atypia or mitotic activity. There was no perineural invasion, lymphovascular invasion or extracapsular infiltration by the tumour.
Figure 2.
Histological evaluation showed an encapsulated mass surrounded by normal parotid parenchyma and composed predominantly of oncocytic epithelial cells. The fatty component varied greatly from minor (A) to almost equally distributed component (B).
Discussion
Lipoma in general is a relatively common tumour of subcutaneous soft tissue. However, its occurrence in the salivary glands is rare. It has been noted that only approximately 0.5% of all salivary gland tumours are lipomas [1,23-27]. Lipoma is also quite rare in the oral cavity with a reported incidence of 1.1-4% of all benign oral cavity lesions [3,20,28]. Since Nagao [2] first described sialolipoma as a pathological entity in 2001, there have been so far 35 cases of sialolipoma (including the one we present) reported in the literature (summarized in Table 1). Although sialolipoma and oncocytic lipoadenoma still remain as rare tumours, increased awareness of these entities has resulted in increased number of reported cases during the last few years.
Sialolipomas present at wide age range with the youngest patient reported being 7 weeks old [4] and the oldest 84 years old [11]. Children were affected in 4 cases [4,7,9,22]; all of them represented congenital tumours. The mean age of presentation is 52 years. This benign tumour shows a slight predilection for females, with a male to female ratio of approximately 1:1.4.
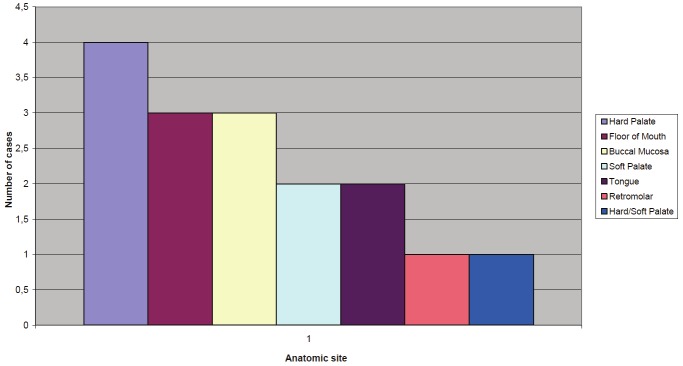
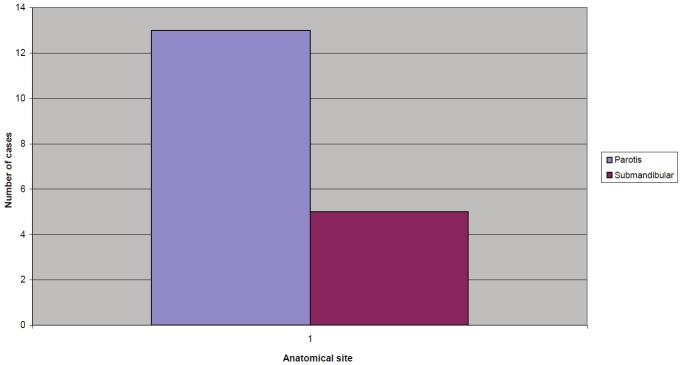
Both major and minor salivary glands can be affected but most lesions arise in the parotid gland. In this review we found an almost equal distribution of the tumour between major and minor salivary glands (16 cases localized in minor salivary glands, 18 in major salivary glands).
The parotid gland is the most common localisation of sialolipoma with 13 described cases (including the present case) [2,4,6,7,9,13,22]. The submandibular gland was involved in the other five cases affecting major salivary glands [12,15,17,19,21], whereas there has been so far no report of sublingual gland involvement. As far as minor salivary glands are concerned, the most common localisation of sialolipomas is the hard palate with 5 cases described [2,8,16,18,19], followed by the floor of the mouth [5,10,20] and the buccal mucosa [3,11,20] (3 cases each), the soft palate [2,11], the tongue [3,20] (2 reported cases each) and the retromolar region [20] (1 case) (Figure 3, 4).
Figure 3.
Distribution of minor salivary gland sialolipomas/lipoadenomas.
Figure 4.
Distribution of major salivary gland sialolipomas/lipoadenomas.
The majority of the patients presented with an asymptomatic mass or swelling in the respective site. The duration of symptoms varied greatly from 15 days to 11 years. Since many patients did not have any other complaints related to the tumour, there have been many cases where the tumour remained undiagnosed for many years, until it significantly increased in size.
Treatment has been surgical in all the reported cases. In the 13 cases where the tumour was localised in the lateral lobe of the parotid gland the treatment of choice was lateral parotidectomy in 9 of them, while local excision was performed in the other 4 cases. Therapy was local excision for all tumours at other sites. No case of recurrence has been reported so far.
The excised lesion was either spherical or oval in shape with sizes ranging from 0.9 to 7 cm (mean size: 3.2 cm).
The histopathological description of reported sialolipomas was consistent with the original description by Nagao [2]. The tumor is always encapsulated and consisted of mature adipose tissue with islets of epithelial salivary gland cells with the normal ductuloacinar structure of a salivary gland.
The amount of fatty tissue ranges in the 14 cases where this information was provided between 40 and 90% with a mean value of 68.7 %. No atypia of the epithelial element was noticed in any case. Atrophy of the glandular elements is also a common finding. Other findings that were reported were ductal ectasia, periductal fibrosis, inflammatory cell infiltrate, oncocytic ductal metaplasia and myxoid change [16]. The low staining for Ki67 reflects a low proliferative activity.
However, our case was composed of 90% oncocytes thus justifying its characterization as “oncocytic lipoadenoma”. The presence of oncocytic metaplasia is mentioned in 10 of previously reported cases [2,12,14-17,19,20]. Pusiol et al [17] characterized oncocytic metaplasia in a sialolipoma as “uncommon but not unexpected” and proposed the use of the term “oncocytic sialolipoma”. However, it still remains unclear, if the non-oncocytic sialolipoma and the oncocytic lipoadenoma represent different manifestations of the same disease process.
Regarding the pathogenesis of the lesion, Nagao [2] suggested that the glandular component had become entrapped during lipomatous proliferation and believed that it was not of neoplastic origin. This is why he suggested the term sialolipoma, to signify that the tumor is a type of lipoma and not of hamartomatous origin. Interestingly, in one case reported by Parente et al [12], a disorganized proliferation of neural and vascular structures was noticed, which led the authors to suggest that sialolipoma might be of hamartomatous origin. Akrish et al [19] disregarded Parente’s suggestion of hamartomatous nature and proposed the hypothesis that a dysfunction of a salivary gland, leading to a modification of the normal gland function underlies the formation of this tumour. To support this hypothesis Akrish et al referred to clinical characteristics such as the complete absence of recurrence capacity, the prolonged natural history of the lesion, as well as histopathological features like the noted duct ectasia, periductal fibrosis, oncocytic metaplasia, the replacement of glandular tissue with mature adipose tissue as well as the inflammatory infiltrates.
The clinical differential diagnosis should include all the benign salivary gland lesions. A CT can give hints regarding the presence of a lipoma, since a density of 50-150 Hounsefield Units is typical for such a tumour [13]. MRT may also suggest diagnosis and allows for assessment of fatty and non-fatty components.
In the histopathological differential diagnosis of the sialolipoma and oncocytic lipoadenoma, lipomatosis, and pleomorphic adenoma with lipometaplasia should be included. Pleomorphic adenoma can be excluded by the presence of normal salivary tissue. In contrast to sialolipoma, oncocytic lipoadenoma is characterized by lack of predominant organoid salivary gland elements and paucity or absence of normal ductuloacinic structures [3,15,18,29]. Microscopic differential diagnosis of sialolipoma should include also myoepithelioma and other salivary gland lesions with extensive lipometaplasia [11]. Lipomatosis is characterized by intensive shrinkage of acinar cells and it is a variant of interstitial lipomatosis [15,30]. Sialolipoma has a distinct enlarged main mass, which helps its separation from lipomatosis. Fibrolipoma, the second most common oral lipoma contains also mature adipose tissue [29]. However, in this case there exist no identifiable salivary elements, the fat tissue being contained within dense connective tissue.
Spindle cell lipoma is another lesion that needs to be distinguished from sialolipoma. It may affect the parotid region and present typically as a well-circumscribed fatty tumour with bland spindle cells, ropey collagen, and adipocytes [29].
In conclusion, oncocytic lipoadenoma is probably not as uncommon as was initially believed and this entity should be included in the differential diagnosis of slow growing mass of the salivary glands. Although oncocytic metaplasia has been recognized in several of the reported sialolipomas, we believe that the term “oncocytic sialolipoma” is more appropriate for oncocyte-predominant lesions.
References
- 1.Barnes L, Everson JW, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. World Health Organization classifica tion of tumours; p. 275. [Google Scholar]
- 2.Nagao T, Sugano I, Ishida Y, Asoh A, Munakata S, Yamazaki K, Konno A, Kondo Y, Nagao K. Sialolipoma: A report of seven cases of a new variant of salivary gland lipoma. Histopathology. 2001;38:30. doi: 10.1046/j.1365-2559.2001.01054.x. [DOI] [PubMed] [Google Scholar]
- 3.Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipoma of oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2003;32:49–53. doi: 10.1054/ijom.2002.0317. [DOI] [PubMed] [Google Scholar]
- 4.Hornigold R, Morgan PR, Pearce A, Gleeson MJ. Congenital sialolipoma of the parotid gland first reported case and review of the literature. International Journal of Pediatric Otorhinolaryngology. 2005;69:429–434. doi: 10.1016/j.ijporl.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Lin YJ, Lin LM, Chen YK, Shen YH, Hsue SS, Wang WC, Lin CC. Sialolipoma of the floor of the mouth: A case report. Kaohsiung J Med Sci. 2004;20:410. doi: 10.1016/S1607-551X(09)70178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michaelidis IG, Stefanopoulos PK, Sambaziotis D, Zahos MA, Papadimitriou GA. Sialolipoma of the parotid gland. J Craniomaxillofac Surg. 2006;34:43. doi: 10.1016/j.jcms.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Bansal B, Ramavat AS, Gupta S, Singh S, Sharma A, Gupta K, Mittal AK, Kudesia M. Congenital sialolipoma of parotid gland: a report of rare and recently described entity with review of literature. Pediatr Dev Pathol. 2007 May-Jun;10:244–6. doi: 10.2350/06-09-0170.1. [DOI] [PubMed] [Google Scholar]
- 8.Sakai T, Iida S, Kishino M, Okura M, Kogo M. Sialolipoma of the hard palate. J Oral Pathol Med. 2006;35:376. doi: 10.1111/j.1600-0714.2006.00409.x. [DOI] [PubMed] [Google Scholar]
- 9.Kadivar M, Shahzadi SZ, Javadi M. Sialolipoma of the parotid gland with diffuse sebaceous differentiation in a female child. Pediatr Dev Pathol. 2007 Mar-Apr;10:138–41. doi: 10.2350/06-05-0091.1. [DOI] [PubMed] [Google Scholar]
- 10.Ponniah I, Lavanya N, Suresh Kumar P. Island of salivary gland in adipose tissue: A report of three cases. J Oral Pathol Med. 2007;36:558. doi: 10.1111/j.1600-0714.2007.00544.x. [DOI] [PubMed] [Google Scholar]
- 11.Ramer N, Lumerman HS, Ramer Y. Sialolipoma: report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:809–813. doi: 10.1016/j.tripleo.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Parente P, Longobardi G, Bigotti G. Hamartomatous sialolipoma of the submandibular gland: Case report. Br J Oral Maxillofac Surg. 2008;46:599. doi: 10.1016/j.bjoms.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Doğan S, Can IH, Unlü I, Süngü N, Gönültaş MA, Samim EE. Sialolipoma of the parotid gland. J Craniofac Surg. 2009;20:847. doi: 10.1097/SCS.0b013e3181a2ef7d. [DOI] [PubMed] [Google Scholar]
- 14.Fritzsche FR, Bode PK, Stinn B, Huber GF, Noske A. Sialolipom der Glandula parotis. Pathologe. 2009;30:478–480. doi: 10.1007/s00292-009-1233-1. [DOI] [PubMed] [Google Scholar]
- 15.Jang YW, Kim SG, Pai H, Park JW, Lee YC, Rotaru H. Sialolipoma: A case report and review of 27 cases. Oral Maxillofac Surg. 2009;13:109. doi: 10.1007/s10006-009-0153-9. [DOI] [PubMed] [Google Scholar]
- 16.Okada H, Yokoyama M, Hara M, Akimoto Y, Kaneda T, Yamamoto H. Sialolipoma of the palate: A rare case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:571. doi: 10.1016/j.tripleo.2009.05.045. [DOI] [PubMed] [Google Scholar]
- 17.Pusiol T, Franceschetti I, Scialpi M, Piscioli I. Oncocytic sialolipoma of the submandibular gland with sebaceous differentiation: a new pathological entity. Indian J Pathol Microbiol. 2009 Jul-Sep;52:379–82. doi: 10.4103/0377-4929.55000. [DOI] [PubMed] [Google Scholar]
- 18.de Moraes M, de Matos FR, de Carvalho CP, de Medeiros AM, de Souza LB. Sialolipoma in minor salivary gland: case report and review of the literature. Head Neck Pathol. 2010 Sep;4:249–52. doi: 10.1007/s12105-010-0187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akrish S, Leiser Y, Shamira D, Peled M. Sialolipoma of the salivary gland: two new cases, literature review and histogenetic hypothesis. J Oral Maxillofac Surg. 2011 May;69:1380–4. doi: 10.1016/j.joms.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 20.Nonaka CF, Pereira KM, de Andrade Santos PP, de Almeida Freitas R, da Costa Miguel MC. Sialolipoma of minor salivary glands. Ann Diagn Pathol. 2011 Feb;15:6–11. doi: 10.1016/j.anndiagpath.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Sato K, Gotoh C, Uchida H, Kawashima H, Yoshida M, Kitano Y, Kishimoto H. Sialolipoma of the submandibular gland in a child. J Pediatr Surg. 2011 Feb;46:408–10. doi: 10.1016/j.jpedsurg.2010.09.097. [DOI] [PubMed] [Google Scholar]
- 22.Kidambi T, Been MJ, Maddalozzo J. Congenital sialolipoma of the parotid gland: presentation, diagnosis, and management. Am J Otolaryngol. 2012 Mar;33:279–81. doi: 10.1016/j.amjoto.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 23.Samuels HS, Oatis GW Jr. Lipoma of the hard palate. Oral Surg Oral Med Oral Pathol. 1969;28:134–136. doi: 10.1016/0030-4220(69)90210-2. [DOI] [PubMed] [Google Scholar]
- 24.Walts AE, Perzik SL. Lipomatous lesions of the parotid area. Arch Otolaryngol. 1976;102:230–232. doi: 10.1001/archotol.1976.00780090072010. [DOI] [PubMed] [Google Scholar]
- 25.Baker SE, Jensen JL, Correll RW. Lipomas of the parotid gland. Oral Surg Oral Med Oral Pathol. 1981;52:167–171. doi: 10.1016/0030-4220(81)90315-7. [DOI] [PubMed] [Google Scholar]
- 26.Miles DA, Langlais RP, Aufdemorte TB, Glass BJ. Lipoma of the soft palate. Oral Surg Oral Med Oral Pathol. 1984;57:77–80. doi: 10.1016/0030-4220(84)90266-4. [DOI] [PubMed] [Google Scholar]
- 27.Houston GD, Brannon RB. Lipoma of the parotid gland. Oral Surg Oral Med Oral Pathol. 1985;60:72–74. doi: 10.1016/0030-4220(85)90219-1. [DOI] [PubMed] [Google Scholar]
- 28.Lombardi T, Odell EW. Spindle cell lipoma of the oral cavity: report of a case. J Oral Pathol Med. 1994;23:237–9. doi: 10.1111/j.1600-0714.1994.tb01120.x. [DOI] [PubMed] [Google Scholar]
- 29.Furlong MA, Fanburg-Smith JC, Childers EL. Lipoma of the oral and maxillofacial region: site and subclassification of 125 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:441–450. doi: 10.1016/j.tripleo.2004.02.071. [DOI] [PubMed] [Google Scholar]
- 30.Seifert G. Lipomatose cystische Pankreasfibrose und lipomatose Parotisatrophie. Beitr Pathol Anat. 1959;121:64–80. [PubMed] [Google Scholar]