Abstract
The scientific study of how discrimination harms health requires theoretically grounded methods. At issue is how discrimination, as one form of societal injustice, becomes embodied inequality and is manifested as health inequities.
As clarified by ecosocial theory, methods must address the lived realities of discrimination as an exploitative and oppressive societal phenomenon operating at multiple levels and involving myriad pathways across both the life course and historical generations.
An integrated embodied research approach hence must consider (1) the structural level—past and present de jure and de facto discrimination; (2) the individual level—issues of domains, nativity, and use of both explicit and implicit discrimination measures; and (3) how current research methods likely underestimate the impact of racism on health.
TWO DECADES AGO, IN 1992, the US Centers for Disease Control and Prevention sponsored a groundbreaking meeting on racism, Black women, and the risk of preterm delivery.1 At the time, despite centuries of debate over the causes of racial/ethnic inequalities in health,2,3 scant scientific research had explicitly and rigorously investigated whether—and if so, how—racial discrimination harms health.2–4 Just over decade later, in 2003, the National Institutes of Health held its first-ever meeting on the subject, Racial/Ethnic Bias and Health,5 the same year the Institute of Medicine published its first major report on racial discrimination in health care.6 Since then, studies on discrimination and health have burgeoned, with new evidence prompting new controversies about both concepts and methods, singly and combined.7–14
Amidst all the debate and new findings, one point stands out: the scientific study of how discrimination harms health requires theoretically grounded methods. In this article, I accordingly discuss key conceptual issues relevant to research on racism and health and their methodological implications for testing hypotheses about how racial discrimination, as one form of societal injustice, becomes embodied inequality7,15–20—and hence manifested as health inequities. Although my focus is on racial discrimination and health in the United States, the concerns raised are pertinent for any type of discrimination in any country context.
METHODS REQUIRE THEORY AND CONTEXT
Because choice of methods depends on the hypotheses being tested, which in turn depend on the theoretical frameworks employed, rigorous scientific research requires transparency about both theories and methods.17,21,22 The theory I draw on is the ecosocial theory of disease distribution,15–17,22 which concerns who and what drive social inequalities in health. The box on the following page shows the theory’s key constructs and core propositions. A central focus is on how we literally biologically embody exposures arising from our societal and ecological context, thereby producing population rates and distributions of health. At issue are socially patterned exposure-induced pathogenic pathways, mediated by physiology, behavior, and gene expression, that affect the development, growth, regulation, and death of our body’s biological systems, organs, and cells, culminating in disease, disability, and death. The contrast is to frameworks that treat causes of disease—and of group differences in biological characteristics and disease rates—as primarily innate, as has often been argued for racial/ethnic disparities in health.2–4,17–19 Consider, for example, the past 2 centuries’ within- and across-generation social inequalities in US infant mortality rates: the most plausible explanation is that they constitute the biological expression—hence embodiment—of changing exogenous conditions.1–4,7,15–19
Ecosocial Theory: Core Constructs and Core Propositions
| Core constructsa |
| 1. Embodiment: referring to how we literally incorporate, biologically, in societal and ecological context, the material and social world in which we live. |
| 2. Pathways of embodiment: via diverse, concurrent, and interacting pathways, involving adverse exposure to social and economic deprivation, exogenous hazards (e.g., toxic substances, pathogens, and hazardous conditions), social trauma (e.g., discrimination and other forms of mental, physical, and sexual trauma), targeted marketing of harmful commodities (e.g., tobacco, alcohol, other licit and illicit drugs), inadequate or degrading health care; and degradation of ecosystems, including as linked to alienation of Indigenous populations from their lands. |
| 3. Cumulative interplay of exposure, susceptibility, and resistance across the life course: referring to the importance of timing and accumulation of, plus responses to, embodied exposures, involving gene expression, not simply gene frequency. |
| 4. Accountability and agency: both for social disparities in health and research to explain these inequities. |
| Core propositionsa |
| 1. People literally embody, biologically, their lived experience, in societal and ecologic context, thereby creating population patterns of health and disease. |
| 2. Societies’ epidemiological profiles are shaped by the ways of living afforded by their current and changing societal arrangements of power, property, and the production and reproduction of both social and biological life, involving people, other species, and the biophysical world in which we live. |
| 3. Determinants of current and changing societal patterns of disease distribution, including health inequities, are (a) exogenous to people’s bodies, and (b) manifest at different levels and involve different spatiotemporal scales, with macro-level phenomena are more likely to drive and constrain meso- and microlevel phenomena than vice versa; to the extent genes are relevant to societal distributions of disease, at issue is gene expression, not gene frequency. |
| 4. In societies exhibiting social divisions based on property and power, and in which those with the most power and resources constitute a small percentage of the population, the more prevalent the health outcome, the greater the absolute burden (and potentially the relative burden) on those with less power and fewer resources, because they constitute the majority of the population; a corollary is that for more rare or infrequent (nonendemic) diseases, it cannot be presumed, in advance, whether social inequalities in the outcome exist, and, if they do, the direction of the gradient. |
| 5. Explanations of disease distribution cannot be reduced solely to explanations of disease mechanisms, because the latter do not account for why rates and patterns change, in complex ways, over time and place. |
| 6. Practice of a reflexive epidemiology that situates in broader societal context an investigation’s motivating theories, hypotheses, methods of analysis, and interpretation of findings will improve the likelihood of epidemiologists being better positioned to understand and convey the meanings and limitation of our study results and explanations for population patterns of health, disease, and well-being. |
Source. Krieger.17(pp214–215)
All processes involved are conditional on extant political economy and political ecology of the societies in which the embodied populations patterns of health, disease, and well-being are manifested.
Ecosocial theory accordingly requires explicit consideration of pathways of embodiment in relation to types and levels of exposure, the period and spatial expanse involved (i.e., spatiotemporal scale), and historical context, along with phenomena that affect susceptibility and resistance to exposure, ranging from micro (e.g., role of the gut microbiome in innate immunity) to macro (e.g., social organizing to challenge health inequities). Also germane are issues of accountability (causal responsibility for) and agency (the power and ability to act) at every level, because they pertain to not only the magnitude of health inequities but also how they are monitored, analyzed, and addressed. As with any theory, the point is to frame and guide analysis of the phenomena of interest—in this case, population distributions of health, disease, disability, and well-being—and, as with any reflexive science, to generate knowledge relevant to altering the phenomena under study, in this case, the existence of health inequities.17
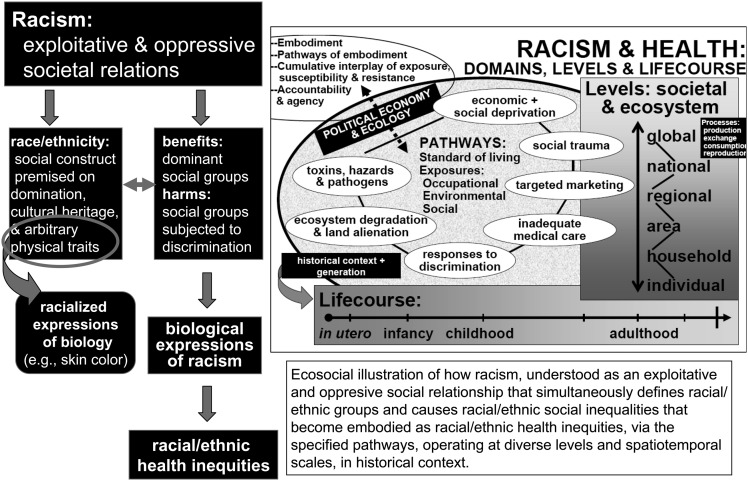
Figure 1 illustrates the components of an ecosocial analysis of racism and health.7,17,18 The point is not that every study can or should attempt to measure every specified pathway at every level and at all relevant spatiotemporal scales—which obviously is impossible to do—but rather that systematic theorizing about what is or is not measured, and how, can aid interpretation of study findings.15–17
FIGURE 1—
Ecosocial theory: schematic illustration as applied to analyzing the embodiment of racial inequality and its implications for health inequities.
Source. Krieger.7,17,18
To guide both the research questions posed and the methods used, ecosocial theory posits that inequitable race relations simultaneously—and not sequentially—(1) benefit the groups who claim racial superiority at the expense of those whom they deem intrinsically inferior, (2) racialize biology to produce and justify the very categories used to demarcate racial/ethnic groups, and (3) generate inequitable living and working conditions that, via embodiment, result in the biological expression of racism—and hence racial/ethnic health inequities.7,17,18,22 A corollary is that there are many pathways, not just 1, by which discrimination harms health. As shown in Figure 1, major pathways involve economic and social deprivation; excess exposure to toxins, hazards, and pathogens; social trauma; health-harming responses to discrimination; targeted marketing of harmful commodities; inadequate medical care; and, especially (but not only) for indigenous peoples, ecosystem degradation and alienation from the land.7,17,18 Moreover, as emphasized by ecosocial theory’s simultaneous focus on exposure, susceptibility, and resistance, how people resist injustice and its health-harming effects, individually and collectively, and the resilience that enables them to do so also must be examined.15–18
Historical context in turn determines which pathways matter and are operative, at what level and at what point in the life course. To provide context, indicators of the current sociopolitical and economic conditions23–30 are provided in Tables 1 to 3. Data are presented on (1) well-known stark US racial/ethnic inequities in economic and political power23–28 and health status25 (albeit well known chiefly to academics, but not to much of the US public29) and (2) disparate views on discrimination, whereby in 2010 fully 48% of the US White population agreed with the statement, “Today discrimination against Whites has become as big as a problem as discrimination against Blacks and other minorities,” although 70% of Black respondents and 68% of Hispanics disagreed.30 The complex connections—and disconnections—between evidence and awareness are, in accordance with ecosocial theory’s attention to accountability and agency, key to framing analysis of and interventions to address health inequities,29 including the impact of racial discrimination on health.
TABLE 1—
Analyzing US Racial/Ethnic Health Inequities in Context: Relevant Socioeconomic, Sociopolitical, and Embodied Facts
| Racial/Ethnic Inequity Indicators | Total US Population | White Non-Hispanic | Asiana | Hispanic | Black Non-Hispanicb | American Indian/ Alaska Native |
| Wealth (2004): median household assets,23 $ | 79 800 | 113 822 | 107 690 | 13 375 | 8 650 | … |
| Poverty (2009),25,26 % | 14.3 | 9.4 | 12.5 | 25.3 | 25.8 | 25.3 (2006–2008) |
| Unemployed (2009),24 % | 9.3 | 8.5 | 7.3 | 12.1 | 14.8 | … |
| Incarceration of men (2008),25 per 100 000 population | 1403 | 727 | … | 1760 | 11 137 | … |
| Political parity ratio (2004),28 % in political office/% in population | ||||||
| Congress | … | Men, 2.28; Women, 0.30 | Men, 0.53; Women, 0.00 | Men, 0.49; Women, 0.21 | Men, 0.84; Women, 0.33 | … |
| State legislatures | … | Men, 2.04; Women, 0.52 | Men, 0.41; Women, 0.15 | Men, 0.34; Women, 0.49 | Men, 0.89; Women, 0.46 | … |
| No health insurance (2009),25,26 % | 16.7 | 12.0 | 17.2 | 32.4 | 21.0 | 33.0 |
| Infant mortality rate (2006),25 per 1000 live births | 6.7 | 5.6 | 4.5 | 5.4 | 13.4 | 8.3 |
| Person-years lost before 75 years of age (2007)25 | 7083.5 | 6736.5 | 3404.9 | 5447.4 | 11 259.8 | 8463.6 |
| Self-reported fair or poor health status (2009),25 % | 9.9 | 8.0 | 8.4 | 13.3 | 14.2 | 16.3 |
| Severe psychological distress (2008–2009),c25 % | 3.2 | 3.2 | 1.1 | 3.4 | 3.7 | 3.8 |
Note. Ellipses indicate data not reported, which is indicative of imposed invisibility and is an informative social fact characterizing social context.
Economic data and data on self-reported health and psychological distress are for Asians only; all other health data reported for Asians and Pacific Islanders combined.
Person-years of life lost before 75 years of age are reported for Blacks only; all other data for the Black non-Hispanic population.
Serious psychological distress in past 30 days among adults aged 18 years and older, as measured by the Kessler 6 scale (range = 0–24; severe psychological distress ≥ 13).
TABLE 2—
Trends in US Income and Concentration of Wealth
| Bottom 20% of US Population by Wealth |
Top 20% of US Population by Wealth |
Top 5% of US Population by Wealth |
||||
| Year | Wealth | Mean Income, $ | Wealth | Mean Income, $ | Wealth | Mean Income, $ |
| 1970 | 4.1 | 3064 | 43.3 | 9796 | 16.6 | 34 601 |
| 1980 | 4.2 | 6411 | 44.1 | 49 248 | 16.5 | 70 010 |
| 1990 | 3.8 | 9833 | 46.6 | 94 404 | 18.5 | 148 124 |
| 2000 | 3.6 | 14 122 | 49.8 | 156 919 | 22.1 | 278 063 |
| 2009 | 3.4 | 15 289 | 50.3 | 189 486 | 21.7 | 325 023 |
| Trend | ↓ | ↑ | ↑ | ↑↑↑ | ↑↑ | ↑↑ |
Note. Wealth is the share of aggregate income received by each fifth and top 5% of households. Mean income is in 2009 dollars according to the US Census.
Source. US Census Bureau.23
TABLE 3—
Postelection National Poll Results for Statement on Racial Discrimination, November 3–7, 2010
| “Today discrimination against Whites has
become as big a problem as discrimination against Blacks and other
minorities.” |
||
| Population Group | Agree, % | Disagree, % |
| Total | 44 | 54 |
| White | 48 | 50 |
| Tea Party | 62 | 36 |
| Republican | 56 | 42 |
| Independent | 53 | 46 |
| Democrat | 30 | 68 |
| Black | 30 | 70 |
| Hispanic | 32 | 68 |
Source. Jones and Cox.30
METHODOLOGICAL CHALLENGES FOR ANALYZING STRUCTURAL DETERMINANTS
A major challenge is to develop rigorous methods to study the health impact of structural determinants of racial inequality, including laws; institutional policies and practices; national, regional, state, and local economic and political infrastructures; and neighborhood and workplace conditions.4,7,27,28,31–35 At issue is the substantive content of variables deployed and not simply whether multilevel, life course, or birth cohort methods are used.36,37
State-sanctioned discrimination, past and present, is of particular concern. Not surprisingly, because the federal government abolished legal (i.e., de jure) racial discrimination in the mid-1960s,38 most contemporary US research on institutional racism and health primarily focuses on present day de facto discriminatory policies and practices, chiefly in relation to (1) health care systems6,11 and (2) residential, educational, and (to a lesser extent) occupational segregation.8,12,31–35
An important gap in current research, however, rendered visible by ecosocial theory’s emphasis on accountability and agency, concerns the racialized health consequences of contemporary legal discrimination. Underscoring this point is nascent work on the myriad consequences of the legally color-blind, albeit racially motivated, US War on Drugs and its role in producing or exacerbating health-debilitating racial/ethnic inequalities.39–44 As Alexander explains,
President Ronald Reagan officially declared the current drug war in 1982, when drug crime was declining, not rising. From the outset, the war had little to do with drug crime and nearly everything to do with racial politics. The drug war was part of a grand and highly successful Republican Party strategy of using racially coded political appeals on issues of crime and welfare to attract poor and working class white voters who were resentful of, and threatened by, desegregation, busing, and affirmative action. In the words of H. R. Haldeman, President Richard Nixon's White House Chief of Staff: “[T]he whole problem is really the blacks. The key is to devise a system that recognizes this while not appearing to.”45(pp43,44)
Consequently, despite substantial evidence that rates of illicit drug use are similar across all US racial/ethnic groups,25(Table 63),39 permitted discretionary judgment has resulted in stark racial/ethnic inequities in arrests, convictions, and sentencing—followed by legal discrimination against ex-felons, who not only are denied the right to vote and serve on juries but also confront legal prohibitions limiting access to such well-known determinants of health as employment, housing, education, and public benefits.39,40,43,44 The exclusion of prisoners from most health studies, with their typical focus on the noninstitutionalized civilian population, in turn means that most research findings likely underestimate the extent of—and contribution of racial discrimination to—racial/ethnic health inequities.43
Nor is history dead within us. As ecosocial theory clarifies, measuring only contemporary exposure is likely to dilute estimates of the impact of racial discrimination on health.17,18 A case in point is the mid-1960s abolition of US Jim Crow laws—i.e., laws enacted in the late 19th and early 20th centuries that sanctioned legal racial discrimination (predominantly against Black Americans, but also affecting American Indians, Latinos, and Asian Americans) in voting, education, employment, health care, housing, the legal system, and use of public facilities, spaces, services, and transportation.38,46–49 In light of mounting evidence of the importance of early life conditions and cumulative disadvantage for both adult health and transgenerational transmission of risk,37,43 a reasonable hypothesis is that Jim Crow laws, as well as their abolition, had both immediate and enduring health consequences.18 In 2011, all US-born persons aged 65 years and older (i.e., the age group in which the bulk of mortality occurs) were born, came of age, and had already lived the first 20 years of their lives, and perhaps had their first child, when Jim Crow was legal in 21 out of 50 states plus the District of Columbia,46 with de facto discrimination in the remaining 29 states.
Yet, to date, scant research has investigated the impact of Jim Crow laws—or their abolition—for present-day racial/ethnic health disparities.18,50–53 Two sets of findings suggest that such analyses may be useful. First, hinting at immediate effects, not only did Black infant mortality rates sharply drop in the US rural South after passage of the 1964 Civil Rights Act,50 but also, for both infant death and premature mortality (death before 65 years of age), the magnitude of US socioeconomic health inequities, both overall and within racial/ethnic groups, shrank considerably between 1965 and 1980, only to widen or stagnate thereafter.53 One likely explanation is that the earlier period encompassed the passage of the Civil Rights Act, the policies of the War on Poverty, and the establishment of Medicare, Medicaid, the Occupational Safety and Health Administration, and the Environmental Protection Agency; thereafter, in reaction, subsequent administrations curbed both government regulations and initiatives promoting equity.18,27,53
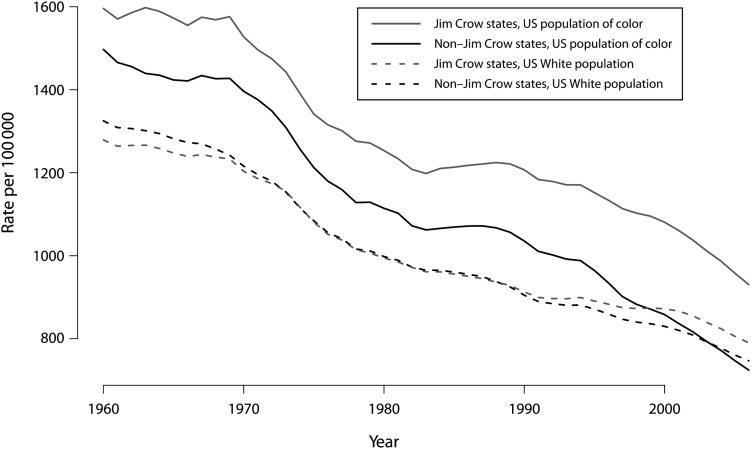
Second, suggesting enduring effects, the data presented in Figure 2 show the far greater—and continued—salience of Jim Crow status for mortality among US populations of color as compared with the US White population. A parallel argument regarding the continuing relevance of past as well as current injustice to contemporary racial/ethnic health inequities appears in the literature on Indigenous people’s health, concerning the ongoing somatic and mental health consequences of historical trauma.20,54,55
FIGURE 2—
The Jim Crow geography of mortality: US racial/ethnic inequities in all-cause mortality, 1960–2006.
Source. N. Krieger, J. T. Chen, A. Koshelva, P. D. Waterman unpublished data, 2012, with written permission from all authors.
METHODOLOGICAL CHALLENGES INVOLVING INDIVIDUALS, LEVELS, AND SPATIOTEMPORAL SCALE
Study of structural determinants is essential for analyzing how racism harms health, but research is also needed on how individuals embody these determinants. A starting point is to remember that individual-level data are more than simply individual—precisely because no one is an individual one day and a member of a population another. Each person is both, simultaneously.17 At issue are not only people’s individual experiences, both material and psychological, but also their reference points for evaluating them—and for acting to alter future risk. Identification of discrimination at the individual level requires group-level knowledge—whether knowledge about group mores for what constitutes dignified treatment versus the denial of dignity31,56 or, in the case of discrimination regarding wages, occupational hazards, and medical referrals, knowledge about what others have experienced.7,31
Individual Explicit (Self-Report) Data
Domains matter.
Two distinct types of instruments appear in the literature on racial discrimination and health: (1) explicit measures of exposure to diverse domains, and (2) measures that emphasize psychosocial aspects of interpersonal interactions with less or no information about where the interactions occurred.7–14 Widely used examples of the former are (1) the Experiences of Discrimination (EOD) scale, which asks about discrimination in 9 domains (“at school”; “getting hired or getting a job”; “at work”; “getting housing”; “getting medical care”; “getting service in a store or restaurant”; “getting credit, bank loans, or a mortgage”; “on the street or in a public setting”; and “from the police or in the courts”) and also about people’s responses to unfair treatment,57,58 and (2) the major discrimination component of the Everyday Discrimination Scale (EDS), which specifies 6 domains (work, police, education, housing, bank, receipt of services) among its 9 items.59 Also part of the EDS is a measure of “day-to-day unfair treatment,”59 which focuses on various types of unfair treatment, with the 2 domains mentioned (in the 10 items) pertaining to stores and restaurants.
Currently, a growing number of researchers are using this latter EDS measure, regarding day-to-day unfair treatment, on its own, rather than in conjunction with the domain-oriented major discrimination EDS subscale.60–67 Yet, from both a data quality and also a prevention and policy perspective, asking about the multiple domains in which discrimination occurs is critical—as a key complement to, not replacement for, questions that focus on psychosocial aspects of the exposure. In part, this is because specification of domains is important for cognitively grounding the question and response31 and because critical theoretically informed review of such lists can reveal gaps and hence potential new domains for inclusion (e.g., racial discrimination in cyberspace68). Beyond any psychometric considerations, however, are key points pertaining to agency and accountability: the occurrence of discrimination in diverse domains, such as discrimination at work, in housing, and in education, is legally actionable,7,31,49 and knowing where discrimination occurs, as opposed to treating it only as a free-floating psychosocial stressor, is relevant to ending it.
Nativity matters.
Nativity is important not only because of growing anti-immigrant discrimination,49,69 but also because if, indeed, “race” is a social construct—a premise informing much of the research on racial discrimination and health4,7–10,18,19—then it follows that people born and raised outside of the United States have to learn how race is produced here and what US racial discrimination is like.70–73 Tellingly, research indicates that recent US immigrants of color are the least likely to report having experienced racial discrimination,70–79 despite their greater likelihood of encountering discrimination based on language.76,78,80 The robust body of work on the healthy immigrant effect further indicates that, at least for the first generation, immigrants typically have better health than their US-born counterparts.81,82 Yet, to date, few US investigations on racial discrimination and health—apart from those explicitly focused on immigration status74–80—routinely take nativity into account in their analyses. This omission, however, can lead to 3 underappreciated serious problems79:
Misleading estimates of the prevalence of exposure, because estimates derived from analyses that lump together the US-born and foreign-born population without regard for nativity can obscure the higher self-reported burden among the US-born population;
Biased estimates (and most likely underestimates) of the association between racial discrimination and health, whether attributable to confounding (i.e., lack of control for nativity), effect modification (at a given level of exposure, the exposure–outcome association varies by nativity), or both;
Inaccurate estimates of the population-attributable fraction (which depends on both the frequency of exposure and magnitude of the exposure–outcome association83).
At a time when foreign-born people constitute an ever-higher proportion of most US populations of color,71 including among Black Americans (upwards of 30% are foreign born in such cities as Boston, New York City, Washington, and Miami84,85), rigorous research on racial discrimination and health must reckon with issues of nativity.
Direct questions about racial discrimination matter.
Currently, the 2 main approaches used in explicit self-report measures either (1) ask explicitly about racial discrimination in the stem of the question (as in the EOD measure57.58), versus (2) ask first about unfair treatment, and if any is reported, follow up with a question about attribution, for example, to race/ethnicity or something else (as in the EOD measure59). As has been noted for at least a decade,7,80,86,87 these approaches differ significantly.
Attesting to differences in these 2 approaches, new empirical data from the 2007 California Health Interview Study unambiguously demonstrate—by employing identically phrased questions and a split-sample design80,87—that self-reports of unfair treatment (without any attribution) are much higher—and demonstrate far less racial/ethnic variation—than self-reports of unfair treatment attributed to race/ethnicity and self-reports in response to a 1-stage question that asks directly about racial discrimination.80 By implication, unfair treatment (without attribution) would contribute less to explaining racial/ethnic health disparities and would also underestimate the health impact of racial discrimination. Even so, scientific investigations continue to treat findings arrived at through these 2 different methods as directly comparable.60,62,88,89 The larger issue raised by these findings is whether self-report data are adequate for measuring exposure to racial discrimination.
Individual Implicit Data
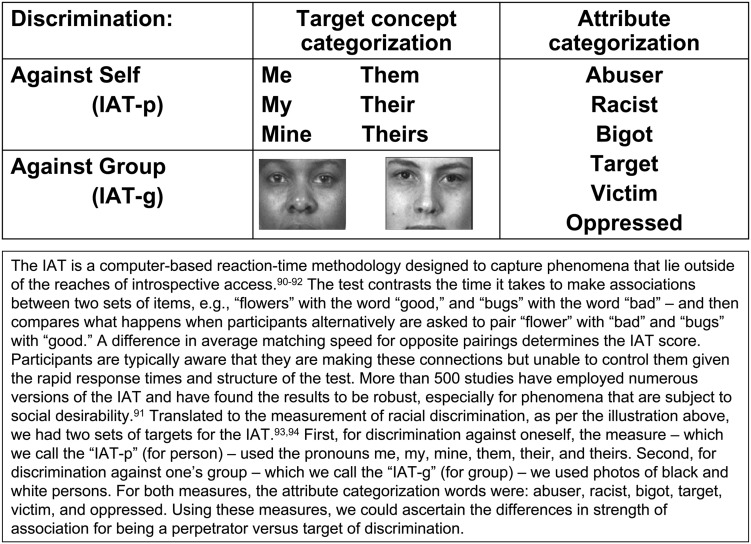
One of the newer approaches in the racial discrimination and health literature that seek to minimize well-known cognitive problems affecting self-report data is the Implicit Association Test90–94 (IAT; Figure 3), a methodology initially developed to measure prejudice. Motivating its use in health research is the concern that the people most affected by discrimination may be least able or willing to say so, even as such experiences may nevertheless affect their health.7,57 Two lines of empirical evidence support this hypothesis.
FIGURE 3—
Implicit Association Test and use for measuring exposure to racial discrimination.
First, the phenomenon psychologists refer to as the “person–group discrimination discrepancy” reveals that people typically report more discrimination for their group, on average, than for themselves personally—even though it is not possible for all individuals to experience, on average, less discrimination than their group.93–96 Second, several studies have observed a linear association between discrimination and health among more affluent persons: among groups with fewer resources, risk was higher among respondents who reported no discrimination than among those who reported moderate discrimination, with the highest risk, however, occurring among respondents who reported high exposure (i.e., a J-shaped curve).97–99 Together, these findings imply that self-reports of racial discrimination among exposed groups may underestimate exposure, especially among those with the least resources, even as this exposure can still adversely affect their health; one consequence would be underestimation of the impact of racial discrimination on health.7,18
Tellingly, the first 2 studies to use the IAT to measure racial discrimination have already shown that (1) the implicit measure does not detect the person–group discrimination discrepancy observed with the explicit measure, suggesting that this phenomenon reflects self-presentional bias, and (2) the correlation between implicit and explicit measures is small, implying that they capture different phenomena.93,94
The second study also reported 2 notable health-related findings.94 First, the IAT and the EOD responses were independently associated with risk of hypertension among Black Americans. Second, in models comparing the Black and White participants that controlled for age, gender, socioeconomic position (educational level of the respondent and both parents), body mass index, social desirability, and response to unfair treatment, Black participants remained at significantly higher risk of being hypertensive (odds ratio [OR] = 1.4; 95% confidence interval [CI] = 1.0, 1.9). Their excess risk, however, was effectively eliminated and rendered statistically nonsignificant (OR = 1.1; 95% CI = 0.7, 1.7) by additionally adjusting for exposure to racial discrimination by using both the IAT and the EOD measure. These preliminary results thus point to the likely utility of health research on discrimination supplementing self-report data with IAT data.
EMBODYING EXPOSURE TO MULTIPLE TYPES OF DISCRIMINATION
Further underscoring the need for a more critical and integrated approach to investigating discrimination and health is the eocosocial inverse hazard law, modeled after Hart’s famous inverse care law,100 which posits that “the accumulation of health hazards tends to vary inversely with the power and resources of the populations affected.”101(p1970) At issue is the cumulative embodiment of multiple types of discrimination, deprivation, and other harmful exposures.
An empirical demonstration of why such an embodied approach is needed is analysis of data from the United for Health study, which recruited predominantly lower-income, employed women and men from diverse racial/ethnic groups, both US-born and foreign-born, from the Greater Boston area during 2003 and 2004.102 Among members of this study, we documented high exposure to (1) socioeconomic deprivation, (2) occupational hazards (i.e.., chemicals, dusts, fumes, and ergonomic strain), (3) social hazards (i.e., racial discrimination, workplace abuse, and sexual harassment at work), and (4) relationship hazards (i.e., intimate partner violence and unsafe sex).103–106 Despite being union members, one third of the study participants earned less than a living wage (equal to $10.54/hour at the time of the study) and 40% were below the US poverty line, with the Black and Latino workers nearly twice as likely as Whites to be poor.103
Fully 85% of study members reported at least 1 high exposure to occupational hazards in the past year; nearly half (46%) reported 3 or more high exposures, and 17% reported 5 or more high exposures. Although some variation existed by race/ethnicity and gender, the majority of workers in each racial/ethnic-gender group were highly exposed.104,105 Simultaneously, more than 85% of the participants reported exposure to at least 1 of the 3 social hazards; exposure to all 3 reached 20% to 30% among the Black workers, the most highly exposed group.103 For sexual harassment, an additional social category was relevant: sexuality. Specifically, lesbian, gay, bisexual, and transgender workers reported twice as much sexual harassment as did their heterosexual counterparts.103 Furthermore, within each racial/ethnic group, about one third of the men reported having ever been a perpetrator of intimate partner violence, and about one third of the women reported having been a target of such violence.106
As exemplified by analyses of severe psychological distress, attaining an accurate picture of risk required considering all the social hazards together. Findings revealed that analyses that included data on only 1 type of hazard yielded biased estimates of risk. Moreover, those that included all 3 hazards demonstrated the high toll imposed by racial discrimination, independent of other exposures.106
A RIGOROUS SCIENCE OF RESEARCH ON DISCRIMINATION AND HEALTH
In conclusion, as the examples provided in this article show, rigorous methods for the scientific study of discrimination and health require (1) conceptual clarity about the exploitative and oppressive realities of racism and other forms of adverse discrimination; (2) careful attention to domains, pathways, level, and spatiotemporal scale, in historical context; (3) structural-level measures; (4) individual-level measures, albeit without relying solely on self-report data or reducing discrimination to solely a psychosocial exposure; and (5) an embodied analytic approach. After all, we are not one day White or a person of color, another day working class or a professional, still another day a woman or a man or transgendered, on yet another day straight or lesbian, gay, bisexual, or transgender, and yet another an immigrant versus native born.7,15–18 We are all of these at once—and our research needs to integrate these conjoint social facts the same ways our bodies do, each and every day.
The stakes for getting our science right are high—both scientifically and practically. Use of critical theory–informed methods can help clarify that most extant research is likely to yield conservative, not inflated, estimates of the impact of racial discrimination on health; it can also sharpen the ability to counter fallacious attacks that research on this topic is politically,107 as opposed to scientifically, correct.108 Although data by themselves cannot rectify health inequities, the absence of data demonstrating harm nevertheless is itself harmful17,31—as underscored by the time-worn adage “no data, no problem.”109 Our responsibility, as public health researchers, is to use the best science possible—conceptually and methodologically—to build public clarity about the extent and health consequences of racial discrimination, as one necessary contribution to the urgent work of promoting health equity.
Acknowledgments
This work was partially supported by the National Institutes of Health (honorarium and travel costs only; no grant was awarded to the author).
This article is based on a plenary lecture presented at The Science of Research on Discrimination and Health conference; February 2–4, 2011; Bethesda, MD.
Human Participant Protection
No protocol approval was required, because no human participants were involved.
References
- 1.Rowley DL, Toteston H, Racial differences in preterm delivery: developing a new research paradigm. Am J Prev Med. 1993;9(suppl 6):1–123.8123282 [Google Scholar]
- 2.Ernst W, Harris B, eds. Race, Science and Medicine, 1700–1960. London, UK: Routledge; 1999. [Google Scholar]
- 3.Krieger N. Shades of difference: theoretical underpinnings of the medical controversy on Black/White differences in the United States, 1830–1870. Int J Health Serv. 1987;17(2):259–278. [DOI] [PubMed] [Google Scholar]
- 4.Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9(Suppl 6):82–122. [PubMed] [Google Scholar]
- 5.Cain VS, Kington RS. Investigating the role of racial/ethnic bias in health outcomes. Am J Public Health. 2003;93(12):191–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Washington, DC: National Academies Press, 2003. [PubMed]
- 7.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Services 1999; 29(2):295–352; republished and slightly updated as: Krieger N. Discrimination and health. In: Berkman L, Kawachi I, eds. Social Epidemiology. Oxford, UK: Oxford University Press, 2000:36–75. [DOI] [PubMed] [Google Scholar]
- 8.Williams DR, Neighbors JW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. [DOI] [PubMed] [Google Scholar]
- 10.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kressin NR, Raymond KL, Manze M. Perceptions of race/ethnicity–based discrimination: a review of measures and evaluation of their usefulness for the health care setting. J Health Care Poor Underserved. 2008;19(3):697–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bastos JL, Celeste RK, Faerstein E, Barros AJD. Racial discrimination and health: a systematic review of scales with a focus on their psychometric properties. Soc Sci Med. 2010;70(7):1091–1099. [DOI] [PubMed] [Google Scholar]
- 15.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39(7):887–903. [DOI] [PubMed] [Google Scholar]
- 16.Krieger N. Embodiment: a conceptual glossary for epidemiology. J Epidemiol Community Health. 2005;59(5):350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krieger N. Epidemiology and the People’s Health: Theory and Context. New York, NY: Oxford University Press; 2011.
- 18.Krieger N. The science and epidemiology of racism and health: racial/ethnic categories, biological expressions of racism, and the embodiment of inequality—an ecosocial perspective. In: Whitmarsh I, Jones DS, eds. What’s the Use of Race? Genetics and Difference in Forensics, Medicine, and Scientific Research. Cambridge, MA: MIT Press; 2010:225–255. [Google Scholar]
- 19.Gravlee CC. How race becomes biology: embodiment of social inequality. Am J Phys Anthropol. 2009;139(1):47–57. [DOI] [PubMed] [Google Scholar]
- 20.Walters KL, Mohammed SA, Evans-Campbell T, Beltrán RE, Chae DE, Duran B. Bodies don’t just tell stories, they tell histories: embodiment of historical trauma among American Indians and Alaska Natives. Du Bois Rev. 2011;8(1):179–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ziman J. Real Science: What It Is, and What It Means. Cambridge, UK: Cambridge University Press; 2000.
- 22.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30(4):668–677. [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau. Historical income tables: income inequality. Available at: http://www.census.gov/hhes/www/income/data/historical/inequality/index.html. Accessed August 19, 2011.
- 24.Bureau of Labor Statistics. Labor Force Characteristics by Race and Ethnicity, 2009. Washington, DC: US Department of Labor; 2010. Report 1026.
- 25.National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD: Centers for Disease Control and Prevention; 2010. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed August 19, 2011.
- 26.Office of Minority Health. American Indian/Alaska Native profile. Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3amplvlid=26. Accessed August 19, 2011.
- 27.Neckerman KM, ed. Social Inequality. New York, NY: Russell Sage Foundation; 2004.
- 28.Hardy-Fanta C, Lien P, Pinderhughes DM, Sierra CM. Gender, race, and descriptive representation in the United States: findings from the Gender and Multicultural Leadership Project. J Women Polit Policy. 2006;28(3–4):7–41. [Google Scholar]
- 29.Booske BC, Robert SA, Rohan AMK. Awareness of racial and socioeconomic health disparities in the United States: the National Opinion Survey on Health and Health Disparities, 2008–2009. Prev Chron Dis. 2011; 8(4):A73 Available at: http://www.cdc.gov/ped/issues/2011/jul/10_0166.htm. Accessed August 18, 2011. [PMC free article] [PubMed] [Google Scholar]
- 30.Jones RP, Cox D. Old Alignment, Emerging Fault Lines: Religion in the 2010 Election and Beyond—Findings From the 2010 Post-Election American Values Survey. Washington, DC: Public Religion Institute; 2010.
- 31.National Research Council. Measuring Racial Discrimination. Blank RM, Babady R, Citro CF, Washington, DC: National Academies Press; 2004. [Google Scholar]
- 32.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acevedo-Garcia D, Lochner K. Residential segregation and health. : Kawachi I, Berkman L, eds. Neighborhoods and Health. New York, NY: Oxford University Press; 2003:265–287. [Google Scholar]
- 34.Baron S, Cone J, Markowitz SB, Souza K. Introduction to a special issue: occupational health disparities. Am J Ind Med. 2010;53(2):82–83. [DOI] [PubMed] [Google Scholar]
- 35.Krieger N. Workers are people too: societal aspects of occupational health disparities—an ecosocial perspective. Am J Ind Med. 2010;53(2):104–115. [DOI] [PubMed] [Google Scholar]
- 36.Berkman L, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000.
- 37.Kuh D, Ben-Shlomo Y, eds. A Life Course Approach to Chronic Disease Epidemiology: Tracing the Origins of Ill-Health From Early to Adult Life. 2nd rev ed. New York, NY: Oxford University Press; 2004.
- 38.Fairclough A. Better Day Coming: Blacks and Equality, 1890–2000. New York, NY: Viking; 2001.
- 39.Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York, NY: New Press; 2010.
- 40.Treadwell HM, Nottingham JH. Standing in the gap: prisons and health. Am J Public Health. 2008;98(Suppl 1):S170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moore LD, Elkavich A. Who’s using and who’s doing time: incarceration, the war on drugs, and public health. Am J Public Health. 2008;98(suppl 9):S176–S180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005;61(3):673–684. [DOI] [PubMed] [Google Scholar]
- 43.London AS, Myers NA. Race, incarceration, and health: a life-course approach. Res Aging. 2006;28(3):409–422. [Google Scholar]
- 44.Schnittker J, Massoglia M, Uggen C. Incarceration and the health of the African American community. Du Bois Rev. 2011;8(1):133–141. [Google Scholar]
- 45.Alexander M. The new Jim Crow: how the war on drugs gave birth to a permanent American undercast. Mother Jones. March 8, 2010. Available at: http://motherjones.com/politics/2010/03/new-jim-crow-war-on-drugs. Accessed August 19, 2011.
- 46.Murray P. States’ Laws on Race and Color. Athens, GA: Women’s Division of Christian Services; 1950.
- 47.Anderson C. Eyes Off the Prize: The United Nations and the African American Struggle for Human Rights, 1944–1955. Cambridge, UK: Cambridge University Press; 2003.
- 48.Chafe WH, Gavins R, Korstad R, eds. Remembering Jim Crow: African Americans Tell About Life in the Segregated South. New York, NY: New Press; 2001.
- 49.US Department of Justice, Civil Rights Division. Available at: http://www.justice.gov/crt. Accessed August 19, 2011.
- 50.Almond DV, Chay KY, Greenstone M. Civil rights, the War on Poverty, and Black–White convergence in infant mortality in the rural South and Mississippi. December 31, 2006. MIT Economics Working Paper 07–04. Available at: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=961021. Accessed August 19, 2011. [Google Scholar]
- 51.Quadagno J, McDonald S. Racial segregation in southern hospitals: how Medicare ‘‘broke the back of segregated health services.” In: Green EC, ed. The New Deal and Beyond: Social Welfare in the South Since 1930. Athens: University of Georgia Press; 2003:120–137.
- 52.Smith DB. Racial and ethnic health disparities and the unfinished civil rights agenda. Health Aff (Millwood). 2005;24(2):317–324. [DOI] [PubMed] [Google Scholar]
- 53.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol. 2004;33(3–4):119–130. [DOI] [PubMed] [Google Scholar]
- 55.Carson B, Dunbar T, Chenhall RD, Bailie R. Social Determinants of Indigenous Health. Crows Nest, Australia: Allen & Unwin; 2007. [Google Scholar]
- 56.Appiah A. The Honor Code: How Moral Revolutions Happen. New York, NY: WW Norton; 2010.
- 57.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. [DOI] [PubMed] [Google Scholar]
- 58.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. [DOI] [PubMed] [Google Scholar]
- 59.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. [DOI] [PubMed] [Google Scholar]
- 60.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24(3):438–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ajrouch KJ, Reisine S, Lim S, Sohn W, Ismail A. Perceived everyday discrimination and psychological distress: does social support matter? Ethn Health. 2010;15(4):417–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in Black and White Americans. Psychosom Med. 2010;72(3):266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pérez DJ, Fortuna L, Alegría M. Prevalence and correlates of everyday discrimination among U.S. Latinos. J Community Psychol. 2008;36(4):421–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health. 2007;97(7):1275–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Banks KH, Kohn-Woods LP, Spencer M. An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Ment Health J. 2006;42(6):555–570. [DOI] [PubMed] [Google Scholar]
- 66.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96(7):1265–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lewis TT, Everson-Rose S, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68(3):362–368. [DOI] [PubMed] [Google Scholar]
- 68.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fennelly K. Prejudice towards immigrants in the Midwest. : Massey DS, ed. New Faces in New Places: The Changing Geography of American Immigration. New York, NY: Russell Sage Foundation; 2008:151–210.
- 70.Waters MC. Black Identities: West Indian Immigrant Dreams and American Realities. New York, NY: Russell Sage Foundation; 2001.
- 71.Waters MC, Ueda R, Marrow HB, eds. The New Americans: A Guide to Immigration Since 1965. Cambridge, MA: Harvard University Press, 2007.
- 72.Hall SP, Carter RT. The relationship between racial identity, ethnic identity, and perceptions of racial discrimination in an Afro-Caribbean descent sample. J Black Psychol. 2006;32(2):155–175. [Google Scholar]
- 73.Deaux K, Bikmen N, Gilkes A, et al. Becoming American: Stereotype threat effects in Afro-Caribbean immigrant groups. Soc Psychol Q. 2007;70(4):384–404. [Google Scholar]
- 74.Dominguez TP, Strong EF, Krieger N, Gillman MW, Rich-Edwards JW. Differences in the self-reported racism experiences of US-born and foreign-born Black pregnant women. Soc Sci Med. 2009;69(2):258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65(7):1524–1535. [DOI] [PubMed] [Google Scholar]
- 76.Araújo BY, Borrell LN. Understanding the link between discrimination, mental health outcomes, and life chances among Latinos. Hisp J Behav Sci. 2006;28(2):245–266. [Google Scholar]
- 77.Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc Sci Med. 2007;64(10):1984–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yoo HC, Gee GC, Takeuchi D. Discrimination and health among Asian American immigrants: disentangling racial from language discrimination. Soc Sci Med. 2009;68(4):726–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Krieger N, Kosheleva A, Waterman PD, Chen JT, Koenen K. Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born Black Americans. Am J Public Health 2011;101(9):1704–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shariff-Marco S, Breen N, Landrine H, et al. Measuring everyday racial/ethnic discrimination in health surveys. Du Bois Rev. 2011;8(1):159–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health. 2003;93(2):277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatatoa RA, Cohen B, eds. Critical Perspectives on Racial and Ethnic Differences in Later Life. Washington, DC: National Research Council, National Academies Press; 2003:227–266.
- 83.Hanley JA. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health. 2001;55(7):508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kent MM. Immigration and America’s Black population. Popul Bull. 2007;62(4):1–16. [Google Scholar]
- 85.US Census Bureau. American Community Survey. Available at: http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=ACS&_submenuId=&_lang=en&_ts=. Accessed August 19, 2011.
- 86.Brown TN. Measuring self-perceived racial and ethnic discrimination in social surveys. Sociol Spectr. 2001;21(3):377–392. [Google Scholar]
- 87.Shariff-Marco S, Gee GC, Breen N, et al. A mixed-methods approach to developing a self-reported racial/ethnic discrimination measure for use in multiethnic health surveys. Ethn Dis. 2009;19(4):447–453. [PMC free article] [PubMed] [Google Scholar]
- 88.Albert MA, Cozier Y, Ridker PM, et al. Perceptions of race/ethnic discrimination in relation to mortality among Black women: results from the Black Women’s Health Study. Arch Intern Med. 2010;170(10):896–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Taylor TR, Williams CD, Makambi KH, et al. Racial discrimination and breast cancer incidence in US Black women: the Black Women’s Health Study. Am J Epidemiol. 2007;166(1):46–54. [DOI] [PubMed] [Google Scholar]
- 90.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85(2):197–216. [DOI] [PubMed] [Google Scholar]
- 91.Greenwald AG, Poehlman TA, Uhlmann E, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. [DOI] [PubMed] [Google Scholar]
- 92.Fazio RH, Olson MA. Implicit measures in social cognition: their meaning and use. Annu Rev Psychol. 2003;54:297–327. [DOI] [PubMed] [Google Scholar]
- 93.Carney DR, Banaji MR, Krieger N. Implicit measures reveal evidence of personal discrimination. Self Identity. 2010;9(2):162–176. [Google Scholar]
- 94.Krieger N, Carney D, Lancaster K, Waterman PD, Kosheleva A, Banaji M. Combining implicit and explicit measures of racial discrimination in health research. Am J Public Health. 2010;100(8):1485–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Crosby F. Relative Deprivation and Working Women. New York, NY: Oxford University Press; 1982.
- 96.Taylor DM, Wright SC, Moghaddam FM, Lalonde RN. The personal/group discrimination discrepancy. Pers Soc Psychol Bull. 1990;16(2):254–262. [Google Scholar]
- 97.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young Black and White adults. Am J Public Health. 1996;86(10):1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Huebner DM, Davis MC. Perceived antigay discrimination and physical health outcomes. Health Psychol. 2007;26(5):627–634. [DOI] [PubMed] [Google Scholar]
- 99.Chae DH, Lincoln KD, Adler NE, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Soc Sci Med. 2010;71(6):1182–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tudor Hart J. The inverse care law. Lancet. 1971;297(7696):405–412. [DOI] [PubMed] [Google Scholar]
- 101.Krieger N, Chen JT, Waterman PD, et al. The inverse hazard law: blood pressure, sexual harassment, racial discrimination, workplace abuse and occupational exposures in US low-income Black, White, and Latino workers. Soc Sci Med. 2008;67(12):1970–1981. [DOI] [PubMed] [Google Scholar]
- 102.Barbeau EM, Hartman C, Quinn MM, Stoddard AM, Krieger N. Methods for recruiting White, Black, and Hispanic working-class women and men to a study of physical and social hazards at work: the United for Health Study. Int J Health Serv. 2007;37(1):127–144. [DOI] [PubMed] [Google Scholar]
- 103.Krieger N, Waterman PD, Hartman C, et al. Social hazards on the job: workplace abuse, sexual harassment, and racial discrimination—a study of Black, Latino, and White low-income women and men workers in the United States. Int J Health Serv. 2006;36(1):51–85. [DOI] [PubMed] [Google Scholar]
- 104.Quinn MM, Sembajwe G, Stoddard AM, et al. Social disparities in the burden of occupational exposures: results of a cross-sectional study. Am J Ind Med. 2007;50(12):861–875. [DOI] [PubMed] [Google Scholar]
- 105.Sembajwe G, Quinn M, Kriebel D, Stoddard A, Krieger N, Barbeau E. The influence of sociodemographic characteristics on agreement between self-reports and expert exposure assessments. Am J Ind Med. 2010;53(10):1019–1031. [DOI] [PubMed] [Google Scholar]
- 106.Krieger N, Kaddour A, Koenen K, et al. Occupational, social, and relationship hazards and psychological distress among low-income workers: implications of the “inverse hazard law.” J Epidemiol Community Health. 2011. [DOI] [PubMed] [Google Scholar]
- 107.Satel SL. PC, MD: How Political Correctness Is Corrupting Medicine. New York, NY: Basic Books; 2000.
- 108.Krieger N. Stormy weather: race, gene expression, and the science of health disparities. Am J Public Health. 2005;95(12):2155–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Krieger N. Data, “race,” and politics: a commentary on the epidemiological significance of California’s Proposition 54. J Epidemiol Community Health. 2004;58(8):632–633. [DOI] [PMC free article] [PubMed] [Google Scholar]