Abstract
Introduction
Early tracheal extubation is a common goal after cardiac surgery. Our study aims to examine whether timing of tracheal extubation predicts improved postoperative outcomes and late survival after cardiac surgery. We also evaluated the optimal timing of extubation and its association with better postoperative outcomes.
Methods
Between 2002 and 2006, 1164 patients underwent early tracheal extubation (<6 hours after surgery) and 1571 had conventional extubation (>6 hours after surgery). Propensity score adjustment and multivariable logistic regression analysis were used to adjust for imbalances in the patients’ preoperative characteristics. Receiver operating characteristic curves (ROC) were used to identify the best timing of extubation and improved postoperative outcomes. Cox regression analysis was used to identify whether early extubation is a risk factor for decreased late mortality.
Results
Results - Early extubation was associated with lower propensity score-adjusted rate of operative mortality (Odds Ratio =0.55, 95% Confidence Intervals =0.31-0.98, p=0.043). Extubation within 9 hours emerged as the best predictor of improved postoperative morbidity and mortality (sensitivity =85.5%, specificity =52.7%, accuracy =64.5%). Early extubation also predicted decreased late mortality (Hazard Ratio =0.45, 95% Confidence Intervals 0.31-0.67, p<0.001).
Conclusions
Early extubation may predict improved outcomes after cardiac surgery. Extubation within 9 hours after surgery was the best predictor of uncomplicated recovery after cardiac surgery. Those patients intubated longer than 16 hours have a poorer postoperative prognosis. Early extubation predicts prolonged survival up to 16 months after surgery.
Keywords: early extubation, coronary artery bypass, mortality
Introduction
Early tracheal extubation is a common goal of postoperative recovery after cardiac surgery. It is associated with decreased rates of pulmonary complications and decreased use of hospital resources [1,2,3,4,5,6,7,8]. Though many investigations have elucidated the value of early extubation after cardiac surgery, the optimal timing has not been determined.
This propensity-matched study was designed to evaluate optimal timing of early extubation and correlate timing of extubation with early and late outcomes.
Methods
The Division of Cardiothoracic Surgery at Carolinas Heart and Vascular Institute computerized database was utilized to identify all patients who had coronary artery bypass (CABG), isolated valve surgery, or valve/CABG combination at Carolinas Medical Center between January 2002 to December 2006; 2735 patients were thus identified. Of those, 1164 were extubated within six hours (early extubation group) and 1571 were extubated six hours or greater after surgery (conventional extubation group). The same group of cardiac surgeons performed all procedures. Data including baseline demographics, procedural data, and perioperative outcomes were entered prospectively in a pre-specified database by a dedicated data-coordinating center.
Standard research approval was obtained via our Institutional Review Board before data identification, analysis, and study approval was initiated. Health Insurance Portability and Accountability Act of 1996 regulations were followed at all times to maintain personal patient information confidentiality.
The Society of Thoracic Surgeons’ (STS) national cardiac database definitions were used for the purposes of the study. Early extubation is defined as removal of breathing tube <6 hours after arrival to cardiovascular intensive care unit (ICU). Pneumonia is defined as one of the following: positive cultures of sputum, blood, pleural fluid, empyema fluid, trans-tracheal fluid or transthoracic fluid; consistent with the diagnosis and clinical findings of pneumonia (may include chest x-ray diagnosis of pulmonary infiltrates). Pulmonary embolism is defined as diagnosis by study as V/Q scan or angiogram. Septicemia is defined as positive blood cultures post-operatively. Prolonged intensive care unit length of stay is greater than 24 hours. Prolonged hospital length of stay is defined as hospital stay more than the 75th percentile of hospital length of stay (>9 days). Reintubation is defined as reintubation for any reason during hospitalization. Operative Mortality is defined as operative death within 30 days of procedure. Cerebrovascular accident is defined as a central neurological deficit persisting for greater than 72 hours. Hemorrhage-related re-exploration is defined as operative re-intervention required for bleeding or tamponade. Renal failure is defined as an increase in serum creatinine greater than 2.0 mg/dl, and a doubling of creatinine over baseline preoperative value, and/or a new requirement for dialysis/hemofiltration.
Anesthesia and Intra-operative Management. Monitoring included electrocardiography, pulse oximetry, and end-tidal CO2 as well as routine use of pulmonary arterial and radial arterial catheters. Anesthetic induction and maintenance routinely included intravenous Fentanyl (10-20 micrograms/kg), Midazolam (5-10 mg), Propofol as necessary, and Pavulon (10-20 mg). Additionally, inhalational anesthesia was provided with Isoflurane. Anticoagulation with intravenous Heparin was achieved and maintained with the aid of the Hepcon Hemostasis Management System (Medtronic). Transesophageal echocardiography was routine.
Post-Operative Intensive Care Unit Management. Patients were brought to the ICU immediately after surgery and supported with mechanical ventilation, with goals of peak inspiratory pressures less than 30 cm H2O, pH 7.35-7.45, pO2 >80 and pCO2 <50. Bispectral index sedation monitoring (BIS) was utilized to assist the titration of propofol sedation (typically 0-50 mcg/kg/minute intravenously) as needed. A BIS value of 80 or greater was considered appropriate for extubation. Patients were warmed for goal temperature >36 °C. Inotropes, vasopressors, vasodilators, and volume were utilized as needed for goals of cardiac index >2.2, systemic venous oxygen saturations >65%, and systolic blood pressures from 100-120 mmHg (unless patient specific characteristics dictated otherwise). Post-operative volume of chest tube drainage, hemodynamics, temperature, urine output, blood products transfusion, and analgesics/sedation were recorded hourly and discussed between team members with early extubation being continuously considered. Patients were extubated when consistently hemodynamically stable, tolerating spontaneous breathing trial, hemostatic, and neurologically appropriate. Contraindications to extubation, without physician approval, included cardiac index <2.2 liters/min/M2, systolic blood pressure <90 or >160 mm Hg, heart rate >130, pO2 <80 or pCO2 >50 chest tube drainage >100 ml/hour, urine output <40 ml/hour, and a neurologic deficit. Statistical Analysis. Univariate comparisons of preoperative, operative, and postoperative variables were performed between groups (early extubation and conventional extubation group). Dichotomous variables were compared using a Fisher’s exact test and nonparametric variables were assessed with the Wilcoxon Rank Sum test. All tests were two-sided and p values 0.05 were considered statistically significant. All analyses were conducted using SAS (SAS Institute, Cary, NC). Propensity Score Adjustment. Propensity score adjustment was used on the postoperative outcomes to correct for imbalances between groups at baseline. A logistic regression model was created with early extubation/conventional extubation as the outcome and significant baseline characteristics (p<0.05) from the bivariate analysis as the covariates. Propensity scores were generated and included as regression (covariance) adjustments in each of the logistic regression outcome models [10]. The ability of the propensity score to effectively balance the compared groups at baseline was confirmed using separate logistic models with early-conventional extubation group type as the dependent variable and the covariate and propensity score as the independent variables. Multivariable Modeling. A multivariable, stepwise forward logistic regression analysis was used to determine independent predictors of
1) pneumonia,
2) sepsis,
3) prolonged ICU LOS,
4) prolonged hospital LOS,
5) readmission to the ICU,
6) reintubation,
7) cerebrovascular accident,
8) renal failure,
9) hemorrhage-related re-exploration,
10) operative mortality.
The criterion for variable entry and removal into the logistic models was a univariate probability level of p<0.05. The quality of fit of the logistic models was tested with the Hosmer and Lemeshow goodness-of-fit test. Survival Analysis A Proportional Hazards Cox regression model was used to evaluate the effect of early extubation on survival, while adjusting for the patients’ baseline characteristics. Kaplan-Meier curves were generated to show the survival patterns between the two study groups over 16 months after surgery.
Timing of Early Extubation. Receiver operator characteristics (ROC) curves were utilized to evaluate how the timing of extubation affects operative mortality, reintubation, and combined morbidity in cardiac surgery. Curves were generated at each hour of extubation up to 30 hours. The specificity and sensitivity of each hour of extubation to predict postoperative outcomes is reported.
Results
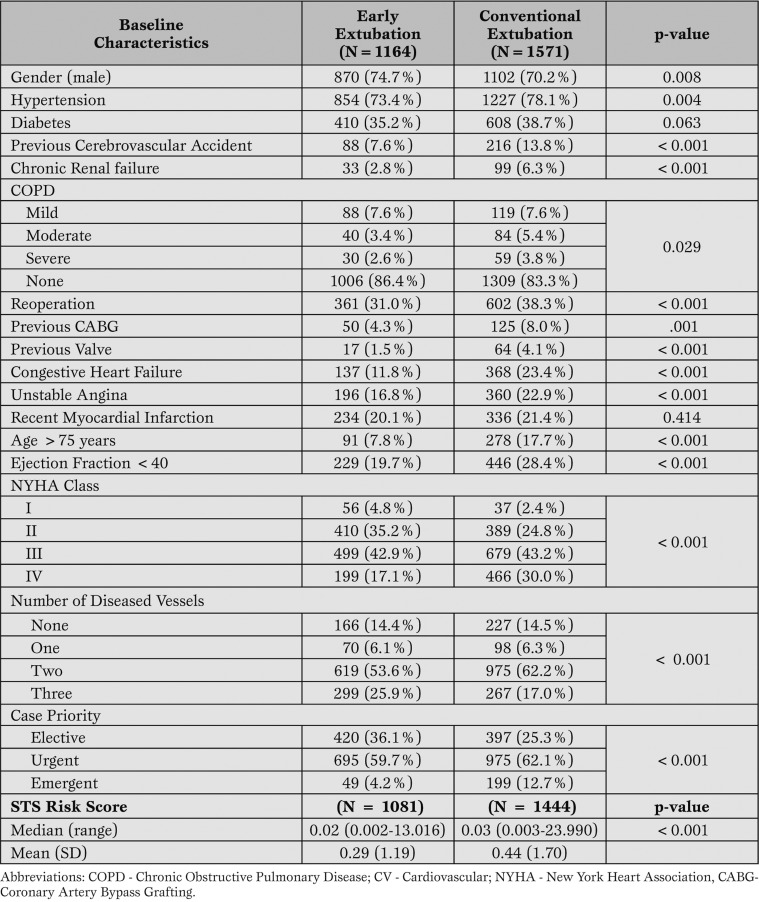
Preoperative Characteristics. Univariate comparisons of patients’ preoperative characteristics between the early extubation group (n=1164) and the conventional extubation group (n=1571) are presented in Table 1.
Table 1.
Patients' Baseline Characteristics in Patients with Early (<6 hours) and Late (>6 hours) Extubation.
Early extubation patients were more likely to be males and have multi-vessel coronary artery disease compared to conventional extubation group patients. Conventional extubation group patients were more likely to have hypertension, chronic renal failure, previous cerebrovascular accident, and reoperation.
Additional characteristics of this group include unstable angina, depressed left ventricular ejection fraction, advanced age (greater than 75 years), be in class III/IV by New York Heart Association (NYHA) functional classification, and have urgent or emergent operation. In addition, the STS Risk Scores for Mortality were significantly higher in the conventional extubation group.
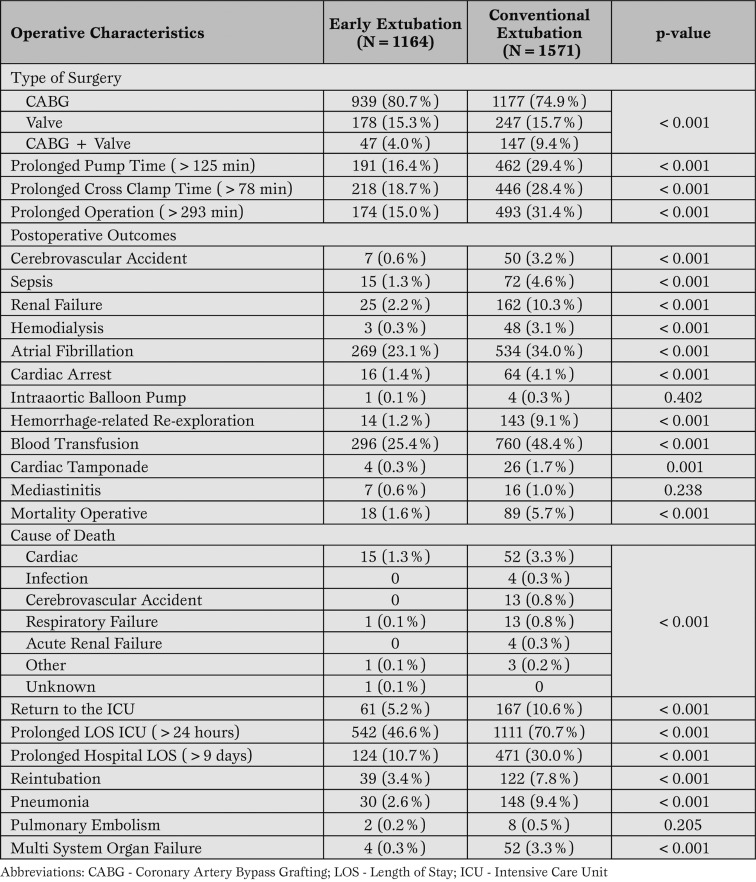
Operative and Postoperative Characteristics. Operative and postoperative results are presented in Table 2.
Table 2.
Patients' Operative and Postoperative Characteristics in Patients with Early (<6 hours) and Late (>6 hours) Extubation.
Early extubation patients were more likely to have undergone isolated CABG compared to conventional extubation group patients. Pump, cross clamp and operation times were longer on average for the conventional extubation group.
Conventional extubation group patients had a higher rate of operative mortality, history of cerebrovascular accident, sepsis, renal failure, atrial fibrillation, hemodialysis, cardiac arrest, hemorrhage-related re-exploration, cardiac tamponade, and blood transfusion.
Conventional extubation group patients were also more likely to be readmitted to the ICU, had higher reintuba-tion rates, and had more prolonged ICU and hospital length of stay.
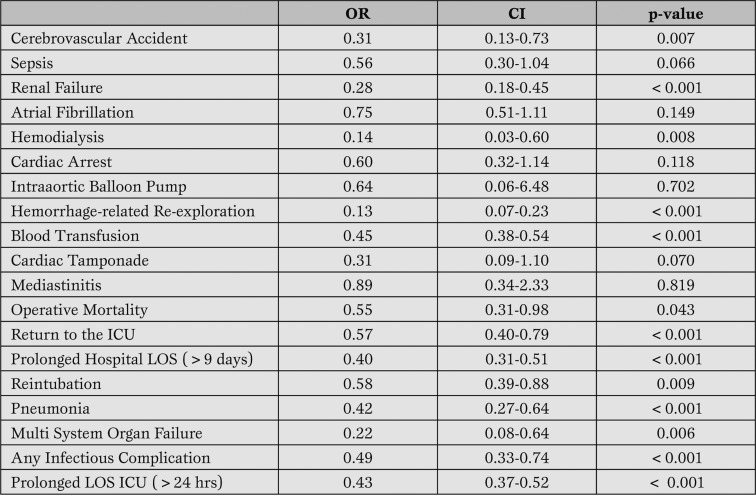
Propensity Score Adjustment and Multivariable Modeling. Propensity scores were calculated and shown to balance out the differences at baseline between the early extubation and the conventional extubation group patients (ONLINE Appendix 1 www.itacta.org) with p <0.05 being statistically significant. The propensity score-adjusted outcomes are shown in Table 3.
Table 3.
Early Extubation and Propensity Score-Adjusted Postoperative Outcomes.
Early extubation was associated with decreased rates of pneumonia (p<0.001), stroke (p=0.007), acute renal failure (p<0.001), hemorrhage-related re-exploration (p<0.001), ICU length of stay (p<0.001) and hospital length of stay (p<0.001), ICU readmission (p<0.001), reintubation (p=0.009), and operative mortality (p=0.043). Multivariable models were used as a supplementary analysis and confirmed these findings with the exception of sepsis (ONLINE Appendix 2 www.itacta.org).
Specifically, pneumonia (OR=0.35), prolonged ICU LOS (OR=0.43), prolonged hospital LOS (OR=0.37), readmission to ICU (OR=0.50), reintubation (OR=0.48), cerebrovascular accident (OR=0.21), renal failure (OR=0.24), re-operation for bleeding (OR=0.13), and mortality (OR=0.46) were all decreased within the early extubation group.
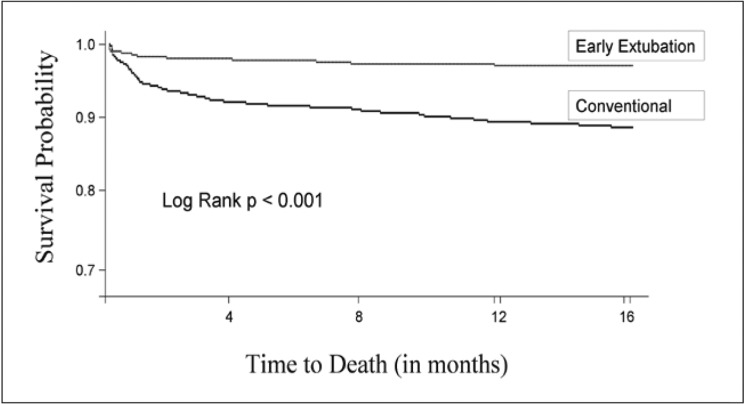
Survival Analysis. Late mortality was assessed out to 16 months after cardiac surgery (Figure 1).
Figure 1.
Kaplan-Meier Curve for Late Mortality.
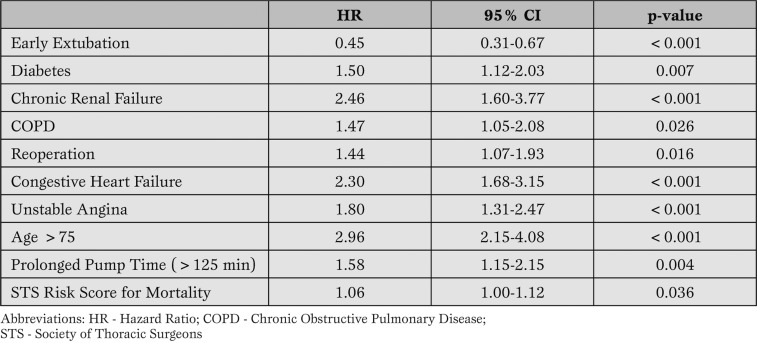
Hazard analysis is presented in Table 4.
Table 4.
Risk Factors for Late Mortality After Cardiac Surgery.
With a hazard ratio (HR) of 0.45, early extubation was associated with decreased late mortality (p<0.001) when adjusting for other significant covariates.
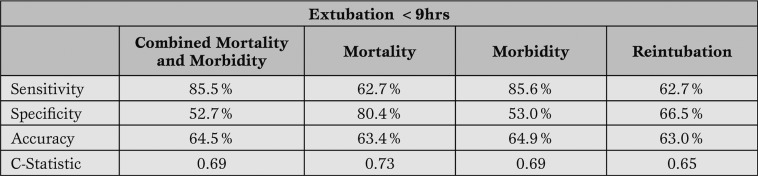
Timing of Early Extubation. A sub-analysis was conducted to determine the optimal timing of extubation to predict improved postoperative outcomes. Extubation within 9 hours emerged as the best predictor of improved postoperative outcomes including morbidity, mortality and reintubation (Table 5).
Table 5.
Specificity,Sensitivity and Accuracy of Extubation <9 Hours to Predict Postoperative Outcomes
Detailed analysis is presented within ONLINE Appendix 3 www.itacta.org.
Discussion
Mechanical ventilation after cardiac surgery is used to improve oxygenation and ventilation as well as reduce cardiac workload in the hemodynamically unstable patient [3,5].
Early extubation has been correlated with decreased rates of mortality, morbidity, and resource utilization and may function as a predictor of an uncomplicated hospital course [1,2,3,4,5,6,7,8,9,11,12,13,14,15].
With this study, we evaluated timing of early extubation and its relation to post-operative complications, death, and resource utilization. Additionally, we examined late mortality in the early versus conventional extubation groups.
Despite the Society of Thoracic Surgeons’ definition for early extubation being extubation within six hours after surgery, an important finding of our study is that extubation up to nine hours after surgery appears to be a better predictor of post-operative outcomes (ONLINE Appendix 3 www.itacta.org). Operative mortality and cardiac cause of death were lower in the early extubation group (p<0.001) as were rates of sepsis, cerebrovascular accident, renal failure, hemodialysis, atrial fibrillation, cardiac arrest, hemorrhage-related re-exploration, and blood transfusion (p<0.001), (Table 2).
Prolonged intubation and continued hemodynamic instability after cardiac surgery leads to significantly increased morbidity and mortality [17]. Mechanical ventilatory support for 16 hours or more demonstrated a trend towards worse post-operative outcomes (ONLINE Appendix 3 www.itacta.org).
This mirrors the findings from previous studies where poorer post-operative results occurred in those extubated in greater than 24 hours [4,18]. Early extubation was associated with improved survival up to 16 months after cardiac surgery (p<0.001) while chronic renal failure, congestive heart failure, unstable angina, and advanced age diminished late survival (Table 4). Similar findings were demonstrated by Cheng et al where there were no deaths in the one year follow-up in those patients extubated early [1]. This study is among the first to demonstrate early extubation as a predictor of improved early and late outcomes after cardiac surgery. Limitations. Limitations of this study include all those inherent to any retrospective single-institution analysis.
All data elements, however, were prospectively entered into a cardiac surgery research database with strict definitions, and the data analysis was performed using appropriately risk-adjusted statistical models to adjust for differences in preoperative risk factors. The accuracy of predicting improved outcomes in those patients extubated in <9 hours is 65%.
Conclusions
Early extubation is among the earliest post-operative predictors for those patients who are more likely to have a smooth post-operative course and decreased complications after cardiac surgery. Further studies are recom-mended to confirm the findings of this study and implement changes in clinical practice.
Footnotes
Disclosure The authors do not have any disclosure of any personal or financial support and there is no actual or potential conflict of interest for the subject manner.
References
- Cheng DC, Wall C, Djaiani G. et al. Randomized assessment of resource use in fast-track cardiac surgery 1-year after hospital discharge. Anesthesiology. 2003;98:651–657. doi: 10.1097/00000542-200303000-00013. [DOI] [PubMed] [Google Scholar]
- Reyes A, Vega G, Blancas R. et al. Early vs. conventional extubation after cardiac surgery with cardiopulmonary bypass. Chest. 1997;112:193–201. doi: 10.1378/chest.112.1.193. [DOI] [PubMed] [Google Scholar]
- Hawkes CA, Dhileepan S, Foxcroft D. Early extubation for adult cardiac surgery patients. The Cochrane Database of Systemic Reviews. 2007;3 doi: 10.1002/14651858.CD003587. [DOI] [PubMed] [Google Scholar]
- Cheng DC, Karski J, Peniston C. et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. Journal Thorac Cardiovasc Surg. 1996;112:755–764. doi: 10.1016/S0022-5223(96)70062-4. [DOI] [PubMed] [Google Scholar]
- Guller U, Anstrom KJ, Holman WL. et al. Outcomes of early extubation after cardiac surgery in the elderly. Ann Thorac Surg. 2004;77:781–788. doi: 10.1016/j.athoracsur.2003.09.059. [DOI] [PubMed] [Google Scholar]
- Konstantakos AK, Lee JH. Optimizing timing of early extubation in coronary artery bypass surgery patients. Ann Thorac Surg. 2000;69:1842–1845. doi: 10.1016/s0003-4975(00)01248-0. [DOI] [PubMed] [Google Scholar]
- Myles PS, Daly DJ, Djaiani G. et al. A systematic review of the safety and effectiveness of fast-track cardiac anesthesia. Anesthesiology. 2003;99:982–987. doi: 10.1097/00000542-200310000-00035. [DOI] [PubMed] [Google Scholar]
- London MJ, Shroyer AL, Coll JR. et al. Early extubation following cardiac surgery in a veterans population. Anesthesiology. 1998;88:1447–1458. doi: 10.1097/00000542-199806000-00006. [DOI] [PubMed] [Google Scholar]
- Roosens C, Heerman J, De Somer F. et al. Effects of off-pump coronary surgery on the mechanics of the respiratory system, lung, and chest wall. Comparison with extracorporeal circulation. Crit Care Med. 2002;30:2430–2437. doi: 10.1097/00003246-200211000-00005. [DOI] [PubMed] [Google Scholar]
- D\'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Rady MY, Ryan T. Perioperative predictors of extubation failure and the effect on clinical outcome after cardiac surgery. Crit Care Med. 1999;27:340–347. doi: 10.1097/00003246-199902000-00041. [DOI] [PubMed] [Google Scholar]
- Camp SL, Stamou SC, Stiegel MR. et al. Quality improvement program increase early tracheal extubation rate and decreases pulmonary complications and resource utilization after cardiac surgery. Journal of Cardiac Surgery. doi: 10.1111/j.1540-8191.2008.00783.x. [In Press] [DOI] [PubMed] [Google Scholar]
- Stamou SC, Camp SL, Stiegel MR. et al. Continuous quality improvement program and morbidity after cardiac surgery. American Journal of Cardiology. 2008;102:772–777. doi: 10.1016/j.amjcard.2008.04.061. [DOI] [PubMed] [Google Scholar]
- Stamou SC, Turner S, Stiegel MR. et al. Quality improvement program decreases mortality after cardiac surgery. Journal of Thoracic and Cardiovascular Surgery. 2008;136:494–499. doi: 10.1016/j.jtcvs.2007.08.081. [DOI] [PubMed] [Google Scholar]
- Lobdell KW, Camp SL, Stamou S. et al. Quality improvement in cardiac critical care. HSR Proceedings in Intensive Care and Cardiovascular Anesthesia. 2009;1:16–20. [PMC free article] [PubMed] [Google Scholar]
- Wahl GW, Swineburne AJ, Fedullo AJ. et al. Long-term outcome when major complications follow coronary artery bypass graft surgery. 1996;110:1394–1389. doi: 10.1378/chest.110.6.1394. [DOI] [PubMed] [Google Scholar]
- Cohen AJ, Katz MG, Frenkel G. et al. A. Morbid results of prolonged intubation after coronary artery bypass surgery. Chest. 2000;118:1724–1731. doi: 10.1378/chest.118.6.1724. [DOI] [PubMed] [Google Scholar]
- Kern H, Redlich U, Hotz H. et al. Risk factors for prolonged ventilation after cardiac surgery using APACHE II, SAPS II, and TISS: comparison. Intensive Care Medicine. 2001;27:407–415. doi: 10.1007/s001340000802. [DOI] [PubMed] [Google Scholar]