Abstract
Introduction
Volatile anesthetics improve post-ischemic recovery. A meta-analysis suggested that the cardioprotective properties of desflurane and sevoflurane could reduce mortality and cardiac morbidity in cardiac surgery. Recent American College of Cardiology / American Heart Association Guidelines recommended volatile anesthetic agents during non-cardiac surgery for the maintenance of general anesthesia in patients at risk for myocardial infarction but whether these cardioprotective properties exist in non-cardiac surgery settings is controversial. We therefore performed a meta-analysis of randomized studies to investigate this issue.
Methods
Two investigators independently searched PubMed. Inclusion criteria were random allocation to treatment, comparison of a total intravenous anesthesia regimen vs an anesthesia plan including desflurane or sevoflurane, performed on adult patients undergoing non-cardiac surgery. The primary endpoints were the incidence of perioperative myocardial infarction and death.
Results
A total of 6219 patients from 79 randomized trials were identified. No myocardial infarctions or deaths were reported in any of the studies we examined.
Conclusions
This meta-analysis highlights a weakness in the literature and the results can be used to design future studies: the cardioprotective properties of desflurane and sevoflurane have never been studied in noncardiac surgery. No randomized study, among those which compared desflurane or sevoflurane to intravenous anesthetics, has addressed major outcomes such as myocardial infarction or mortality. Large, multicentre, randomized clinical trials including patients undergoing high-risk non-cardiac surgery and reporting clinically relevant outcomes such as myocardial infarction and mortality are needed.
Keywords: myocardial infarction, death, volatile anesthetics, desflurane, sevoflurane, anesthesia
Introduction
Myocardial injury after surgery could be associated with increase complications and prolonged hospital stay. A recent meta-analysis [1] showed that desflurane and sevoflurane could reduce postoperative mortality and incidence of myocardial infarction (MI) following cardiac surgery with significant advantages in terms of reduced postoperative cardiac troponin (cTn) release, need for inotropic support, time on mechanical ventilation, intensive care unit (ICU) and overall hospital stay.
Volatile anesthetics improve post-ischemic recovery at the cellular level, in isolated hearts, and in animals [2]. Whether their cardioprotective effects are clinically important is still debated.
According to the recent “American College of Cardiology/American Heart Association Guidelines” volatile anesthetics can be beneficial during non-cardiac surgery for the maintenance of general anesthesia in hemodinamically stable patients at risk for myocardial ischemia, [3] but no evidence-based medicine exists in non-cardiac surgery.
To address the question whether the choice of an anesthetic regimen might influence patients’ outcome after non-cardiac surgery, we have independently conducted a systematic review and meta-analysis of data pooled from existing trials to determine the impact of desflurane and sevoflurane on perioperative MI and death in patients undergoing noncardiac surgery. Desflurane and sevoflurane appear to have the most prominent cardioprotective properties in experimental studies [4,5] and are the only anesthetic drugs that reduce morbidity and mortality in surgical patients [1].
Methods
Search Strategy
Pertinent studies were independently searched in BioMedCentral and PubMed. The full PubMed search strategy was developed according to Biondi-Zoccai et al, [6] and is available in the appendix. No language restriction was enforced and non-English-language articles were translated before further analysis.
Study Selection
References obtained from database and literature searches were first independently examined at the title/abstract level by four trained investigators with divergences resolved by consensus, and then, if potentially pertinent, retrieved as complete articles. The following inclusion criteria were employed for potentially relevant studies: random allocation to treatment, comparison of a total intravenous anesthesia (TIVA) versus an anesthesia plan including administration of desflurane or sevoflurane, performed in cardiac surgery with no restriction in dose and time of administration.
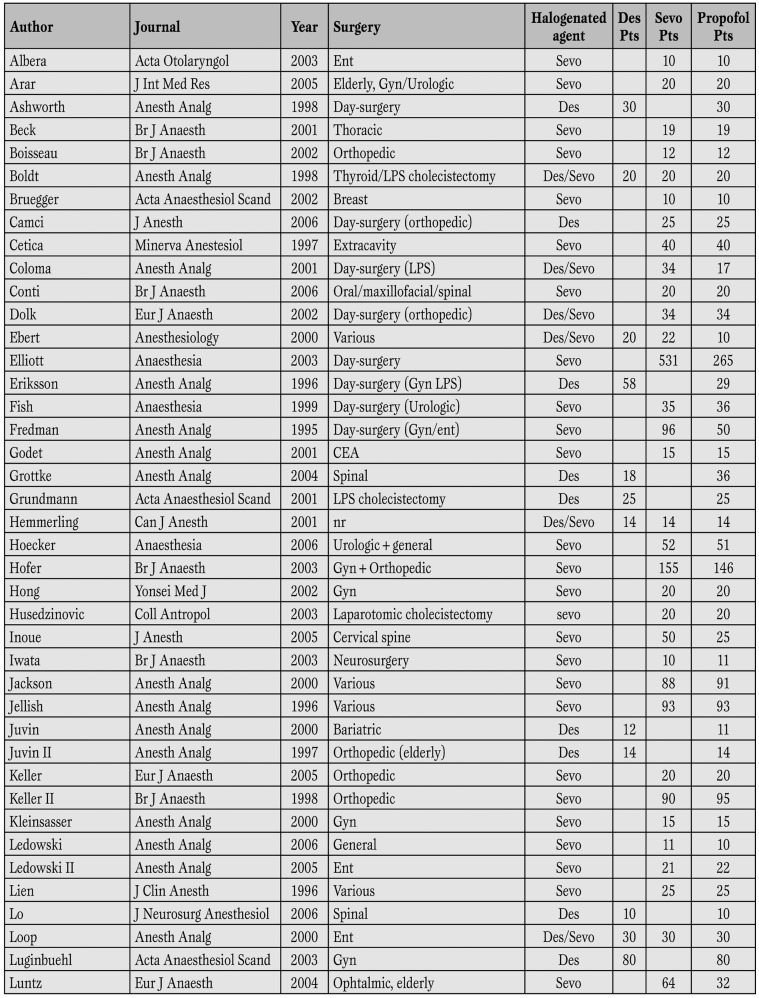
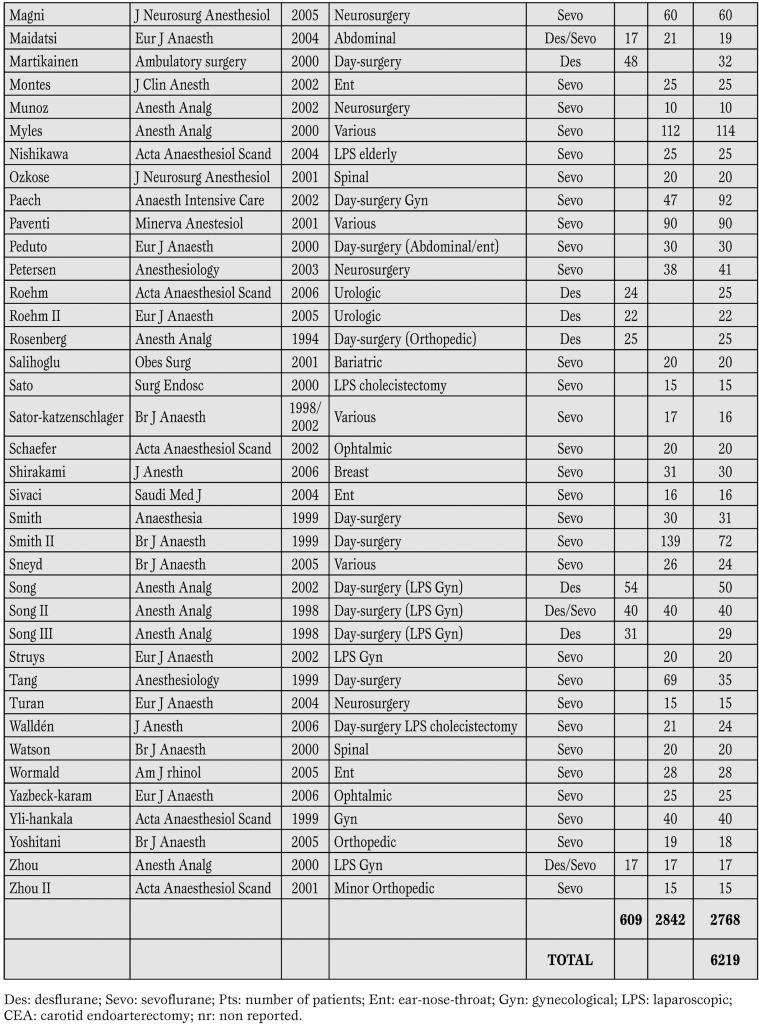
The exclusion criteria were: duplicate publications, studies conducted in cardiac surgery, studies on pediatric patients, non-human experimental studies. Four investigators, independently assessed compliance to selection criteria and selected studies for the final analysis, with divergences finally resolved by consensus (Table 1).
Table 1 part 1.
The 79 studies included in the meta-analysis.
Table 1 part 2.
Des: desflurane; Sevo: sevoflurane; Pts: number of patients; Ent: ear-nose-throat; Gyn: gynecological; LPS: laparoscopic; CEA: carotid endoarterectomy; nr: non reported.
Data Abstraction and Study Characteristics
Baseline, procedural and outcome data were independently abstracted by four trained investigators with divergences resolved by consensus.
Specifically, we extracted study end-points and main outcomes; study design (including patient selection, randomization, single-/multi-center design, open or single-/double-blind design); clinical setting; population; anesthetic protocol; choice of intravenous anesthetics; adverse events. At least two attempts at contacting original authors via electronic or conventional mail was made in case of missing data.
The primary end-point of the present review was the rate of in-hospital MI as per author definition while the co-primary end-point was the rate of hospital mortality. Secondary endpoints were: peak cardiac troponin release, cardiac adverse events other than MI (arrhythmias, heart failure), intensive care unit (ICU) and hospital stay, time on mechanical ventilation, other major adverse events (renal failure, respiratory failure.
Data Analysis and Synthesis
Computations were performed with RevMan 4.2 (a freeware available from The Cochrane Collaboration) [7]. Statistical heterogeneity and inconsistency was measured using, respectively, Cochran Q tests and I2. Binary outcomes from individual studies were analyzed in order to compute individual and pooled odds ratios (OR) with pertinent 95% confidence intervals (CI, with equivalence set at 1, OR<1 favoring the first treatment, and OR>1 favoring the second treatment), by means of the Peto fixed effect method in case of low statistical inconsistency (I2≤25%) and by means of a random effect method (which better accommodates clinical and statistical variations) in case of moderate or high statistical inconsistency (I2>25%). Weighted mean differences (WMD) and 95% CI were computed for continuous variables, again by means of a fixed effect method in case of low statistical inconsistency (I2≤25%) and by means of a random effect method in case of moderate or high statistical inconsistency (I2>25%) [7].
Statistical significance was set at the two-tailed 0.05 level for hypothesis testing and at 0.10 for heterogeneity testing, and unadjusted P values are reported throughout. This study was performed in compliance with The Cochrane Collaboration and the Quality of Reporting of Meta-Analyses (QUOROM) guidelines [8,9].
Results
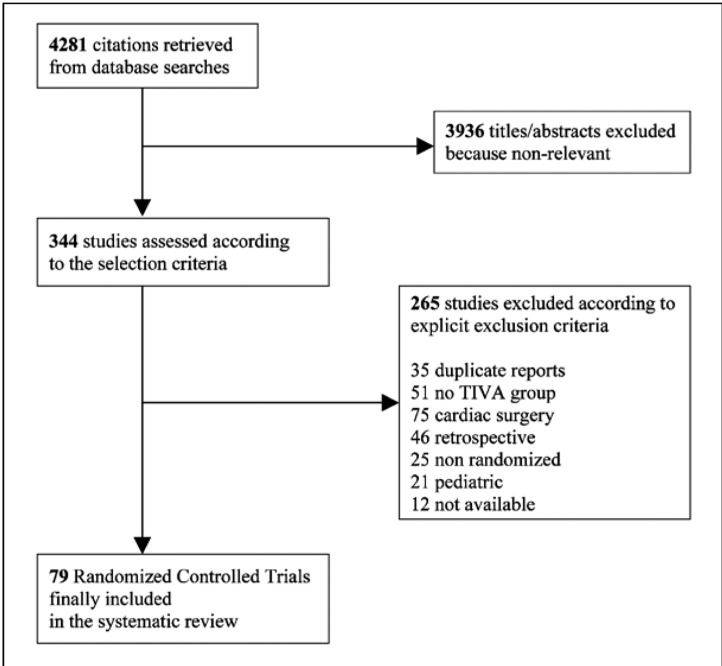
Database searches, snowballing and contacts with experts yielded a total of 4281 citations. Excluding 3936 non-pertinent titles or abstracts, we retrieved in complete form and assessed according to the selection criteria 344 studies. A total of 265 studies were further excluded according to our exclusion criteria (Figure 1).
Figure 1.
Flow diagram of the systematic review process.
We finally identified 79 eligible randomized clinical trials, which were included in the final analysis (Table 1) (complete references are available from the authors for readers).
Study Characteristics
The 79 included trials randomized 6219 patients (2768 to TIVA and 3451 receiving desflurane or sevoflurane in their anesthesia plan). (Table 1) All studies used propofol as the main hypnotic agent in the TIVA group. Surgical settings varied across studies and included vascular, thoracic, orthopedic, general, gynecological, urological, ear-nose-throat, bariatric, ophthalmic, surgery and neurosurgery. Nineteen studies were conducted in day-surgery settings. All authors administered volatile or intravenous anesthetics throughout the procedure.
Volatile anesthetic dosage varied across studies, ranging 0.33-2 MAC in the 609 patients receiving desflurane and 0.25-2 MAC in the 2842 patients receiving sevoflurane. All studies had a single-center design, and included populations which were too small to allow for significant results in clinical relevant outcome variables.
Study quality appraisal showed that most studies appeared of suboptimal quality, as testified by the common lack of details on the method used for randomized sequence generation and allocation. Only a handful of randomized controlled trials (RCTs) were of high quality, while many others lacked important details to appraise the risk of selection, performance, attrition, or detection biases.
Quantitative Data Synthesis
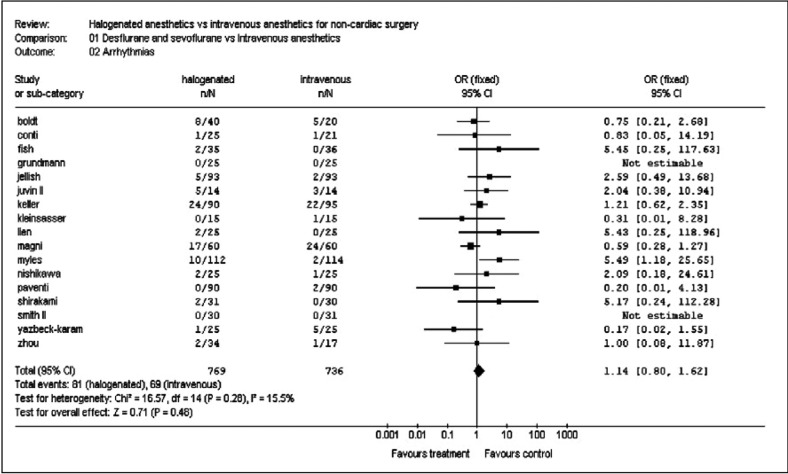
No author reported any postoperative myocardial infarction or death among the study population, nor any significant cardiac adverse event. No difference in the incidence of arrhythmias (81/769 [10.5%] in the volatile anesthetics group vs 69/736 [9.4%] in the control arm, OR=1.14 [0.80-1.62], p for effect=0.48, p for heterogeneity=0.28, I2=15.5%) was noted (Figure 2).
Figure 2.
Pooled estimators of incidence of intraoperative arrhythmias.
No other cardiac adverse events were reported. Hospital stay was identical between groups (WMD 0.01 days [-0.06, 0.07], p for effect=0.88, p for heterogeneity =0.48, I2=0% with 1201 included patients). Postoperative renal or respiratory failure and release of cardiac biomarkers were not reported.
We attempted to contact all authors twice. Nineteen out of eighty authors answered our request for additional data, and responses confirmed that no deaths or myocardial infarctions were observed among their patients. When directly interrogated as to why they did not include cardiac adverse events in their reports, 16% of authors answered that they were not aware of the cardioprotective properties of halogenated anesthetics, 63% that they did not observe any adverse event during their study and decided not to report it, and 21% replied that they did not monitor patients for cardiac complications.
Discussion
We performed a meta-analysis of pooled data from several small, underpowered studies to demonstrate whether the cardioprotective properties of desflurane and sevoflurane could decrease the rate of MI and death in patients undergoing non-cardiac surgery. We found that comparison between halogenated agents and propofol in non-cardiac surgery in terms of cardiac morbidity and mortality is, so far, unattainable because of lack of published data. Postoperative mortality and myocardial infarction rate were either null or non reported in all studies included in our meta-analysis.
Desflurane and sevoflurane have been recently shown to reduce incidence of morbidity and mortality following cardiac surgery: a meta-analysis found a 4-fold decrease of mortality (0.4% vs 1.6%, p=0.02) and a 2-fold decrease of myocardial infarctions (2.4% vs 5.1%, p=0.008). The authors also found advantages in terms of cTn release, ICU and overall hospital stay, need for inotropic support and mechanical ventilation, and one-year major cardiac events. Multicentre experiences had previously demonstrated that halogenated anesthetics reduce cTn release following coronary artery bypass grafting surgery, [10,11] while discordant results exist in valvular surgery [12,13] and a pilot study yielded no results in patients undergoing stenting procedures [14].
Whether these cardioprotective properties also exist in noncardiac surgical settings is still controversial, owing to the scarce available data. The use of volatile anesthetics for hemodynamically stable patients at risk for myocardial ischemia undergoing noncardiac surgical procedures has recently been recommended as a class of evidence IIA, level B, [3] but no prospective or retrospective study supports this recommendation. Previous meta-analyses on volatile and intravenous anesthetics in non-cardiac surgery did not investigate clinically relevant outcomes, focusing on induction characteristics, [15] postoperative recovery times [15,16] and incidence of postoperative nausea and vomiting (PONV) [17,18,19]. Most authors agreed that propofol reduces PONV, while awakening and extubation times appear to be shorter in patients treated with halogenated anesthetics.
We believe that, while it is important to ascertain the quality of our daily work in terms of patient comfort before, during and after surgery, but it is vital to understand what tools we have to influence the very outcome of our patients. In a recently published review, Bassi et al compared the outcome of patients undergoing one-lung ventilation under either intravenous or inhalational anesthesia, and reached our same conclusions: it was impossible to conduct a meta-analysis because no author reported patient outcome. Most studies were of poor quality, and this made it impossible to use analytical methods in order to reach a solid result.
The observation that volatile anesthetics have cardioprotective properties that last after their elimination led to the concept of pharmacological preconditioning or anesthetic preconditioning [20]. These properties are enhanced by their administration in the reperfusion phase [4] and seem to be related to their timing and modalities of administration during cardiac surgery [21,22].
All volatile anesthetics induce a dose-dependent decrease in myocardial contractility and cardiac loading conditions. These depressant effects decrease myocardial oxygen demand and may, therefore, have a beneficial role on the myocardial oxygen balance during myocardial ischemia. Experimental evidence has clearly demonstrated that in addition to these indirect protective effects, volatile anesthetic agents also have direct protective properties against reversible and irreversible ischemic myocardial damage.
These properties have not only been related to a direct preconditioning effect but also to an effect on the extent of reperfusion injury [23,24,25,26,27]. Since the mechanisms that lead to anesthetic preconditioning are not fully understood yet, it cannot be excluded that the protective effects of desflurane and sevoflurane that have been observed may be due to properties other than preconditioning alone.
Limitations
Drawbacks of systematic reviews and meta-analyses are well known [8,9]. Particular attention should be drawn to the overall suboptimal quality of the RCT included. The fact that none of the included studies encountered any major adverse event suggests that postoperative death and MI were both poorly reported and/or adjudicated in the analyzed studies. While this may weaken the results of our meta-analysis, it strengthens our opinion that patient outcome should never be forgotten in clinical studies.
Conclusions
Volatile anesthetics have low costs and carry very few risks, and have been demonstrated to reduce morbidity and mortality following cardiac surgery. In contrast to recent guidelines, the results of our study cannot support the hypothesis that their routine use can reduce perioperative myocardial injury in non-cardiac surgery. The fact, however, that no cardiac protection by desflurane or sevoflurane could be shown in this analysis does not mean that these substances do not provide such protection in high risk patients undergoing non-cardiac surgery: it does, instead, stress the scarce awareness among anesthesiologists that patient outcome can be affected by our anesthetic plan.
Large, multicentre, randomized clinical trials including patients undergoing high-risk non-cardiac surgery and reporting data on clinically relevant outcomes are needed to achieve a demonstration of anesthetic-induced cardioprotection: this represents a difficult task because of the low mortality rate in modern surgery, and because of the number of interfering factors.
Appendix
Search strategy for PubMed, developed according to Biondi-Zoccai et al. [6] (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR (clinical trial[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind[tw])) OR (latin square[tw]) OR placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR comparative study[mh] OR evaluation studies[mh] OR follow-up studies[mh] OR prospective studies[mh] OR cross-over studies[mh] OR control*[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (animal[mh] NOT human[mh]) NOT (comment[pt] OR editorial[pt] OR meta-analysis[pt] OR practice-guideline[pt] OR review[pt])) AND (desfluran* OR sevofluran* OR propofol*) AND (cardiac AND (operation OR intervention OR surgery OR bypass))).
Abbreviations
- ICU
Intensive care unit
- MI
Myocardial infarction
- PONV
Post operative nausea and vomiting
- RCT
Randomized controlled trial
- TIVA
Total intravenous anesthesia
Footnotes
Source of support This study was conducted with departmental sources and supported in part by \'Un cuore per la vita\'.
Conflict of interest Landoni Giovanni acknowledges receiving speaker fess form Abbott, Baxter and Minrad. No other conflict of interest exists.
References
- Landoni G, Biondi-Zoccai GG, Zangrillo A. et al. Desflurane and sevoflurane in cardiac surgery: a meta-analysis of randomized clinical trials. J Cardiothorac Vasc Anesth. 2007;21:502–511. doi: 10.1053/j.jvca.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Chiari P, Bouvet F, Piriou V. et al. Anaesthetic-induced myocardial preconditioning: fundamental basis and clinical implications. Ann Fr Anesth Reanim. 2005;24:383–396. doi: 10.1016/j.annfar.2005.01.020. [DOI] [PubMed] [Google Scholar]
- Fleisher LA, Beckman JA, Brown KA. et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation. 2007;116:1971–1996. doi: 10.1161/CIRCULATIONAHA.107.185700. [DOI] [PubMed] [Google Scholar]
- Preckel B, Schlack W, Comfere T. et al. Effects of enflurane, isoflurane, sevoflurane and desflurane on reperfusion injury after regional myocardial ischaemia in the rabbit heart in vivo. Br J Anaesth. 1998;81:905–912. doi: 10.1093/bja/81.6.905. [DOI] [PubMed] [Google Scholar]
- Pirou V, Chiari P, Lhuillier F. et al. Pharmacological preconditioning: comparison of desflurane, sevoflurane, isoflurane and halothane in rabbit myocardium. Br J Anaesth. 2002;89:486–491. [PubMed] [Google Scholar]
- Biondi-Zoccai GG, Agostoni P, Abbate A. et al. A simple hint to improve Robinson and Dickersin\'s highly sensitive PubMed search strategy for controlled clinical trials. Int J Epidemiol. 2005;34:224–225. doi: 10.1093/ije/dyh311. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S. The Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. 2005 [Available at: http://www.cochrane.org/resources/handbook/hbook.htm; Accessed October 10th] [Google Scholar]
- Moher D, Cook DJ, Eastwood S. et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- Biondi-Zoccai GG, Lotrionte M, Abbate A. et al. Compliance with QUOROM and quality of reporting of overlapping meta-analyses on the role of acetylcysteine in the prevention of contrast associated nephropathy: case study. Bmj. 2006;332:202–209. doi: 10.1136/bmj.38693.516782.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarracino F, Landoni G, Tritapepe L. et al. Myocardial damage prevented by volatile anesthetics: a multicenter randomized controlled study. J Cardiothorac Vasc Anesth. 2006;20:477–483. doi: 10.1053/j.jvca.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Tritapepe L, Landoni G, Guarracino F. Cardiac protection by volatile anaesthetics: a multicentre randomized controlled study in patients undergoing coronary artery bypass grafting with cardiopulmonary bypass. Eur J Anaesthesiol. 2007;24:323–331. doi: 10.1017/S0265021506001931. [DOI] [PubMed] [Google Scholar]
- Landoni G, Calabrò MG, Marchetti C. et al. Desflurane versus propofol in patients undergoing mitral valve surgery. J Cardiothorac Vasc Anesth. 2007;21:672–677. doi: 10.1053/j.jvca.2006.11.017. [DOI] [PubMed] [Google Scholar]
- Cromheecke S, Pepermans V, Hendrickx E. et al. Cardioprotective properties of sevoflurane in patients undergoing aortic valve replacement with cardiopulmonary bypass. Anesth Analg. 2006;103:289–296. doi: 10.1213/01.ane.0000226097.22384.f4. [DOI] [PubMed] [Google Scholar]
- Landoni G, Zangrillo A, Fochi O. et al. Cardiac protection with volatile anesthetics in stenting procedures. J Cardiothorac Vasc Anesth. 2008;22:543–547. doi: 10.1053/j.jvca.2008.02.020. [DOI] [PubMed] [Google Scholar]
- Robinson BJ, Uhrich TD, Ebert TJ. et al. A review of recovery from sevoflurane anaesthesia: comparisons with isoflurane and propofol including meta-analysis. Acta Anaesthesiol Scand. 1999;43:185–190. doi: 10.1034/j.1399-6576.1999.430211.x. [DOI] [PubMed] [Google Scholar]
- Dexter F, Tinker JH. Comparisons between desflurane and isoflurane or propofol on time to following commands and time to discharge. A metaanalysis. Anesthesiology. 1995;83:77–82. doi: 10.1097/00000542-199507000-00009. [DOI] [PubMed] [Google Scholar]
- Tramer M, Moore A, McQuay H. et al. Propofol anaesthesia and postoperative nausea and vomiting: quantitative systematic review of randomized controlled studies. Br J Anaesth. 1997;78:247–255. doi: 10.1093/bja/78.3.247. [DOI] [PubMed] [Google Scholar]
- Gupta A, Stierer T, Zuckerman R. et al. Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: a systematic review. Anesth Analg. 2004;98:632–641. doi: 10.1213/01.ane.0000103187.70627.57. [DOI] [PubMed] [Google Scholar]
- Sneyd JD, Carr A, Byrom WD. et al. A meta-analysis of nausea and vomiting following maintenance of anaesthesia with propofol or inhalational agents. Eur J Anaesthesiol. 1998;15:433–445. doi: 10.1046/j.1365-2346.1998.00319.x. [DOI] [PubMed] [Google Scholar]
- De Hert SG, Turani F, Mathur S. et al. Cardioprotection with volatile anesthetics: mechanisms and clinical implications. Anesth Analg. 2005;100:1584–1593. doi: 10.1213/01.ANE.0000153483.61170.0C. [DOI] [PubMed] [Google Scholar]
- De Hert SG, Van der Linden PJ, Cromheeke S. et al. Cardioprotective properties of sevoflurane in patients undergoing coronary surgery with cardiopulmonary bypass are related to the modalities of its administration. Anesthesiology. 2004;101:299–310. doi: 10.1097/00000542-200408000-00009. [DOI] [PubMed] [Google Scholar]
- Bignami E, Biondi-Zoccai G, Landoni G. et al. Volatile Anesthetics Reduce Mortality in Cardiac Surgery. J Cardiothorac Vasc Anesth. 2009;23:594–599. doi: 10.1053/j.jvca.2009.01.022. [DOI] [PubMed] [Google Scholar]
- De Hert SG. Volatile anesthetics and cardiac function. Semin Cardiothorac Vasc Anesth. 2006;10:33–42. doi: 10.1177/108925320601000107. [DOI] [PubMed] [Google Scholar]
- Landoni G, Fochi O, Bignami E. Volatile anesthetics for periprocedural cardiac protection. A review. Minerva Cardioangiol. 2008;56:429–434. [PubMed] [Google Scholar]
- Landoni G, Fochi O, Tritapepe L. et al. Cardiac protection by volatile anesthetics. A review. Minerva Anestesiol. 2009;75:269–273. [PubMed] [Google Scholar]
- Landoni G, Fochi O, Torri G. et al. Cardiac protection by volatile anaesthetics: a review. Curr Vasc Pharmacol. 2008;6:108–111. doi: 10.2174/157016108783955284. [DOI] [PubMed] [Google Scholar]
- Landoni G, Bignami E, Oliviero F, Zangrillo A. Halogenated anaesthetics and cardiac protection in cardiac and non-cardiac anaesthesia. Ann Card Anaesth. 2009;12:4–9. doi: 10.4103/0971-9784.45006. [DOI] [PubMed] [Google Scholar]