Abstract
Fibrodysplasia ossificans progressiva (FOP; MIM #135100) is a debilitating genetic disorder of connective tissue metamorphosis. It is characterized by malformation of the great (big) toes during embryonic skeletal development and by progressive heterotopic endochondral ossification (HEO) postnatally, which leads to the formation of a second skeleton of heterotopic bone. Individuals with these classic clinical features of FOP have the identical heterozygous activating mutation (c.617G>A; R206H) in the gene encoding ACVR1 (also known as ALK2), a bone morphogenetic protein (BMP) type I receptor. Disease activity caused by this ACVR1 mutation also depends on altered cell and tissue physiology that can be best understood in the context of a high-fidelity animal model. Recently, we developed such a knock-in mouse model for FOP (Acvr1R206H/+) that recapitulates the human disease, and provides a valuable new tool for testing and developing effective therapies. The FOP knock-in mouse and other models in Drosophila, zebrafish, chickens and mice provide an arsenal of tools for understanding BMP signaling and addressing outstanding questions of disease mechanisms that are relevant not only to FOP but also to a wide variety of disorders associated with regenerative medicine and tissue metamorphosis.
FOP: the clinical picture
Fibrodysplasia ossificans progressiva (FOP; MIM #135100) is a debilitating genetic disorder of connective tissue metamorphosis. It is characterized by malformation of the great (big) toes during embryonic skeletal development and by progressive heterotopic endochondral ossification (HEO; see Box 1 for glossary) postnatally, leading to the formation of a second skeleton of heterotopic bone. Although FOP is an extremely rare disease and the most severe form of HEO in humans, its lessons are relevant to every common, non-genetic form of HEO, such as that which occurs after soft tissue injury (Kaplan et al., 2004; Pignolo and Foley, 2005), injury to the central nervous system (van Kuijk et al., 2002), total joint replacement surgery (Neal et al., 2002) and severe war wounds (Potter et al., 2006; Forsberg et al., 2009), as well as HEO that occurs in atherosclerosis and end-stage valvular heart disease (Mohler et al., 2001). In addition, disease mechanisms revealed by FOP might be harnessed and exploited to create new skeletal elements for regenerative medicine in individuals with fracture non-unions, failed spine fusions, traumatic bone loss or congenital agenesis of skeletal elements.
Box 1. Glossary.
Aggressive fibromatosis: an aggressive tumor-like condition characterized by fibrous tissue proliferation
Alkaline phosphatase: an enzyme produced by mature bone cells and measured in the blood
Aponeuroses: large sheets of connective tissue that connect skeletal muscles
Chimeric mice: genetically engineered mice in which some of the cells are wild-type and some are mutant
Fascia: large sheets of connective tissue that separate skeletal muscles
Flare-up: an episodic activation of FOP characterized by edema (swelling), pain and decreased range of motion
Heterotopic endochondral ossification (HEO): the formation of extraskeletal bone through cartilaginous anlagen
Knock-in mice: genetically engineered mice in which a normal copy of a gene of interest is replaced with a mutated version of that gene at the endogenous genetic locus
Osteochondroma: benign endochondral neoplasms or developmental lesions that have a cartilage cap and arise from the underlying bone
Tissue metamorphosis: the postnatal transformation of one differentiated tissue (such as skeletal muscle, tendon, ligament, fascia or aponeurosis) into another (such as bone)
Transgenic mice: genetically engineered mice in which one or more copies of a mutant gene are inserted at non-homologous sites within the mouse genome.
The two defining clinical features of classic FOP are congenital malformations of the great toes and progressive heterotopic ossification in characteristic anatomical patterns (Kaplan et al., 2008a; Shore et al., 2006). Heterotopic ossification is typically seen first in the dorsal, axial, cranial and proximal regions of the body, and later in the ventral, appendicular, caudal and distal regions (Kaplan et al., 1990; Cohen et al., 1993; Rocke et al., 1994).
During the first decade of life, children with FOP develop inflammatory soft tissue swellings (known as flare-ups) that appear suddenly and expand rapidly. A flare-up is the first clinical indication of the tissue metamorphosis, which involves the catabolism of soft connective tissues (including aponeuroses, fascia, ligaments, tendons and skeletal muscles) and their replacement by extraskeletal bone through HEO (Kaplan et al., 1993a). FOP is frequently misdiagnosed, and is often mistaken for aggressive fibromatosis or various musculoskeletal tumors (Kitterman et al., 2005).
Minor trauma such as intramuscular immunizations (Lanchoney et al., 1995), mandibular blocks for dental work (Luchetti et al., 1996), muscle fatigue, blunt muscle trauma from bumps, bruises and falls (Glaser et al., 1998), or influenza-like illnesses (Scarlett et al., 2004) can trigger painful episodes of progressive HEO, suggesting that inflammation plays a crucial role in disease progression (Kaplan et al., 2005a). Trauma induced by operative removal of heterotopic bone also leads to new bone formation (Kaplan et al., 1993a; Kaplan et al., 2008a).
Although skeletal muscle is the tissue most often affected by heterotopic ossification, extraskeletal bone also forms in other connective tissues such as aponeuroses, fascia, ligaments and tendons. The diaphragm, tongue and extraocular muscles are spared from FOP. Cardiac muscle and smooth muscle are not affected (Connor and Evans, 1982).
Flare-ups of FOP are episodic; disability is cumulative. Most affected individuals develop HEO by 7 years of age, with severely restricted mobility of the spine and upper limbs by 15 years (Cohen et al., 1993; Rocke et al., 1994). Most affected individuals are confined to a wheelchair by the third decade of life, and require lifelong assistance in performing activities of daily living (Cohen et al., 1993; Rocke et al., 1994). Weight loss often follows ankylosis of the jaw. The median age of survival is 40 years (Kaplan et al., 2010a), and death often results from complications of thoracic insufficiency syndrome (Kussmaul et al., 1998; Kaplan and Glaser, 2005; Kaplan et al., 2010a).
In addition to heterotopic bone formation, individuals with FOP also exhibit malformations of the normotopic skeleton. Malformations of great toes are characteristic, whereas malformations of the thumbs are less frequent (Connor and Evans, 1982; Kaplan et al., 2005b; Kaplan et al., 2010b). Developmental anomalies are often observed in the cervical spine (Schaffer et al., 2005), and costo-vertebral and temporomandibular joints (Kaplan et al., 2010b). Spinal deformity is common (Shah et al., 1994; Moore et al., 2009). Osteochondromas are commonly observed, most notably at the proximal medial tibias (Deirmengian et al., 2008). Conductive hearing loss can occur owing to fixation of the otic ossicles (Levy et al., 1999).
Radiographic and radionuclide findings support that heterotopic bone undergoes normal modeling and remodeling (Kaplan et al., 1994; Mahboubi et al., 2001). The incidence of fractures is not increased in individuals with FOP. However, when fractures occur in heterotopic bone, the healing process is characteristically accelerated (Einhorn and Kaplan, 1994). Bone scans are abnormal before conventional radiographs can detect HEO. Computed tomography and magnetic resonance imaging of early FOP lesions have been described, but contribute little additional clinical information (Shirkhoda et al., 1995; Mahboubi et al., 2001).
Routine laboratory evaluations are usually normal in individuals with FOP, although increased serum alkaline phosphatase activity has been observed during disease activity (Lutwak, 1964; Kaplan et al., 2008a). Elevated urinary basic fibroblast growth factor levels have also been correlated with disease flare-ups (Kaplan et al., 1998).
The worldwide prevalence of FOP is approximately 1 in 2,000,000. Phenotypic variability in the timing and intensity of flare-ups is observed, without evidence of ethnic, racial, gender or geographic predisposition (Shore et al., 2005).
Reproductive fitness in FOP is low, and most cases result from spontaneous new mutations. Fewer than ten families with autosomal dominant inheritance of FOP have been reported (Shore et al., 2006). Inheritance can be from mothers or fathers (Kaplan et al., 1993b; Shore et al., 2005). Maternal mosaicism can occur (Janoff et al., 1996) and a paternal age effect has been reported (Rogers and Chase, 1979).
Environmental factors influence the phenotype of FOP. In three pairs of monozygotic twins with FOP, the congenital toe malformations were identical within each pair (Hebela et al., 2005). However, postnatal heterotopic ossification within each twin pair varied depending on life history and environmental influences such as tissue trauma and viral infections, supporting the idea that genetic factors direct the disease phenotype during prenatal development, whereas environmental factors have a major influence on postnatal progression of HEO (Hebela et al., 2005).
Histopathology of FOP lesions
Lesion formation in FOP is a pathological process of skeletal metamorphosis in which the normal structure and function of a tissue (skeletal muscle, for example) is destroyed and replaced by that of another tissue (bone). This process has been well described, and begins with a catabolic stage that is associated with muscle cell injury and death that is characterized by an inflammatory mononuclear cell infiltrate involving lymphocytes, macrophages and mast cells (Kaplan et al., 1993a; Gannon et al., 1997; Gannon et al., 1998; Gannon et al., 2001; Hegyi et al., 2003; Pignolo et al., 2005; Shore and Kaplan, 2010).
Immediately following the catabolic phase, a robust anabolic phase supervenes, which is characterized by a fibroproliferative lesion that matures through an endochondral process and culminates in the formation of a new ossicle of heterotopic bone that contains mature marrow elements (Kaplan et al., 1993a; Pignolo et al., 2005; Shore and Kaplan, 2010). As the process of tissue metamorphosis spreads through contiguous and adjacent sites with subsequent episodic flare-ups, skeletal elements ramify to form a disabling second skeleton of heterotopic bone.
Recent cell lineage tracing studies investigated the origins of the progenitor cells that participate in the various stages of bone morphogenetic protein (BMP)-induced heterotopic ossification in mouse models (Lounev et al., 2009). Despite the osteogenic response of skeletal myoblasts to BMPs in vitro, MyoD+ skeletal muscle precursors contribute minimally to heterotopic ossification (<5%) (Lounev et al., 2009). Cells of smooth muscle origin also did not contribute to the chondrogenic or osteogenic anlagen. However, cells that expressed the vascular endothelial marker Tie2 contributed to all stages of BMP-induced heterotopic ossification, constituting 40–50% of lesional cells at the fibroproliferative, chondrogenic and osteogenic stages of maturation. Importantly in FOP, cells of Tie2+ origin seem to be responsible in part for the formation of the fibroproliferative lesion (Medici et al., 2010; Wosczyna et al., 2012).
A unique FOP case study together with murine bone marrow transplantation experiments implicated the innate immune system in disease flare-ups. However, the presence of the FOP mutation in cells of the innate immune system was not required to induce a flare-up of disease activity (Kaplan et al., 2007a). Rather, normal innate immune cells were sufficient to trigger disease flare-ups in the connective tissues of a genetically susceptible chimeric host. Activation of inflammatory pathways through the innate immune system seems to be an important trigger for postnatal flare-ups of FOP (Kaplan et al., 2005a).
The ACVR R206H mutation in FOP
Individuals with classic clinical features of FOP all have the identical heterozygous activating mutation (c.617G>A; R206H) in the gene encoding ACVR1 (also known as ALK2), a BMP type I receptor. Codon 206 is highly conserved and occurs within the glycine-serine (GS) region of the cytoplasmic domain of ACVR1 (Shore et al., 2006). Phenotypic and genotypic variants of FOP (atypical FOP) have been described (Fukuda et al., 2008; Furuya et al., 2008; Kaplan et al., 2009a; Bocciardi et al., 2009; Carvalho et al., 2010; Petrie et al., 2009; Ratbi et al., 2010; Gregson et al., 2011; Whyte et al., 2012).
The ACVR1 R206H mutation is fully penetrant; all persons examined who carry this mutation have FOP. DNA sequencing of genomic DNA supports that there is no locus heterogeneity in FOP (Shore et al., 2006). All known individuals with FOP (classic or atypical) harbor heterozygous activating mutations in ACVR1 (Kaplan et al., 2009a).
Diagnosis of individuals with classic FOP can be made based on clinical evaluation alone, by associating the great toe malformations with rapid appearance of soft tissue lesions (Kaplan et al., 2008b). Clinical diagnosis of FOP can be confirmed by DNA sequence analysis of the ACVR1 gene (Kaplan et al., 2008b). DNA sequencing can also be used to evaluate suspected cases of atypical FOP or FOP variants (Kaplan et al., 2008b).
Effects of the ACVR1 R206H mutation on BMP signaling
All of the ACVR1 mutations identified in individuals with classic or atypical FOP occur in highly conserved amino acids, indicating their functional importance (Kaplan et al., 2009a). Protein structure homology modeling of the resulting ACVR1 proteins predicts that these mutant receptors are likely to activate the ACVR1 protein and enhance receptor signaling (Kaplan et al., 2009a; Groppe et al., 2007; Bocciardi et al., 2009; Petrie et al., 2009). Several articles provide excellent reviews of this crucially important signaling pathway (Huse et al., 2001; Derynck and Zhang, 2003; Shi and Massagué, 2003; Gazzerro and Canalis, 2006; Schmierer and Hill, 2007; Wu and Hill, 2009).
A series of studies demonstrated that signal transduction through the BMP pathway is altered in cells from individuals with FOP (Shafritz et al., 1996; Ahn et al., 2003; Serrano de la Peña et al., 2005; Fiori et al., 2006; Billings et al., 2008), with increased phosphorylation of BMP pathway signaling mediators (BMP-specific Smad proteins and p38MAPK) and increased expression of BMP transcriptional targets in the absence of exogenous BMP ligand. Subsequent in vitro and in vivo analyses demonstrated that BMP signaling activation can be induced by the mutant ACVR1 R206H receptor, which activates BMP signaling without the need for BMP to initiate the signaling cascade, and stimulates an additional increased pathway activation in response to BMP (Shen et al., 2009; Fukuda et al., 2009; van Dinther et al., 2010; Song et al., 2010).
Codon 206 is within the intracellular GS activation domain, adjacent to the protein kinase domain, of ACVR1. Protein homology modeling of the ACVR1 receptor predicts that the protein conformation of the ACVR1 R206H mutant is altered and could lead to changes in the ability of the receptor to interact with proteins that bind the receptor GS domain (Groppe et al., 2007; Kaplan et al., 2009a). The GS domain of all type I TGFβ/BMP superfamily receptors is a crucial site for binding and activation of the pathway-specific Smad signaling proteins. It is also a specific binding site for FKBP1A (also known as FKBP12), a highly conserved modulatory protein that prevents leaky activation of type I receptors in the absence of ligand but is released on ligand binding (Huse et al., 1999; Huse et al., 2001). Investigations support that the ACVR1 R206H protein has reduced binding to FKBP1A even in the absence of BMP (Shen et al., 2009; Song et al., 2010; van Dinther et al., 2010; Groppe et al., 2011), indicating that an impaired FKBP1A-ACVR1 interaction contributes to BMP-independent BMP pathway signaling.
Animal models of FOP
Animal models of human genetic disease are vital for validating the exact genetic cause of a condition, for understanding the cellular and molecular mechanisms of disease pathology, and for developing translational strategies to prevent disease and treat affected individuals. An ideal model for FOP would recapitulate the complete FOP phenotype, including the characteristic skeletal malformations and the progressive heterotopic bone formation through an endochondral process.
BMP implantation
Pioneering studies (Urist, 1965) led to the identification of BMPs as a family of proteins with the unique capacity to induce the entire program of endochondral bone formation. Directly introducing recombinant BMP proteins to in vivo sites was an initial approach used to develop models of heterotopic ossification (Wozney et al., 1988). The resulting HEO replicates all of the histological stages that are observed in FOP in humans (Glaser et al., 2003). HEO has also been achieved though injection of cells expressing viral constructs that overexpress BMPs (Gugala et al., 2003).
Modeling FOP in flies and fish
The evolutionarily conserved BMP signaling pathway has been studied in several highly informative animal models, including Drosophila melanogaster (Bangi and Wharton, 2006; Twombly et al., 2009; Le and Wharton, 2012) and the zebrafish, Danio rerio (Little and Mullins, 2009), providing important insight into the cellular and molecular mechanisms of BMP signaling and the activities of the ACVR1 receptor and its orthologs in vivo (Little and Mullins, 2009). BMP signaling in mammalian systems has been examined predominantly in the mouse to investigate molecular mechanisms and developmental consequences of signaling.
Transgenic mice overexpressing BMP: Nse-BMP4
Transgenic overexpression of BMPs driven through a variety of promoters has not been associated with induction of HEO. An exception is a transgenic mouse that specifically overexpresses BMP4 under control of the neuron-specific enolase (Nse) promoter. Nse-BMP4 mice exhibit FOP-like HEO following an inflammatory or neuro-inflammatory induction (Kan et al., 2004; Kan et al., 2009). Double transgenic mice overexpressing both Noggin and BMP4 under control of the Nse promoter showed full rescue of heterotopic bone formation (Kan et al., 2004).
Constitutively active ACVR1 in chick embryos and mice (ALK2Q207D)
A constitutively active form of ACVR1 has been shown in chick embryos to enhance chondrogenesis, expand cartilage elements, promote joint fusions and induce heterotopic ossification (Zhang et al., 2003). These features are similar to clinical findings in individuals with FOP and occur in response to dysregulation of the BMP signaling pathway (Shore et al., 2006; Kaplan et al., 2009b; Shore and Kaplan, 2010).
Global constitutive activation of ACVR1 in mouse models causes embryonic lethality; however, transgenic mice containing a Cre-inducible constitutively active allele (ALK2Q207D) have been developed (Fukuda et al., 2006). Whereas local Cre-induced postnatal constitutively active ACVR1 expression and BMP signaling did not yield heterotopic ossification (due to lack of an inflammatory stimulus), intramuscular injection of Cre-expressing adenovirus or Cre-expressing adenovirus and cardiotoxin to induce muscle injury and inflammation resulted in HEO and joint fusion, and caused functional impairment at the site of injection (Yu et al., 2008; Medici et al., 2010).
A knock-in mouse model of classic FOP (Acvr1R206H/+)
None of the previously described BMP implantation or transgenic mouse models fully reproduces the congenital phenotype or clinical progression of FOP. Therefore, more faithful disease models are required to understand the molecular and cellular mechanisms that direct HEO in FOP as well as to serve as in vivo systems to test potential therapies.
We recently developed an Acvr1 R206H (c.617G>A) knock-in mouse (Acvr1R206H/+). Unlike transgenic mouse models in which multiple copies of a mutant gene of interest are randomly inserted into the genome, the knock-in technology uses homologous recombination to exchange one of the two normal copies of the mouse Acvr1 gene with a copy of the mutant gene in its endogenous chromosomal location, thereby preserving the precise genetic and molecular regulation of the target gene. Although mouse germline transmission of the Acvr1 R206H mutation is perinatal lethal, mice that are 70–90% chimeric for Acvr1R206H/+ cells exhibit every clinical feature of classic FOP, including embryonic skeletal malformations and postnatal HEO through the identical progression of cellular events seen in the human condition (Chakkalakal et al., 2012).
The Acvr1R206H/+ knock-in mice show fidelity to the human disease and develop FOP, just as in humans, confirming a phenotypic specificity caused by the FOP (R206H) ACVR1 mutation (Chakkalakal et al., 2012). Acvr1R206H/+ knock-in chimeric mice showed malformations of hind limb first digits, analogous to those seen in individuals with classic FOP. Acvr1R206H/+ mice also showed the full spectrum of congenital malformations observed in individuals with FOP: fusion of subaxial cervical facet joints, costovertebral malformations, and osteochondromas of the proximal tibias and scattered other sites. Importantly, knock-in Acvr1R206H/+ mice also developed spontaneous and injury-induced FOP-like lesions that progressed into mature heterotopic endochondral bone, as in individuals with FOP (Chakkalakal et al., 2012). These mice validate the idea that the recurrent activating mutation of the BMP type I receptor ACVR1 (R206H) occurring in all individuals with classic clinical features of the disease (Shore et al., 2006) is the direct genetic cause of FOP and of all of its resulting pathology (Chakkalakal et al., 2012).
The Acvr1R206H/+ knock-in mouse model sheds light on many important questions about the cellular targets of the FOP mutation, including those that could only be addressed in viable chimeras exhibiting the classic FOP phenotype. In particular, the model confirmed findings that cells of Tie2+ origin differentiate to form mature heterotopic bone through an endochondral pathway (Lounev et al., 2009; Medici et al., 2010; Wosczyna et al., 2012). Both wild-type and mutant Tie2+ mesenchymal progenitor cells constitute much of the early anabolic fibroproliferative lesion in the chimeric mice and can differentiate into heterotopic bone. This suggests that the Acvr1R206H mutation is not required in precursor cells, and that wild-type precursor cells can receive instructive signals in a cell non-autonomous manner to guide their differentiation through an endochondral pathway (Chakkalakal et al., 2012). These findings support the physiological importance of designing preventions and treatments that target both cell autonomous and cell non-autonomous responses to BMP signaling (Chakkalakal et al., 2012).
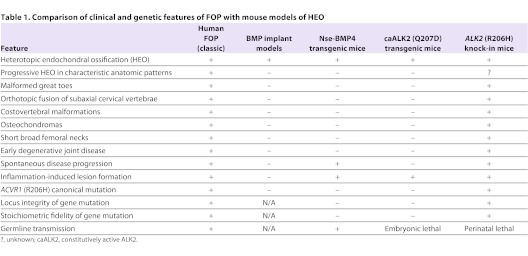
The FOP chimeric knock-in mouse model is novel among animal models in that it recapitulates of all of the features of a complex human disease with complete fidelity, and thus provides a valuable tool to address important physiological questions and therapeutic strategies that can be applied to the treatment of FOP and related disorders (Table 1) (Chakkalakal et al., 2012). Together with other models, it will be useful for addressing some of the outstanding questions regarding FOP (Box 2) and for improving treatments (see below).
Table 1.
Comparison of clinical and genetic features of FOP with mouse models of HEO
Box 2. Outstanding questions.
What are the premonitory biomarkers of FOP flare-ups?
How does the canonical ACVR1 (ALK2) mutation influence the innate immune system that has been associated with induction of flare-ups?
How does the BMP pathway drive the progression of the disease, and what other interacting pathways are involved?
What progenitor cells contribute to HEO?
What are the most effective therapies to prevent or abort FOP flare-ups?
Treatment strategies for FOP
Currently there are no effective medical treatment options to prevent the formation of heterotopic bone in FOP. Removal of heterotopic bone is avoided, because surgical trauma to tissues is likely to induce additional bone formation (Kaplan et al., 1993a; Kitterman et al., 2005; Kaplan et al., 2008a). Guidelines for symptomatic management of FOP are available on the IFOPA website (www.ifopa.org). Glucocorticoids are used to manage symptoms of flare-ups affecting major joints of the appendicular skeleton, especially when used immediately after the onset of a flare-up (Kaplan et al., 2008a). Non-steroidal anti-inflammatory agents, cyclooxygenase-2 inhibitors, mast cell stabilizers and leukotriene inhibitors are reported by patients to manage chronic pain and ongoing disease progression (Kaplan et al., 2008a).
The identification of the recurrent point mutation that causes FOP in all classically affected individuals (∼98% of all known cases of FOP) provides a specific target for drug development (Kaplan et al., 2007b). Innovative therapeutic approaches to treating FOP include:
Blocking activity of the mutant FOP receptor with soluble BMP antagonists, inhibitory RNA technology, monoclonal antibodies directed against ACVR1, or small-molecule selective signal transduction inhibitors of ACVR1 receptor activity (Glaser et al., 2003; Kaplan et al., 2007b; Yu et al., 2008; Hong and Yu, 2009; Kaplan et al., 2012)
Inhibiting the inflammatory and/or neuro-inflammatory triggers of FOP flare-ups (Kan et al., 2011; Salisbury et al., 2011)
Diverting the responding mesenchymal stromal cells to a soft tissue fate (Zasloff et al., 1998; Shimono et al., 2011; Kaplan and Shore, 2011)
Altering the inductive and/or conducive microenvironments that promote the formation of FOP lesions (Kaplan et al., 2011).
Conclusion
The discovery of the FOP gene (ACVR1) and the creation of a knock-in animal model of FOP provide important tools to unravel the pathophysiology of this disease, but many outstanding questions remain. As Thomas Maeder wrote, “FOP and its problems lie at the crossroads of several seemingly unrelated disciplines. Answers to questions that FOP poses will also address grander issues of how the body first creates its shape and then knows where to stop, how tissues decide to become what they are, and why they do not turn into something else” (Maeder, 1998).
Footnotes
COMPETING INTERESTS
The authors declare that they have no competing or financial interests.
FUNDING
This work was supported in part by the International Fibrodysplasia Ossificans Progressiva Association, the Center for Research in FOP and Related Disorders, the Ian Cali Endowment for FOP Research, the Whitney Weldon Endowment for FOP Research, the Isaac and Rose Nassau Professorship of Orthopaedic Molecular Medicine (to F.S.K.), the Cali-Weldon Research Professorship in FOP (to E.M.S.), the Rita Allen Foundation, the Penn Center for Musculoskeletal Disorders, and the National Institutes of Health (NIH R01-AR41916).
REFERENCES
- Ahn J., Serrano de la Peña L., Shore E. M., Kaplan F. S. (2003). Paresis of a bone morphogenetic protein-antagonist response in a genetic disorder of heterotopic skeletogenesis. J. Bone Joint Surg. Am. 85, 667–674 [DOI] [PubMed] [Google Scholar]
- Bangi E., Wharton K. (2006). Dual function of the Drosophila Alk1/Alk2 ortholog Saxophone shapes the Bmp activity gradient in the wing imaginal disc. Development 133, 3295–3303 [DOI] [PubMed] [Google Scholar]
- Billings P. C., Fiori J. L., Bentwood J. L., O’Connell M. P., Jiao X., Nussbaum B., Caron R. J., Shore E. M., Kaplan F. S. (2008). Dysregulated BMP signaling and enhanced osteogenic differentiation of connective tissue progenitor cells from patients with fibrodysplasia ossificans progressiva (FOP). J. Bone Miner. Res. 23, 305–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bocciardi R., Bordo D., Di Duca M., Di Rocco M., Ravazzolo R. (2009). Mutational analysis of the ACVR1 gene in Italian patients affected with fibrodysplasia ossificans progressiva: confirmations and advancements. Eur. J. Hum. Genet. 17, 311–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho D. R., Navarro M. M. M., Martins B. J., Coelho K. E., Mello W. D., Takata R. I., Speck-Martins C. E. (2010). Mutational screening of ACVR1 gene in Brazilian fibrodysplasia ossificans progressiva patients. Clin. Genet. 77, 171–176 [DOI] [PubMed] [Google Scholar]
- Chakkalakal S. A., Zhang D., Culbert A. L., Convente M. R., Caron R. J., Wright A. C., Maidment A. D. A., Kaplan F. S., Shore E. M. (2012). An Acvr1 R206H knock-in mouse has fibrodysplasia ossificans progressiva. J. Bone Miner. Res. 27, 1746–1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen R. B., Hahn G. V., Tabas J. A., Peeper J., Levitz C. L., Sando A., Sando N., Zasloff M., Kaplan F. S. (1993). The natural history of heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. A study of forty-four patients. J. Bone Joint Surg. Am. 75, 215–219 [DOI] [PubMed] [Google Scholar]
- Connor J. M., Evans D. A. (1982). Fibrodysplasia ossificans progressiva. The clinical features and natural history of 34 patients. J. Bone Joint Surg. Br. 64, 76–83 [DOI] [PubMed] [Google Scholar]
- Deirmengian G. K., Hebela N. M., O’Connell M., Glaser D. L., Shore E. M., Kaplan F. S. (2008). Proximal tibial osteochondromas in patients with fibrodysplasia ossificans progressiva. J. Bone Joint Surg. Am. 90, 366–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derynck R., Zhang Y. E. (2003). Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature 425, 577–584 [DOI] [PubMed] [Google Scholar]
- Einhorn T. A., Kaplan F. S. (1994). Traumatic fractures of heterotopic bone in patients who have fibrodysplasia ossificans progressiva. A report of 2 cases. Clin. Orthop. Relat. Res. 308, 173–177 [PubMed] [Google Scholar]
- Fiori J. L., Billings P. C., de la Peña L. S., Kaplan F. S., Shore E. M. (2006). Dysregulation of the BMP-p38 MAPK signaling pathway in cells from patients with fibrodysplasia ossificans progressiva (FOP). J. Bone Miner. Res. 21, 902–909 [DOI] [PubMed] [Google Scholar]
- Forsberg J. A., Pepek J. M., Wagner S., Wilson K., Flint J., Andersen R. C., Tadaki D., Gage F. A., Stojadinovic A., Elster E. A. (2009). Heterotopic ossification in high-energy wartime extremity injuries: prevalence and risk factors. J. Bone Joint Surg. Am. 91, 1084–1091 [DOI] [PubMed] [Google Scholar]
- Fukuda T., Scott G., Komatsu Y., Araya R., Kawano M., Ray M. K., Yamada M., Mishina Y. (2006). Generation of a mouse with conditionally activated signaling through the BMP receptor, ALK2. Genesis 44, 159–167 [DOI] [PubMed] [Google Scholar]
- Fukuda T., Kanomata K., Nojima J., Kokabu S., Akita M., Ikebuchi K., Jimi E., Komori T., Maruki Y., Matsuoka M., et al. (2008). A unique mutation of ALK2, G356D, found in a patient with fibrodysplasia ossificans progressiva is a moderately activated BMP type I receptor. Biochem. Biophys. Res. Commun. 377, 905–909 [DOI] [PubMed] [Google Scholar]
- Fukuda T., Kohda M., Kanomata K., Nojima J., Nakamura A., Kamizono J., Noguchi Y., Iwakiri K., Kondo T., Kurose J., et al. (2009). Constitutively activated ALK2 and increased SMAD1/5 cooperatively induce bone morphogenetic protein signaling in fibrodysplasia ossificans progressiva. J. Biol. Chem. 284, 7149–7156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuya H., Ikezoe K., Wang L. X., Ohyagi Y., Motomura K., Fujii N., Kira J., Fukumaki Y. (2008). A unique case of fibrodysplasia ossificans progressiva with an ACVR1 mutation, G356D, other than the common mutation (R206H). Am. J. Med. Genet. 146A459–463 [DOI] [PubMed] [Google Scholar]
- Gannon F. H., Kaplan F. S., Olmsted E., Finkel G. C., Zasloff M. A., Shore E. (1997). Bone morphogenetic protein 2/4 in early fibromatous lesions of fibrodysplasia ossificans progressiva. Hum. Pathol. 28, 339–343 [DOI] [PubMed] [Google Scholar]
- Gannon F. H., Valentine B. A., Shore E. M., Zasloff M. A., Kaplan F. S. (1998). Acute lymphocytic infiltration in an extremely early lesion of fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 346, 19–25 [PubMed] [Google Scholar]
- Gannon F. H., Glaser D., Caron R., Thompson L. D., Shore E. M., Kaplan F. S. (2001). Mast cell involvement in fibrodysplasia ossificans progressiva. Hum. Pathol. 32, 842–848 [DOI] [PubMed] [Google Scholar]
- Gazzerro E., Canalis E. (2006). Bone morphogenetic proteins and their antagonists. Rev. Endocr. Metab. Disord. 7, 51–65 [DOI] [PubMed] [Google Scholar]
- Glaser D. L., Rocke D. M., Kaplan F. S. (1998). Catastrophic falls in patients who have fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 346, 110–116 [PubMed] [Google Scholar]
- Glaser D. L., Economides A. N., Wang L., Liu X., Kimble R. D., Fandl J. P., Wilson J. M., Stahl N., Kaplan F. S., Shore E. M. (2003). In vivo somatic cell gene transfer of an engineered Noggin mutein prevents BMP4-induced heterotopic ossification. J. Bone Joint Surg. Am. 85, 2332–2342 [DOI] [PubMed] [Google Scholar]
- Gregson C. L., Hollingworth P., Williams M., Petrie K. A., Bullock A. N., Brown M. A., Tobias J. H., Triffitt J. T. (2011). A novel ACVR1 mutation in the glycine/serine-rich domain found in the most benign case of a fibrodysplasia ossificans progressiva variant reported to date. Bone 48, 654–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groppe J. C., Shore E. M., Kaplan F. S. (2007). Functional modeling of the ACVR1 (R206H) mutation in FOP. Clin. Orthop. Relat. Res. 462, 87–92 [DOI] [PubMed] [Google Scholar]
- Groppe J. C., Wu J., Shore E. M., Kaplan F. S. (2011). In vitro analyses of the dysregulated R206H ALK2 kinase-FKBP12 interaction associated with heterotopic ossification in FOP. Cells Tissues Organs 194, 291–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gugala Z., Olmsted-Davis E. A., Gannon F. H., Lindsey R. W., Davis A. R. (2003). Osteoinduction by ex vivo adenovirus-mediated BMP2 delivery is independent of cell type. Gene Ther. 10, 1289–1296 [DOI] [PubMed] [Google Scholar]
- Hebela N., Shore E. M., Kaplan F. S. (2005). Three pairs of monozygotic twins with fibrodysplasia ossificans progressiva: the role of environment in the progression of heterotopic ossification. CRBMM 3, 205–208 [Google Scholar]
- Hegyi L., Gannon F. H., Glaser D. L., Shore E. M., Kaplan F. S., Shanahan C. M. (2003). Stromal cells of fibrodysplasia ossificans progressiva lesions express smooth muscle lineage markers and the osteogenic transcription factor Runx2/Cbfa-1: clues to a vascular origin of heterotopic ossification? J. Pathol. 201, 141–148 [DOI] [PubMed] [Google Scholar]
- Hong C. C., Yu P. B. (2009). Applications of small molecule BMP inhibitors in physiology and disease. Cytokine Growth Factor Rev. 20, 409–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huse M., Chen Y. G., Massagué J., Kuriyan J. (1999). Crystal structure of the cytoplasmic domain of the type I TGF beta receptor in complex with FKBP12. Cell 96, 425–436 [DOI] [PubMed] [Google Scholar]
- Huse M., Muir T. W., Xu L., Chen Y. G., Kuriyan J., Massagué J. (2001). The TGF beta receptor activation process: an inhibitor- to substrate-binding switch. Mol. Cell 8, 671–682 [DOI] [PubMed] [Google Scholar]
- Janoff H. B., Muenke M., Johnson L. O., Rosenberg A., Shore E. M., Okereke E., Zasloff M., Kaplan F. S. (1996). Fibrodysplasia ossificans progressiva in two half-sisters: evidence for maternal mosaicism. Am. J. Med. Genet. 61, 320–324 [DOI] [PubMed] [Google Scholar]
- Kan L., Hu M., Gomes W. A., Kessler J. A. (2004). Transgenic mice overexpressing BMP4 develop a fibrodysplasia ossificans progressiva (FOP)-like phenotype. Am. J. Pathol. 165, 1107–1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan L., Liu Y., McGuire T. L., Berger D. M., Awatramani R. B., Dymecki S. M., Kessler J. A. (2009). Dysregulation of local stem/progenitor cells as a common cellular mechanism for heterotopic ossification. Stem Cells 27, 150–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan L., Lounev V. Y., Pignolo R. J., Duan L., Liu Y., Stock S. R., McGuire T. L., Lu B., Gerard N. P., Shore E. M., et al. (2011). Substance P signaling mediates BMP-dependent heterotopic ossification. J. Cell. Biochem. 112, 2759–2772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Glaser D. L. (2005). Thoracic insufficiency syndrome in patients with fibrodysplasia ossificans progressiva. CRBMM 3, 213–216 [Google Scholar]
- Kaplan F. S., Shore E. M. (2011). Derailing heterotopic ossification and RARing to go. Nat. Med. 17, 420–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Tabas J. A., Zasloff M. A. (1990). Fibrodysplasia ossificans progressiva: a clue from the fly? Calcif. Tissue Int. 47, 117–125 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., Tabas J. A., Gannon F. H., Finkel G., Hahn G. V., Zasloff M. A. (1993a). The histopathology of fibrodysplasia ossificans progressiva. An endochondral process. J. Bone Joint Surg. Am. 75, 220–230 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., McCluskey W., Hahn G., Tabas J. A., Muenke M., Zasloff M. A. (1993b). Genetic transmission of fibrodysplasia ossificans progressiva. Report of a family. J. Bone Joint Surg. Am. 75, 1214–1220 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., Strear C. M., Zasloff M. A. (1994). Radiographic and scintigraphic features of modeling and remodeling in the heterotopic skeleton of patients who have fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 304, 238–247 [PubMed] [Google Scholar]
- Kaplan F., Sawyer J., Connors S., Keough K., Shore E., Gannon F., Glaser D., Rocke D., Zasloff M., Folkman J. (1998). Urinary basic fibroblast growth factor. A biochemical marker for preosseous fibroproliferative lesions in patients with fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 346, 59–65 [PubMed] [Google Scholar]
- Kaplan F. S., Glaser D. L., Hebela N., Shore E. M. (2004). Heterotopic ossification. J. Am. Acad. Orthop. Surg. 12, 116–125 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., Shore E. M., Gupta R., Billings P. C., Glaser D. L., Pignolo R. J., Graf D., Kamoun M. (2005a). Immunological features of fibrodysplasia ossificans progressiva and the dysregulated BMP4 pathway. CRBMM 3, 189–194 [Google Scholar]
- Kaplan F. S., Glaser D. L., Shore E. M., Deirmengian G. K., Gupta R., Delai P., Morhart R., Smith R., Le Merrer M., Rogers J. G., et al. (2005b). The phenotype of fibrodysplasia ossificans progressiva. CRBMM 3, 183–188 [Google Scholar]
- Kaplan F. S., Glaser D. L., Shore E. M., Pignolo R. J., Xu M., Zhang Y., Senitzer D., Forman S. J., Emerson S. G. (2007a). Hematopoietic stem-cell contribution to ectopic skeletogenesis. J. Bone Joint Surg. Am. 89, 347–357 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., Glaser D. L., Pignolo R. J., Shore E. M. (2007b). A new era for fibrodysplasia ossificans progressiva: a druggable target for the second skeleton. Expert Opin. Biol. Ther. 7, 705–712 [DOI] [PubMed] [Google Scholar]
- Kaplan F. S., Le Merrer M., Glaser D. L., Pignolo R. J., Goldsby R. E., Kitterman J. A., Groppe J., Shore E. M. (2008a). Fibrodysplasia ossificans progressiva. Best Pract. Res. Clin. Rheumatol. 22, 191–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Xu M., Glaser D. L., Collins F., Connor M., Kitterman J., Sillence D., Zackai E., Ravitsky V., Zasloff M., et al. (2008b). Early diagnosis of fibrodysplasia ossificans progressiva. Pediatrics 121, e1295–e1300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Xu M., Seemann P., Connor J. M., Glaser D. L., Carroll L., Delai P., Fastnacht-Urban E., Forman S. J., Gillessen-Kaesbach G., et al. (2009a). Classic and atypical fibrodysplasia ossificans progressiva (FOP) phenotypes are caused by mutations in the bone morphogenetic protein (BMP) type I receptor ACVR1. Hum. Mutat. 30, 379–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Pignolo R. J., Shore E. M. (2009b). The FOP metamorphogene encodes a novel type I receptor that dysregulates BMP signaling. Cytokine Growth Factor Rev. 20, 399–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Zasloff M. A., Kitterman J. A., Shore E. M., Hong C. C., Rocke D. M. (2010a). Early mortality and cardiorespiratory failure in patients with fibrodysplasia ossificans progressiva. J. Bone Joint Surg. Am. 92, 686–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F. S., Groppe J. C., Seemann P., Pignolo R. J., Shore E. M. (2010b). Fibrodysplasia ossificans progressiva: developmental implications of a novel metamorphogene. In Bone and Development (ed. Bronner F., Farach-Carson M. C., Roach H. I.). London, UK: Springer-Verlag [Google Scholar]
- Kaplan F. S., Lounev V. Y., Wang H., Pignolo R. J., Shore E. M. (2011). Fibrodysplasia ossificans progressiva: a blueprint for metamorphosis. Ann. N. Y. Acad. Sci. 1237, 5–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan J., Kaplan F. S., Shore E. M. (2012). Restoration of normal BMP signaling levels and osteogenic differentiation in FOP mesenchymal progenitor cells by mutant allele-specific targeting. Gene Ther. 19, 786–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitterman J. A., Kantanie S., Rocke D. M., Kaplan F. S. (2005). Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 116, e654–e661 [DOI] [PubMed] [Google Scholar]
- Kussmaul W. G., Esmail A. N., Sagar Y., Ross J., Gregory S., Kaplan F. S. (1998). Pulmonary and cardiac function in advanced fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 346, 104–109 [PubMed] [Google Scholar]
- Lanchoney T. F., Cohen R. B., Rocke D. M., Zasloff M. A., Kaplan F. S. (1995). Permanent heterotopic ossification at the injection site after diphtheria-tetanus-pertussis immunizations in children who have fibrodysplasia ossificans progressiva. J. Pediatr. 126, 762–764 [DOI] [PubMed] [Google Scholar]
- Le V. Q., Wharton K. A. (2012). Hyperactive BMP signaling induced by ALK2(R206H) requires type II receptor function in a Drosophila model for classic fibrodysplasia ossificans progressiva. Dev. Dyn. 241, 200–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy C. E., Lash A. T., Janoff H. B., Kaplan F. S. (1999). Conductive hearing loss in individuals with fibrodysplasia ossificans progressiva. Am. J. Audiol. 8, 29–33 [DOI] [PubMed] [Google Scholar]
- Little S. C., Mullins M. C. (2009). Bone morphogenetic protein heterodimers assemble heteromeric type I receptor complexes to pattern the dorsoventral axis. Nat. Cell Biol. 11, 637–643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lounev V. Y., Ramachandran R., Wosczyna M. N., Yamamoto M., Maidment A. D., Shore E. M., Glaser D. L., Goldhamer D. J., Kaplan F. S. (2009). Identification of progenitor cells that contribute to heterotopic skeletogenesis. J. Bone Joint Surg. Am. 91, 652–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti W., Cohen R. B., Hahn G. V., Rocke D. M., Helpin M., Zasloff M., Kaplan F. S. (1996). Severe restriction in jaw movement after routine injection of local anesthetic in patients who have fibrodysplasia ossificans progressiva. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 81, 21–25 [DOI] [PubMed] [Google Scholar]
- Lutwak L. (1964). Myositis ossificans progressiva: mineral, metabolic, and radioactive calcium studies of the effects of hormones. Am. J. Med. 37, 269–293 [DOI] [PubMed] [Google Scholar]
- Maeder T. (1998). A few hundred people turned to bone. The Atlantic Monthly 281, 81–89 [Google Scholar]
- Mahboubi S., Glaser D. L., Shore E. M., Kaplan F. S. (2001). Fibrodysplasia ossificans progressiva. Pediatr. Radiol. 31, 307–314 [DOI] [PubMed] [Google Scholar]
- Medici D., Shore E. M., Lounev V. Y., Kaplan F. S., Kalluri R., Olsen B. R. (2010). Conversion of vascular endothelial cells into multipotent stem-like cells. Nat. Med. 16, 1400–1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler E. R., 3rd, Gannon F., Reynolds C., Zimmerman R., Keane M. G., Kaplan F. S. (2001). Bone formation and inflammation in cardiac valves. Circulation 103, 1522–1528 [DOI] [PubMed] [Google Scholar]
- Moore R. E., Dormans J. P., Drummond D. S., Shore E. M., Kaplan F. S., Auerbach J. D. (2009). Chin-on-chest deformity in patients with fibrodysplasia ossificans progressiva. A case series. J. Bone Joint Surg. Am. 91, 1497–1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal B., Gray H., MacMahon S., Dunn L. (2002). Incidence of heterotopic bone formation after major hip surgery. ANZ J. Surg. 72, 808–821 [DOI] [PubMed] [Google Scholar]
- Petrie K. A., Lee W. H., Bullock A. N., Pointon J. J., Smith R., Russell R. G., Brown M. A., Wordsworth B. P., Triffitt J. T. (2009). Novel mutations in ACVR1 result in atypical features in two fibrodysplasia ossificans progressiva patients. PLoS ONE 4, e5005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignolo R. J., Foley K. L. (2005). Nonhereditary heterotopic ossification. CRBMM 3, 261–266 [Google Scholar]
- Pignolo R. J., Suda R. K., Kaplan F. S. (2005). The fibrodysplasia ossificans progressiva lesion. CRBMM 3, 195–200 [Google Scholar]
- Potter B. K., Burns T. C., Lacap A. P., Granville R. R., Gajewski D. (2006). Heterotopic ossification in the residual limbs of traumatic and combat-related amputees. J. Am. Acad. Orthop. Surg. 14, S191–S197 [DOI] [PubMed] [Google Scholar]
- Ratbi I., Borcciadi R., Regragui A., Ravazzolo R., Sefiani A. (2010). Rarely occurring mutation of ACVR1 gene in Moroccan patient with fibrodysplasia ossificans progressiva. Clin. Rheumatol. 29, 119–121 [DOI] [PubMed] [Google Scholar]
- Rocke D. M., Zasloff M., Peeper J., Cohen R. B., Kaplan F. S. (1994). Age- and joint-specific risk of initial heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 301, 243–248 [PubMed] [Google Scholar]
- Rogers J. G., Chase G. A. (1979). Paternal age effect in fibrodysplasia ossificans progressiva. J. Med. Genet. 16, 147–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury E., Rodenberg E., Sonnet C., Hipp J., Gannon F. H., Vadakkan T. J., Dickinson M. E., Olmsted-Davis E. A., Davis A. R. (2011). Sensory nerve induced inflammation contributes to heterotopic ossification. J. Cell. Biochem. 112, 2748–2758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarlett R. F., Rocke D. M., Kantanie S., Patel J. B., Shore E. M., Kaplan F. S. (2004). Influenza-like viral illnesses and flare-ups of fibrodysplasia ossificans progressiva. Clin. Orthop. Relat. Res. 423, 275–279 [DOI] [PubMed] [Google Scholar]
- Schaffer A. A., Kaplan F. S., Tracy M. R., O’Brien M. L., Dormans J. P., Shore E. M., Harland R. M., Kusumi K. (2005). Developmental anomalies of the cervical spine in patients with fibrodysplasia ossificans progressiva are distinctly different from those in patients with Klippel-Feil syndrome: clues from the BMP signaling pathway. Spine 30, 1379–1385 [DOI] [PubMed] [Google Scholar]
- Schmierer B., Hill C. S. (2007). TGF-beta-SMAD signal transduction: molecular specificity and functional flexibility. Nat. Rev. Mol. Cell Biol. 8, 970–982 [DOI] [PubMed] [Google Scholar]
- Serrano de la Peña L., Billings P. C., Fiori J. L., Ahn J., Kaplan F. S., Shore E. M. (2005). Fibrodysplasia ossificans progressiva (FOP), a disorder of ectopic osteogenesis, misregulates cell surface expression and trafficking of BMPRIA. J. Bone Miner. Res. 20, 1168–1176 [DOI] [PubMed] [Google Scholar]
- Shafritz A. B., Shore E. M., Gannon F. H., Zasloff M. A., Taub R., Muenke M., Kaplan F. S. (1996). Overexpression of an osteogenic morphogen in fibrodysplasia ossificans progressiva. N. Engl. J. Med. 335, 555–561 [DOI] [PubMed] [Google Scholar]
- Shah P. B., Zasloff M. A., Drummond D., Kaplan F. S. (1994). Spinal deformity in patients who have fibrodysplasia ossificans progressiva. J. Bone Joint Surg. Am. 76, 1442–1450 [DOI] [PubMed] [Google Scholar]
- Shen Q., Little S. C., Xu M., Haupt J., Ast C., Katagiri T., Mundlos S., Seemann P., Kaplan F. S., Mullins M. C., et al. (2009). The fibrodysplasia ossificans progressiva R206H ACVR1 mutation activates BMP-independent chondrogenesis and zebrafish embryo ventralization. J. Clin. Invest. 119, 3462–3472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Massagué J. (2003). Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell 113, 685–700 [DOI] [PubMed] [Google Scholar]
- Shimono K., Tung W. E., Macolino C., Chi A. H.-T., Didizian J. H., Mundy C., Chandraratna R. A., Mishina Y., Enomoto-Iwamoto M., Pacifici M., et al. (2011). Potent inhibition of heterotopic ossification by nuclear retinoic acid receptor-γ agonists. Nat. Med. 17, 454–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirkhoda A., Armin A.-R., Bis K. G., Makris J., Irwin R. B., Shetty A. N. (1995). MR imaging of myositis ossificans: variable patterns at different stages. J. Magn. Reson. Imaging 5, 287–292 [DOI] [PubMed] [Google Scholar]
- Shore E. M., Kaplan F. S. (2010). Inherited human diseases of heterotopic bone formation. Nat. Rev. Rheumatol. 6, 518–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore E. M., Feldman G. J., Xu M., Kaplan F. S. (2005). The genetics of fibrodysplasia ossificans progressiva. CRBMM 3, 201–204 [Google Scholar]
- Shore E. M., Xu M., Feldman G. J., Fenstermacher D. A., Cho T.-J., Choi I. H., Connor J. M., Delai P., Glaser D. L., LeMerrer M., et al. (2006). A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat. Genet. 38, 525–527 [DOI] [PubMed] [Google Scholar]
- Song G. A., Kim H. J., Woo K. M., Baek J. H., Kim G. S., Choi J. Y., Ryoo H. M. (2010). Molecular consequences of the ACVR1(R206H) mutation of fibrodysplasia ossificans progressiva. J. Biol. Chem. 285, 22542–22553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twombly V., Bangi E., Le V., Malnic B., Singer M. A., Wharton K. A. (2009). Functional analysis of saxophone, the Drosophila gene encoding the BMP type I receptor ortholog of human ALK1/ACVRL1 and ACVR1/ALK2. Genetics 183, 563–579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urist M. R. (1965). Bone: formation by autoinduction. Science 150, 893–899 [DOI] [PubMed] [Google Scholar]
- van Dinther M., Visser N., de Gorter D. J., Doorn J., Goumans M. J., de Boer J, ten Dijke P. (2010). ALK2 R206H mutation linked to fibrodysplasia ossificans progressiva confers constitutive activity to the BMP type I receptor and sensitizes mesenchymal cells to BMP-induced osteoblast differentiation and bone formation. J. Bone Miner. Res. 25, 1208–1215 [DOI] [PubMed] [Google Scholar]
- van Kuijk A. A., Geurts A. C. H., van Kuppevelt H. J. M. (2002). Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord 40, 313–326 [DOI] [PubMed] [Google Scholar]
- Whyte M. P., Wenkert D., Demertzis J. L., DiCarlo E. F., Westenberg E., Mumm S. (2012). Fibrodysplasia ossificans progressiva: middle-age onset of heterotopic ossification from a unique missense mutation (c.974G>C, p.G325A) in ACVR1. J. Bone Miner. Res. 27, 729–737 [DOI] [PubMed] [Google Scholar]
- Wosczyna M. N., Biswas A. A., Cogswell C. A., Goldhamer D. J. (2012). Multipotent progenitors resident in the skeletal muscle interstitium exhibit robust BMP-dependent osteogenic activity and mediate heterotopic ossification. J. Bone Miner. Res. 27, 1004–1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wozney J. M., Rosen V., Celeste A. J., Mitsock L. M., Whitters M. J., Kriz R. W., Hewick R. M., Wang E. A. (1988). Novel regulators of bone formation: molecular clones and activities. Science 242, 1528–1534 [DOI] [PubMed] [Google Scholar]
- Wu M. Y., Hill C. S. (2009). Tgf-beta superfamily signaling in embryonic development and homeostasis. Dev. Cell 16, 329–343 [DOI] [PubMed] [Google Scholar]
- Yu P. B., Deng D. Y., Lai C. S., Hong C. C., Cuny G. D., Bouxsein M. L., Hong D. W., McManus P. M., Katagiri T., Sachidanandan C., et al. (2008). BMP type I receptor inhibition reduces heterotopic [corrected] ossification. Nat. Med. 14, 1363–1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zasloff M. A., Rocke D. M., Crofford L. J., Hahn G. V., Kaplan F. S. (1998). Treatment of patients who have fibrodysplasia ossificans progressiva with isotretinoin. Clin. Orthop. Relat. Res. 346, 121–129 [PubMed] [Google Scholar]
- Zhang D., Schwarz E. M., Rosier R. N., Zuscik M. J., Puzas J. E., O’Keefe R. J. (2003). ALK2 functions as a BMP type I receptor and induces Indian hedgehog in chondrocytes during skeletal development. J. Bone Miner. Res. 18, 1593–1604 [DOI] [PubMed] [Google Scholar]