Abstract
INTRODUCTION
Cystic lymphangioma is a rare benign vascular tumor that may arise in various sites, revealed at any age. Abdominal locations represent less than 10% of the cases preferentially involving the mesentery. We report a case of primary lymphangioma arising from the kidney.
PRESENTATION OF CASE
A 50-year-old woman was admitted for severe left lumbar pain. Abdominal ultrasonography and computed tomography revealed a 6 × 10 cm multiloculated cystic mass with hydronephrosis, extending along the left renal hilum. Surgical exploration revealed a retroperitoneal cystic tumor. Anatomopathologic examination concluded it to be a cystic lymphangioma.
DISCUSSION
The cystic lymphangioma is a benign malformative tumor of the lymphatic system. Surgery is the best curative treatment with complete excision, the prognosis is excellent.
CONCLUSION
Primary renal lymphangioma is exceedingly rare. Medical imaging has certain limits for the diagnosis which required histological confirmation. The treatment of choice is surgical.
Keywords: Cystic lymphangioma, Benign tumor, Diagnosis, Treatment
1. Introduction
Renal lymphangioma is a rare disorder characterized by developmental malformation of the perirenal lymphatic system.1 The lymphatic tissue around the kidney fails to establish a normal communication with the rest of the lymphatic system. This leads to dilatation of the lymphatic channels around the kidneys that can lead to formation of an unilocular or multilocular cystic mass.1 Usually seen in children, it also occurs infrequently in adults. Neck (75%) and axillary lesions (20%) are the most common manifestations of lymphangioma, but it can occur in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis.2 Lymphangioma of the kidney is extremely rare and, to our knowledge, only a few cases have been documented. We report a case of primary lymphangioma arising from the kidney and discuss the clinical, radiological and therapeutic options according of this tumor to the current literature.
2. Case report
A 50-year-old woman presented to our hospital with complaints of severe left lumbar pain. The patient had no significant medical or family history. She did not describe any kind of hematuria or fever and had no history of previous urinary stone disease or urinary tract infection.
Biochemical investigations revealed normal renal and liver function parameters. Urinalysis was normal. Chest X-ray was within normal limits. Ultrasonography of the abdomen revealed enlargement and lobulated outline of left kidney (14.9 cm) with mildly increased renal cortical echotexture. There were multiple cystic areas of varying sizes in the periphery and cystic lesions. None of the perinephric cysts showed any echogenic debris. On the right side much smaller perirenal cystic lesions were also seen. The liver, spleen, pancreas and gallbladder were normal on sonography. Computed tomography, with and without intravenous contrast, revealed a left huge retroperitoneal multilocular cystic mass (6 cm × 10 cm) with hydronephrosis, extending along the renal hilum (Figs. 1–3). Because of the cyst's impact on the left kidney, surgical treatment was performed using a retroperitoneal approach. During the surgical procedure, an 8 cm tumor was detected at the hilum of the left kidney. Macroscopically, the tumor was composed of multiple cystic lesions of varying sizes, filled with clear fluid. A small portion of the region was sent for frozen-section histopathological evaluation. The diagnosis was lymphangioma of the kidney. Because lymphangioma is a benign tumor, enucleation of the tumor was performed.
Fig. 1.
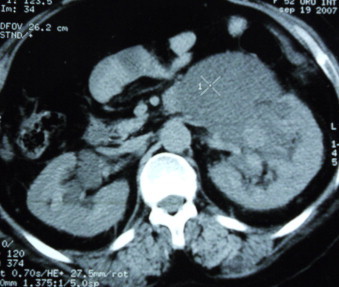
Computed tomography scan showing huge cystic lesion in the left pararenal area with hydronephrosis.
Fig. 2.
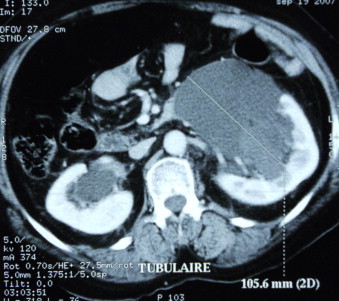
Abdominal CT showing a 10.1 cm × 6.73 cm kidney multiloculated cystic mass with hydronephrosis.
Fig. 3.
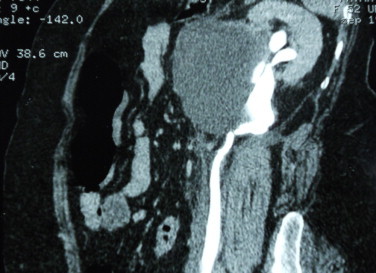
CT reveals a huge cystic mass (6 cm × 10 cm) extending along the renal hilum.
Histopathological examination showed many cystic lesions which formed by endothelial cells with focal inflammation. No signs of malignancy were seen. The surface of these cells stains positive for factors VIII, a marker for endothelium and an indicator of vascular origin, negative for keratin. These findings indicated that the tumor was cystic lymphangioma of the kidney (Fig. 4).
Fig. 4.
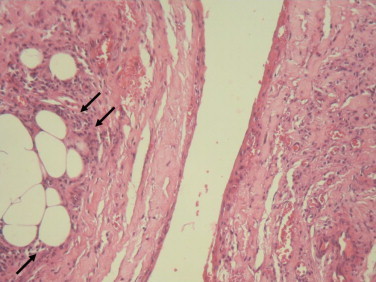
Microscopic examination shows fibromuscular walls and lymphatic vessels with endothelium cystic lesions.
The postoperative course was uneventful and the patient was discharged four days after the operation. She has been monitored for three years and remains well, with no evidence of recurrence.
3. Discussion
Lymphangiomas are rare benign malformations of the lymphatic system. Microscopically, they are classified as capillary or cavernous according to the size of the lymphatic spaces. The most common locations of the lymphangiomas are the neck and axilla (95%), and the remaining 5% are scattered throughout the body. They seem to be developmental malformations in which failure of developing lymphatic tissue to form a normal communication with the remaining lymphatic system leads to lymphangiectasia. Abnormal lymphatic channels may be simple or multilocular.3
Renal lymphangioma or lymphangiomatosis is a very rare disorder of the lymphatic system.4 The entity is thought to be the result of obstruction of the lymphatic ducts through the renal pedicle. These benign lesions have no sex predilection and have reported at all ages, from birth to 79 years of age, with most occurring during childhood and over the age of 40.2 The age distribution suggests that lymphangioma is a congenital malformation. However, it may be discovered late due to slow growth in a relatively silent area of the body.5Clinically, renal lymphangioma can be diagnosed incidentally by imaging methods or patients may present with lumbar pain or vague abdominal symptoms.6,7 Some other clinical manifestations are hypertension, hematuria, proteinuria, intracystic hemorrhage or chyluria.7,8 Lymphangiomas may enlarge and symptoms may become exacerbated during pregnancy.9 However, children may present with only nephromegaly and may be associated with obstructive uropathy.10 Lymphangioma in adults is usually characterized by peripelvic and perirenal thin-walled cysts.7 In most cases perirenal and peripelvic involvement is seen, although some may be exclusively perirenal as our patient or peripelvic involvement.7–11
Generally, diagnosis is made by ultrasound and/or CT scan, which are both very sensitive and relatively specific;12 CT and US show a cystic lesion of lymphangioma with a smooth, thin wall and septa, but sometimes irregular or calcified in appearance. The CT appearance of the fluid can vary from water density to higher densities representing increasingly mucoid fluid, hemorrhagic fluid, or calcium.2 Plain abdominal X-rays are less helpful.13 At MRI imaging, lymphangiomas appear as septate masses with heterogenous low signal intensity on T1-weighted images and with high signal intensity on T2-weighted images, but may present variable signals secondary to varying amounts of protein or hemorrhage.2
The differential diagnosis of this condition includes: autosomal dominant policystic kidney disease, although in this condition the renal parenchyma is diffusely abnormal; tumors such as liposarcoma, leiomyosarcoma, fibrosarcoma, malignant teratomas and multilocular cystic nephroma, which are predominantly cystic or necrotic, but these malignancies usually contain substantial solid components; abscess and urinoma may also produce a similar appearance, but almost all these conditions can be differentiated with the help of clinical history, normal biochemical parameters and typical imaging findings of perirenal and parapelvic involvement sparing the renal parenchyma.14The choice of treatment depends on type, size and location of the cyst. If lymphangioma of the kidney is small and does not cause any symptoms, it does not need to be surgically treated, because of its benign nature. Surgery is often required to ameliorate symptoms and for definitive diagnosis, since imaging studies are often unable to differentiate lymphangiomas from other cystic growths. If preoperative diagnosis confirms lymphangioma, it is sufficient for this tumor to be treated non-surgically only, such as injection of sclerotizing agents. Aspiration followed by sclerotherapy has been illustrated in a few case reports. Sclerotherapy may show excellent results in patients with a single lobe cyst, but repeated and frequent sclerotherapy may be required for patients with multilocular cystic lymphangioma.13–15Complete surgical excision of cystic lymphangioma as in our patient, still remains the primary treatment of choice. Yet, in order to reduce the risk of recurrence, the resection should be as complete as possible. Nevertheless, the sacrifice of adjacent structures must be avoided, and in difficult cases surgical and nonsurgical methods as sclerotherapy, may be combined generally sequentially.12,13
Laparoscopic complete excision of a multilocular renal cyst lymphangioma, has rarely been described in the literature. Barbara et al. report two successful cases of a complete resection of a retroperitoneal cystic lymphangioma.13 However, as was with the present case, most cases cannot be diagnosed accurately by imaging studies due to the rarity and lack of recognition of lymphangioma.
4. Conclusion
The cystic lymphangioma is a benign and rare tumor of the adult. The polymorphism and non specificity of clinical and radiological aspects make that the diagnosis is rarely realized at the preoperative period. Its confirmation is histologic only; the surgery with total resection is the favorite treatment. The prognosis of the cystic lymphangioma, although dominated by the risk of recidivism, is excellent.
Conflict of interest statement
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contributions
All authors contribute to manuscript.
References
- 1.Mani N.B., Sodhi K.S., Singh P., Katariya S., Poddar U., Thapa B.R. Renal lymphangiomatosis: a rare cause of bilateral nephromegaly. Australas Radiol. 2003;47(2):184–187. doi: 10.1046/j.0004-8461.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- 2.Honma I., Takagi Y., Shigyo M., Sunaoshi K., Wakabayashi J., Harada O. Lymphangioma of the kidney. Int J Urol. 2002;9(3):178–182. doi: 10.1046/j.1442-2042.2002.00437.x. [DOI] [PubMed] [Google Scholar]
- 3.Sarikaya B., Akturk Y., Bekar U., Topaloglu S. Bilateral renal lymphangiomatosis mimicking hydronephrosis: multidetector CT urographic findings. Abdom Imaging. 2006;31(6):732–734. doi: 10.1007/s00261-005-8014-y. [DOI] [PubMed] [Google Scholar]
- 4.Farb J.B., Lee E.Y. Clinical image. Infiltrative renal lymphangioma in a pediatric patient. Pediatr Radiol. 2006;36(7):718. doi: 10.1007/s00247-005-0108-8. [DOI] [PubMed] [Google Scholar]
- 5.Wadhwa P., Kumar A., Sharma S., Dogra P.N., Hemal A.K. Renal lymphangiomatosis: imaging and management of a rare renal anomaly. Int Urol Nephrol. 2007;39(2):365–368. doi: 10.1007/s11255-006-9002-z. [DOI] [PubMed] [Google Scholar]
- 6.Pickering S.P., Fletcher B.D., Bryan P.J., Abramowsky C.R. Renal lymphangioma: a cause of neonatal nephromegaly. Pediatr Radiol. 1984;14(6):445–448. doi: 10.1007/BF02343441. [DOI] [PubMed] [Google Scholar]
- 7.Varela J.R., Bargiela A., Requejo I., Fernandez R., Darriba M., Pombo F. Bilateral renal lymphangiomatosis: US and CT findings. Eur Radiol. 1998;8(2):230–231. doi: 10.1007/s003300050368. [DOI] [PubMed] [Google Scholar]
- 8.Kekre N.S., Arun N., Date A. Retroperitoneal cystic lymphangioma causing intractable chyluria. Br J Urol. 1998;81(2):327–328. doi: 10.1046/j.1464-410x.1998.00337.x. [DOI] [PubMed] [Google Scholar]
- 9.Ozmen M., Deren O., Akata D., Akhan O., Ozen H., Durukan T. Renal lymphangiomatosis during pregnancy: management with percutaneous drainage. Eur Radiol. 2001;11(1):37–40. doi: 10.1007/s003300000550. [DOI] [PubMed] [Google Scholar]
- 10.Chiu J.S., Wu C.J., Sun G.H., Lin S.H. Obstructive uropathy associated with bilateral renal lymphangiomatosis. Nephrol Dial Transplant. 2004;19(11):2923. doi: 10.1093/ndt/gfh291. [DOI] [PubMed] [Google Scholar]
- 11.Younathan C.M., Kaude J.V. Renal peripelvic lymphatic cysts (lymphangiomas) associated with generalized lymphangiomatosis. Urol Radiol. 1992;14(3):161–164. doi: 10.1007/BF02926920. [DOI] [PubMed] [Google Scholar]
- 12.Konen O., Rathaus V., Dlugy E., Freud E., Kessler A., Shapiro M. Childhood abdominal cystic lymphangioma. Pediatr Radiol. 2002;32(2):88–94. doi: 10.1007/s00247-001-0612-4. [DOI] [PubMed] [Google Scholar]
- 13.Wildhaber B.E., Chardot C., Le Coultre C., Genin B. Total laparoscopic excision of retroperitoneal cystic lymphangioma. J Laparoendosc Adv Surg Tech A. 2006;16(5):530–533. doi: 10.1089/lap.2006.16.530. [DOI] [PubMed] [Google Scholar]
- 14.Daali M., Touiti I., Hssaida R., Ameur M., Abbar M. Renal lymphangioma. Prog Urol. 2001;11(3):520–522. [PubMed] [Google Scholar]
- 15.Boussetta S., El Malki H.O., Chenna M., Mohcine R., Ifrine L., Belkouchi A. Retroperitoneal cystic lymphangioma in adults. J Afr Hépatol Gastroentérol. 2010;4:110–113. [Google Scholar]


