Abstract
Introduction
Out-of-hospital cardiac arrest has a low survival rate to hospital discharge. Recent studies compared a simplified form of CPR, based on chest compression alone versus standard CPR including ventilation. We performed systematic review and meta-analysis of randomized controlled trials, focusing on survival at hospital discharge.
Methods
We extensively searched the published literature on out-of hospital CPR for non traumatic cardiac arrest in different databases.
Results
We identified only three randomized trials on this topic, including witnessed and not-witnessed cardiac arrests. When pooling them together with a meta-analytic approach, we found that there is already clinical and statistical evidence to support the superiority of the compression-only CPR in terms of survival at hospital discharge, as 211/1842 (11.5%) patients in the chest compression alone group versus 178/1895 (9.4%) in the standard CPR group were alive at hospital discharge: odds ratio from both Peto and DerSimonian-Laird methods =0.80 (95% confidence interval 0.65-0.99), p for effect =0.04, p for heterogeneity =0.69, inconsistency =0%).
Conclusions
Available evidence strongly support the superiority of bystander compression-only CPR. Reasons for the best efficacy of chest compression-only CPR include a better willingness to start CPR by bystanders, the low quality of mouth-to-mouth ventilation and a detrimental effect of too long interruptions of chest compressions during ventilation. Based on our findings, compression-only CPR should be recommended as the preferred CPR technique performed by untrained bystander.
Keywords: cardiopulmonary resuscitation, meta-analysis, systematic review, cardiac arrest, randomized trials, compression-only
Introduction
Out-of-hospital cardiac arrest is still a major public health issue [1], claiming hundreds of thousands of lives worldwide yearly. Unfortunately, survival rate to hospital discharge has improved little over the past decades [2]. Bystander-initiated cardiopulmonary resuscitation (CPR) is essential to increase the chance of survival and neurological recovery [3]. Despite huge efforts to train laypeople to recognize and treat cardiac arrest, incidence of bystander CPR remains very low [4]. Reluctance to perform mouth-to-mouth ventilation is one of the major reason [5,6]. Whereas CPR including ventilation is still considered the gold standard approach before advanced life support can be instituted, a growing number of studies compared a simplified form of CPR, based on chest compression alone versus standard CPR including ventilation. Animal studies showed no difference in survival [7] or even worse outcomes [8] when ventilation was added to chest compressions; nevertheless, in animal models of cardiac arrest due to respiratory causes a positive effect of ventilations was demonstrated [9]. In humans, observational studies of bystander-initiated CPR comparing standard and compressions-only CPR reported similar survival rates [10,11,12]; however, interpretation of the results is made difficult due to the high heterogeneity of the causes of cardiac arrest and of the rescue characteristics. Chest compression-only CPR is simpler than standard CPR to teach (during courses but even by dispatchers under real conditions), and likely a higher percentage of bystanders would accept to perform it while avoiding mouth-to-mouth contact [6]: the demonstration that it is (at least) as effective as standard CPR can be crucial to improve survival rate in out-of-hospital cardiac arrest.
With the underlying hypothesis that out-of-hospital cardiac arrest bystander-initiated compression-only CPR is equivalent to CPR including ventilation (standard CPR), we performed a comprehensive systematic review and meta-analysis of randomized controlled trials, focusing on survival at hospital discharge.
Methods
Search strategy
Pertinent studies were independently searched in BioMedCentral, CENTRAL, and PubMed (updated September 1st , 2010) by several trained investigator. The full search strategies in Pubmed was “(cpr OR resuscitation) AND compression AND breath* AND cardiac AND arrest AND survival)”. Further hand or computerized searches involved the recent ( 2008-2010 ) conference proceedings from the International Anesthesia Research Society, American Heart Association, American College of Cardiology, American Society of Anesthesiology and European Society of Cardiology congresses. In addition, we employed backward snowballing (ie scanning of reference of retrieved articles and pertinent reviews) and contacted international experts for further studies. No language restriction was enforced, and non-English-language articles were translated when appropriate.
Study selection
References obtained from database and literature searches were first independently examined at the title/abstract level by several investigators with divergences resolved by consensus, and then, if potentially pertinent, retrieved as complete articles.
The following inclusion criteria were employed for potentially relevant studies:
a. random allocation to treatment;
b. comparison of chest-compression-only versus standard CPR.
The exclusion criteria were:
a. non-parallel design (ie cross-over) randomized trials,
b. duplicate publications (in this case only the article reporting the longest follow-up was abstracted);
c. non-human experimental studies;
d. no outcome data.
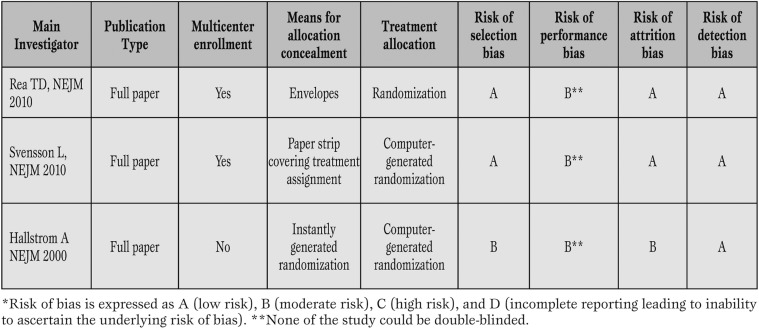
Two investigators independently assessed compliance to selection criteria and selected studies for the final analysis, with divergences finally resolved by consensus (Table 1).
Table 1.
Design features and appraisal of the internal validity of included studies. *
Data abstraction and study characteristics
Baseline and outcome data were independently abstracted by several investigators with divergences resolved by consensus (Table 2). The primary end-point of the present review was survival (hospital discharge).
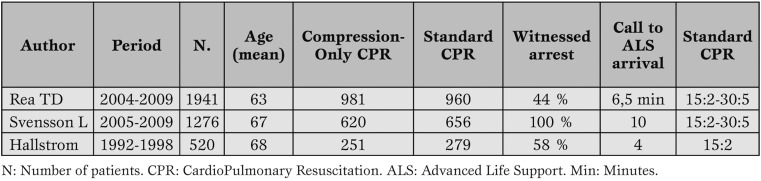
Table 2.
Overall characteristics of 3737 patients who received either Compression-only (1852 patients) or Standard-CPR (1895 patients) for out of hospital cardiopulmonary resuscitation.
Internal validity assessment
The internal validity of included trials was appraised according to The Cochrane Collaboration methods, ie judging the risk for selection bias (ie the bias due to the unbalanced enrolment of specific patient subsets in one of the groups), performance bias (ie the bias due to differences in the management of patients or ancillary treatment, beyond the intervention object of randomized allocation), attrition bias (ie the bias due to incomplete follow-up or different length of follow-up), or difference in number of withdrawals), and reporting bias (difference between reported and unreported findings), and expressed as low risk of bias (A), moderate risk of bias (B), high risk of bias (C), or incomplete reporting leading to inability to ascertain the underlying risk of bias (D). In addition, allocation concealment explicitly distinguished as adequate (A), unclear (B), inadequate (C), or not used (D) (Table 1). Two independent and experienced reviewers (GL, GB-Z) appraised study quality, with divergences resolved by consensus.
Data analysis and synthesis
Binary outcomes from individual studies were analyzed in order to compute individual risk ratios (RR) with pertinent 95% confidence intervals (CI), and a pooled summary effect estimate was calculated by means of a fixed effects model. Statistical heterogeneity and inconsistency was measured using, respectively, Cochrane Q tests and I2. The risk of small study bias was not assessed given the inclusion of 3 studies only. Statistical significance was set at the two-tailed 0.05 level. Computations were performed with RevMan 5.0 (The Cochrane Collaboration, Copenhagen, Denmark).
Results
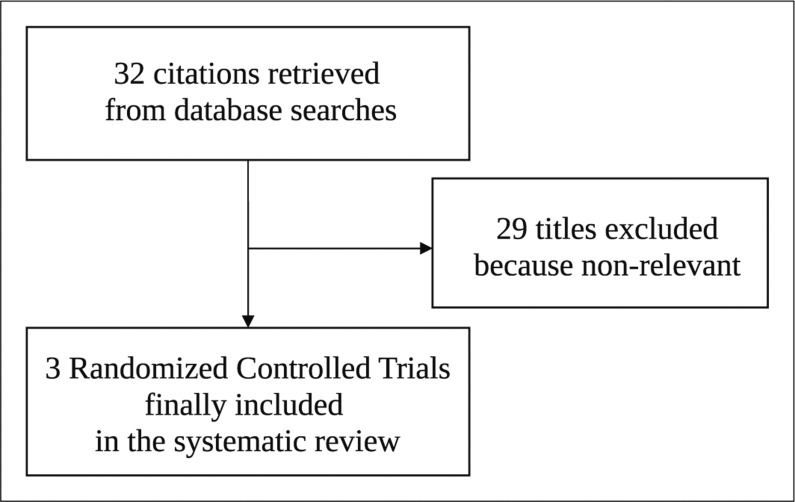
Database searches, snowballing and contacts with experts yielded a total of 32 citations (Figure 1). Excluding 29 non-pertinent titles or abstracts, we retrieved in complete form and assessed according to the selection criteria 3 studies [13,14,15]. which were included in the final analysis.
Figure 1.
Flow chart of the systematic review process (RCT=randomized clinical trial).
Study characteristics
The 3 randomized controlled studies included 3737 patients (1895 to chest-compression-only and 1842 to the standard CPR group) (Table 2). All studies were performed in non-traumatic out of hospital patients and stated that the updated international basic life support and advanced life support guidelines were strictly followed.
All studies were of high quality (Table 1) as testified by the details on the method used for randomized sequence generation and allocation, adequate allocation concealment and low risk of selection, performance, attrition and detection bias. One study employed a multicenter design, a feature which does not strictly impact on internal validity, but usually increases external validity of a trial. All studies reported on mortality.
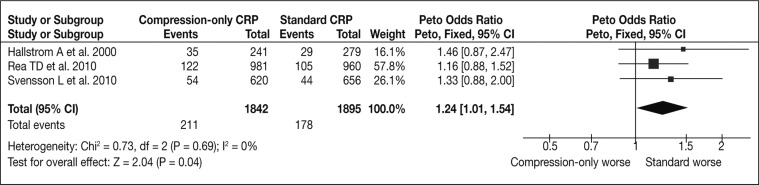
Quantitative data synthesis
Overall analysis showed that, in comparison to standard CPR, chest-compression-only was associated to increased survival at hospital discharge (211/1842 [11.5%] vs 178/1895 [9.4%], RR=1.24 [1.01-1.54], p=0.04) (Figure 2).
Figure 2.
Forest plot for the comparison of standard CPR vs compression-only CPR on hospital survival after cardiopulmonary resuscitation.
Similar results were obtained at sensitivity analyses using random-effect methods or risk differences (all p<0.05).
Only one study [13] considered the favourable neurological outcome suggesting better outcome in clinical subgroups of patients receiving chest-compression-only.
Discussion
Available evidence from randomized controlled trials strongly supports the superiority of bystander-initiated compression-only CPR, given that patients who experienced out-of-hospital cardiac arrest could be saved by limiting CPR to chest compression. These results are crucial to significantly improve the first response to out-of-hospital cardiac arrests, a worldwide major public health problem.
Previous findings from observational studies in humans [11,12,16,17] documented that spontaneously performed (i.e., not dispatcher instructed) compression-only CPR was as effective as standard CPR. In the SOS-KANTO study [10], including witnessed cardiac arrests, compression-only CPR resulted in a higher proportion of patients with a favourable neurological outcome than standard CPR in patients with apnoea, shockable rhythm and resuscitation started within 4 minutes; ventilations did not add benefits in any subgroup. On the contrary, two recent nationwide observational studies [18,19] conducted in Japan concluded that standard CPR should be preferred in out-of-hospital cardiac arrests of noncardiac origin, both in adults and in children; in this group, the two CPR techniques were similarly effective for arrests of cardiac origin. Among the tree randomized controlled studies included in this meta-analysis, only one study [15] included paediatric patients <8 years old, but results of this subgroup were not separately reported; the study by Rea et coworkers reported a tendency towards a worse efficacy of compression-only CPR than standard CPR in cardiac arrests of noncardiac origin, and a tendency towards a better efficacy in shockable rhythm and in rapid (<6 minutes) response by the Emergency medical System.
The results of the present meta-analysis are consistent with the most recent observational study on 4415 cardiac arrests not due to trauma or asphyxia, drug overdose or drowning [20], in which a 5-years data collection was accompanied by a statewide public education campaign aimed to increase bystander compression-only CPR. In this study, the incidence of bystander-initiated CPR increased every year, as did the proportion of compression-only CPR; more importantly, overall survival increased significantly over time. Overall survival to hospital discharge was equal between the no bystander CPR and the standard CPR groups, while survival and neurological outcome were significantly better in the compression-only CPR group; compression-only CPR resulted particularly effective when the cardiac arrest was witnessed and presented with a shockable rhythm. In 1128 patients with cardiac arrest of presumed noncardiac origin, not included in the study, survival was lower and not different among the two technique and no bystander CPR.
Several reasons could explain the best efficacy of chest compression-only CPR. It is well documented that both interruptions of chest compressions during ventilation and positive -pressure ventilations have detrimental effects on survival rate [8]. Oxygenation and ventilation could be allowed - at least initially- by passive ventilation during chest compressions, by spontaneous gasping and by the lungs capacity to act as a reservoir [21] In addition, compression-only CPR is easier to teach, to remember and to perform, and it does not require mouth-to-mouth contact, so resulting in a better willingness to start CPR by bystanders [20]. It is worth noting that in two of the three analyzed studies [13,15] bystanders randomly assigned to standard CPR were significantly more likely to withhold CPR than callers assigned to compression-only group.
Based on our findings, compression-only CPR should be considered as the preferred bystander CPR technique, even if ventilations still have a crucial role in cardiac arrests of presumed noncardiac origin [18], in children [19] and when resuscitation is started more than 4 minutes after the arrest. [10]. However, it should be considered that most victims of cardiac arrest are adults, and the cause is cardiac in about 2/3 of cases [20].
The importance of ventilations in cardiac arrests lasting more than 3-4 minutes is more controversial, as two recent studies in a porcine models reported contradictory results [22,23].
Likely laypersons training on CPR should be simplified to privilege compression-only CPR; in 2008 the American Heart Association already recommended that untrained bystanders should provide compression-only CPR for adults with sudden cardiac arrest [24]. However, fatigue can be a relevant problem decreasing the quality of compressions and a change of CPR providers every one minute instead of every two minutes has been suggested. [25]
Conclusions
Available evidence from randomized controlled trials suggests that compression-only CPR is superior to standard CPR at least when performed by untrained bystander. These results have relevant implications on teaching, and if adequately publicized they should favour a crucial increase in the rate of bystanders performed CPR.
Acknowledgments
We thank Lara Sussani, RA, Zuppelli Paola, RA for the support in data collection and data entry and for revising the manuscript.
Footnotes
Funding Sources: None. The study was supported by departmental funds only.
Conflict of interest No conflict of interest acknoweledged by the authors.
References
- Lloyd-Jones D, Adams R, Carnethon M. et al. Heart disease and stroke statistics - 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. circulation. 2009;119:21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- Sasson C, Rogers M A, Dahl J, Kellermann A L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- Stiell I, Nichol G H, Wells G. et al. Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. circulation. 2003;108:1939–1944. doi: 10.1161/01.CIR.0000095028.95929.B0. [DOI] [PubMed] [Google Scholar]
- Abella B S, Aufderheide T P, Eigel B. et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation. A scientific statement from the American Heart Association for healthcare providers policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- Locke C J, Berg R A, Sanders Ab. et al. Bystander cardiopulmonary resuscitation. Concerns about mouth-to-mouth contact. Arch Intern Med. 1995;155:938–943. doi: 10.1001/archinte.155.9.938. [DOI] [PubMed] [Google Scholar]
- Cho C G, Sohn Y D, Kang K H. et al. The effect of basic life support education on laypersons\' willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81:691–694. doi: 10.1016/j.resuscitation.2010.02.021. [DOI] [PubMed] [Google Scholar]
- Berg R A, Kern K B, Hilwig R W. et al. Assisted ventilation does not improve outcome in a porcine model of single-rescuer bystander cardiopulmonary resuscitation. Circulation. 1997;95:1635–1641. doi: 10.1161/01.cir.95.6.1635. [DOI] [PubMed] [Google Scholar]
- Ewy G A, Zuercher M, Hilwig R W. et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation. 2007;116:2525–2530. doi: 10.1161/CIRCULATIONAHA.107.711820. [DOI] [PubMed] [Google Scholar]
- Dorph E, Wik L, Stromme T A. et al. Oxygen delivery and return of spontaneous circulation with ventilation: compression ratio 2:30 versus chest compressions only CPR in pigs. Resuscitation. 2004;64:309–318. doi: 10.1016/j.resuscitation.2003.12.001. [DOI] [PubMed] [Google Scholar]
- SOS-KANTO study group . Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet. 2007;369:920–926. doi: 10.1016/S0140-6736(07)60451-6. [DOI] [PubMed] [Google Scholar]
- Bohm V, Rosenqvist M, Herlitz J. et al. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116:2908–2912. doi: 10.1161/CIRCULATIONAHA.107.710194. [DOI] [PubMed] [Google Scholar]
- Iwami T, Kawamura T, Hiraide A. et al. Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation. 2007;116:2900–2907. doi: 10.1161/CIRCULATIONAHA.107.723411. [DOI] [PubMed] [Google Scholar]
- Rea T D, Fahrenbruch C, Culley L. et al. CPR with chest compression alone or with rescue breathing. N Engl J Med. 2010;636:423–433. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- Svensson L, Bohm K, Castren M. et al. Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N Engl J Med. 2010;636:434–442. doi: 10.1056/NEJMoa0908991. [DOI] [PubMed] [Google Scholar]
- Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. N Engl J Med. 2000;342:1546–1553. doi: 10.1056/NEJM200005253422101. [DOI] [PubMed] [Google Scholar]
- Ong M E, Ng F S, Anushia P. et al. Comparison of chest compression and standard cardiopulmonary resuscitation for out-of-hospital cardiac arrest in Singapore. Resuscitation. 2008;78:119–126. doi: 10.1016/j.resuscitation.2008.03.012. [DOI] [PubMed] [Google Scholar]
- Waalewijn R A, Tijssen J G, Koster R B. Bystander initiated actions in out-of-hospital cardiopulmonary resuscitation: results from the Amsterdam Resuscitation Study (ARRESUST). Resuscitation. 2001;50:273–279. doi: 10.1016/s0300-9572(01)00354-9. [DOI] [PubMed] [Google Scholar]
- Kitamura T, Iwami T, Kawamura T. et al. By-stander initiated rescue breathing for out-of-hospital cardiac arrests of noncardiac origin. Circulation. 2010;122:293–299. doi: 10.1161/CIRCULATIONAHA.109.926816. [DOI] [PubMed] [Google Scholar]
- Kitamura T, Iwami T, Kawamura T. et al. onventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective nationwide population-based cohort study. Lancet. 2010;375:1321–1322. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- Bobrow B J, Spaite D W, Berg R A. et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- Berg R A, Nadkarni V M. Hands-only cardiopulmonary resuscitation: bench-to-bedside or bedside-to-bench? Crit Care Med. 2010;38:2073–2075. doi: 10.1097/CCM.0b013e3181f3ddb1. [DOI] [PubMed] [Google Scholar]
- Yannopoulos D, Matsuura T, McKnite S. et al. No assisted ventilation cardiopulmonary resuscitation and 24-hour neurological outcomes in a porcine model of cardiac arrest. Crit Care Med. 2010;38:254–260. doi: 10.1097/CCM.0b013e3181b42f6c. [DOI] [PubMed] [Google Scholar]
- Wang S, Li C, Ji X. et al. Effect of continuous compressions and 30:2 cardiopulmonary resuscitation on global ventilation/perfusion values during resuscitation in a porcine model. Crit Care Med. 2010;38:2024–2030. doi: 10.1097/CCM.0b013e3181eed90a. [DOI] [PubMed] [Google Scholar]
- Sayre M R, Berg R A, Cave D M. et al. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- Nishiyama C, Iwami T, Kawamura T. et al. Quality of chest compressions during continuous CPR: comparison between chest compression-only CPR and conventional CPR. Resuscitation. 2010;81:1151–1155. doi: 10.1016/j.resuscitation.2010.05.008. [DOI] [PubMed] [Google Scholar]