Abstract
Muscular dystrophies are a group of genetic disorders that specifically affect skeletal muscle and are characterized by progressive muscle degeneration and weakening. To develop therapies and treatments for these diseases, a better understanding of the molecular basis of muscular dystrophies is required. Thus, identification of causative genes mutated in specific disorders and the study of relevant animal models are imperative. Zebrafish genetic models of human muscle disorders often closely resemble disease pathogenesis, and the optical clarity of zebrafish embryos and larvae enables visualization of dynamic molecular processes in vivo. As an adjunct tool, morpholino studies provide insight into the molecular function of genes and allow rapid assessment of candidate genes for human muscular dystrophies. This unique set of attributes makes the zebrafish model system particularly valuable for the study of muscle diseases. This review discusses how recent research using zebrafish has shed light on the pathological basis of muscular dystrophies, with particular focus on the muscle cell membrane and the linkage between the myofibre cytoskeleton and the extracellular matrix.
Introduction
Muscular dystrophies (MDs) are a heterogeneous group of genetic diseases that affect different muscle groups, depending on the specific form of dystrophy. The genetic causes of more than 30 genetically distinct types of MD have been identified thus far (Bushby et al., 2009; Kaplan, 2011). The progressive degeneration of dystrophic muscles in these disorders is characterized by: abundant small-diameter fibres with central nuclei (indicating regeneration), infiltration of mononucleate cells, accumulating fibrosis and a broader variation in the size of myofibre cross-sectional areas compared with muscle in healthy individuals. In severe MDs such as Duchenne MD (DMD), affected individuals demonstrate muscle weakness from early childhood onwards, become wheelchair-dependent in their early teens and usually die in their early thirties from lung or heart failure. DMD is caused by mutations in dystrophin that lead to defects in the dystrophin-associated glycoprotein complex (DGC), which forms a link between the cytoskeleton of the muscle fibre and the extracellular matrix (ECM) (Fig. 1). Deficiencies in other components of the DGC, such as laminin-2, can elicit MD with similarly devastating symptoms (Fig. 1). On the other side of the clinical spectrum are MDs with very mild symptoms, as shown by individuals suffering from Becker MD (BMD), who in rare cases can be ambulant even late in life (England et al., 1990). Interestingly, BMD is caused by mutations that lead to only partial loss of dystrophin function. Other MDs are caused by deficiencies in the second major sarcolemmal complex, which mediates adhesion through integrins (Fig. 1). Sarcolemma-spanning integrins bind to laminin on the outside of myofibres and interact with actin on the cytosolic side, thereby forming a link between the myofibre cytoskeleton and the ECM.
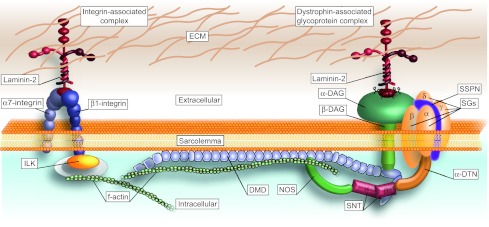
Fig. 1.
Two protein complexes constitute the main mechanical link between the actin cytoskeleton and the ECM. Owing to their pivotal role in muscle integrity, deficiencies in components of the integrin-associated complex (left) or the dystrophin-associated glycoprotein complex (DGC; right) can result in MDs. DAG, dystroglycan; DMD, dystrophin; DTN, dystrobrevin; ILK, integrin-linked kinase; NOS, nitric oxide synthase; SG, sarcoglycan; SNT, syntrophin; SSPN, sarcospan.
In addition to pharmacological approaches, different therapeutic avenues for MDs are being explored, including stem cell transplantation, gene therapy based on delivery of full-length or truncated dystrophin, and remodelling of mutated transcripts by antisense oligonucleotides (Pichavant et al., 2011). Despite remarkable advances, however, no curative treatment for any form of MD exists. To discover the genetic basis of as-yet-unidentified MDs and to further develop treatments, the establishment of animal models that can be studied more efficiently and to a greater extent than affected humans is vital.
Over the past two decades, the zebrafish (Danio rerio) has received tremendous attention owing to its advantages as a model system. The rapid external development of easily manipulatable translucent embryos together with the efficient husbandry has sparked the establishment of many models of human diseases in zebrafish, and these models often closely resemble the human condition (Lieschke and Currie, 2007). The unique combination of these advantages makes the zebrafish particularly suited for the study of muscle. Importantly, as demonstrated by synteny analysis and cross-species mutant rescue experiments (Catchen et al., 2011), the transcriptional network that activates teleost myogenesis is conserved, and orthologues of the vast majority of human MD disease genes can be identified in the zebrafish genome (Steffen et al., 2007).
In addition to zebrafish models of MDs (listed in Table 1), which facilitated many exciting insights into MD pathologies, studies of chaperones and heat-shock proteins that assist the assembly of the contractile apparatus (Etard et al., 2007; Wohlgemuth et al., 2007; Hawkins et al., 2008; Sarparanta et al., 2012) have also shed light on the basic biology of muscle cell formation and maintenance. However, this review focuses on the recent contributions of zebrafish models to our understanding of MDs that result from defects in the sarcolemma and the ECM.
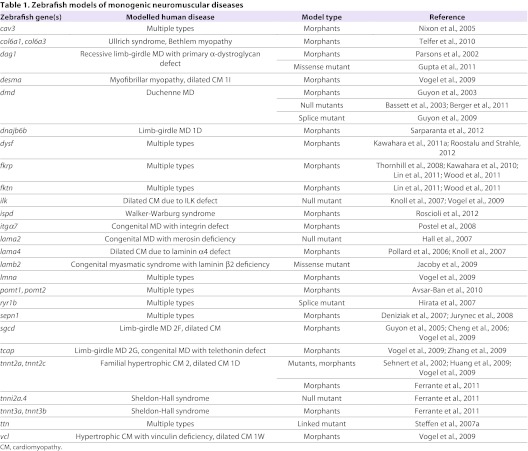
Table 1.
Zebrafish models of monogenic neuromuscular diseases
Modelling DMD and BMD
In general, a complete loss of dystrophin function results in DMD (OMIM 310200), one of the most severe and common forms of MD, and partial loss leads to the milder BMD (OMIM 300376). Nearly three decades of research on the dystrophin-deficient mouse have provided valuable insights into the biochemical function of dystrophin. Dystrophin is one of the core components of the DGC (Fig. 1) and plays a pivotal role not only in transferring the contraction force from the contractile apparatus to the ECM, but also in cell signalling, membrane stabilization and Ca2+ influx (Markert et al., 2011). Despite the detailed knowledge available on dystrophin function, no resolutive cure has been developed, partially due to the fact that dystrophin-deficient mice fail to recapitulate the clinical severity of DMD in humans (Hoffman et al., 1987; Kang, 2011). Current management of DMD is mainly based on administration of corticosteroids, which slow disease progression but do not constitute a cure.
Zebrafish models of DMD
Dystrophin deficiency has been modelled both by morpholino knockdown and by using identified null mutations in zebrafish dystrophin (Bassett et al., 2003; Guyon et al., 2003). The zebrafish dmdta222a mutant (synonyms: sapje, sap) was isolated in a forward genetic screen via its reduction in birefringence, a quantifiable effect easily detectable under polarized light (Fig. 2B,B′) (Granato et al., 1996; Berger et al., 2012). This dystrophic mutant was subsequently identified as a carrier of a dystrophin null allele (Bassett et al., 2003); other zebrafish mutant alleles were later identified (Guyon et al., 2009; Berger et al., 2011). Subsequent comparison of the dystrophin-deficient zebrafish to humans with DMD revealed that it closely resembles the human condition in severity and progression (Berger et al., 2010). In zebrafish, as in humans, dystrophin is initially expressed at the peripheral ends of the myofibres and gradually shifts to non-junctional sites (Wessels et al., 1991; Clerk et al., 1992; Chambers et al., 2001; Berger et al., 2010). In both species, dystrophin loss progressively leads to abundant necrotic myofibres being replaced by mononucleate infiltrates, extensive fibrosis accompanied by inflammation, and broader variation in the size of muscle fibre cross-sectional areas (compared with healthy muscle) (Fig. 2C,C′). Furthermore, the lack of muscle progenitor proliferation to compensate for the extensive skeletal muscle loss, as has been suggested to occur in humans, is paralleled in zebrafish (Berger et al., 2010). An interesting finding from the study of dmd zebrafish is that dystrophin-deficient mutants that are anaesthetised with Tricaine, an anaesthetic that blocks sodium channels, do not display detached myofibres. On removal of the anaesthetic, however, fibre detachment can be observed in real time (Berger et al., 2010). Although the precise mechanism that leads to muscle injury requires further investigation, generation of muscle force seems to play a crucial role in triggering myofibre detachment, at least in zebrafish. Such in vivo observations obtained with zebrafish demonstrate that using the advantages of different model systems leads to novel insights into the onset and progression of disease pathologies.
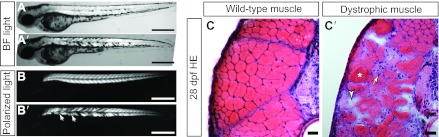
Fig. 2.
Characteristics of dystrophic muscle in zebrafish. At 3 days post fertilisation (dpf), it is challenging to distinguish a wild-type larva (A) from a dystrophic larva (A′) under bright-field conditions (apart from the marked misplaced pigment cells of the dystrophic mutant). In contrast, birefringence effectively visualizes the myofibril under polarized light, whereby somites with detached myofibres of dystrophic mutants (B′) appear darker (indicated by arrows) than wild-type somites (B). Cross-sections of 28-dpf-old wild-type (C) and dystrophin-deficient (C′) larvae stained with H&E (HE). As in humans, the dystrophin-deficient muscle of the dmd mutant is characterized by myofibre atrophy (arrowhead), infiltration of mononucleate cells (arrow), eosinophilic myofibres (asterisk) and broader variation of myofibre cross-sectional areas. Scale bars: 0.5 mm.
Dystrophin-deficient zebrafish contribute to the exploration of potential therapies for DMD
Currently, the most promising therapeutic approach for DMD is the administration of antisense oligonucleotides that alter the splicing of dystrophin pre-mRNA transcript, thereby excluding targeted exons from the mature mRNA and partially restoring functional protein (Muntoni and Wood, 2011). Although many uncertainties arising from ongoing clinical studies remain (van Deutekom et al., 2007; Kinali et al., 2009), statistically evaluated analysis of exon skipping in dystrophin-deficient zebrafish demonstrated that 20–30% of normal dystrophin transcript levels are needed to recover a severe dystrophic pathology (Berger et al., 2011). Issues regarding systemic antisense oligonucleotide administration in individuals with DMD, however, have not been addressed by this study, because oligonucleotides were injected into the yolk sack of 0.5-hour-old zebrafish embryos.
The advantages of the zebrafish were also employed in a small-molecule screen that identified 19 compounds that prevented dystrophic pathology in dystrophin-deficient zebrafish (Kawahara et al., 2011b). Zebrafish can also be used to analyze lead drugs such as PTC124, which was claimed to promote read-through of premature stop codons in the dystrophin gene (Welch et al., 2007), a claim that was subsequently disputed (Auld et al., 2010). In addition, our own data show consistently that administration of PTC124 up to toxic levels has no effect on the phenotype of dystrophin-deficient zebrafish (our unpublished results). Again, these findings demonstrate the value of the zebrafish model for fast and statistically evaluated testing of potential therapies.
Modelling dystroglycanopathies
The dystroglycan (DAG1) gene encodes α- and β-dystroglycan, which are core components of the DGC (Fig. 1). In this complex, α-dystroglycan needs to be glycosylated to bind to laminin-2, in this way linking the subsarcolemmal cytoskeleton to the ECM. Several patients have been reported that have aberrant glycosylation of α-dystroglycan that leads to a reduced binding of α-dystroglycan to laminin-2 (Godfrey et al., 2011). These individuals display a wide range of muscle symptoms, and their conditions are commonly referred to as dystroglycanopathies.
Mutations in dag1
To date, only one patient with a missense mutation in DAG1 has been reported (Hara et al., 2011). Dag1 null mice are early embryonic lethal owing to disruption of an extraembryonic basement membrane, the rodent-specific Reichert’s membrane, which controls materno-embryonic exchange upon in utero fetal implantation (Williamson et al., 1997). In contrast to the mouse model, the external development of zebrafish embryos circumvents the early embryonic lethality seen in the rodent, thereby allowing the study of the role of the orthologous dag1 gene in muscle integrity. In a morpholino-based knockdown study of the zebrafish dag1 gene, Parsons and colleagues demonstrated the pivotal role of dystroglycan for muscle integrity (Parsons et al., 2002). More recently, two zebrafish loss-of-function dag1 mutants have been described: the dag1hu3072 mutant contains a premature stop codon, and the patchytail mutant contains a missense mutation; both lack α- and β-dystroglycan protein (Gupta et al., 2011; Lin et al., 2011). In contrast to dag1hu3072 mutants, in which myofibres detach from myosepta and subsequent sarcolemmal rupture has been described (Lin et al., 2011), patchytail mutants only display widened myosepta (Gupta et al., 2011); these differences reflect the broad variation of clinical aspects seen in human dystroglycanopathies.
Interestingly, morpholino-based knockdown of maternal and zygotic contributions of dystroglycan leads to complete loss of dystrophin protein (Lin et al., 2011). Dystrophin is also absent from many fibres in dystroglycan-deficient chimaeric mice (Côté et al., 1999), and deletion of the β-dystroglycan-binding region in dystrophin leads to loss of dystroglycan (Fritz et al., 1995; Rafael et al., 1996), reinforcing the notion that dystrophin and the dystroglycans are necessary for the assembly and stability of the DGC.
Secondary dystroglycanopathies are evoked by altered glycosylation of dystroglycan
As mentioned above, defective glycosylation of α-dystroglycan can abolish binding to laminin-2, thereby resulting in MD. Over the past few years, genes involved in the glycosylation of α-dystroglycan have been reported, namely POMT1, POMT2, POMGNT1, LARGE, FKTN and FKRP. With the exception of pomgnt1, analyses of morpholino-induced knockdown in zebrafish confirm that the orthologous enzymes function similarly in zebrafish and humans (Thornhill et al., 2008; Avsar-Ban et al., 2010; Kawahara et al., 2010; Lin et al., 2011). In addition, it has been reported that zebrafish fukutin (fktn) or fukutin-related protein (fkrp) morphants show endoplasmic reticulum stress and activation of the unfolded protein response. Furthermore, vacuoles of notochord cells in these morphants contain protein accumulations that are marked by immunoreactivity with IIH6 (Lin et al., 2011), a monoclonal antibody detecting glycosylated α-dystroglycan (Ervasti and Campbell, 1993). Similar accumulations of low-molecular-weight protein complexes were also detected in α-dystroglycan-deficient zebrafish, indicating that protein secretion in dystrogly-canopathies is affected beyond glycosylation of α-dystroglycan (Lin et al., 2011).
Recently, mutations in the ISPD gene have been identified as the second most common cause of Walker-Warburg syndrome, a type of congenital MD (Roscioli et al., 2012). Morpholinos targeting ispd in zebrafish induced a phenotype that recapitulates the features of Walker-Warburg syndrome, confirming that the detected mutations in ISPD were eliciting the human condition. In addition, a cooperative interaction between ispd, fktn and fkrp in glycosylating α-dystroglycan was identified in zebrafish, demonstrating that functions previously unidentified in vertebrates can be elucidated in zebrafish (Roscioli et al., 2012). This study reinforces the usefulness of zebrafish studies for providing functional data for mutations identified in muscle disease patient cohorts.
Modelling congenital MD
The heterotrimeric laminins are major structural components of the basal lamina and are formed by three distinct chains: one α-, one β- and one γ-chain. Laminin-2 is the major muscle isoform of laminin, and is formed by a combination of α2-, β1- and γ1-chains. It can bind to either α7β1 integrin or, through α-dystroglycan, the DGC, thereby representing a core component of the two major complexes that connect the actin cytoskeleton of the myofibres to the ECM (Fig. 1). Humans with mutations in laminin α2 can acquire severe congenital MD with merosin deficiency (MDC1A; OMIM 607855) (Helbling-Leclerc et al., 1995). Although various mouse models of laminin α2 deficiency have provided valuable insights into disease development, the exact molecular basis of MDC1A pathology is not fully understood (Gawlik and Durbeej, 2011). Analysis of the zebrafish mutant candyfloss (caf), which carries a null allele of lama2, has revealed that myofibre detachment is triggered by mechanical load of the fibres rather than an intrinsic defect in cell signalling (Hall et al., 2007). Consistent with laminin-2 being located in the basal lamina outside the fibre, the sarcolemma of detaching fibres is not compromised, and detached fibres subsequently undergo apoptosis rather than necrosis, unlike the necrosis seen in DMD, where the sarcolemma is compromised (Fig. 1) (Hall et al., 2007). Importantly, muscle formation and myoblast fusion are normal in caf mutants, and primary motor neurons appear unaffected (Hall et al., 2007), further suggesting that mechanical load on the myofibre is the primary cause of muscle pathology in MDC1A.
Interestingly, the zebrafish mutant softy (sof), which carries a missense mutation in the lamb2 gene, also shows myofibre detachment at the myotendinous junction (Jacoby et al., 2009). In contrast to the dmd and caf mutants, detached myofibres remain viable and form ectopic myosepta in sof mutants, exposing a newly identified pathway that could be targeted in therapy for MDs (Jacoby et al., 2009). Although mutations in LAMB2 have so far only been associated with neuromuscular junction defects in individuals suffering from congenital myasthenic syndrome (OMIM 608931) (Maselli et al., 2009), the dystrophic phenotype of sof mutants indicates that LAMB2 is a candidate gene for genetically uncharacterized human MDs.
Another laminin-2 receptor in skeletal muscle is the heterodimeric α7β1 integrin, which, together with integrin-linked kinase (ILK), forms part of the integrin-ECM adhesion complex that structurally links the actin cytoskeleton and the ECM (Fig. 1). In rare cases, mutations in α7 integrin (ITGA7) lead to congenital MD with integrin α7 deficiency (OMIM 613204), in which patients exhibit delayed motor milestones (Hayashi et al., 1998). In zebrafish, morpholino-based knockdown of itga7 induces a dystrophic phenotype similar to the lost-contact (loc) mutant, which carries an ilk null allele that leads to loss of integrin function (Knöll et al., 2007; Postel et al., 2008). In both loc mutants and itga7 morphants, myofibres detach from the myosepta, leading to progressive paralysis (Postel et al., 2008). Importantly, the zebrafish-based study of Knöll and colleagues demonstrates an epistatic regulation between ilk and lama4, which led to the identification of previously unknown ILK and LAMA4 mutations in individuals with dilated cardiomyopathy (Knöll et al., 2007). Also noteworthy is the report that knockdown of the integrin binding partner kindlin-2 also leads to skeletal muscle damage in zebrafish (Dowling et al., 2008). Although no humans have been identified with mutations in the orthologous KIND2 to date, it might be a candidate gene for MD.
Modelling limb-girdle MD
To date, 25 types of limb-girdle MDs caused by mutations in at least 21 different genes have been catalogued (Kaplan, 2011). One of these genes encodes δ-sarcoglycan, a component of the DGC (Fig. 1), and morpholino-based studies in zebrafish have revealed that it is also required for muscle integrity in zebrafish (Guyon et al., 2005; Cheng et al., 2006). Another of these genes encodes dysferlin (DYSF) (Bashir et al., 1998; Liu et al., 1998), a key player in the repair of sarcolemmal lesions, which are frequently provoked in myofibres by mechanical stress (Bansal et al., 2003). Knockdown of dysf in zebrafish results in muscle abnormalities (Kawahara et al., 2011a) and, in a recent study, this model was used to shed new light on the exact sequential steps of sarcolemmal repair (Roostalu and Strähle, 2012). Taking advantage of the ability to undertake subcellular high-resolution imaging in living muscle in zebrafish, the authors visualized at the lesion site the formation of a repair patch that is independently assembled by the cytoplasmic annexin A6 (Anxa6) and vesicles enriched with dysferlin. Subsequently, Anxa2a is recruited to the repair patch, followed by Anxa1a, which covers the sarcolemmal lesion (Roostalu and Strähle, 2012). These studies provide a new understanding of the mechanism directed by dysferlin during the patch repair process at the damaged sarcolemma of a muscle cell, and highlight the potential to observe dynamic molecular interactions in live zebrafish.
Modelling Ullrich congenital MD and Bethlem myopathy
In addition to defective sarcolemma-spanning complexes, deficiencies in the ECM (which provides structural support to myofibres) can also cause MDs. Mutations in COL6A1, COL6A2 or COL6A3, which together form the ECM protein collagen VI, can elicit Ullrich congenital MD (UCMD; OMIM 254090) or Bethlem myopathy (BM; OMIM 158810) (Jöbsis et al., 1996; Camacho Vanegas et al., 2001). Individuals with UCMD typically suffer from severe muscle weakness with excessive joint hypermobility and contractures, whereas those with the milder BM usually have slow, progressive muscle weakness. Although Col6a1 loss-of-function mice only have a mild myopathy, reminiscent of BM (Bonaldo et al., 1998), both diseases have been modelled by using two distinct morpholinos in zebrafish (Telfer et al., 2010). Morpholinos targeting exon 9 of the orthologous zebrafish col6a1 led to a severe UCMD-like phenotype with early onset of motor deficits, whereas targeting of exon 13 induced mild myopathy with late onset of motor deficits, reminiscent of BM (Telfer et al., 2010). The ameliorative effect of the proton pump modifier cyclosporine A, described in col6a1-deficient mice (Irwin et al., 2003), was confirmed in UCMD-like zebrafish. Interestingly, although cyclosporine A improved mitochondrial appearance and decreased apoptosis, sarcolemmal integrity was not ameliorated in UCMD-like zebrafish (Telfer et al., 2010). As noted for dystrophin-deficient zebrafish above (Berger et al., 2010), severe human MDs such as UCMD or DMD are more closely modelled in zebrafish than in mice. Moreover, these zebrafish models are powerful and highly efficient for evaluating therapeutic strategies.
Concluding remarks
The results discussed above illustrate the fact that many common MDs have been successfully modelled in zebrafish. The classical ways of generating disease models in zebrafish via forward genetics based on random mutagenesis or morpholino suppression have been an important adjunct to disease gene discovery and validation. However, the lack of gene targeting has been a bottleneck in the zebrafish field. The non-directional nature of these mutations, however, enables the discovery of hypomorphic or dominant-negative alleles, which are usually induced by missense mutations. In principle, such mutations can also be re-engineered by targeted recombination – but which mutation elicits a phenotype is difficult to predict. The random mutation approach can also lead to the identification of gene functions that have not yet been associated with a certain disease condition. Nonetheless, zebrafish are at the beginning of a new age of genome manipulation: direct gene disruption is now possible with zinc-finger-nuclease and TALEN technology (Sander et al., 2011). The plummeting costs of sequencing have also enabled the identification of mutations based on the sequencing of whole DNA libraries of mutagenized genomes. This approach has sparked large-scale ventures such as the Zebrafish Mutation Project, which aims to generate a knockout allele for every zebrafish protein-coding gene (http://www.sanger.ac.uk/Projects/D_rerio/zmp). These approaches will undoubtedly increase the ability to generate human disease models in zebrafish.
Another major scientific stronghold of the fish is the ease with which dynamic cell processes can be visualized in vivo and in real time with time-lapse movies. The ability to image living muscle tissue in a disease context and to examine pathology onset in real time is a significant advantage of the zebrafish system. Myofibre detachment has been documented in dystrophin-deficient live zebrafish (Berger et al., 2010) and even subcellular processes such as the repair of myofibre lesions can be studied in this way (Roostalu and Strähle, 2012). Owing to the cost-effective breeding and husbandry of the zebrafish, small-molecule screens can be performed against dystrophic phenotypes at relatively high throughput to identify and further analyze lead drugs (Berger and Currie, 2007; Kawahara et al., 2011b). In future, more screens will be performed to identify additional compounds that might one day become effective medications to treat MD in humans.
In summary, although zebrafish are phylogenetically more distant from humans than mammalian model organisms, the main functions of the orthologous muscle genes reviewed above are conserved between zebrafish and human. Together with the unique set of tools available, the zebrafish system therefore provides valuable models for studying human MD.
Acknowledgments
We thank T. Sztal, P. R. Jusuf and T. E. Hall for critical reading.
Footnotes
COMPETING INTERESTS
The authors declare that they do not have any competing or financial interests.
FUNDING
This work was supported by the National Health and Medical Research Council of Australia [grant number 1024482] and the Muscular Dystrophy Association USA [grant number 201098].
REFERENCES
- Auld D. S., Lovell S., Thorne N., Lea W. A., Maloney D. J., Shen M., Rai G., Battaile K. P., Thomas C. J., Simeonov A., et al. (2010). Molecular basis for the high-affinity binding and stabilization of firefly luciferase by PTC124. Proc. Natl. Acad. Sci. USA 107, 4878–4883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avsar-Ban E., Ishikawa H., Manya H., Watanabe M., Akiyama S., Miyake H., Endo T., Tamaru Y. (2010). Protein O-mannosylation is necessary for normal embryonic development in zebrafish. Glycobiology 20, 1089–1102 [DOI] [PubMed] [Google Scholar]
- Bansal D., Miyake K., Vogel S. S., Groh S., Chen C. C., Williamson R., McNeil P. L., Campbell K. P. (2003). Defective membrane repair in dysferlin-deficient muscular dystrophy. Nature 423, 168–172 [DOI] [PubMed] [Google Scholar]
- Bashir R., Britton S., Strachan T., Keers S., Vafiadaki E., Lako M., Richard I., Marchand S., Bourg N., Argov Z., et al. (1998). A gene related to Caenorhabditis elegans spermatogenesis factor fer-1 is mutated in limb-girdle muscular dystrophy type 2B. Nat. Genet. 20, 37–42 [DOI] [PubMed] [Google Scholar]
- Bassett D. I., Bryson-Richardson R. J., Daggett D. F., Gautier P., Keenan D. G., Currie P. D. (2003). Dystrophin is required for the formation of stable muscle attachments in the zebrafish embryo. Development 130, 5851–5860 [DOI] [PubMed] [Google Scholar]
- Berger J., Currie P. (2007). The role of zebrafish in chemical genetics. Curr. Med. Chem. 14, 2413–2420 [DOI] [PubMed] [Google Scholar]
- Berger J., Berger S., Hall T. E., Lieschke G. J., Currie P. D. (2010). Dystrophin-deficient zebrafish feature aspects of the Duchenne muscular dystrophy pathology. Neuromuscul. Disord. 20, 826–832 [DOI] [PubMed] [Google Scholar]
- Berger J., Berger S., Jacoby A. S., Wilton S. D., Currie P. D. (2011). Evaluation of exon-skipping strategies for Duchenne muscular dystrophy utilizing dystrophin-deficient zebrafish. J. Cell. Mol. Med. 15, 2643–2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger J., Sztal T., Currie P. D. (2012). Quantification of birefringence readily measures the level of muscle damage in zebrafish. Biochem. Biophys. Res. Commun. 423, 785–788 [DOI] [PubMed] [Google Scholar]
- Bonaldo P., Braghetta P., Zanetti M., Piccolo S., Volpin D., Bressan G. M. (1998). Collagen VI deficiency induces early onset myopathy in the mouse: an animal model for Bethlem myopathy. Hum. Mol. Genet. 7, 2135–2140 [DOI] [PubMed] [Google Scholar]
- Bushby K., Lochmüller H., Lynn S., Straub V. (2009). Interventions for muscular dystrophy: molecular medicines entering the clinic. Lancet 374, 1849–1856 [DOI] [PubMed] [Google Scholar]
- Camacho Vanegas O., Bertini E., Zhang R. Z., Petrini S., Minosse C., Sabatelli P., Giusti B., Chu M. L., Pepe G. (2001). Ullrich scleroatonic muscular dystrophy is caused by recessive mutations in collagen type VI. Proc. Natl. Acad. Sci. USA 98, 7516–7521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catchen J. M., Braasch I., Postlethwait J. H. (2011). Conserved synteny and the zebrafish genome. Methods Cell Biol. 104, 259–285 [DOI] [PubMed] [Google Scholar]
- Chambers S. P., Dodd A., Overall R., Sirey T., Lam L. T., Morris G. E., Love D. R. (2001). Dystrophin in adult zebrafish muscle. Biochem. Biophys. Res. Commun. 286, 478–483 [DOI] [PubMed] [Google Scholar]
- Cheng L., Guo X. F., Yang X. Y., Chong M., Cheng J., Li G., Gui Y. H., Lu D. R. (2006). Delta-sarcoglycan is necessary for early heart and muscle development in zebrafish. Biochem. Biophys. Res. Commun. 344, 1290–1299 [DOI] [PubMed] [Google Scholar]
- Clerk A., Strong P. N., Sewry C. A. (1992). Characterisation of dystrophin during development of human skeletal muscle. Development 114, 395–402 [DOI] [PubMed] [Google Scholar]
- Côté P. D., Moukhles H., Lindenbaum M., Carbonetto S. (1999). Chimaeric mice deficient in dystroglycans develop muscular dystrophy and have disrupted myoneural synapses. Nat. Genet. 23, 338–342 [DOI] [PubMed] [Google Scholar]
- Dowling J. J., Gibbs E., Russell M., Goldman D., Minarcik J., Golden J. A., Feldman E. L. (2008). Kindlin-2 is an essential component of intercalated discs and is required for vertebrate cardiac structure and function. Circ. Res. 102, 423–431 [DOI] [PubMed] [Google Scholar]
- England S. B., Nicholson L. V., Johnson M. A., Forrest S. M., Love D. R., Zubrzycka-Gaarn E. E., Bulman D. E., Harris J. B., Davies K. E. (1990). Very mild muscular dystrophy associated with the deletion of 46% of dystrophin. Nature 343, 180–182 [DOI] [PubMed] [Google Scholar]
- Ervasti J. M., Campbell K. P. (1993). A role for the dystrophin-glycoprotein complex as a transmembrane linker between laminin and actin. J. Cell Biol. 122, 809–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etard C., Behra M., Fischer N., Hutcheson D., Geisler R., Strähle U. (2007). The UCS factor Steif/Unc-45b interacts with the heat shock protein Hsp90a during myofibrillogenesis. Dev. Biol. 308, 133–143 [DOI] [PubMed] [Google Scholar]
- Fritz J. D., Danko I., Roberds S. L., Campbell K. P., Latendresse J. S., Wolff J. A. (1995). Expression of deletion-containing dystrophins in mdx muscle: implications for gene therapy and dystrophin function. Pediatr. Res. 37, 693–700 [DOI] [PubMed] [Google Scholar]
- Gawlik K. I., Durbeej M. (2011). Skeletal muscle laminin and MDC1A: pathogenesis and treatment strategies. Skelet. Muscle 1, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey C., Foley A. R., Clement E., Muntoni F. (2011). Dystroglycanopathies: coming into focus. Curr. Opin. Genet. Dev. 21, 278–285 [DOI] [PubMed] [Google Scholar]
- Granato M., van Eeden F. J., Schach U., Trowe T., Brand M., Furutani-Seiki M., Haffter P., Hammerschmidt M., Heisenberg C. P., Jiang Y. J., et al. (1996). Genes controlling and mediating locomotion behavior of the zebrafish embryo and larva. Development 123, 399–413 [DOI] [PubMed] [Google Scholar]
- Gupta V., Kawahara G., Gundry S. R., Chen A. T., Lencer W. I., Zhou Y., Zon L. I., Kunkel L. M., Beggs A. H. (2011). The zebrafish dag1 mutant: a novel genetic model for dystroglycanopathies. Hum. Mol. Genet. 20, 1712–1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon J. R., Mosley A. N., Zhou Y., O’Brien K. F., Sheng X., Chiang K., Davidson A. J., Volinski J. M., Zon L. I., Kunkel L. M. (2003). The dystrophin associated protein complex in zebrafish. Hum. Mol. Genet. 12, 601–615 [PubMed] [Google Scholar]
- Guyon J. R., Mosley A. N., Jun S. J., Montanaro F., Steffen L. S., Zhou Y., Nigro V., Zon L. I., Kunkel L. M. (2005). Delta-sarcoglycan is required for early zebrafish muscle organization. Exp. Cell Res. 304, 105–115 [DOI] [PubMed] [Google Scholar]
- Guyon J. R., Goswami J., Jun S. J., Thorne M., Howell M., Pusack T., Kawahara G., Steffen L. S., Galdzicki M., Kunkel L. M. (2009). Genetic isolation and characterization of a splicing mutant of zebrafish dystrophin. Hum. Mol. Genet. 18, 202–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall T. E., Bryson-Richardson R. J., Berger S., Jacoby A. S., Cole N. J., Hollway G. E., Berger J., Currie P. D. (2007). The zebrafish candyfloss mutant implicates extracellular matrix adhesion failure in laminin alpha2-deficient congenital muscular dystrophy. Proc. Natl. Acad. Sci. USA 104, 7092–7097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hara Y., Balci-Hayta B., Yoshida-Moriguchi T., Kanagawa M., Beltrán-Valero de Bernabé D., Gündeşli H., Willer T., Satz J. S., Crawford R. W., Burden S. J., et al. (2011). A dystroglycan mutation associated with limb-girdle muscular dystrophy. N. Engl. J. Med. 364, 939–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins T. A., Haramis A. P., Etard C., Prodromou C., Vaughan C. K., Ashworth R., Ray S., Behra M., Holder N., Talbot W. S., et al. (2008). The ATPase-dependent chaperoning activity of Hsp90a regulates thick filament formation and integration during skeletal muscle myofibrillogenesis. Development 135, 1147–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi Y. K., Chou F. L., Engvall E., Ogawa M., Matsuda C., Hirabayashi S., Yokochi K., Ziober B. L., Kramer R. H., Kaufman S. J., et al. (1998). Mutations in the integrin alpha7 gene cause congenital myopathy. N at. Genet. 19, 94–97 [DOI] [PubMed] [Google Scholar]
- Helbling-Leclerc A., Zhang X., Topaloglu H., Cruaud C., Tesson F., Weissenbach J., Tomé F. M., Schwartz K., Fardeau M., Tryggvason K., et al. (1995). Mutations in the laminin alpha 2-chain gene (LAMA2) cause merosin-deficient congenital muscular dystrophy. Nat. Genet. 11, 216–218 [DOI] [PubMed] [Google Scholar]
- Hoffman E. P., Brown R. H., Jr, Kunkel L. M. (1987). Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell 51, 919–928 [DOI] [PubMed] [Google Scholar]
- Irwin W. A., Bergamin N., Sabatelli P., Reggiani C., Megighian A., Merlini L., Braghetta P., Columbaro M., Volpin D., Bressan G. M., et al. (2003). Mitochondrial dysfunction and apoptosis in myopathic mice with collagen VI deficiency. Nat. Genet. 35, 367–371 [DOI] [PubMed] [Google Scholar]
- Jacoby A. S., Busch-Nentwich E., Bryson-Richardson R. J., Hall T. E., Berger J., Berger S., Sonntag C., Sachs C., Geisler R., Stemple D. L., et al. (2009). The zebrafish dystrophic mutant softy maintains muscle fibre viability despite basement membrane rupture and muscle detachment. Development 136, 3367–3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jöbsis G. J., Keizers H., Vreijling J. P., de Visser M., Speer M. C., Wolterman R. A., Baas F., Bolhuis P. A. (1996). Type VI collagen mutations in Bethlem myopathy, an autosomal dominant myopathy with contractures. Nat. Genet. 14, 113–115 [DOI] [PubMed] [Google Scholar]
- Kang P. B. (2011). The struggle to model muscular dystrophy. Muscle Nerve 44, 157–159 [DOI] [PubMed] [Google Scholar]
- Kaplan J. C. (2011). The 2012 version of the gene table of monogenic neuromuscular disorders. Neuromuscul. Disord. 21, 833–861 [DOI] [PubMed] [Google Scholar]
- Kawahara G., Guyon J. R., Nakamura Y., Kunkel L. M. (2010). Zebrafish models for human FKRP muscular dystrophies. Hum. Mol. Genet. 19, 623–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawahara G., Serafini P. R., Myers J. A., Alexander M. S., Kunkel L. M. (2011a). Characterization of zebrafish dysferlin by morpholino knockdown. Biochem. Biophys. Res. Commun. 413, 358–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawahara G., Karpf J. A., Myers J. A., Alexander M. S., Guyon J. R., Kunkel L. M. (2011b). Drug screening in a zebrafish model of Duchenne muscular dystrophy. Proc. Natl. Acad. Sci. USA 108, 5331–5336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinali M., Arechavala-Gomeza V., Feng L., Cirak S., Hunt D., Adkin C., Guglieri M., Ashton E., Abbs S., Nihoyannopoulos P., et al. (2009). Local restoration of dystrophin expression with the morpholino oligomer AVI-4658 in Duchenne muscular dystrophy: a single-blind, placebo-controlled, dose-escalation, proof-of-concept study. Lancet Neurol. 8, 918–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knöll R., Postel R., Wang J., Krätzner R., Hennecke G., Vacaru A. M., Vakeel P., Schubert C., Murthy K., Rana B. K., et al. (2007). Laminin-alpha4 and integrin-linked kinase mutations cause human cardiomyopathy via simultaneous defects in cardiomyocytes and endothelial cells. Circulation 116, 515–525 [DOI] [PubMed] [Google Scholar]
- Lieschke G. J., Currie P. D. (2007). Animal models of human disease: zebrafish swim into view. Nat. Rev. Genet. 8, 353–367 [DOI] [PubMed] [Google Scholar]
- Lin Y. Y., White R. J., Torelli S., Cirak S., Muntoni F., Stemple D. L. (2011). Zebrafish Fukutin family proteins link the unfolded protein response with dystroglycanopathies. Hum. Mol. Genet. 20, 1763–1775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Aoki M., Illa I., Wu C., Fardeau M., Angelini C., Serrano C., Urtizberea J. A., Hentati F., Hamida M. B., et al. (1998). Dysferlin, a novel skeletal muscle gene, is mutated in Miyoshi myopathy and limb girdle muscular dystrophy. Nat. Genet. 20, 31–36 [DOI] [PubMed] [Google Scholar]
- Markert C. D., Ambrosio F., Call J. A., Grange R. W. (2011). Exercise and Duchenne muscular dystrophy: toward evidence-based exercise prescription. Muscle Nerve 43, 464–478 [DOI] [PubMed] [Google Scholar]
- Maselli R. A., Ng J. J., Anderson J. A., Cagney O., Arredondo J., Williams C., Wessel H. B., Abdel-Hamid H., Wollmann R. L. (2009). Mutations in LAMB2 causing a severe form of synaptic congenital myasthenic syndrome. J. Med. Genet. 46, 203–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntoni F., Wood M. J. (2011). Targeting RNA to treat neuromuscular disease. Nat. Rev. Drug Discov. 10, 621–637 [DOI] [PubMed] [Google Scholar]
- Parsons M. J., Campos I., Hirst E. M., Stemple D. L. (2002). Removal of dystroglycan causes severe muscular dystrophy in zebrafish embryos. Development 129, 3505–3512 [DOI] [PubMed] [Google Scholar]
- Pichavant C., Aartsma-Rus A., Clemens P. R., Davies K. E., Dickson G., Takeda S., Wilton S. D., Wolff J. A., Wooddell C. I., Xiao X., et al. (2011). Current status of pharmaceutical and genetic therapeutic approaches to treat DMD. Mol. Ther. 19, 830–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postel R., Vakeel P., Topczewski J., Knöll R., Bakkers J. (2008). Zebrafish integrin-linked kinase is required in skeletal muscles for strengthening the integrin-ECM adhesion complex. Dev. Biol. 318, 92–101 [DOI] [PubMed] [Google Scholar]
- Rafael J. A., Cox G. A., Corrado K., Jung D., Campbell K. P., Chamberlain J. S. (1996). Forced expression of dystrophin deletion constructs reveals structure-function correlations. J. Cell Biol. 134, 93–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roostalu U., Strähle U. (2012). In vivo imaging of molecular interactions at damaged sarcolemma. Dev. Cell 22, 515–529 [DOI] [PubMed] [Google Scholar]
- Roscioli T., Kamsteeg E. J., Buysse K., Maystadt I., van Reeuwijk J., van den Elzen C., van Beusekom E., Riemersma M., Pfundt R., Vissers L. E., et al. (2012). Mutations in ISPD cause Walker-Warburg syndrome and defective glycosylation of α-dystroglycan. Nat. Genet. 44, 581–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander J. D., Cade L., Khayter C., Reyon D., Peterson R. T., Joung J. K., Yeh J. R. (2011). Targeted gene disruption in somatic zebrafish cells using engineered TALENs. Nat. Biotechnol. 29, 697–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarparanta J., Jonson P. H., Golzio C., Sandell S., Luque H., Screen M., McDonald K., Stajich J. M., Mahjneh I., Vihola A., et al. (2012). Mutations affecting the cytoplasmic functions of the co-chaperone DNAJB6 cause limb-girdle muscular dystrophy. Nat. Genet. 44, 450–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen L. S., Guyon J. R., Vogel E. D., Beltre R., Pusack T. J., Zhou Y., Zon L. I., Kunkel L. M. (2007). Zebrafish orthologs of human muscular dystrophy genes. BMC Genomics 8, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfer W. R., Busta A. S., Bonnemann C. G., Feldman E. L., Dowling J. J. (2010). Zebrafish models of collagen VI-related myopathies. Hum. Mol. Genet. 19, 2433–2444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornhill P., Bassett D., Lochmüller H., Bushby K., Straub V. (2008). Developmental defects in a zebrafish model for muscular dystrophies associated with the loss of fukutin-related protein (FKRP). Brain 131, 1551–1561 [DOI] [PubMed] [Google Scholar]
- van Deutekom J. C., Janson A. A., Ginjaar I. B., Frankhuizen W. S., Aartsma-Rus A., Bremmer-Bout M., den Dunnen J. T., Koop K., van der Kooi A. J., Goemans N. M., et al. (2007). Local dystrophin restoration with antisense oligonucleotide PRO051. N. Engl. J. Med. 357, 2677–2686 [DOI] [PubMed] [Google Scholar]
- Welch E. M., Barton E. R., Zhuo J., Tomizawa Y., Friesen W. J., Trifillis P., Paushkin S., Patel M., Trotta C. R., Hwang S., et al. (2007). PTC124 targets genetic disorders caused by nonsense mutations. Nature 447, 87–91 [DOI] [PubMed] [Google Scholar]
- Wessels A., Ginjaar I. B., Moorman A. F., van Ommen G. J. (1991). Different localization of dystrophin in developing and adult human skeletal muscle. Muscle Nerve 14, 1–7 [DOI] [PubMed] [Google Scholar]
- Williamson R. A., Henry M. D., Daniels K. J., Hrstka R. F., Lee J. C., Sunada Y., Ibraghimov-Beskrovnaya O., Campbell K. P. (1997). Dystroglycan is essential for early embryonic development: disruption of Reichert’s membrane in Dag1-null mice. Hum. Mol. Genet. 6, 831–841 [DOI] [PubMed] [Google Scholar]
- Wohlgemuth S. L., Crawford B. D., Pilgrim D. B. (2007). The myosin co-chaperone UNC-45 is required for skeletal and cardiac muscle function in zebrafish. Dev. Biol. 303, 483–492 [DOI] [PubMed] [Google Scholar]