Abstract
Background
There is no consensus on which drugs/techniques/strategies can affect mortality in the perioperative period of cardiac surgery. With the aim of identifying these measures, and suggesting measures for prioritized future investigation we performed the first international consensus conference on this topic.
Methods
The consensus was a continuous international internet-based process with a final meeting on June 28th 2010 in Milan at the Vita-Salute University. Participants included 340 cardiac anesthesiologists, cardiac surgeons and cardiologists from 65 countries all over the world. A comprehensive literature review was performed to identify topics that subsequently generated position statements for discussion, voting and ranking.
Results
Of the 17 major topics with a documented mortality effect, seven were subsequently excluded after further evaluation due to concerns about clinical applicability and/or study methodology. The following topics are documented as reducing mortality: administration of insulin, levosimendan, volatile anesthetics, statins, chronic beta-blockade, early aspirin therapy, the use of preoperative intra-aortic balloon counterpulsation and referral to high-volume centers. The following are documented as increasing mortality: administration of aprotinin and aged red blood cell transfusion. These interventions were classified according to the level of evidence and effect on mortality and a position statement was generated.
Conclusion
This international consensus conference has identified the non-surgical interventions that merit urgent study to achieve further reductions in mortality after cardiac surgery: insulin, intra-aortic balloon counterpulsation, levosimendan, volatile anesthetics, statins, chronic beta-blockade, early aspirin therapy, and referral to high-volume centers. The use of aprotinin and aged red blood cells may result in increased mortality.
Keywords: anesthesia, intensive care, cardiac anesthesia, cardiac surgery, mortality, cardiopulmonary bypass, consensus development conference, treatment outcome, focused update, prevention and control
Introduction
Every year over one million patients worldwide undergo cardiac surgery [1] and are exposed to significant morbidity and mortality.
Many drugs, techniques and management strategies have been used in an attempt to reduce this mortality.
Currently no consensus exists as to their effect either positive or negative on patient mortality. The goal of this first International Consensus Conference was to identify these ancillary (i.e. non-surgical) interventions; to quantify their impact either positive or negative on all-cause mortality in cardiac surgery; and then to make suggestions to both researchers and donors as to which topics deserve further investigation in the immediate future.
Methods
Cardiac anaesthesiologists, cardiac surgeons, and cardiologists participated in person, through email or through the congress website.
In the period May 2008 - June 2010 a core group of experts in the field undertook a comprehensive review of the published evidence related to the prevention of perioperative mortality in cardiac anesthesia and intensive care.
Each participant suggested one or more topics of interest and submitted them electronically together with one or more articles published in peer-reviewed journals supporting their opinion.
Over 100 international anesthesiology and cardiac surgery scientific societies were contacted and asked to disseminate information about the Consensus Conference (either via email or by means of website links) to allow their authoritative representatives to participate. All journals with an impact factor in the fields of Anesthesiology, Critical Care Medicine, Cardiac and Cardiovascular Systems were contacted and asked to suggest seminal papers to be included in the Consensus Conference.
Over 50 patient and nurse associations were contacted via email and asked to disseminate information about the conference to their members.
The following PubMed search strategy (updated on June 28th 2010) was used to systematically identify related topics: systematic[sb] AND (surgery[tiab] OR surgic*[tiab] OR operation*[tiab]) AND ((myocardial AND infarction) OR (death* OR survival OR mortality OR prognosis)) AND (prevent* OR reducti* OR reduci*).
Participants were asked to suggest topics with the following inclusion criteria:
a) a study published in a peer-reviewed journal;
b) including ancillary (i.e. non-surgical) treatments (drug/technique/strategy) in patients undergoing cardiac surgery;
c) with a statistically significant reduction/increase in mortality.
Only studies that fulfilled all these criteria were accepted as valid for study inclusion. Between June 20th to June 28th 2010, a web site allowed participants the opportunity to vote in support of or against the suggested topics or to suggest new topics, as well as the opportunity to produce scientific articles in support of the different drugs/techniques/strategies. Specific aims of the Consensus Conference were to establish whether:
a) the most recent evidence had been collected;
b) the reduction or increase in mortality was supported by either: randomized controlled trials or meta-analyses of randomized controlled trials, case-matched studies, meta-analyses of case matched studies, or other studies;
c) the evidence had been derived from a subgroup or a primary analysis;
d) the evidence had been derived entirely or partially from cardiac-surgical population; and when among a cardiac surgical population, if it was applicable to every cardiac intervention or to certain subgroups only;
e) the drug/technique/strategy was used in the operative room or in an intensive care unit;
f) mortality was the endpoint, or mortality was included in a composite endpoint.
The Consensus was a continuous interactive web-based process, with the main, final meeting held on June 28th 2010 at the Vita-Salute University of Milan, Italy when all 120 suggested topics were discussed.
Major and minor topics where identified according to the presence or not of at least one article showing a statistically significant reduction/increase in mortality.
After a presentation from both a rapporteur and a co-rapporteur a short statement was drawn up for each major topic describing the reasons for it being considered as providing convincing (Table 1), or non convincing (Table 2) evidence.
Table 1a.
Ten major ancillary (i.e. non-surgical) drugs/techniques/strategies that might influence survival rates in patients undergoing cardiac surgery are presented here in order of level of evidence-based-medicine together with the percentage of agreement that was reached among the partecipant of the Consensus Conference.
Table 1b.
Abbreviation RCT: Randomized controlled trial; IABP: Intra-aortic balloon pump; CABG:Coronary artery bypass grafting; EF: Ejection fraction; LV: Left Ventricle
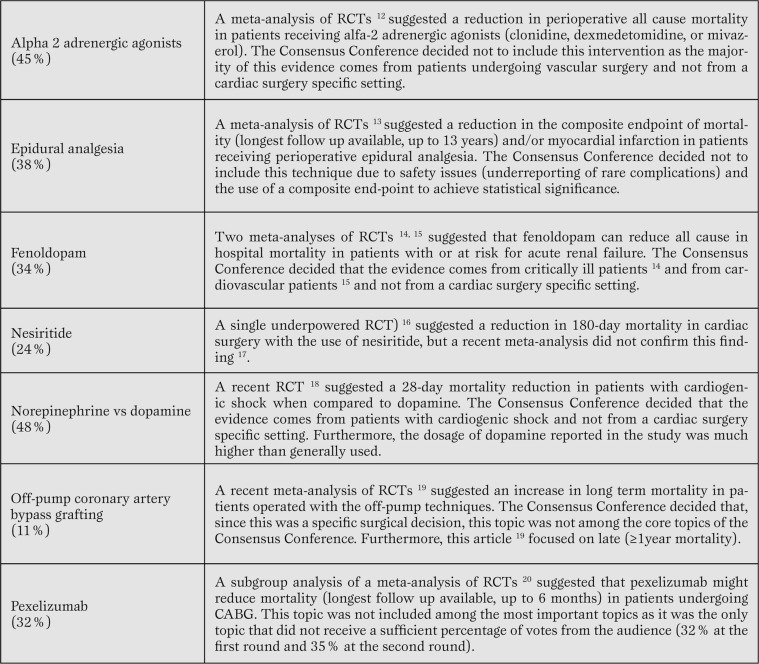
Table 2.
Seven drugs/techniques/strategies had at least one study showing a statistically significant difference in support of their effect on mortality. Despite this the Consensus Conference decided not to include them among the most important topics fot the reasons provided below. In addition we have reported the percentage of partecipants that proposed the intervention as having an effect on mortality during the first web-vote.
Thus, for each convincing major topic the Consensus Conference approved a position statement, and highlighted the appropriate peer-reviewed published evidence.
Final statements were created, discussed and corrected during the conference and later on exposed to the judgment of all the web participants: from June 29th to September 30th 2010 participants were asked to support or challenge the findings and statements from the meeting via a web questionnaire and were asked again to disclose any potential conflict of interest.
The Consensus Conference decided not to address echocardiography and the drugs/techniques/strategies already addressed in the guidelines for the management of Sepsis and ARDS, and for peri-operative blood conservation and transfusions.
Results
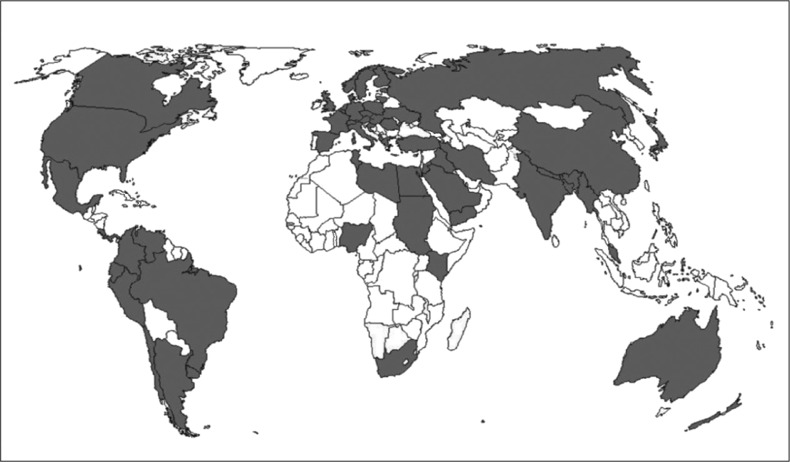
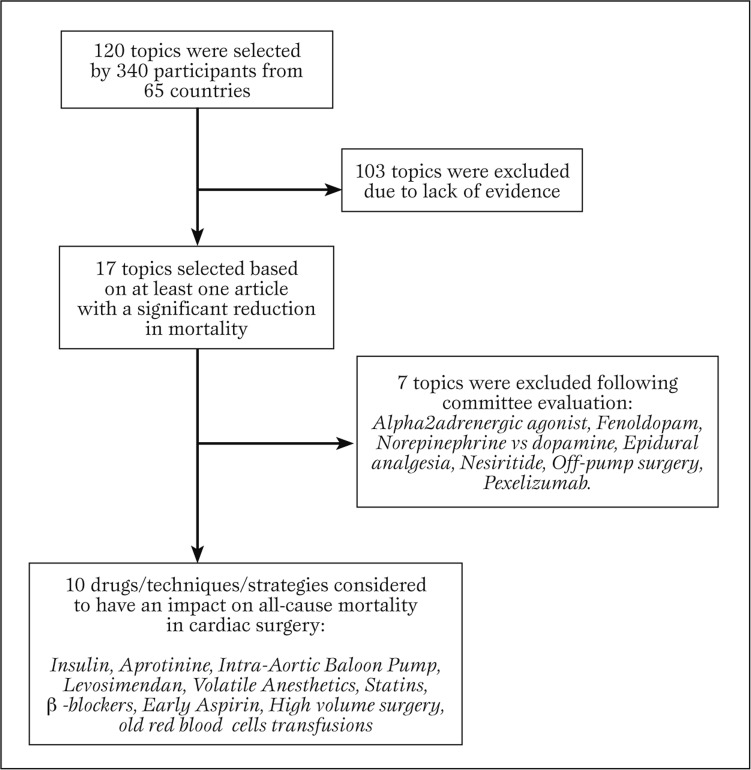
Three-hundred-forty participants from 65 countries (Figure 1 and Figure 2) suggested 120 topics: 17 of them were supported by an article with a significant effect on mortality [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,16,17,18,19,20] while 103 topics were not (Figure 3).
Figure 1.
The 65 countries that partecipated in the consensus conference
Figure 2.
Most European countries partecipated in the consensus conference
Figure 3.
Flow chart on the selection of major topics (from the 120 suggested topics to the identification of the topics with a statistically significant effect on perioperative mortality in cardaic surgery).
Ten drugs/techniques/strategies were considered to have evidence strong enough to support their effect on mortality and are listed in table 1 together with a consensus statement.
The level of agreement of participants before and after the meeting of Milan on June 28th is detailed in table 1 and 2 with 214 and 150 participants voting at the first and second round respectively.
Declared conflict of interests ranged from 2% (IABP, statins) to 6% (levosimendan, volatile agents) without affecting results and percentages of agreement.
Seven topics with an article supporting their effect on mortality were not included among the final topics and are listed in table 2 with the reasons for their exclusion.
The suggested topics without at least one peer reviewed published article to support their effect on mortality were either eliminated (if not deemed of potential value) or grouped and summarized as minor topics in table 3 (if considered of potential value).
Table 3.
Minor topics (without a statistically significant study to support their effect on mortality).
The Consensus Conference stated that these minor topics might be beneficial/detrimental in terms of survival in the perioperative setting, but acknowledged that there is still no evidence base to support them.
Discussion
This is the first consensus statement of its kind examining non-surgical interventions aimed at reducing mortality in cardiac surgery. It was hoped that its creation would provide a starting point for researchers and donors as well as serve as a guide for clinicians. The findings contained in this document provide then, for the first time, a comprehensive review of these non-surgical interventions.
The majority of the interventions described as potentially having an impact on mortality (Table 1) are cheap and simple to perform which hold the promise that their worldwide adoption or in some cases avoidance, could have a significant impact on cardiac mortality worldwide. To realise the potential life saving effects of these interventions it is imperative that steps be taken to validate these findings. This should be in the form of an RCT large enough to detect a reduction in mortality. It is sobering to realise that no randomized clinical trial of more than 10,000 patients has ever been conducted in the field of perioperative cardiac surgery.
It is reasonable to assume that these findings may, at least in part, be applicable to non-cardiac surgery and general intensive care settings. As these populations are much larger their use may result in even greater mortality reductions.
The Consensus Conference identified seven other interventions with a potential effect on mortality (Table 2).
These were excluded for a wide range of reasons ranging from concerns regarding study endpoints to the exclusion of studies conducted in populations other than cardiac surgery. Their exclusion does not reflect a rejection of the intervention in its entirety and there is value in further investigating these interventions.
Systematic reviews with meta-analysis have become popular in the anesthesia and surgical literature and currently dominate the evidence based hierarchy [21].
They have a high impact on healthcare decision makers, clinicians, and patients alike and are a guide to decision making with a similar clarity to that of randomized trials. To gain maximal benefit from systematic reviews it would be beneficial if researchers adopt a standardised manner of randomized study reporting.
This would significantly improve the ability to compare various studies with each other. Furthermore, researchers, reviewers and editorial boards of peer reviewed journal should understand the importance of reporting clinically relevant outcomes with the intention to treat analysis even when publishing small RCTs focusing on surrogate endpoints.
The manner in which this conference has been conducted is a reflection of how use can be made of current electronic resources to maximise participation and more importantly to ensure that all relevant clinical information is identified and evaluated.
With the ever increasing proliferation of clinical evidence this consensus conference may serve as a model on how to synthesis and disseminate clinically relevant information.
In a field such as cardiac surgery where patients are still faced with a high risk of perioperative morbidity and mortality it is imperative to foster the dissemination of results that may impact on patient outcome.
It is interesting to note that the two interventions that received the highest percentage of support (beta-blockers - 94% and the use of early aspirin - 87%) received this support without there being any RCTs or meta-analysis of RCTs regarding their use in cardiac surgery.
This suggests that clinicians and scientists are not fully aware or do not completely agree with the evidence based hierarchy. It may in addition reflect a tendency to extrapolate findings from one aspect of medicine and apply it to another without consideration to the levels of support for these actions.
Finally all 17 of the papers described in table 1 and 2 were published in the last decade, suggesting that scientific awareness and investigation into this field is rapidly increasing.
Limitations of the present work - In general there is a dearth of evidence based medicine in this sector of cardiac surgery. Only two out of ten major papers described large RCTs, and three papers were meta-analysis of small RCTs.
The other five papers were either non-RCTs or meta-analysis including non-RCTs, testifying the paucity of large RCTs in this specific setting.
Conclusions
By conducting a comprehensive updated International Consensus Congress we have identified all the ten ancillary drugs/techniques/strategies that might reduce mortality in cardiac surgery.
We thus suggest that future research and funding be directed toward these topics.
Endorsements
The Consensus Conference was endorsed by the Italian Ministry of Health, the Italian Association of Cardiothoracic Anesthesiologists (ITACTA), the Italian Society for Cardiac Surgery (SICCH), the Meta-analysis and Evidence-based Medicine Training in Cardiology (METCARDIO), EXPO Milano 2015, the SIAARTI (Società Italiana Analgesia Anestesia Rianimazione Terapia Intensiva) study group of cardiothoracic and vascular anesthesia, the Colombian Cardiovascular Committee of the Colombian Anesthesia Society, and the Italian Critical Care Nurses Association (AISACE).
Acknowledgments
Participants from the following 65 countries, listed in alphabetical order, contributed to the conference: Albania, Argentina, Australia, Austria, Azerbaijan, Bahrain, Bangladesh, Belgium, Brazil, Canada, Chile, China, Colombia, Costa Rica, Croatia, Czech Republic, Denmark, Ecuador, Egypt, Estonia, Finland, France, Georgia, Germany, Greece, Hungary, India, Iran, Iraq, Italy, Japan, Jordania, Kenya, Libya, Lithuania, Malaysia, Mexico, Myanmar, Nederland's, Nepal, New Zeland, Nigeria, Norway, Panama, Peru, Poland, Romania, Russia, Saudi Arabia, Slovak Republic, South Africa, Spain, Sudan, Sweden, Seitzerland, Taiwan, Tunisia, Turkey, Turks and Caicos, Uruguay, UK, Ukraine, USA, Venezuela, Yemen.
Abbreviations
- CABG
Coronary artery bypass grafting
- EF
Ejection fraction
- IABP
Intra-aortic balloon pump
- LV
Left ventricle
- RCT
Randomized controlled trial
Footnotes
Source of Support The consensus conference was supported by departmental funds only. Dr R.N. Rodseth is supported by a CIHR Scholarship (the Canada-HOPE Scholarship).
Conflict of interest Landoni G. received speaker fees from: Abbot, Baxter, Minrad, Cephalon, Orion. Caramelli F. received speaker fees from Cephalon.
Cite as: Landoni G, Augoustides JG, Guarracino F, Santini F, Ponschab M, Pasero D, Rodseth RN, Biondi-Zoccai G, Silvay G, Salvi L, Camporesi E, Comis M, Conte M, Bevilacqua S, Cabrini L, Cariello C, Caramelli F, De Santis V, Del Sarto P, Dini D, Forti A, Galdieri N, Giordano G, Gottin L, Greco M, Maglioni E, Mantovani L, Manzato A, Meli M, Paternoster G, Pittarello D, Rana NK, Ruggeri L, Salandin V, Sangalli F, Zambon M, Zucchetti M, Bignami E, Alfieri O, Zangrillo A. Mortality reduction in cardiac anesthesia and intensive care: results of the first International Consensus Conference. HSR Proceedings in Intensive Care and Cardiovascular Anesthesia 2011; 3 (1): 9-19
References
- DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Report. 2008;30:1–20. [PubMed] [Google Scholar]
- Van den Berghe G, Wouters P, Weekers F. et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- Fergusson DA, Hébert PC, Mazer CD. BART Investigators et al. A comparison of aprotinin and lysine analogues in high-risk cardiac surgery. N Engl J Med. 2008;358:2319–2331. doi: 10.1056/NEJMoa0802395. [DOI] [PubMed] [Google Scholar]
- Field ML, Rengarajan A, Khan O. et al. Preoperative intra aortic balloon pumps in patients undergoing coronary artery bypass grafting. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD004472.pub2. [DOI] [PubMed] [Google Scholar]
- Landoni G, Mizzi A, Biondi-Zoccai G. et al. Reducing mortality in cardiac surgery with levosimendan: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. 2010;24:51–57. doi: 10.1053/j.jvca.2009.05.031. [DOI] [PubMed] [Google Scholar]
- Landoni G, Biondi-Zoccai GG, Zangrillo A. et al. Desflurane and sevoflurane in cardiac surgery: a meta-analysis of randomized clinical trials. J Cardiothorac Vasc Anesth. 2007;21:502–511. doi: 10.1053/j.jvca.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Takagi H, Kawai N, Umemoto T. Preoperative statin therapy reduces postoperative all-cause mortality in cardiac surgery: a meta-analysis of controlled studies. J Thorac Cardiovasc Surg. 2009;137:52–53. doi: 10.1016/j.jtcvs.2008.02.045. [DOI] [PubMed] [Google Scholar]
- Ferguson TB Jr, Coombs LP, Peterson ED. Preoperative beta-blocker use and mortality and morbidity following CABG surgery in North America. JAMA. 2002;287:2221–2227. doi: 10.1001/jama.287.17.2221. [DOI] [PubMed] [Google Scholar]
- Mangano DT. Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002;347:1309–1317. doi: 10.1056/NEJMoa020798. [DOI] [PubMed] [Google Scholar]
- Birkmeyer JD, Stukel TA, Siewers AE. et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- Koch CG, Li L, Sessler DI. et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;358:1229–1239. doi: 10.1056/NEJMoa070403. [DOI] [PubMed] [Google Scholar]
- Wijensundera DN, Bender JS, Beattie WS. et al. Alpha-2 adrenergic agonists for the prevention of cardiac complications among patients undergoing surgery. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD004126.pub2. [DOI] [PubMed] [Google Scholar]
- Bignami E, Landoni G, Biondi-Zoccai GG. et al. Epidural analgesia improves outcome in cardiac surgery: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. 2010;24:586–597. doi: 10.1053/j.jvca.2009.09.015. [DOI] [PubMed] [Google Scholar]
- Landoni G, Biondi-Zoccai GG, Tumlin JA. et al. Beneficial impact of fenoldopam in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Am J Kidney Dis. 2007;49:56–68. doi: 10.1053/j.ajkd.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Landoni G, Biondi-Zoccai GG, Marino G. et al. Fenoldopam reduces the need for renal replacement therapy and in-hospital death in cardiovascular surgery: a meta-analysis. J Cardiothorac Vasc Anesth. 2008;22:27–33. doi: 10.1053/j.jvca.2007.07.015. [DOI] [PubMed] [Google Scholar]
- Mentzer RM Jr, Oz MC, Sladen RN. et al. Effects of perioperative nesiritide in patients with left ventricular dysfunction undergoing cardiac surgery: the NAPA Trial. J Am Coll Cardiol. 2007;49:716–726. doi: 10.1016/j.jacc.2006.10.048. [DOI] [PubMed] [Google Scholar]
- Nigwekar SU, Hix JK. The role of natriuretic peptide administration in cardiovascular surgery-associated renal dysfunction: a systematic review and meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. 2009;23:151–160. doi: 10.1053/j.jvca.2008.11.007. [DOI] [PubMed] [Google Scholar]
- De Backer D, Biston P, Devriendt J. et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362:779–789. doi: 10.1056/NEJMoa0907118. [DOI] [PubMed] [Google Scholar]
- Takagi H, Matsui M, Umemoto T. et al. Off-pump coronary artery bypass may increase late mortality: a meta-analysis of randomized trials. Ann Thorac Surg. 2010;89:1881–1888. doi: 10.1016/j.athoracsur.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Testa L, Van Gaal WJ, Bhindi R. et al. Pexelizumab in ischemic heart disease: a systematic review and meta-analysis on 15,196 patients. J Thorac Cardiovasc Surg. 2008;136:884–893. doi: 10.1016/j.jtcvs.2007.12.062. [DOI] [PubMed] [Google Scholar]
- Biondi-Zoccai GG, Agostoni P, Abbate A. Parallel hierarchy of scientific studies in cardiovascular medicine. Ital Heart J. 2003;4:819–820. [PubMed] [Google Scholar]