Abstract
AIM
To investigate the efficacy of Ferrara rings (FR) implantation in the treatment of keratoconus.
METHODS
It was a retrospective case series descriptive study. The sample was comprised of 50 patients 79 eyes diagnosed with progressive keratoconus. This included 24 (48%) males and 26 (52%) females between the age of 13 and 44 years. All participants underwent surgical implantation of FR in the period between January 2009 and September 2010 at Jordan University Hospital. Thorough ophthalmologic examinations were applied to measure vital variables for each pathological condition before and after surgery.
RESULTS
Findings indicated an overall significant postoperative improvement in both uncorrected visual acuity (UCVA) and best spectacle corrected visual acuity (BSCVA) throughout follow up visits. Moreover, results illustrated a significant decrease in spherical equivalent (SE) and keratometric readings (lower, higher and the average).
CONCLUSION
Surgical intervention strategies are being frequently developed to meet the needs of patients with keratoconus. The implantation of Ferrara rings has proven to be a safe and feasible alternative procedure for the treatment of mild-moderate keratoconus especially for patients with contact lenses intolerance. We have found that this procedure has improved visual outcomes in all eyes studied. Nevertheless, further research is needed to investigate long term outcomes.
Keywords: cornea, keratoconus, Ferrara rings, intracorneal ring segments.
INTRODUCTION
Keratoconus is a bilateral, progressive non-inflammatory corneal ectasia that tends to affect young age groups in their late teens[1]. Despite intensive clinical and laboratory investigations, its precise etiology is unknown[2],[3]. In keratoconus, corneal changes result in a mild to severe decrease in the best corrected visual acuity (BCVA) as a result of progressive myopia, regular and irregular astigmatism, in addition to apical scarring in advanced cases[4].
Although the treatment offered is based mainly on the stage of the disease and its progression, nevertheless, management of keratoconus tends to be a complex process. In early stages of keratoconus, management options included spectacles and rigid gas-permeable (RGP) contact lenses. Due to advances in material technology, the variety and quality of techniques and tools available to ophthalmologists have improved drastically in recent years. Typically today, advanced stages require invasive techniques such as intrastromal corneal ring segments (ICRS), phakic intraocular lenses, corneal collagen cross linking (CXL), deep anterior lamellar keratoplast and penetrating keratoplasty[5]. CRS were first introduced to correct mild-moderate myopia[6],[7] and has been investigated as a surgical option for keratoconus correction to delay or avoid corneal grafting[8]. ICRSs act by exerting an “arc-shortening effect” on the corneal lamellae that flattens the central cornea. This procedure is considered safe and reversible as no corneal tissue is removed[9]. All the commercially available ICRS are made of polymethylmethacrylate (PMMA). Ferrara rings (Mediphacos, Inc., Belo Horizonte, Brazil) are characterized by triangular cross-sections that induce a prismatic effect on the cornea when the flat posterior surface is inserted facing the corneal endothelium. The optical zone provided by the segments is 5.0mm in diameter. The objective of this study is to assess the efficacy of Ferrara rings in the treatment of keratoconus.
SUBJECTS AND METHODS
Subjects
This research was undertaken at Jordan University Hospital. An ethical approval was obtained from the institutional review board. A total of 50 patients 79 eyes took part in this retrospective case series descriptive study. This included 24 males (48%) and 26 females (52%) diagnosed with progressive Keratoconus. All patients underwent surgical implantation of Ferrara rings in the period between January 2009 and September 2010 at Jordan University Hospital. Ages of participants ranged between 13 and 44 years with a mean age of 25.26 (SD=5.84). Participants' demographic characteristics were shown in Table 1.
Table 1. Characteristics of the study population.
| Variable | n (%) |
| Demographic factors | |
| Gender | |
| Males | 24 (48) |
| Females | 26 (52) |
| Age mean ± SD years | 25.26±5.84 |
| Operative related factors | |
| Right eye | 43 (54.4) |
| Left eye | 36 (45.6) |
Patients' inclusion criteria included: progressive keratoconus determined by keratometric values ≥ 1D over one year, severely affected visual acuity and contact lens intolerance in addition to irregular astigmatism with at least one clinical sign of keratoconus such as Vogt's striae or thin vertical streaks located in the posterior corneal stroma. On the other hand, patients with corneal opacity or corneal dystrophy as well as patients who failed to attend any of the follow up visits were excluded from this study. Patients' preoperative ophthalmologic examinations indicated that uncorrected visual acuity (UCVA) ranged between 0.05 and 0.60 with a mean of 0.17 (SD=0.13), best spectacles corrected visual acuity (BSCVA) ranged between 0.05 and 1.00 with a mean of 0.48 (SD=0.23), higher keratometric readings (KS) between 35 and 68 (52.73±5.73), lower keratometric readings (KF) between 39 and 65 (48.17±4.87), Spheres between -14 and 3 (-3.32±3.52), Cylinders between -8 and 0.00 (-4.19±1.59), Axis between -3.25 and 180 (90.25±57.31) and Spherical Equivalents (SE) between -15.50 and 1.00 (-3.40±3.42). Patients' postoperative data displayed in table (3) were utilized for comparisons purposes (Table 2).
Table 3. Ferrara rings technical specifications.
| Parameter | Ferrara rings |
| Variable apical diameter | 5.0mm-6.0mm |
| Cross- section | Triangular |
| Segments/each | 90, 120, 140, 160 or 210 degrees |
| Hole | 0.20mm in each end |
| Segments thickness | 0.15mm-0.35mm |
| Base | 0.60mm |
Table 2. Postoperative data.
| Variable | One-month follow up |
Three-month follow up |
Six-month follow up |
|||
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | |
| UCVA | 0.37 (0.18) | 0.05-0.8 | 0.41 (0.17) | 0.05-0.9 | 0.44 (0.18) | 0.10-1 |
| BSCVA | 0.51 (0.17) | 0.1-1 | 0.57 (0.21) | 0.10-1 | 0.62 (0.20) | 0.20-1 |
| Ks | 48.53 (5.23) | 35-67 | 48.17 (4.83) | 37-66 | 48.44 (4.99) | 37-67 |
| Kf | 45.26 (4.79) | 33-63 | 45.19 (5.12) | 33-65 | 45.63 (4.54) | 36-63 |
| Km | 46.88 (4.90) | 34-65 | 46.57 (4.76) | 35-64.5 | 46.79 (4.74) | 35.50-65 |
| Sphere | -1.08 (2.45) | -14-5 | -0.67 (1.83) | -7-4 | -0.65 (1.49) | -4-5 |
| Cylinder | -3.05 (1.70) | -8-0.00 | -2.86 (1.42) | -6-0.00 | -2.87 (1.67) | -6.50-1 |
| Axis | 91.39 (52.52) | 0.00-180 | 86.02 (49.24) | 0.00-180 | 89.14 (50.31) | -3.75-180 |
| SE | -2.32 (2.75) | -14-9.25 | -2.16 (1.86) | -8-2.63 | -2.04 (1.92) | -7-5 |
SD (standard deviation).
(n=79)
Methods
FR segments were used based on the nomogram provided by the manufacturer. Procedures adhered to the Declaration of Helsinki for research involving human subjects. All patients provided informed consent before surgery. Surgeries were performed in the operating room under sterile conditions by the same surgeon under topical anesthetic drops (Benoxinate 0.4%) except for 4 cases where patients requested general anesthesia.
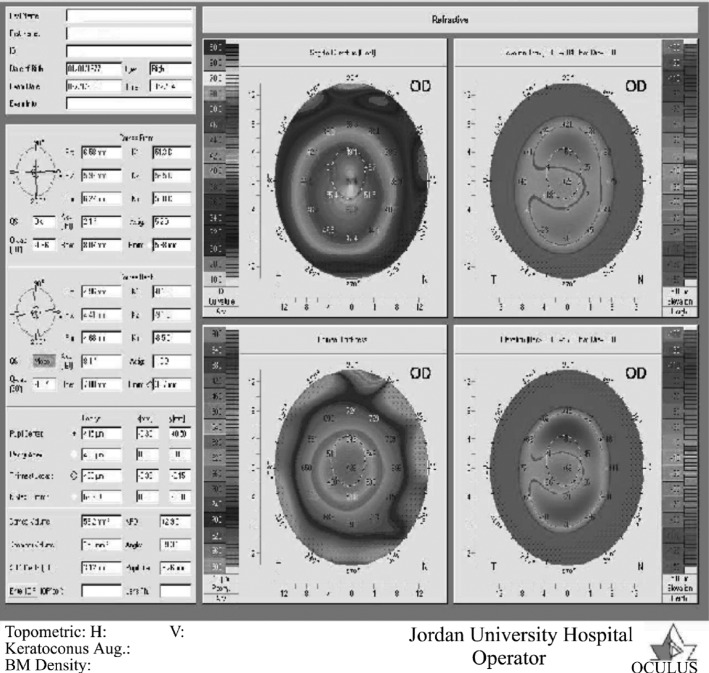
The center of the cornea was determined by asking the patient to fixate the center of the coaxial microscope bulb filament and then the center is marked with a methylene blue marker using a Sinskey hook. Based on preoperative corneal topography (Pentacam from Oculus) (Figure 1), the steepest corneal meridian was marked utilizing a special marker which also marked the exact ring tunnel with an inner zone of 5.00mm and an outer zone of 7.00mm in diameter.
Figure 1. Abu ameerh. Preoperative corneal topography (pentacam from oculus).
With a 1mm wide square blade diamond knife, the initial incision was made on the marked steepest meridian at 80% depth of the thinnest corneal thickness of the tunnel. After pocketing the incision site, one or two concentric stromal corneal tunnels with an internal radius of curvature of 2.50mm and an extension of 160 degrees were created and the ring segment or segments were implanted in the tunnel. No sutures were placed and a soft bandage contact lens was applied for 48 hours. A combination of Chloramphenicol and dexamethasone eye drops was used every four hours for 14 days. Patients were instructed to avoid eye rubbing. Technical specifications for Ferrara rings used in this procedure were displayed (Table 3).
Statistical Analysis
Statistical analysis was performed using SPSS version 17[10]. Descriptive statistics were presented to describe participants and study variables. Differences between pre and post- operative data were investigated using one way repeated- measures ANOVA (P< 0.05). Furthermore, Mauchly's test of sphericity was carried out to examine whether there was any violation of the sphericity assumption. The Greenhouse-Geisser correction was applied to manage this violation. Post hoc tests with a Bonferroni correction (P< 0.008) were performed to allocate differences between visits.
Results
Seventy-nine eyes of 50 patients with Keratoconus who underwent a surgical procedure to implant Ferrara ring segments, at Jordan University Hospital, were included in this study. The sample consisted of 24 males and 26 females. Prior to the main analysis; a number of checks were carried out on the data. One way repeated measures ANOVA with a Greenhous-Geisser correction indicating that UCVA differed statistically between visits, F (2.75, 234) =68.27, P=0.00 with an effect size of 0.46. Post hoc tests using a Bonferroni correction revealed that UCVA increased significantly from the preoperative visit (0.17±0.13) after one month (visit 1), three months (visit 2) and six months (visit 3) (0.37±0.18), (0.41±0.17) and (0.44±0.18) respectively with P=0.00. Moreover, a comparison between postoperative data showed a significant increase in UCVA from (0.37±0.18) in visit 1 to (0.44±0.18) in visit 3, P=0.01.
Comparisons of BSCVA revealed statistical differences between visits, F (2.35, 234) =13.08, P=0.00 with an effect size of 0.14. Results illustrate a significant increase in BSCVA at visit 2 (0.57±0.21) and visit 3 (0.62±0.20) when compared to the preoperative visit (0.48±0.23) with P=0.01 and P=00 respectively. In addition, significant increases were also reported at visit 2 (0.57±0.21), P=0.01 and visit 3 (0.62±0.20), P=0.00 compared to visit 1 (0.51±0.17).
There was also statistical differences in Ks between visits, F (1.54, 234) =96.55, P=0.00 with an effect size of 0.55. Comparisons between the preoperative visit and visit 1, visit 2 and visit 3 produced a significant decrease (52.73±5.73), (48.53±5.23), (48.17±4.83) and (48.14±4.99) respectively, P=0.00. Comparisons of lower keratometric readings (Kf) demonstrate an overall statistical difference between visits, F (2.29, 234)=47.38, P=0.00 with an effect size of 0.37. Results confirm a significant decrease between the preoperative visit (48.17±4.87) and all three follow up visits 1 through visit 3 (45.26±4.79), (45.19±5.12) and (45.63±4.54) respectively with P=0.00.
Results also proved statistical differences between visits in the keratometric readings average (Km), F (1.84, 234) =134.59, P=0.00 with an effect size of 0.63. Comparisons denote a significant decrease between the preoperative visit (50.50±5.08) and visit 1 (46.88±4.90), visit 2 (46.57±4.76) and visit 3 (46.79±4.74).
Comparisons of Sphere data show statistical differences between different visits, F (1.95, 234) =38.21, P=0.00 with an effect size of 0.32. A significant increase was reported when comparing the preoperative visit (-3.32±3.52) to visit 1 (-1.08±2.45), visit 2 (-0.67±1.83) and visit 3 (-0.65±1.49), P=0.00.
Additionally, Cylinder data display statistical differences between visits, F (2.47, 234) =19.63, P=0.00 with an effect size of 0.20. Results exhibit a significant increase when comparing the preoperative visit (-4.19±1.59) to visit 1, 2 and 3 (-3.05±1.70), (-2.86±1.42) and (-2.87±1.67) respectively.
Non significant statistical Differences were identified in the values of Axis between different visits, F (2.69, 234) =0.17, P=0.90 with an effect size of 0.002. Results illustrate a non significant increase between the preoperative visit (90.25±59.31) and visit 1 (91.39±52.52). However, a non significant decrease was presented when comparing the preoperative visit (90.25±59.31) to both visit 2 (86.02±49.24) and visit 3 (89.14±50.31), P=1.
Finally, statistical differences were also found in the Spherical Equivalent (SE), F (2.34, 234)=49.20, P=0.00 with an effect size of 0.038. A significant increase was obtained when comparing the preoperative visit to visit 1, 2 and 3 (-5.40±3.42), (-2.32±2.75), (-2.16±1.86) and (-2.04±1.92) respectively, P=0.00.
DISCUSSION
The core purpose of intra-corneal ring segments (ICRS) is achieving modifications to the corneal curvature and subsequently adjusting astigmatism. Research in the medical field also reported the efficacy of these implants in reducing refractive errors and corneal steeping in Keratoconus. These results correspond with the Barraquer thickness law which states that central cornea flattening is achieved by adding tissue to the corneal periphery[11]. Main advantages of this technique are highlighted through the fact that this procedure is reversible and that there is no need to remove tissue from the cornea. Furthermore, evidence was also presented in support of the ring segments' effective management of sphere and cylinder[12].
Many types of ICRS were developed and investigated in previous reports for the treatment of keratoconus. Differences in section profile and diameter of implantation are essential dissimilarities between these segments. The Ferrara ring segment, which has a triangular interior surface, has gained increasing attention over the past few years because it may have a stronger affect in flattening the central cornea. This therapeutic influence might be explained in light of its design which allows a closer position to the corneal center when compared with Intacs. Nevertheless, long term outcomes are still being investigated. Moreover, the need for larger numbers of patients and longer follow up periods is well recognized throughout previous literature. This paper aims at contributing to the development of adequate interventions to meet the needs of keratoconus patients with contact lens intolerance and improve their quality of life.
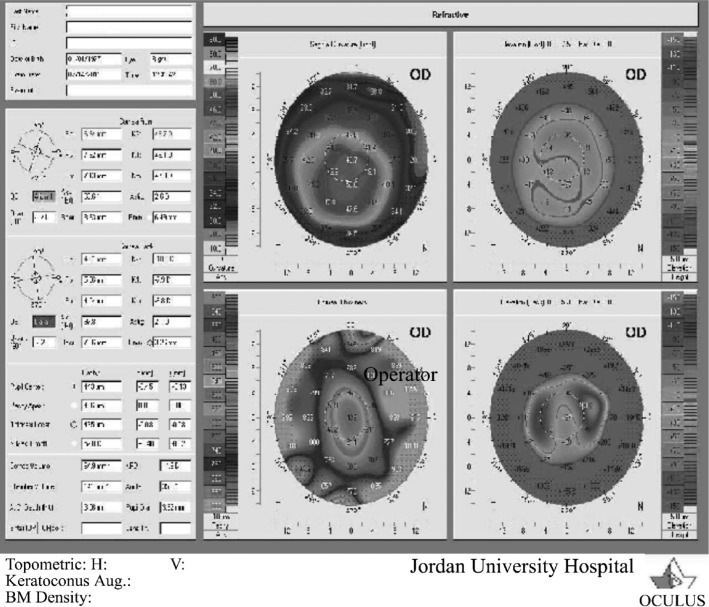
As confirmed by the vast majority of previous studies[13]-[20], our findings also indicate a statistically significant increase in both UCVA and BSCVA throughout follow up visits. A comparison between pre and post corneal topography (Pentacam from Oculus) illustrates improvements in refraction (Figure 1, Figure 2). The maximum increase in UCVA occurred at visit one (mean raised from 0.17 to 0.37) whereas, the highest rise in BSCVA came about from visit two to visit three (mean increased from 0.57 to 0.62).
Figure 2. (Abu ameerh). postoperative corneal topography (pentacam from oculus).
This can be explained by Ferrara rings' potential to remodel the corneal profile and consequently reducing corneal steepening and astigmatism associated with keratoconus. It is also worth mentioning that spectacle correction cannot provide an optimized visual quality nor improve corneal ability adequately in all cases. This enhances the notion that considers ICRS a corrective alternative solution especially for patients with contact lens intolerance. Bearing in mind the essence purpose of delaying or even avoiding corneal grafting, Ferrara rings tend to preserve corneal asphericity and facilitate visual rehabilitation rapidly after implantation.Our study also presents a further investigation into the amount of astigmatism and myopia indicating a significant reduction in all eyes. Results also show a decrease in the spherical equivalent. The maximum reduction in all three visits occurs in visit one (cylinder reduced from -4.19 to - 3.05, sphere decreased from -3.32 to -1.08 and spherical equivalent downgraded from -5.40 to -2.32). Furthermore, additional reduction was also noted in the subsequent visits.
A possible explanation is presented by Dr. Siganos[14] who suggests that ring segments have a “prismatic design” which reduces glare and reflects light internally rather than bouncing it to the side. Additionally, K values (Ks, Kf, Km) demonstrate a significant decrease throughout visits. This decrease is salient at visit one while it is gradual and more fluctuating between postoperative visits (. This supports the idea that ICRS early postoperative outcomes reveal the most benefits for patients' visual rehabilitation. A further support of these findings is derived from prior research which presents similar results[12],[15],[20]-[22].Although rare; several post- surgical complications have been reported previously. Among those are asymmetric placement, inadequate depth of channel, migration, segment decentration, infectious keratitis, and extrusion, none were noticed as a consequence of our surgical procedure.
In conclusion, FICRS implantation may be a reasonable procedure in correcting myopia and astigmatism in patients with keratoconus. This method may delay or even avoid the need for more invasive surgical procedure. However, further clinical studies with more patients and longer follow ups are still needed to evaluate long term stability of these results. The implantation of Ferrara ring segments was proven to be a safe and adjustable procedure which reduces corneal steeping and improves visual outcomes in eyes with keratoconus. Spreading awareness among patients postoperatively, along with early detection and intervention, played a vital role in prevention against complications.
Acknowledgments
This research is a joint responsibility between authors. To our knowledge, this is the first study to investigate the effectiveness of Ferrara ring segments implantation in a Jordanian sample. Up till now there has been no approved protocol among Ophthalmologists in Jordan on which surgical intervention should be done for patients with keratoconus. However, our research might provide a balanced evidence to guide policy and practice regarding this important matter. The authors also acknowledge the need for further research with larger numbers of patients and longer follow up periods.
REFERENCES
- 1.Duke-Elder S, Leigh AG. System of Ophthalmology. Diseases of the outer eye. London: Henry Kimpton. 1965:964–976. [Google Scholar]
- 2.Kemp EG, Lewis EJ. Immunoglobulin patterns in keratoconus with particular reference to total and specific IgE levels. Br J Ophthalmol. 1982;66(11):717–720. doi: 10.1136/bjo.66.11.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karseras AG, Ruben M. Aetiology of keratoconus. Br J Ophthalmol. 1976;60(7):522–525. doi: 10.1136/bjo.60.7.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomidokoro A, Oshika T, Amano S, Higaki S, Naoyuki M, Kazunori M. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology. 2000;107(7):1328–1332. doi: 10.1016/s0161-6420(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 5.Espandar L, Meyer J. Keratoconus: Overview and update on treatment. Middle East Afr J Ophthalmol. 2010;17(1):15–20. doi: 10.4103/0974-9233.61212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrara de A, Cunha P. Tecnica cirgica para correcao de myopia; anel corneano intra-estromal. Rev Bras Oftalmol. 1995;54(8):577–588. [Google Scholar]
- 7.Cochener B, Le Floch G, Colin J. Intra-corneal rings for the correction of weak myopias. J Fr Ophtalmol. 1998;21(3):191–208. [PubMed] [Google Scholar]
- 8.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26(8):1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 9.Alio JL, Artola A, Ruiz-Moreno JM, Hassanein A, Galal A, Awadalla M. Changes in keratoconic corneas after intracorneal ring segment explanation and reimplantation. Ophthalmology. 2004;111(4):747–751. doi: 10.1016/j.ophtha.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 10.Norusis M. SPSS/PC + for the IBM PC/XT at SPSS. Chicago, Inc; 1986. [Google Scholar]
- 11.Barraquer J. Modification of refraction by means of intracorneal inclusion. Int Ophthalmol Clin. 1966;6(1):53–78. [PubMed] [Google Scholar]
- 12.Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease – a review. Clin Exp Ophthalmol. 2010;38:154–167. doi: 10.1111/j.1442-9071.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 13.Guttman C. Intrastromal ring segments option for treating keratoconus. Stage lll or lV keratoconus may benefit from central cornea flattening by Ferrara ring segments. Ophthalmology Times. 2000:10. [Google Scholar]
- 14.Siganos D, Ferrara P, Chatzinikolas K, Bessis N, Papastergion G. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002;28(11):1947–1951. doi: 10.1016/s0886-3350(02)01495-5. [DOI] [PubMed] [Google Scholar]
- 15.Kwitko S, Severo N. Ferrara intracorneal ring segments for keratoconus. J Cataract Reract Surg. 2004;30(4):812–820. doi: 10.1016/j.jcrs.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Charters L. Intrastromal ring segments promising for keratectasia. Technique able to improve best-corrected visual acuity, contact lens fit. Ophthalmology Times. 2006:64. [Google Scholar]
- 17.Torquetti L, Berble R, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009;35(10):1768–1773. doi: 10.1016/j.jcrs.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 18.Hamdi I M. Optical and topographic changes in Keratoconus after implantation of Ferrara intracorneal ring segments. J Refract Surg. 2010;26(11):871–880. doi: 10.3928/1081597X-20100114-05. [DOI] [PubMed] [Google Scholar]
- 19.Ancele E, Malecaze F, Arne J, Fournie P. Predictive factors for successful Ferrara intracorneal ring segment implantation in keratoconus. J Fr Ophthalmol. 2011;34(8):513–520. doi: 10.1016/j.jfo.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Mate-Istvan I, Tomi T, Borda A. Acta Medica Marisiensis. 3. Vol. 57. University of Medicine and Farmacy; Romania: 2011. Ferrara intra-corneal ring segments for treatment of keratoconus; pp. 226–228. [Google Scholar]
- 21.Bethke W. Test driving the new Ferrara ring. Review of Ophthalmology. 2001;8(11):136–137. [Google Scholar]
- 22.Gharaibeh AM, Muhsen SM, Abu Khader IB, Ababneh OH, Abu-Ameerh MA, Albdour MD. Keraring intrastromal corneal ring segments for correction of keratoconus. Cornea. 2012;31(2):115–120. doi: 10.1097/ICO.0b013e3182215a15. [DOI] [PubMed] [Google Scholar]