Abstract
Objective:
Accurate prediction of the surgical outcome is important in treating dentofacial deformities. Visualized treatment objectives usually involve manual surgical simulation based on tracing of cephalometric radiographs. Recent technical advancements have led to the use of computer assisted imaging systems in treatment planning for orthognathic surgical cases. The purpose of this study was to examine and compare the ability and reliability of digitization using Dolphin Imaging Software with traditional manual techniques and to compare orthognathic prediction with actual outcomes.
Materials and Methods:
Forty patients consisting of 35 women and 5 men (32 class III and 8 class II) with no previous surgery were evaluated by manual tracing and indirect digitization using Dolphin Imaging Software. Reliability of each method was assessed then the two techniques were compared using paired t test.
Result:
The nasal tip presented the least predicted error and higher reliability. The least accurate regions in vertical plane were subnasal and upper lip, and subnasal and pogonion in horizontal plane. There were no statistically significant differences between the predictions of groups with and without genioplasty.
Conclusion:
Computer-generated image prediction was suitable for patient education and communication. However, efforts are still needed to improve accuracy and reliability of the prediction program and to include changes in soft tissue tension and muscle strain.
Keywords: Dolphin Imaging Software, Prediction, Visual Treatment Objectives (VTO)
INTRODUCTION
Surgical correction of dentofacial deformities for facial aesthetic improvement is the ultimate goal of orthognathic surgical intervention [1]. Therefore, a successful orthognathic surgery includes the precise surgical technique and occlusal correction with the accomplishment of aesthetic goals that are gratification to both patients and professionals [2–5].
Cephalometric radiographs have become an essential tool in the orthognathic surgery procedure. Traditionally, cephalometric images have been analyzed by tracing the radiograph manually, which is time-consuming and has the disadvantage of random and systematic error when locating landmarks [6]. Computer technology has made digital tracing possible, either by direct or indirect digitization of the radiograph [7].
Orthognathic prediction tracing is important for several reasons:
The actual procedure and the required anteroposterior and vertical movements may be decided upon by the model surgery.
The change of soft tissue responding to hard tissue movement may be ascertained.
To determine whether or not an adjunctive surgical procedure like genioplasty is necessary. By superimposition of the photographs, patients may be given an idea of the surgical outcome. Computer-aided diagnosis and treatment planning has become more common in the recent years and it has been shown that predictive software works well in usual cases. Hence, Dolphin Imaging has become increasingly popular among surgeons and orthodontists. After programming of the hard tissue movement into the Dolphin System, the outline of the soft tissue is changed based on ratios which have been explained and included into the Dolphin System before [8–11].
After the cephalograms are scanned, version 10 of the Dolphin Imaging Software implies the indirect digitization of dental, skeletal and soft-tissue landmarks. In order to help landmark position, the image may be improved and magnified [6]. Since the change in soft tissue profile is directly related to the hard tissue changes, it is important that the system accurately predicts hard tissue changes. Clinical usefulness of the Dolphin System is determined by accurate prediction of the hard tissue. There were two main objectives for this study; first, to assess the precision of Dolphin Imaging Version 10 in comparison with the traditional manual tracing; second to know which of the following two is more appropriate: 1) Achieving soft tissue esthetic goals by changing the underlining hard tissue. 2) Prediction of soft tissue using E-line or H-line that may help to estimate hard tissue changes before surgery. The patient’s profile arising from soft tissue response to the underlying skeletal changes and the soft tissue profile and coverage is more important than the hard tissue. That is why one needs to know which of the above two is more convenient.
MATERIALS AND METHODS
The sample consisted of 40 patients (35 women and five men, 32 were class III and eight were class II) who met the following criteria:
Adults older than 19 years (mean age, 23.5; age range, 19 to 28 years).
Underwent orthognathic surgery.
No congenital craniofacial deformities or trauma and no head and neck surgical history.
Patients must have lateral cephalometry before and at least 6 months after orthognathic surgery in the Natural Head Position (NHP) with teeth in centric relation and relaxed lip posture with a clear shadow of the soft tissue. All of the cases had undergone orthodontic treatment prior to orthognathicsurgery, the surgical correction should have been performed by one of the two consultant maxillofacial surgeons. The surgical procedures for correction of the malocclusions were variable (Table 1). A treatment plan for each patient was developed based on clinical examination, preoperative study models and preoperative cephalometric evaluation. The pre- and postsurgery lateral cephalograms were digitized. In the manual procedure both pre- and post-operative cephalograms were traced on the acetate papers. All the pre-operative cephalograms were predicted upon an orthognathic procedure and then we compared real post-operative cephalograms and manual predicted pictures. In the software procedure, both pre- and post-operative cephalograms were scanned for Dolphin imaging software (version 10) and were traced and predicted with that software, and then we superimposed traced post operativecephalograms and predicted cephalograms.
Table 1.
Surgical procedures
| Procedure | Number |
|---|---|
| Mandibular advancement | 6 |
| Mandibular setback | 4 |
| Maxillary advancement | 3 |
| Maxillary impaction | 1 |
| Maxillary advancement and impaction | 5 |
| Bimaxillary osteotomy | 20 |
| Maxillary advancement and mandibular setback | 14 |
| Maxillary impaction and mandibular advancement | 2 |
| Maxillary impaction and mandibular setback | 4 |
| Genioplasty | 13 |
To determine operator reliability and reproducibility, and to establish reproducibility of both methods, all 80 radiographs were retraced for both methods.
We compared predicted cephalograms produced by Dolphin and manual methods to know which procedure was closer to reality; i.e., post-operative cephalograms. To allow optimal landmark identification both manually and automatically, all tracings and digitizations were performed in a dark room by the same operator.
Method of prediction
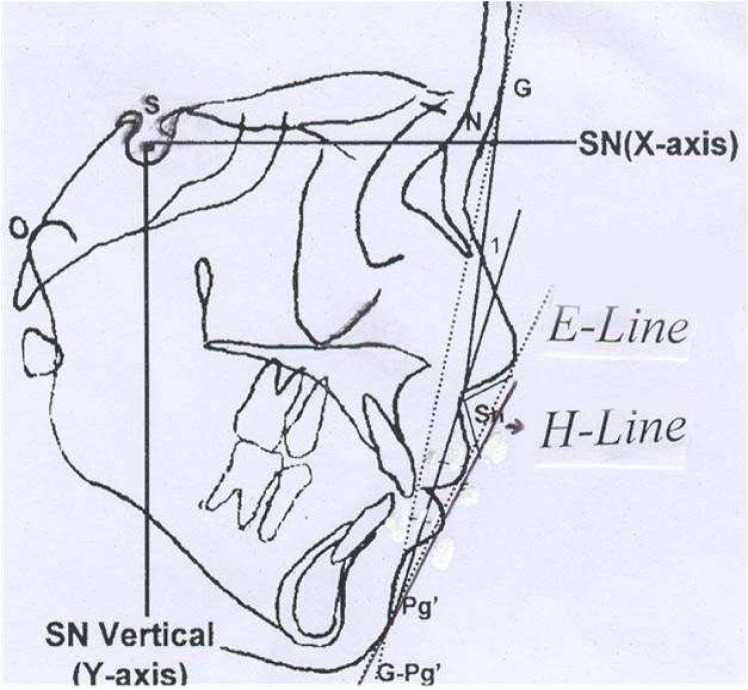
The sagittal and vertical treatment changes were evaluated by linear measurements within an X–Y coordinate system (Fig 1). The SN plane was defined as the horizontal reference plane (x-axis), and a line perpendicular to this plane through sella was defined as the vertical reference plane (y-axis). Landmarks of sella (S), nasion (N), and porion (Po) in the presurgical tracing were all transferred to the postsurgical tracing in the same patient.
Fig 1.
A, Cephalometric landmarks used in this study: S, sella; N, nasion; Po, porion; G, glabella; Prn, tip of nose; Sn, subnasale; A’_ soft tissue A point; UL, upper lip; LL, lower lip; B’_ soft tissue B point; Pg’_ soft tissue pogonion; Pg, pogonion; LIX, lower incisal apex; LI, lower incisal tip; UI, upper incisal tip; UIX, upper incisal apex. B, Linear measurement: E-line: The line that is tangent to tip of nose and soft tissue pogonion. H-line: The line that is tangent to upper lip and soft tissue pogonion.
To guarantee accurate relocation of the X–Y planes, tracings of presurgical and postsurgical cephalograms were placed on each other at the cranial base.
Digital tracing and prediction
The cephalograms were scanned using a flatbed scanner (Microtec scan wizard 5, 9600×4800 DPI, running on Microsoft Windows 2003). After finding two 100 mm-apart selected spots on the calibration ruler, the landmarks were digitized by the Dolphin system directly on-screen with a cross-hair detector conducted by the mouse. In case of encountering any problem, manipulation and enhancement were used to help point recognition.
First the tracing was digitized and input into the computer system. Then the skeletal and dental landmarks were pointed out by Dolphin software on the lateral cephalogram.
The hard tissue image was moved according to the treatment change in the software. The estimated outline of the soft tissue and the equivalent coordinates of the soft tissue points were produced automatically.
The ratio of soft tissue to hard tissue movement is varied according to the specific parts of the hard tissue.
The differences in soft tissue outline between predicted tracing and the actual profile were compared to test the accuracy of this system. The landmarks were the tip of the nose (Prn), subnasal (Sn), soft tissue A point (A'), soft tissue B point (B'), upper lip (UL), lower lip (LL) and soft tissue pogonion (Pg').
The distance from the upper lip to E-line, the lower lip to E-line and the lower lip to H-line were also evaluated.
The perpendicular distance of each of these landmarks in prediction and postsurgical cephalograms to both reference planes (x- and y-axis) was measured. The changes of soft tissue in each case were obtained from the differences between Dolphin and manual prediction compared to the actual postsurgical position.
Manual tracing and prediction
The reasons why we used Epker’s orthodontic-surgical cephalometric prediction tracing for manual prediction [2, 12–18] are as follows:
Epker prediction procedure was composed of both surgical and orthodontic procedures.
We wanted to predict surgical procedures so using surgery references were preferable and among them the Epker prediction procedure was the best.
Statistical Analysis
The data were analyzed using paired t test for statistical analyses. First the mean of prediction error was computed. Then the absolute error was compared with paired t test (Tables 2 and 3).
Table 2.
Soft tissue to hard tissue movement ratio13–17
| Treatment | Soft tissue change |
|---|---|
| Mandibular Advancement & Setback 50% | Chin: Soft tissue 1:1 with bone, lower lip to 70% with incisor |
| Maxillary Advancement | Nose: Nasal tip advances & elevates 2mm for7mm advancement at point A Subnasal: Thickness of upper lip≤17mm, subnasal advances 50% of point A. thickness of upper lip>17 mm, subnasal advances 33% of point A, Base of upper lip: 20% of point A Upper lip: 50% of incisor protraction, shortens 1 to 2 mm |
| Maxillary Impaction | Nose: for 10mm impaction the tip of nose elevates 1mm andadvances 0.5mm Upper lip: shortens 1 to 2mm Lower lip: rotates 1:1 with mandible |
Table 3.
Frequency of predicted errors
| Horizontal (%) | Vertical (%) | |||||
|---|---|---|---|---|---|---|
| <−1 | −1≫1 | >1 | <−1 | −1≫1 | >1 | |
| Pm,m | 15 | 77.5 | 7.5 | 7.5 | 82.5 | 10 |
| Pm,d | 27.5 | 65 | 7.5 | 17.5 | 72.5 | 10 |
| Sn,m | 15 | 75 | 10 | 15 | 77.5 | 7.5 |
| Sn,d | 30 | 62.5 | 7.5 | 22.2 | 65 | 12.5 |
| A,m | 47.5 | 47.5 | 5 | 0 | 90 | 10 |
| A,d | 47.5 | 50 | 12.5 | 5 | 85 | 10 |
| Ul,m | 35 | 57.5 | 7.5 | 10 | 77.5 | 12.5 |
| Ul,d | 45 | 37.5 | 17.5 | 22.5 | 60 | 17.5 |
| Ll,m | 30 | 40 | 30 | 12.5 | 37.5 | 50 |
| Ll,d | 47.5 | 35 | 17.5 | 17.5 | 47.5 | 35 |
| B,m | 22.5 | 37.5 | 15 | 12.5 | 72.5 | 15 |
| B,d | 47.5 | 30 | 22.5 | 20 | 52.5 | 27.5 |
| Pg,m | 27.5 | 52.5 | 20 | 5 | 62.5 | 32.5 |
| Pg,d | 47.5 | 32.5 | 20 | 17.5 | 60 | 22.5 |
NOTE: Predicted errors were divided into three categories: error <−1 mm, error between −1 and 1 mm, and error >1 mm. Abbreviation: Prn, tip of nose; Sn, subnasal; A, A’ point; B, B’ point; Ul, upper lip; Ll, lower lip; Pg, soft tissue pogonion; m, manual; d, dolphin.
RESULTS
The distribution of the predicted errors in the horizontal and vertical planes is shown in Table 2.
The data were divided into three categories (error <−1 mm, error between −1 and 1 mm, and error >1 mm). The most reliable region predicted by the software was the tip of the nose.
That was also the case for manual prediction with an error between −1 and 1 mm on the horizontal plane in 77.5% of the cases. The predictions on the vertical plane— consisting of Prn, A', B', Ll and Pg'—did not have any statistically significant differences compared to those of the postsurgical measurements (p<0.05).
But the predicted errors of Sn (v) (p=0.026) and Ul (v) (0.036) showed statistically significant differences between the predicted and measured landmarks.
The manual prediction was better than the Dolphin Imaging Software predictionin this subject. In horizontal dimension, Sn (p=0.006) and Pg' (p=0.022) showed statistically significant differences between the prediction and actual measurements.
Paired samples t test analysis showed the manual prediction was better than Dolphin prediction. Comparison of the predicted errors between the patients with and without genioplasty procedure revealed no statistically significant differences (Table 3).
This study also showed that the predicted vertical plane was more reliable than the horizontal plane.
The predicted errors of other linear measurements are listed in Table 4.
Table 4.
Frequency predicted errors. Comparison between groups with and without genioplasty
| Horizontal (%) | Vertical (%) | |||||
|---|---|---|---|---|---|---|
| <−1 | −1≫1 | >1 | <−1 | −1≫1 | >1 | |
| Pm,m | 11.1 | 77.8 | 11.1 | 7.4 | 88.9 | 3.7 |
| Pm,d | 22.2 | 70.3 | 7.4 | 11.1 | 74.1 | 14.8 |
| Sn,m | 11.1 | 85.2 | 3.7 | 14.8 | 77.8 | 7.4 |
| Sn,d | 33.3 | 63 | 3.7 | 22.2 | 63 | 14.8 |
| A,m | 44.5 | 48.1 | 7.4 | 33.3 | 55.6 | 11.1 |
| A,d | 33.9 | 55.6 | 11.1 | 3.7 | 85.2 | 11.1 |
| Ul,m | 26 | 66.6 | 7.4 | 7.4 | 77.8 | 11.1 |
| Ul,d | 48.1 | 29.6 | 22.3 | 22.3 | 55.4 | 22.3 |
| Ll,m | 33.3 | 40.7 | 26 | 11.1 | 37 | 51.8 |
| Ll,m,g | 23 | 38.5 | 38.5 | 15.4 | 38.5 | 46.1 |
| Ll,d | 48.2 | 33.3 | 18.5 | 22.2 | 40.8 | 37 |
| Ll,d,g | 48.1 | 38.5 | 15.4 | 7.7 | 61.5 | 30.8 |
| B,m | 26 | 33.3 | 40.5 | 14.8 | 66.7 | 18.5 |
| B,m,g | 15.4 | 46.1 | 38.5 | 7.7 | 84.6 | 7.7 |
| B,d | 37 | 37 | 26 | 22.2 | 51.8 | 26 |
| B,d,g | 69.2 | 15.4 | 15.4 | 15.4 | 53.8 | 30.8 |
| Pg,m | 29.6 | 40.8 | 29.6 | 7.4 | 63 | 29.6 |
| Pg,m,g | 23.1 | 53.8 | 23.1 | 0 | 61.5 | 38.5 |
| Pg,d | 37 | 33.3 | 29.6 | 11.1 | 59.3 | 29.6 |
| Pg,d,g | 69.2 | 30.8 | 0 | 15.4 | 61.5 | 23.1 |
NOTE: Predicted errors were divided into three categories: error <−1 mm, error between −1 and 1 mm, and error >1 mm. Abbreviation: Prn, tip of nose; Sn, subnasal; A, A’ point; B, B’ point; Ul, upper lip; Ll, lower lip; Pg, soft tissue pogonion; m, manual; d, dolphin. ; g, genioplasty.
The linear measurement showed that the software and manual methods predicted upper lips in a more retrusive position than the actual position.
The manual prediction of the location of the lower lips were in a more superior position than the actual ones (p<0.05).
For the H-line, 2.5% of the manual predictions and 25% of Dolphin predictions were concentrated on the ideal distance (a distance between −6 and 2). For the E-line, the manual method predicted that the lower lip was more concentrated on the ideal distance (distance between −2 and 0) and that the upper lip was 32.5% in the ideal distance (distance between −4 and −2). These are shown in Tables 5.
Table 5.
Frequency of E and H-Line predicted errors
|
Horizontal (%)
| ||||
|---|---|---|---|---|
| <−1 | −1≫1 | >1 | ||
| Uper Lip to E Line,m | 32.5 | 47.5 | 20 | |
| Uper Lip to E Line,d | 15 | 52.5 | 32.5 | |
| Lower Lip to E Line,m | 40 | 35 | 25 | |
| Lower Lip to E Line,d | 17.5 | 45 | 37.5 | |
| Lower Lip to H Line,m | 25 | 45 | 30 | |
| Lower Lip to H Line,d | 25 | 45 | 30 | |
NOTE: Predicted errors were divided into three categories: error <−1 mm, error between −1 and 1 mm, and error >1 mm. Abbreviation: m, manual; d, dolphin.
DISCUSSION
The accuracy of the computer-predicted images after orthognathic surgery has been examined in many studies [9, 19, 20–26].
The results of this study showed that the predicted vertical plane was more accurate than the horizontal plane and the tip of nose was the most reliable region the software could predict. Our findings showed that subnasal (Sn) had the least accurate prediction while Chien-Hsun et al. [1] showed that the lower lip had the least accurate prediction.
The low accuracy of the lower lip could be explained in several ways. The lower lip is pliable and subject to the influence of incisor position and angulations, soft tissue thickness and tonicity, perioral musculature and underlying muscle attachments [27]. Since Dolphin version 10 was used in our study as opposed to Dolphin version 8, which was used in Chien-Hsun’s work [1] and because Epker’s prediction procedure is more accurate than the other manual procedures, lower lip prediction results were better in our research. On the other hand, Sn was not clear in cephalometry and it was very hard to exactly locate it with Dolphin or manual tracing and the possibility of surgeon error in cutting the Sn could be potential causes for the low prediction accuracy of Sn in our research. The treatment simulation of the lower lip was shown to be in a more superior position and the upper lip was shown to be in a more retrusive position than the actual postsurgical results.
However, Chew et al. [28] and several other clinical studies [1, 29, 30] have shown overestimations of horizontal positions of the lips. Errors in linear measurement showed that our predicted lips were in acceptable positions.
The results were not similar to those of Upton [31] who stated that the predicted distance from the lips to E-line was larger than actual. These may be due to the fact that we predicted the lower lip more accurately than other researches.
Single-jaw osteotomy cases had better gradings in comparison to bimaxillary osteotomy cases.
Skeletal class III cases managed by bimaxillary osteotomy were least accurately predicted by the computer program. These findings were similar to Chew et al.’s study [28].
In our study, we also aimed to know if we could use E- or H-line as a reference line for predicting soft tissue that might help to estimate the amount of hard tissue movement, a goal which was not achieved.
There are many beautiful people in the world with no perfect cephalometric references.
So, using only these standards is not reliable or presentable for postsurgical orthognathic esthetic evaluation. In other words, esthetics is not just based on the cephalometric scale ratios in the soft tissue, a topic which demands more future search. The autorotation of the mandible is important in prediction, which is a feature that Dolphin Imaging Software version 10 does not offer; rather, Dolphin just makes freeway space that brings about error in the lips and the chin position.
Manual and Dolphin prediction do not allow canting and asymmetric advancements or setbacks because they are only 2-dimensional predictions; so it makes some error in prediction.
The prediction results of orthognathic surgery with or without genioplasty were similar and we did not find any statistically significant differences between the outcomes of the patients with and without genioplasty. This is similar to the findings of Chien-Hsun et al. [1] and Upton et al. who used Quick Ceph to predict the postsurgical soft tissue profile [32], but the clinical significance needs to be further investigated. All programs simulating soft tissue response to surgery are based on algorithms that relate the soft tissues to skeletal repositioning. As a result, these programs are not eventually as reliable as traditional techniques for planning orthognathic movement.
Dolphin Imaging Software may be used to determine postsurgical cephalometric measurements with comparable accuracy to those of the traditional method. The Dolphin Imaging Software version 10 needs to be re-assessed for software errors that may result in clinically significant miscalculations, e.g., to facilitate compensation of radiographic magnification when using linear measurements. It also needs to correct the mandibular autorotation and the lips position. This software provides features like vertically and horizontally adjusting lips and soft tissue. However, it should consider soft tissue tension and muscle strain. A modified version of Dolphin Imaging Software can potentially provide a more accurate and reliable prediction of postsurgical cephalometric measurements, which will lead to a better orthognathic surgery planning.
Acknowledgments
This investigation was supported by vice Chancellor for Reserch Dental School of Tehran University of Medical Sciences, grant No. 132/8703.
REFERENCES
- 1.Lu CH, Ko EW, Huang CS. The accuracy of video imaging prediction in soft tissue outcome after bimaxillaryorthognathic surgery. J Oral MaxillofacSurg. 2003 Mar;61(3):333–42. doi: 10.1053/joms.2003.50058. [DOI] [PubMed] [Google Scholar]
- 2.Epker BN, Stella JP, Fish LC. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St Louis, MO: Mosby Year Book; 1995. p. 574. [Google Scholar]
- 3.Proffit WR, White RP. The need for surgical orthodontic treatment. St Louis, MO: Mosby Year Book; 1991. p. 2. [Google Scholar]
- 4.Sarver DM, Johnston MW, Matukas VJ. Video-imaging for planning and counseling in orthognathic surgery. J Oral MaxillofacSurg. 1988 Nov;46(11):939–45. doi: 10.1016/0278-2391(88)90330-8. [DOI] [PubMed] [Google Scholar]
- 5.Sarver DM, Johnston MW. Video-imaging: techniques for superimposition of cephalometric radiography and profile images. Int J adult OrthodonOrthognathSurg. 1990;5(4):241–8. [PubMed] [Google Scholar]
- 6.Power G, Breckon J, Sherriff M, McDonald F. Dolphin Imaging Software: an analysis of the accuracy of cephalometric digitization and orthognathic prediction. Int J Oral MaxillofacSurg. 2005 Sep;34(6):619–26. doi: 10.1016/j.ijom.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Lew KK. The reliability of computerized soft tissue prediction following bimaxillary anterior subapical osteotomy. Int J Adult OrthodonOrthognathSurg. 1992;7(2):97–101. [PubMed] [Google Scholar]
- 8.Hing NR. The accuracy of computer generated prediction tracings. Int J Oral Maxillofac Surg. 1989 Jun;18(3):148–51. doi: 10.1016/s0901-5027(89)80113-4. [DOI] [PubMed] [Google Scholar]
- 9.Engel GA, Quan RE, Chaconas SJ. Soft tissue change as a result of maxillary surgery. A preliminary study. Am J Orthod. 1979 Mar;75(3):291–300. doi: 10.1016/0002-9416(79)90276-8. [DOI] [PubMed] [Google Scholar]
- 10.Freihofer HP. Latitude and limitations of midface movements. Br J Oral MaxillofacSurg. 1984 Dec;22(6):393–413. doi: 10.1016/0266-4356(84)90047-0. [DOI] [PubMed] [Google Scholar]
- 11.Rakosi T, Jones I, Graber TM. Color atlas of dental medicine orthodontic diagnosis. Stuttgart, New York: Germany thieme medical publisher Inc; 1993. p. 180. Georg ThiemVerlag, [Google Scholar]
- 12.Cohen AM. Uncertainty in cephalometrics. Br J Orthod. 1984 Jan;11(1):44–8. doi: 10.1179/bjo.11.1.44. [DOI] [PubMed] [Google Scholar]
- 13.Epker BN, Stella JP, Fish LC. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St Louis, MO: Mosby Year Book; 1995. p. 276. [Google Scholar]
- 14.Epker BN, Stella JP, Fish L. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St Louis, MO: Mosby Year Book; 1995. p. 810. [Google Scholar]
- 15.Epker BN, Stella JP, Fish LC. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St Louis, MO: Mosby Year Book; 1995. p. 193. [Google Scholar]
- 16.Fonseca RJ. Oral and maxillofacial surgery. 1st ed. Philadelphia, Pensylvania: WB Saunders; 2000. p. 477. [Google Scholar]
- 17.Proffit WR, White RP, Sarver DM. Contemporary treatment of dentofacial deformity. St. Louis, London: Mosby; 2003. p. 215. [Google Scholar]
- 18.Epker BN, Stella JP, Fish LC. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St Louis, MO: Mosby Year Book; 1995. p. 700. [Google Scholar]
- 19.Sinclair PM, Kilpelainen P, Phillips C, White RP, Rogers L, Sarver DM. The accuracy of video imaging in orthognathic surgery. Am J OrthodDentofacialOrthop. 1995 Feb;107(2):177–85. doi: 10.1016/s0889-5406(95)70134-6. [DOI] [PubMed] [Google Scholar]
- 20.Donatsky O, Bjørn-Jørgensen J, Hermund NU, Nielsen H, Holmqvist-Larsen M, Nerder PH. Accuracy of combined maxillary and mandibular repositioning and of soft tissue prediction in relation to maxillary anterosuperior repositioning combined with mandibular set back A computerized cephalometric evaluation of the immediate postsurgical outcome using the TIOPS planning system. J Craniomaxillofac Surg. 2009 Jul;37(5):279–84. doi: 10.1016/j.jcms.2008.12.003. Epub 2009 Feb 1. [DOI] [PubMed] [Google Scholar]
- 21.Donatsky O, Bjørn-Jørgensen J, Hermund NU, Nielsen H, Holmqvist-Larsen M, Nerder PH. Immediate postoperative outcome of orthognathic surgical planning, and prediction of positional changes in hard and soft tissue, independently of the extent and direction of the surgical corrections required. Br J Oral Maxillofac Surg. 2011 Jul;49(5):386–91. doi: 10.1016/j.bjoms.2010.06.005. Epub 2010 Jul 10. [DOI] [PubMed] [Google Scholar]
- 22.Stefanović N, Glisić B, Sćepan I. Reliability of computerized cephalometric outcome predictions of mandibular set-back surgery. SrpArhCelokLek. 2011 Mar-Apr;139(3–4):138–42. doi: 10.2298/sarh1104138s. [DOI] [PubMed] [Google Scholar]
- 23.Chew MT, Sandham A, Wong HB. Evaluation of the linearity of soft- to hard-tissue movement after orthognathic surgery. Am J OrthodDentofacialOrthop. 2008 Nov;134(5):665–70. doi: 10.1016/j.ajodo.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 24.Kaipatur NR, Flores-Mir C. Accuracy of computer programs in predicting orthognathic surgery soft tissue response. J Oral MaxillofacSurg. 2009 Apr;67(4):751–9. doi: 10.1016/j.joms.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Marchetti C, Bianchi A, Muyldermans L, et al. Validation of new soft tissue software in orthognathic surgery planning. Int J Oral MaxillofacSurg. 2011 Jan;40(1):26–32. doi: 10.1016/j.ijom.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Naoumova J, Lindman R. A comparison of manual traced images and corresponding scanned radiographs digitally traced. Eur J Orthod. 2009 Jun;31(3):247–53. doi: 10.1093/ejo/cjn110. [DOI] [PubMed] [Google Scholar]
- 27.Stella JP, Streater MR, Epker BN, Sinn DP. Predictability of upper soft tissue changes with maxillary advancement. J Oral MaxillofacSurg. 1989 Jul;47(7):697–703. doi: 10.1016/s0278-2391(89)80008-4. [DOI] [PubMed] [Google Scholar]
- 28.Chew MT, Koh CH, Sandham A, Wong HB. Subjective evaluation of the accuracy of video imaging prediction following orthognathic surgery in Chinese patients. J Oral MaxillofacSurg. 2008 Feb;66(2):291–6. doi: 10.1016/j.joms.2007.06.629. [DOI] [PubMed] [Google Scholar]
- 29.Kazandjian S, Sameshima GT, Champlin T, Sinclair PM. Accuracy of video imaging for predicting the soft tissue profile after mandibular set-back surgery. Am J OrthodDentofacialOrthop. 1999 Apr;115(4):382–9. doi: 10.1016/s0889-5406(99)70256-8. [DOI] [PubMed] [Google Scholar]
- 30.Konstiantos KA, O’Reilly MT, Close J. The validity of the prediction of Soft Tissue profile changes after LeFort I osteotomy using the dentofacial planner (computer software) Am J OrthodDentofacialOrthop. 1994 Mar;105(3):241–9. doi: 10.1016/S0889-5406(94)70117-2. [DOI] [PubMed] [Google Scholar]
- 31.Upton PM, Sadowsky PL, Sarver DM, Heaven TJ. Evaluation of video imaging prediction in combined maxillary and mandibular orthognathic surgery. Am J OrthodDentofacialOrthop. 1997 Dec;112(6):656–65. doi: 10.1016/s0889-5406(97)70231-2. [DOI] [PubMed] [Google Scholar]
- 32.Sameshima GT, Kawakami RK, Kaminishi RM, Sinclair PM. Predicting soft tissue changes in maxillary impaction surgery: a comparison of two video imaging systems. Angle Orthod. 1997;67(5):347–54. doi: 10.1043/0003-3219(1997)067<0347:PSTCIM>2.3.CO;2. [DOI] [PubMed] [Google Scholar]