ABSTRACT
Purpose: To describe the characteristics of participants in a physiotherapist spinal triage programme, compare the profiles of patients for whom surgery was and was not recommended by a surgeon, and determine the surgical yield among those referred to surgeons. Methods: Data were collected retrospectively by reviewing charts of people who used the service over a 3-year period (2003–2006). Data from up to1,096 people were used in the analysis; complete data were available for 299 people. Descriptive statistics were used to summarize demographics, clinical features, and management recommendations. Characteristics of those who were and were not recommended for surgery were examined using Pearson's chi-square or Fisher's Exact tests. Results: The majority of 746 participants were classified as “mechanical spine” (92.5%), 2.9% were “other body part,” 2.5% were “medical/other,” and only 2% were classified as “surgical spine.” Recommendations for surgery (by a surgeon) were independent of patients' age, sex, duration of symptoms, residence (urban/rural), source of health care funding, and diagnosis. The surgical yield was 80%. Conclusions: Most people were not considered candidates for surgery. Triage assessment by physiotherapists can increase the efficiency of an orthopaedic surgeon's caseload by reducing the number of non-surgical referrals and can thus help to ensure more timely access to appropriate health care.
Key Words: collaborative practice, diagnosis, advanced practice, low back pain, spinal triage programme
RÉSUMÉ
Objectif : Décrire les caractéristiques des participants à un programme de triage en fonction de leurs problèmes à la colonne vertébrale, comparer les profils des patients pour qui une chirurgie était ou non recommandée et déterminer l'étendue de la chirurgie parmi les personnes dirigées vers un professionnel de la chirurgie. Méthode : Les données ont été recueillies rétrospectivement en procédant à un examen des dossiers de personnes qui ont utilisé le service pendant trois ans (de 2003 à 2006). Des données relatives à 1 096 personnes étaient disponibles et des données complètes étaient disponibles pour 299 personnes. Des statistiques descriptives ont été utilisées pour résumer les données démographiques, les caractéristiques cliniques et les recommandations de gestion. Les caractéristiques des personnes ayant ou non fait l'objet d'une recommandation pour une chirurgie ont été examinées à l'aide du test du Khi-carré de Pearson et du test de Fisher. Résultats : La majorité des 746 participants ont été classés comme « mécanique vertébrale » (92,5 %); 2,9 % comme « autres parties du corps »; 2,5 % l'ont été dans « médical/autres » et 2 % ont été classés comme « vertébral chirurgical ». Les recommandations pour une intervention (par un chirurgien) étaient formulées indépendamment de l'âge des patients, de leur sexe, de la durée des symptômes, de leur milieu (urbain ou rural), de la source de financement des soins de santé dans leur cas et du diagnostic posé. L'étendue de la chirurgie était de 80 %. Conclusions : La plupart des personnes n'étaient pas considérées comme des candidats pour une chirurgie. L'évaluation du triage par des physiothérapeutes peut accroître l'efficacité du travail du chirurgien orthopédique en réduisant le nombre de renvois en consultation de personnes qui n'ont pas besoin d'une chirurgie et favoriser par le fait même un accès en temps opportun aux soins de santé appropriés.
Mots clés : champ de pratique étendu, colonne vertébrale, diagnostic, lombalgie, pratique en collaboration, triage des patients
Access to health services is a key component of quality health care. Wait time has been identified by Canadians as an important measure of access and is cited as the most prominent barrier by those who experience difficulties in obtaining care.1,2 People waiting for health care may also experience adverse effects such as reduced function, decreased health-related quality of life, and psychological distress.1,3–5 Furthermore, living with uncertainty about diagnosis, prognosis, and further management may create or perpetuate patient concerns.6
Although wait times for surgery and other procedures can be lengthy, they are only one of several waiting periods across the continuum of care.7 Long wait times for elective orthopaedic surgery have been and continue to be a problem in Canada.8 Waits that occur earlier in the delivery of health care, however—such as waiting for a specialist consultation after referral from a general practitioner (GP)—can account for a significant proportion of overall waiting time: an estimated 40% of total time spent waiting is attributed to waiting for either a specialist appointment or appropriate diagnostic tests.8 Because of considerable variation in what data are collected and how, there are no peer-reviewed pan-Canadian reports on this earlier wait-time segment (e.g., time spent waiting to see a specialist).8 However, a recent report by the Fraser Institute showed that of 12 medical specialties examined, orthopaedic surgery had the second longest median wait from GP referral to specialist appointment (17.1 weeks) and the longest median wait from specialist to treatment (18.5 weeks).9 This indicates a need for innovative approaches to managing and reducing orthopaedic wait times.
Low back pain (LBP) and related disorders are significant population-health problems10–12 that consume considerable health care resources.13–15 For a primary health care provider assessing people presenting with LBP and lower-quadrant symptoms, one of the most important goals is to differentiate between the small number of serious pathologies and the majority of benign conditions. Although LBP is a common presenting symptom of many potentially serious spinal problems, only a small proportion of those presenting with spinal pain have a serious pathology. It is estimated that only 1% of people with LBP have serious spinal pathology (e.g., tumours, infections, inflammatory conditions) requiring urgent specialist investigation and treatment; less than 5% of people with LBP are estimated to have true nerve root pain arising from a disc prolapse, spinal stenosis, or surgical scarring, and only a small proportion of these will require surgical intervention. The remaining 95% of people who present with back pain can be classified as having “non-specific” or mechanical LBP.16,17 To further complicate the clinical picture, the symptoms of other types of pathologies—musculoskeletal (e.g., hip osteoarthritis), neurological (e.g., multiple sclerosis), medical (e.g., cancer), or systemic (e.g., ankylosing spondylitis)—may mimic lumbar-spine-related pathology.18,19
Despite the low total proportion of cases with serious spine pathology or other problems that may be amenable to surgery, people with LBP continue to represent a very large proportion of referrals to orthopaedic surgeons20,21 Surgeons specialize in investigating and treating serious pathology or nerve root problems that fail to resolve; their services are therefore inappropriate for patients with non-specific or mechanical LBP.22,23 Many people referred to surgeons are not considered surgical candidates24,25 and may simply need reassurance that they do not have serious spine pathology.16,22 Reports from a range of settings and patient populations show that no more than 30% of patients who see an orthopaedic surgeon are candidates for surgery.25–28 The large proportion of non-surgical candidates who are referred to surgeons can contribute significantly to wait times for surgical consultation and, ultimately, to longer wait times for other orthopaedic surgical procedures, such as hip and knee joint replacements. Reducing the number of non-surgical consultations in a surgeon's caseload, therefore, may help reduce wait times for patients who may benefit from spinal surgery, as well as redirecting non-surgical candidates for more appropriate treatment earlier. Collaboration between primary health care providers with expertise in assessing and evaluating musculoskeletal disorders and orthopaedic surgeons is one way to approach this problem.
Models in which non-surgical specialists or other health care professionals collaborate with orthopaedic surgeons to provide care to people with musculoskeletal problems are increasingly being reported in the literature.6,29–31 Physiotherapists with advanced orthopaedic training, often practising with a maximized or extended scope, have been shown to be as effective as orthopaedic surgeons in the diagnosis and non-surgical management of many musculoskeletal conditions.29,32–36 Physiotherapists performing this role have also contributed to reduced wait times and improved referral practices;29,37 data from the United Kingdom indicate that when physiotherapists pre-screened patients, the proportion of “appropriate” referrals—patients assessed by the surgeon as requiring surgery—more than doubled.26 In this type of “triage” role,38 physiotherapists screen patients to determine what type of management is appropriate: conservative intervention, referral to a surgeon, and/or diagnostic investigations. Evaluative research examining these types of programmes is sparse, however, and, the few programmes studied focus on general musculoskeletal practices29,39,40 or hip and knee joint arthritis management only.31,41,42 Few physiotherapist-delivered triage services that focus solely on spinal conditions have been described or evaluated in the literature.37,43
The primary purpose of the present study, therefore, was to describe the demographics, clinical features, and recommended management pathways of participants from the first 3 years (October 2003–October 2006) of a spinal triage assessment service delivered by physiotherapists (Objective 1). We also sought to explore which of these variables were associated with an outcome of having surgery performed, recommended, or deferred (Objective 2) and to determine the surgical yield among people referred to surgeons (Objective 3).
METHODS
Background: Description of the Wall Street Spinal Assessment Service
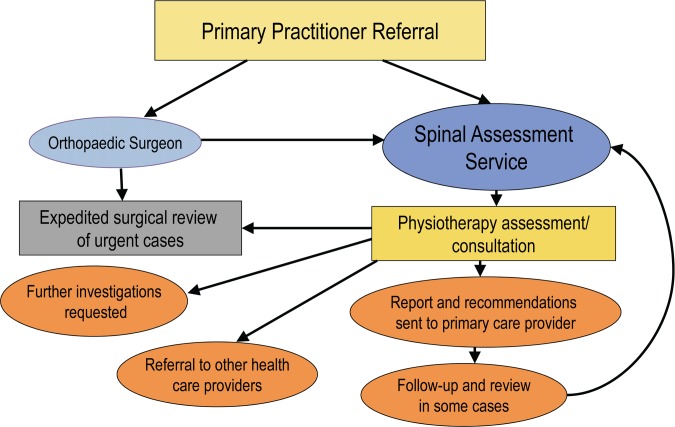
The Wall Street Spinal Assessment Service (WSSAS) is a collaborative effort between a group of three orthopaedic surgeons and four physiotherapists from a private rehabilitation clinic. The programme was initiated to address the problem of excessive referrals to the orthopaedic surgeons of patients with low-back-related conditions, the majority of whom did not require surgery. Before the programme was initiated, the surgeons had expressed frustration at how long people waited to see them (often more than a year) and the high proportion of non-surgical referrals in their caseloads. The surgeon group already had an extensive working relationship with physiotherapists from the rehabilitation clinic, and therefore approached this clinic for with their wait list backlog and to screen subsequent new referrals for primarily low-back-related conditions. Figure 1 shows the WSSAS referral and clinical pathways. People can be referred directly to the service by their primary care provider or through a WSSAS surgeon. At present, anyone referred to the orthopaedic surgeons for spine problems is automatically rerouted to the physiotherapists for screening.
Figure 1.
Description of the Wall Street Spinal Assessment Service referral, assessment, and clinical pathways.
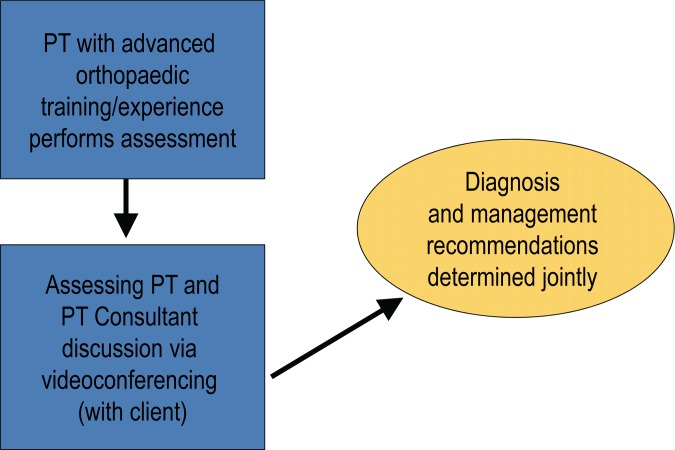
With the client present, the assessing physiotherapist discusses the findings of each assessment with the physiotherapy consultant via videoconferencing (see Figure 2). The clinical diagnosis and recommendations are determined jointly through a collaborative reasoning approach,44 with input from the client. A detailed report outlining the assessment findings, diagnosis, management recommendations, and any recommended further diagnostic tests is then sent to the referring health care provider and any other health care providers involved, including the surgeons if necessary. All physiotherapists involved in the WSSAS have completed advanced orthopaedic training in the Canadian Orthopaedic Syllabus; their experience ranges from 5 to 30 years. Through medical directives, the consultant physiotherapist can refer patients directly to the surgeon and/or order advanced imaging.
Figure 2.
Wall Street Spinal Assessment Service assessment process.
Study design
Our study uses an ex post facto observational design.45 Data were collected retrospectively via chart reviews of people who used the service over a 3-year period (October 2003–October 2006). A total of 1,219 people used the service during this period, but demographic and clinical data of interest were available and collected only for subsets of participants (ranging in number from 448 to 1,162) because certain variables were not recorded (and may not have been known) at the time of assessment. The information was initially collected and collated by employees of the clinic as part of a retrospective quality-assurance chart audit over approximately 6 months (August 2007–February 2008).
Measures
Box 1 describes the variables examined in this study. Demographics (age, sex,), clinical features (symptom duration, diagnostic category), management recommendations, and other factors (e.g., funding source, postal code/residence) were extracted from the initial client intake and assessment forms. The outcome variable “surgical management”—meaning that the patient had undergone surgery (either spine or hip/knee joint replacement) at some point after the initial assessment, was waiting for surgery, or had deferred surgery recommended by a surgeon—was ascertained from a review of other reports and documents in the chart (e.g., surgical reports, surgeon letters, follow-up physiotherapy reports). Data on this variable were collected anywhere between 9 and 52 months after the participant's initial assessment by WSSAS.
Box 1.
Description of Study Variables
| Variable | Units/Categories | Description (if applicable) |
|---|---|---|
| Age | Years | N/A |
| Symptom duration | Months | Self-reported duration of symptoms |
| Sex | Male/Female | N/A |
| Residence | Urban | Second digit of postal code≠0 (i.e., living in a town or city with ≥10,000 residents)46 |
| Rural | Second digit of postal code=046 | |
| Funding | Direct bill | Self-paying client |
| WCB | N/A | |
| Unable to pay | Assessment fee waived | |
| Other insurance | Third-party payer other than WCB | |
| Diagnosis | Surgical spine | Discogenic, stenotic, and medical |
| Mechanical spine | Degenerative and non-degenerative | |
| Other body part | Mechanical or degenerative other body part (i.e., hip or knee osteoarthritis) | |
| Medical/other | Other medical problem (e.g., systemic arthritis, tumour) | |
| Management recommendations | Referral to surgeon | Referral to a WSSAS surgeon |
| Referral to another medical specialist | Referral to medical specialist outside of WSSAS | |
| PT treatment | PT treatment (manual therapy, exercise instruction, education, and other modalities as needed) | |
| PT treatment+surgical referral | PT treatment followed by review by surgeon | |
| Exercise programme | Exercise programme only | |
| Nothing | No further treatment recommended | |
| Surgical management (outcome) | Surgery performed, recommended, or pending | Orthopaedic surgery (i.e., spine; hip or knee replacement) completed, on wait list for surgery, or surgery recommended by surgeon but deferred by patient |
| No surgery | Did not have orthopaedic surgery completed or recommended at the follow-up time point |
WCB=Workers' Compensation Board; WSSAS=Wall Street Spinal Assessment Service; PT=physiotherapy.
The study received ethical approval from the University of Saskatchewan's Biomedical Ethics Board on 15 March 2010; a de-identified Excel spreadsheet of the variables was then forwarded to the primary investigator (BB) for data analysis.
Analysis
Descriptive statistics were calculated on the demographics, clinical features, and clinical pathways of programme participants. The Shapiro–Wilk test was used to assess the distribution of each continuous variable (i.e., age and symptom duration). Because these variables were not normally distributed, we report the median and interquartile ranges (IQRs). Age and symptom duration were recoded into categorical variables based on median value and clinical relevance, respectively.
Categorical variables with more than two levels (funding, management recommendations, diagnosis) were dichotomized (as described in Tables 1–3) to enhance interpretation. Differences in characteristics between participants who had a surgical management outcome and those who did not were examined using Pearson's chi-square test or, for cell counts <5, Fisher's Exact test.47 This analysis was carried out for a reduced sample of people for whom we had complete data for each of the variables of interest (n=299) and for the total sample for each variable (ns=336–672). Because the outcome variable of interest for Objective 2 (i.e., having surgery performed, recommended, or deferred) included both spine and joint-replacement surgery, we examined the diagnostic categories of surgical spine and other body part for significance, both separately and as a combined variable. The proportion of people referred to the surgeon who had a management outcome of surgery was calculated to obtain estimates of the surgical yield for the full and reduced samples (Objective 3). The alpha level was set at 0.05, and all tests of significance were two-tailed. Statistical analysis was done using PASW (Predictive Analytics SoftWare) Statistics Mac version 18.0 (SPSS Inc., Chicago).
Table 1.
Description of Variables: Total Sample
| Variable | Description | No. (%) of patients | n* |
|---|---|---|---|
| Age | >50 y | 563 (51.4) | 1,096 |
| Symptom duration | >6 mo | 277 (58.9) | 470 |
| Sex | Female | 604 (52.0) | 1,162 |
| Residence | Rural | 739 (64.7) | 1,143 |
| Funding | Direct bill | 384 (85.7) | 448 |
| WCB | 25 (5.6) | 448 | |
| Unable to pay | 23 (5.1) | 448 | |
| Other insurance | 16 (3.6) | 448 | |
| Diagnosis | Surgical spine | 15 (2.0) | 746 |
| Mechanical spine | 690 (92.5) | 746 | |
| Other body part | 22 (2.9) | 746 | |
| Medical/other | 19 (2.5) | 746 | |
| Management recommendations | Referral to surgeon | 98 (12.2) | 802 |
| Referral to another specialist | 21 (2.6) | 802 | |
| PT treatment | 593 (73.9) | 802 | |
| PT treatment+surgical referral | 36 (4.5) | 802 | |
| Exercise programme | 4 (0.5) | 802 | |
| No further follow-up | 50 (6.2) | 802 | |
| Management recommendations (dichotomized) | Referral to surgeon (any)† | 134 (16.7) | 802 |
| Surgical management | Surgery performed, recommended, or pending | 30 (4.4) | 677 |
Each variable has a different n, for a variety of reasons (variable may not have been known at the time of the assessment, or the data may not have been recorded at the time of the assessment).
Combination of categories (1) and (4) from Management Recommendations in Box 1.
WCB=Worker's Compensation Board; PT=physiotherapy.
Table 3.
Characteristics of Participants Who Did and Did Not Have Surgery* Performed, Pending, or Deferred: Reduced Sample† (n=299)
| Surgical status; no./total (%) of patients |
||||
|---|---|---|---|---|
| Characteristic | Surgery | No surgery | p-value | |
| Age | >50 y‡ | 4/10 (40.0) | 151/289 (52.2) | 0.45 |
| Symptom duration | >6 mo‡ | 9/10 (90.0) | 169/289 (58.5) | 0.05 |
| Sex | Female | 3/10 (30.0) | 143/289 (49.5) | 0.34 |
| Residence | Rural | 6/10 (60.0) | 213/289 (73.7) | 0.34 |
| Funding | Direct bill‡ | 10/10 (100) | 245/289 (84.8) | 0.37 |
| Diagnosis | Surgical spine‡ | 0/10 (0) | 0/289 (0) | —§ |
| Other body part‡ | 0/10 (0) | 10/289 (3.5) | 1.00 | |
| Surgical spine or other body part‡ | 0/10 (0) | 10/289 (3.5) | 1.00 | |
Any of spine surgery or hip or knee joint replacement surgery.
After list-wise deletion of missing variables.
Dichotomized variables.
Could not be calculated because there was no one with a diagnosis of surgical spine in this sample.
RESULTS
The median age of participants was 51 years (IQR 41, 64), and the median duration of symptoms was 7.2 months (IQR 3.7, 18.2). Based on these median values and clinical relevance, age was dichotomized into ≤50 years and >50 years and symptom duration was dichotomized into ≤6 months and >6 months.
Table 1 lists the frequencies and proportions (valid percent) for each categorical variable for the full sample. Approximately half the participants were women (604/1,162; 52.0%), about half were >50 years old (563/1,096; 51.4%), and the majority lived in “rural” locations, according to their postal codes (739/1,143; 64.7%). Of the 470 patients with data on duration of symptoms, 277 (58.9%) reported symptoms lasting >6 months.
Table 2 compares the characteristics of people who had spine or joint-replacement surgery performed, pending, or deferred for the total sample (ns=336–672) with those of people who did not. The following variables were significant at the 0.05 level: symptom duration >6 months (p=0.010), urban residence (p=0.038), diagnosis of other body part (p=0.034), and diagnosis of surgical spine or other body part (p=0.007).
Table 2.
Characteristics of Participants Who Did and Did Not Have Surgery* Performed, Pending, or Deferred
| Surgical status; no./total (%) of patients |
|||||
|---|---|---|---|---|---|
| Characteristic | Surgery | No surgery | n | p-value | |
| Age | >50 y† | 15/30 (50.0) | 312/642 (48.6) | 672 | 0.88 |
| Symptoms | >6 mo† | 13/14 (92.9) | 207/361 (57.3) | 375 | 0.01 |
| Sex | Female | 11/30 (36.7) | 345/647 (53.3) | 677 | 0.07 |
| Residence | Rural | 14/30 (46.7) | 420/644 (65.2) | 674 | 0.04 |
| Funding | Direct bill† | 12/12 (100) | 278/324 (85.8) | 336 | 0.38 |
| Diagnosis | Surgical spine† | 1/26 (3.8) | 1/601 (0.2) | 627 | 0.08 |
| Other body part† | 3/26 (11.5) | 15/601 (2.5) | 627 | 0.03 | |
| Surgical spine or other body part† | 4/26 (15.4) | 16/601 (2.7) | 627 | 0.01 | |
Any of spine surgery or hip or knee joint replacement surgery.
Dichotomized variables.
Complete data were available for a subset of 299 people after a list-wise deletion of missing variables. Table 3 presents the results of the same analysis, comparing those who had a management outcome of surgery to those who did not. For this reduced sample, none of the variables were significant at p=0.05.
In the total sample (n=671), proportionately more people referred to the surgeon (from the initial triage assessment) had a management outcome of surgery (21/30; 70.0%) than did not (46/641; 7.2%). In the reduced sample (n=299), these proportions were 80.0% (8/10) and 4.2% (12/289) respectively.
DISCUSSION
Reforming primary care involves improving efficiency, coordination, and continuity to ensure that health needs are met in the right place, at the right time, by the appropriate care provider(s).48 When a person presents with LBP and/or lower-quadrant symptoms, one of the most important purposes of the primary health care provider's assessment is to differentiate between the small number of serious pathologies and the majority of benign conditions. The first objective of this exploratory study was to describe demographics, clinical features, and management recommendations for participants in a spinal triage programme. Our most noteworthy finding is the high proportion of participants deemed to have “mechanical spine” problems (92.5%) and the relatively low proportion diagnosed with “surgical spine” (2.0%). This finding reinforces those of previous studies concluding that most patients with back pain referred from primary care providers to orthopaedic surgeons were not considered appropriate surgical candidates, and therefore did not benefit from the surgeons' expertise in surgical management.25,49 Reports from a range of settings and patient populations show that ≤30% of patients who see an orthopaedic surgeon are candidates for surgery.25–28 High proportions of non-surgical referrals are thought to be a main contributor to longer wait times for consultation with orthopaedic surgeons, although the extent to which this is indeed the case requires further study.
A main goal for a primary care practitioner managing patients who present with LBP or lower-quadrant symptoms is to select or recommend the appropriate treatment or management pathways for each patient. In our study, only 16.7% of participants were referred on to the surgeon, which suggests that most people screened by the triage service were not considered by the assessing physiotherapists to need surgical consultation. Furthermore, the high proportions of people referred on to the surgeons who had a management outcome of surgery in both the full (70.0%) and reduced samples (80.0%) suggest that the typical surgical yield of 30% or less can be dramatically altered by physiotherapists performing this triage role. Thus, triage assessment by physiotherapists has the potential to increase the efficiency of an orthopaedic surgeon's caseload by reducing the number of non-surgical referrals, as well as to redirect patients to more appropriate care sooner, rather than having them wait for more than a year to see a surgeon.
Participants who were not referred to the surgeon at the time of the triage assessment but did have surgery performed, pending, or deferred likely underwent a period of conservative care and/or further diagnostic tests after the spinal triage assessment but before the decision to recommend surgical intervention; referral to a surgeon, in these cases, would have been made by the physiotherapist consultant, who may review patients several months after the initial assessment to determine their response to conservative care.
People are referred to the WSSAS with suspected “spine-related” problems; an important role of the WSSAS physiotherapists, however, is the differential diagnosis of conditions that may mimic spinal pathology, as well as determining when referral to a surgeon is appropriate. The second objective of our study was to explore which variables were associated with a “surgical” outcome as determined at the time of chart review (anywhere between 9 and 52 months after the patient's initial WSSAS assessment). This surgical outcome variable, as collected from the chart audit, did not differentiate between people who had surgery, those on a waiting list for surgery, and those for whom surgery was recommended by a surgeon but who chose to defer it. In addition, no distinction was made between people who had spine surgery and those who had a joint (hip or knee) replacement. A small proportion of people referred to the WSSAS are identified (through the PT assessment) as having primarily hip or knee pathology, which can often mimic spine pathology with referral of symptoms to the pelvis and/or lower extremities. Because these problems/diagnoses can be missed or misinterpreted as spine-related problems by the referring care provider, including this group in the analysis is important, as a key role of the WSSAS is to redirect (or triage) people to appropriate management based on the differential diagnosis of the physiotherapists. Therefore, we felt it was important to include people who underwent joint-replacement surgery in our sample, along with those who underwent spine surgery, to reflect this clinical reality.
When only cases with complete data were examined, there were no significant differences between those participants who had surgery performed, recommended, or deferred and those who did not (Objective 2). In the full sample, however, the following variables were significantly different: having symptoms >6 months, rural (vs. urban) residence, and having a classification/diagnosis of “other body part” with or without a “surgical spine” diagnosis (at the time of the triage assessment). Participants with a diagnosis of “surgical spine” or “other body part” (i.e., hip or knee arthritis) were proportionately more likely to have a management outcome of surgery (15.4% vs. 2.7%, p=0.007). This finding seems to indicate that these initial diagnoses by the triage physiotherapists were associated with increased likelihood of a management outcome of surgery; however, since only people referred to the surgeon could be considered for surgery, and having a diagnosis of “surgical spine” is linked to referral to a surgeon, these results should be interpreted with caution. Further research is needed to determine the appropriateness of physiotherapists' referrals to surgeons.
One reason that patients and surgeons may not be comfortable with models of collaborative care is the perception that patients may receive inferior, inaccurate, or inappropriate treatment from another health professional.50,51 Evaluating the “appropriateness” of referral to the surgeon is therefore a key consideration in a programme such as the WSSAS. There is emerging evidence that physiotherapists triaging patients referred to surgeons for a variety of musculoskeletal conditions show acceptable agreement with surgeons with respect to diagnosis and management recommendations, including surgical referral.30,52–54 Research on the use of physiotherapists for triage of patients with spinal conditions only, however, is more limited.37,43 The shift in professional boundaries that places physiotherapists as the first point of contact for orthopaedic referrals means that ensuring a high level of clinical reasoning is paramount. Thus, further research should explore physiotherapists' diagnostic concordance with orthopaedic surgeons for people presenting with LBP and/or spine-related conditions.
The WSSAS uses a model involving assessing and consultant physiotherapists with input from the client (see Figure 2)—an example of collaborative reasoning developing a consensual approach toward the interpretation of examination findings.44,55 The consultant physiotherapist has several years' practice in working collaboratively with the orthopaedic surgeon group.
Differential diagnosis of LBP can be challenging and complex.16,17 Although LBP is most often related to benign underlying patho-anatomical causes that are not amenable to surgery, back pain can be a common presenting symptom of many potentially serious spinal or medical problems. With this increased complexity of clinical cases comes a greater level of professional responsibility and risk. Weatherley and Hourigan43 found that 74% of physiotherapists working in spinal triage roles (n=39) in the United Kingdom reported experiencing stress related to their role. The collaborative reasoning model used by the WSSAS, with the involvement of a consulting physiotherapist in each assessment, may help to ameliorate high levels of stress and improve diagnostic and management appropriateness. To evaluate the role of this model, we are investigating the concordance of diagnostic and management recommendations between the assessing physiotherapist and consultant physiotherapist; a solo assessing physiotherapist; and an orthopaedic surgeon.
This study is based on evaluation of users from the first 3 years of the WSSAS (2003–2006) only. Since the programme's inception, more than 3,000 people have used the service; much of our study sample consists of people waiting to see one of the three participating surgeons, but the WSSAS has since evolved such that fewer users of the service are referred directly to the surgeons and the majority are referred directly to the WSSAS by their primary care provider. This evolution of referral source may affect the distribution of participants' demographics and clinical features; further research is required to determine whether this is indeed the case.
Further study is required to enhance our understanding of effective and efficient management and use of health care resources for LBP and low-back-related conditions. This retrospective study is only a first step toward understanding the potential impact of a spinal triage assessment programme delivered by physiotherapists. Despite research demonstrating the effectiveness of physiotherapists with advanced orthopaedic training in similar triage roles,29,37,41 little is known about the longer-term outcomes and multidimensional predictors of success for a programme such as the WSSAS. Prospective research evaluating participant and health care provider outcomes, using both quantitative and qualitative methods, is needed. Exploration of potential user-, provider-, and system-level barriers and facilitators would also help to enhance spread and uptake of similar models of care in other jurisdictions. Such research would help guide clinicians, health care managers, and policy makers in determining who might benefit from this type of service and how such a service might be implemented in the context of primary care/health care reform.
Our study's main limitations are related to the retrospective design and the use of predetermined variables already collected as part of an internal chart audit, which limited the scope of the variables included. More detailed clinical, psychosocial, and other variables would help to fully explore which factors are related to a surgical spine diagnosis and a management outcome of surgery. We did not have clear operational definitions of some of the variables, notably “diagnosis”; despite the lack of consensus on LBP diagnosis and classification, further research should attempt to define this variable more clearly. Furthermore, there was high variability in the interval between initial assessment and chart review (9–52 months), whereas retrospective reviews of this type often have more tightly controlled time frames. Finally, the outcome of “surgical status” was pulled from reports and chart review, and thus may not have been correctly categorized in all cases; however, the standard administrative procedure of the surgeons' office is to send a surgical report to the physiotherapy clinic for any patient referred through the triage service.
Other limitations relate to the sample size and analysis approach. Although the overall sample size was large, each variable had a different effective sample size because of missing or incomplete data. Because our analysis of which demographic and clinical characteristics and treatment pathway recommendations were associated with a management outcome of surgery was based on a limited sample size, the results should be interpreted with caution. The small proportion of people with a surgical management outcome in our sample further highlights the need for additional research with a large enough sample to account for the small number of “surgical spine” cases, or people who undergo surgery after going through the triage programme. Finally, while dichotomizing variables facilitates analysis and interpretation, it also results in the loss of detailed data that, had the variables not been dichotomized, might have yielded different results.
CONCLUSION
This retrospective study found that most patients with LBP or lower-quadrant symptoms referred from primary care providers to orthopaedic surgeons were not considered by the triage physiotherapists to be candidates for surgery. Further, most users of the spinal triage assessment were classified as having predominantly mechanical spine problems. Of those referred to a surgeon by the triage physiotherapists, most had had surgery, were waiting for surgery, or had deferred surgery. Recommendations for surgery (by a surgeon) were independent of patients' age, sex, duration of symptoms, residence (urban/rural), source of health care funding, and diagnosis in a sample that included only patients with complete data. When the full sample was considered, however, symptom duration >6 months, urban residence, and a diagnosis of “other body part” or of either “surgical spine” or “other body part” were significantly associated with a management outcome of surgery. The proportion of people referred to a surgeon who had surgery performed or recommended (i.e., surgical yield) ranged from 70% in the full sample to 80% in the reduced samples.
Physiotherapists practising in a spinal triage setting have the potential to streamline primary-care management of LBP and reduce wait times for specialist referral, diagnostic testing, and rehabilitation management. Providing timely management recommendations more efficiently than traditional referral pathways can reduce chronicity for people with mechanical pain and expedite referral and management of people who may be candidates for surgery.
KEY MESSAGES
What is already known on this topic
Long waits for orthopaedic elective surgery have been a problem in Canada, and waiting time for an initial consultation with an orthopaedic surgeon can constitute a substantial interruption in the continuum of care. Physiotherapists with advanced orthopaedic training have been shown to be effective in a triage assessment role for a variety of musculoskeletal conditions, but few studies have examined triage assessment of predominantly spine-related pathology.
What this study adds
Our findings provide preliminary evidence that physiotherapists triaging people with spine-related problems referred to orthopaedic surgeons can increase the efficiency of the surgeons' caseload by reducing the number of non-surgical referrals. Most patients referred to orthopaedic surgeons were diagnosed by the triage physiotherapists as having mechanical spinal problems. The minority considered to be surgical candidates and referred to surgeons either had had, were waiting for, or had deferred surgery, for a surgical yield of 70–80% (vs. the typical ≤30% reported in the literature). We propose that if similar models of triage assessment by physiotherapists were adopted by other surgeons whose caseloads include a high proportion of non-surgical low-back-related conditions, wait times would likely be reduced and access improved.
Physiotherapy Canada 2012; 64(4);356–366; doi:10.3138/ptc.2011-29
REFERENCES
- 1.Sanmartin C, Berthelot JM. Report No. 82-575-XIE. Ottawa: Statistics Canada; 2006. Access to health care services in Canada, January to December 2005. [Google Scholar]
- 2.Carriere G, Sanmartin C. Report No. 82-003-XPE. Ottawa: Statistics Canada; 2010. Waiting time for medical specialist consultations in Canada, 2007. [PubMed] [Google Scholar]
- 3.Ackerman IN, Graves SE, Wicks IP, et al. Severely compromised quality of life in women and those of lower socioeconomic status waiting for joint replacement surgery. Arthritis Rheum. 2005;53(5):653–8. doi: 10.1002/art.21439. http://dx.doi.org/10.1002/art.21439. Medline:16208653. [DOI] [PubMed] [Google Scholar]
- 4.Braybrooke J, Ahn H, Gallant A, et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J. 2007;16(11):1832–9. doi: 10.1007/s00586-007-0452-5. http://dx.doi.org/10.1007/s00586-007-0452-5. Medline:17701060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadjistavropoulos H, Snider B, Hadjistavropoulos T. Anxiety in older persons waiting for cataract surgery: Investigating the contributing factors. Can J Aging. 2001;20(1):97–112. http://dx.doi.org/10.1017/S0714980800012150. [Google Scholar]
- 6.Sarro A, Rampersaud YR, Lewis S. Nurse practitioner-led surgical spine consultation clinic. J Adv Nurs. 2010;66(12):2671–6. doi: 10.1111/j.1365-2648.2010.05446.x. http://dx.doi.org/10.1111/j.1365-2648.2010.05446.x. Medline:20831572. [DOI] [PubMed] [Google Scholar]
- 7.Sanmartin C Steering Committee of the Western Canada Waiting List Project. Toward standard definitions of waiting times. Healthc Manage Forum. 2003;16(2):49–53. [Google Scholar]
- 8.Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know [Internet] Ottawa: The Institute; 2006. [cited 2010 Oct 8]. Available from: https://secure.cihi.ca/free_products/WaitTimesReport_06_e.pdf. [Google Scholar]
- 9.Barua B, Rovere M, Skinner BJ. Waiting your turn: wait times for health care in Canada, 2010 report. Vancouver: Fraser Institute; 2010. Report No. 20. [Google Scholar]
- 10.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–5. doi: 10.1016/S0140-6736(99)01312-4. http://dx.doi.org/10.1016/S0140-6736(99)01312-4. Medline:10470716. [DOI] [PubMed] [Google Scholar]
- 11.Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? a review of studies of general patient populations. Eur Spine J. 2003;12(2):149–65. doi: 10.1007/s00586-002-0508-5. Medline:12709853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawrence RC, Felson DT, Helmick CG, et al. National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. http://dx.doi.org/10.1002/art.23176. Medline:18163497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–4. doi: 10.2106/JBJS.E.01273. http://dx.doi.org/10.2106/JBJS.E.01273. Medline:16595438. [DOI] [PubMed] [Google Scholar]
- 14.Gandjour A, Telzerow A, Lauterbach KW INTERCARE International Investigators. European comparison of costs and quality in the treatment of acute back pain. Spine. 2005;30(8):969–75. doi: 10.1097/01.brs.0000158944.54033.60. http://dx.doi.org/10.1097/01.brs.0000158944.54033.60. Medline:15834342. [DOI] [PubMed] [Google Scholar]
- 15.Lim KL, Jacobs P, Klarenbach S. A population-based analysis of healthcare utilization of persons with back disorders: results from the Canadian Community Health Survey 2000-2001. Spine. 2006;31(2):212–8. doi: 10.1097/01.brs.0000194773.10461.9f. http://dx.doi.org/10.1097/01.brs.0000194773.10461.9f. Medline:16418643. [DOI] [PubMed] [Google Scholar]
- 16.Waddell G. The back pain revolution. 2nd ed. Toronto: Churchill Livingstone; 2004. Diagnostic triage; pp. 9–26. [Google Scholar]
- 17.Greenhalgh S, Selfe J. Red flags: a guide to identifying serious pathology of the spine. Toronto: Churchill Livingstone; 2006. [Google Scholar]
- 18.Meadows JTS. Orthopedic differential diagnosis in physical therapy: a case study approach. New York: McGraw-Hill; 1999. [Google Scholar]
- 19.Goodman CC, Snyder TEK. Differential diagnosis for physical therapists: screening for referral. 4th ed. Philadelphia: Saunders Elsevier; 2007. [Google Scholar]
- 20.Hadlow AT. Back pain: a problem of referral. J Bone Joint Surg Br. 2003;85-B(Suppl III):208. [Google Scholar]
- 21.MacKay C, Canizares M, Davis AM, et al. Health care utilization for musculoskeletal disorders. Arthritis Care Res (Hoboken) 2010;62(2):161–9. doi: 10.1002/acr.20064. Medline:20191514. [DOI] [PubMed] [Google Scholar]
- 22.Waddell G. The back pain revolution. 2nd ed. Toronto: Churchill Livingstone; 2004. Epilogue; pp. 457–9. [Google Scholar]
- 23.Chenot JF, Leonhardt C, Keller S, et al. The impact of specialist care for low back pain on health service utilization in primary care patients: a prospective cohort study. Eur J Pain. 2008;12(3):275–83. doi: 10.1016/j.ejpain.2007.06.004. http://dx.doi.org/10.1016/j.ejpain.2007.06.004. Medline:17681811. [DOI] [PubMed] [Google Scholar]
- 24.Canizares M, MacKay M, Davis A, et al. Orthopaedic surgery in Ontario in the era of the wait time strategy. Toronto: Arthritis Community Research & Evaluation Unit; 2006. Report No. 07-2. [Google Scholar]
- 25.Mayman D, Yen D. Maximizing use of a surgical clinic for referrals of patients having back problems. Can J Surg. 1999;42(2):117–9. Medline:10223072. [PMC free article] [PubMed] [Google Scholar]
- 26.Chartered Society of Physiotherapy. Making physiotherapy count. London: The Society; 2004. [Google Scholar]
- 27.Brinker MR, O'Connor DP, Pierce P, et al. Utilization of orthopaedic services in a capitated population. J Bone Joint Surg Am. 2002;84-A(11):1926–32. doi: 10.2106/00004623-200211000-00003. Medline:12429750. [DOI] [PubMed] [Google Scholar]
- 28.Crouch CC, O'Connor DP, Pierce P, et al. Utilization of orthopaedic services for hand and wrist conditions in a capitated population. J Bone Joint Surg Am. 2004;86-A(1):51–6. doi: 10.2106/00004623-200401000-00009. Medline:14711945. [DOI] [PubMed] [Google Scholar]
- 29.Daker-White G, Carr AJ, Harvey I, et al. A randomised controlled trial: shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J Epidemiol Community Health. 1999;53(10):643–50. doi: 10.1136/jech.53.10.643. http://dx.doi.org/10.1136/jech.53.10.643. Medline:10616677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hattam P. The effectiveness of orthopaedic triage by extended scope physiotherapists. Clinical Governance: An International Journal. 2004;9(4):244–52. http://dx.doi.org/10.1108/14777270410566661. [Google Scholar]
- 31.Aiken AB, Harrison MM, Atkinson M, et al. Easing the burden for joint replacement wait times: the role of the expanded practice physiotherapist. Healthc Q. 2008;11(2):62–6. doi: 10.12927/hcq.2008.19618. Medline:18362522. [DOI] [PubMed] [Google Scholar]
- 32.Childs JD, Whitman JM, Sizer PS, et al. A description of physical therapists' knowledge in managing musculoskeletal conditions. BMC Musculoskelet Disord. 2005;6(1):32. doi: 10.1186/1471-2474-6-32. http://dx.doi.org/10.1186/1471-2474-6-32. Medline:15963232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore JH, Goss DL, Baxter RE, et al. Clinical diagnostic accuracy and magnetic resonance imaging of patients referred by physical therapists, orthopaedic surgeons, and nonorthopaedic providers. J Orthop Sports Phys Ther. 2005;35(2):67–71. doi: 10.2519/jospt.2005.35.2.67. Medline:15773564. [DOI] [PubMed] [Google Scholar]
- 34.Boissonnault WG. Primary care for the physical therapist: examination and triage. Toronto: Elsevier; 2005. [Google Scholar]
- 35.Hattam P, Smeatham A. Evaluation of an orthopaedic screening service in primary care. British Journal of Clinical Governance. 1999;4(2):45–9. [PubMed] [Google Scholar]
- 36.Jibuike OO, Paul-Taylor G, Maulvi S, et al. Management of soft tissue knee injuries in an accident and emergency department: the effect of the introduction of a physiotherapy practitioner. Emerg Med J. 2003;20(1):37–9. doi: 10.1136/emj.20.1.37. http://dx.doi.org/10.1136/emj.20.1.37. Medline:12533365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hourigan PG, Weatherley CR. Initial assessment and follow-up by a physiotherapist of patients with back pain referred to a spinal clinic. J R Soc Med. 1994;87(4):213–4. Medline:8182677. [PMC free article] [PubMed] [Google Scholar]
- 38.Aiken AB, McColl MA. Interprofessional healthcare: a common taxonomy to assist with understanding. J Allied Health. 2009;38(3):e92–6. Medline:19753420. [PubMed] [Google Scholar]
- 39.O'Cathain A, Froggett M, Taylor MP. General practice based physiotherapy: its use and effect on referrals to hospital orthopaedics and rheumatology outpatient departments. Br J Gen Pract. 1995;45(396):352–4. Medline:7612338. [PMC free article] [PubMed] [Google Scholar]
- 40.Hendriks EJ, Kerssens JJ, Nelson RM, et al. One-time physical therapist consultation in primary health care. Phys Ther. 2003;83(10):918–31. Medline:14519063. [PubMed] [Google Scholar]
- 41.NHS Modernisation Agency, Department of Health. Improving orthopaedic services: a guide for clinicians, managers and service commissioners. London: NHS Modernisation Agency and Department of Health; 2002. [Google Scholar]
- 42.Alberta Bone and Joint Health Institute. Alberta hip and knee replacement pilot project: scientific evaluation report. Calgary: The Institute; 2007. [Google Scholar]
- 43.Weatherley CR, Hourigan PG. Triage of back pain by physiotherapists in orthopaedic clinics. J R Soc Med. 1998;91(7):377–9. doi: 10.1177/014107689809100709. Medline:9771498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Edwards I, Jones M, Higgs J, et al. What is collaborative reasoning? Adv Physiother. 2004;6(2):70–83. http://dx.doi.org/10.1080/14038190410018938. [Google Scholar]
- 45.Depoy E, Gitlin L. Introduction to research: understanding and applying multiple strategies. Philadelphia: Elsevier Mosby; 2005. [Google Scholar]
- 46.du Plessis V, Beshiri R, Bollman R, et al. Definitions of “rural.” Agricultural and Rural Working Paper No. 61. Ottawa: Statistics Canada Agriculture Division; 2002. [Google Scholar]
- 47.Hazard Munroe B. Statistical methods for health care research. 4th ed. New York: Lippincott; 2001. [Google Scholar]
- 48.Soever L. Primary health care and physical therapists: moving the professions agenda forward. Edmonton: College of Physical Therapists of Alberta; 2006. [Google Scholar]
- 49.Coulter A, Bradlow J, Martin-Bates C, et al. Outcome of general practitioner referrals to specialist outpatient clinics for back pain. Br J Gen Pract. 1991;41(352):450–3. Medline:1839657. [PMC free article] [PubMed] [Google Scholar]
- 50.Carr J, Armstrong S, Hancock B, et al. GPs' perceptions of the nurse practitioner role in primary care. Br J Community Nurs. 2002;7(8):408–13. doi: 10.12968/bjcn.2002.7.8.10646. Medline:12192344. [DOI] [PubMed] [Google Scholar]
- 51.Hooker RS, Cipher DJ, Sekscenski E. Patient satisfaction with physician assistant, nurse practitioner, and physician care: a national survey of medicare beneficiaries. J Clin Outcomes Manag. 2005;12:88–92. [Google Scholar]
- 52.Aiken AB, McColl MA. Diagnostic and treatment concordance between a physiotherapist and an orthopedic surgeon—a pilot study. J Interprof Care. 2008;22(3):253–61. doi: 10.1080/13561820801984134. http://dx.doi.org/10.1080/13561820801984134. Medline:18569412. [DOI] [PubMed] [Google Scholar]
- 53.MacKay C, Davis AM, Mahomed N, et al. Expanding roles in orthopaedic care: a comparison of physiotherapist and orthopaedic surgeon recommendations for triage. J Eval Clin Pract. 2009;15(1):178–83. doi: 10.1111/j.1365-2753.2008.00979.x. http://dx.doi.org/10.1111/j.1365-2753.2008.00979.x. Medline:19239599. [DOI] [PubMed] [Google Scholar]
- 54.Oldmeadow LB, Bedi HS, Burch HT, et al. Experienced physiotherapists as gatekeepers to hospital orthopaedic outpatient care. Med J Aust. 2007;186(12):625–8. doi: 10.5694/j.1326-5377.2007.tb01079.x. Medline:17576177. [DOI] [PubMed] [Google Scholar]
- 55.Edwards I, Jones MA, Carr J, et al. Clinical reasoning strategies in physical therapy. Phys Ther. 2004;84(4):312–30. discussion 331–5 Medline:15049726. [PubMed] [Google Scholar]