Abstract
Introduction
This study was designed to quantitatively evaluate the sealing effect of a polyvinyl chloride tapered endotracheal tube cuff and to compare the tapered cuff with cylindrical endotracheal tube cuffs using an in vitro viscous fluid model.
Methods
Five types of 8.0 mm inner diameter endotracheal tubes (TaperGuard, PortexSacett, PortexSoftseal, Sheridan HVT, Sheridan CF) were fixed in vertically placed 20mm internal diameter acrylic tubes. The cuffs were inflated to 25 mmHg pressure and water was added to the top of the cuff. The amount of water leaking around the cuff at five minutes was measured. Afterwards a viscous fluid was poured above the cuff and the amount of fluid passing around the cuff at five minutes and four hours was measured. Each determination was repeated five times and the data analyzed.
Results
The median (range) amount (ml) of dyed water passing around the cuff at 5 minutes was TaperGuard tube 0 (0-0.2), PortexSacett 81.1 (44.6-107.9), PortexSoftseal 95.4 (91.4-113.7), Sheridan HVT 46.5 (32.7-74.6) and Sheridan CF 52.6 (31.9-62.2), suggesting that TaperGuard significantly (P<0.05) reduced fluid leakage. The viscous fluid leakage at 5 minutes was not significantly different among the groups while the amount of leaked viscous fluid at 4 hours was 0.2 (0-1.1) for the TaperGuard, 57.6 (11.9-117.4) for the PortexSacett, 23.2 (13.8-33.0) for the PortexSoftseal, 5.5 (2.7-15.4) for the Sheridan HVT and 5.6 (1.8-7.9) for the Sheridan CF.
Conclusion
An endotracheal tube with a tapered polyvinyl chloride cuff had significantly less fluid leakage compared to four tubes with cylindrical cuffs.
Keywords: VAP, cuff leak, tapered shape cuff, endotracheal tube
Introduction
Ventilator associated pneumonia is reported to occur in 8-28% of intubated patients, and is associated with prolonged duration of mechanical ventilation, length of intensive care unit (ICU) stay, length of hospitalization and increased costs [1,2]. Aspiration of oropharyngeal pathogens and leakage of contaminated fluid around the endotracheal tube cuff into the lower respiratory tract are possible primary causes of ventilator associated pneumonia [3].
Low-volume, high-pressure cuffs, used until the 1960s, were able to seal the trachea sufficiently [4]. However, they required inflation pressures of 160 to 300 mmHg and it was difficult to estimate the actual pressure exerted on the tracheal wall. The resulting high pressures could compromise tracheal blood flow, resulting in mucosal ulceration, tracheomalacia and perforation [5]. The pressure exerted by the high-volume, low-pressure cuffs, popularized in the early 1970s, is almost equal to the cuff inflation pressure.
These can be used for positive pressure ventilation with a cuff inflation pressure less than 30 mmHg, which is the perfusion pressure of the tracheal wall. However, longitudinal folds can occur since the size of the cuff is larger than the diameter of the trachea.
Longitudinal folds arise on the surface of the inflated cuff within the trachea and they are thought to play an important role in leakage of fluid around the endotracheal tube cuff [4,6,7].
A recently developed endotracheal tube (TaperGuard, Covidien, CO, USA) has a tapered cuff that is intended to seal the trachea better than previously introduced endotracheal tubes. The shape of this tube is effective in preventing leakage via longitudinal folds [8].
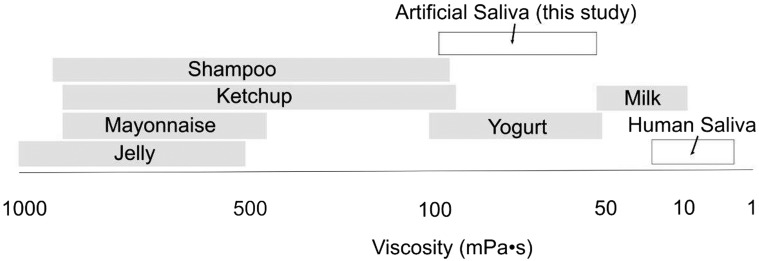
A previous study, evaluating the sealing ability of the tapered cuff, was performed over a short, probably not clinically meaningful duration [8]. The fluid used in previous studies was water with a viscosity lower than human saliva (Figure 1) [7,8,9,10].
Figure 1.
Viscosity of various fluids measured at 25°C (except for human saliva which is measured at 37°C).
We therefore compared a polyvinyl chrolide (PVC) tapered cuff tube with PVC cylindrical cuffs over a longer time than previously reported and using both a water model [6,8,9,10] and a viscous fluid model to provide a more clinically representative model than using water alone.
Methods
We compared four commercially available 8.0 mm internal diameter (ID) endotracheal tubes (PortexSacett, Smiths medical, UK; Portexsoftseal, Smiths medical, UK; Sheridan CF, Hudson RCI, NC, USA; Sheridan HVT, Hudson RCI, NC, USA) with an 8.0 mm ID TaperGuard-PVC tube (Figure 2).
Figure 2.

The cuff of TaperGuard-PVC.
The cuffs of all the endotracheal tubes tested were made of PVC. The TaperGuard-PVC is a tapered cuff, while the other four tested are cylindrical shaped cuffs. Tubes were tested for leakage using water and a viscous fluid (Kyoto Kagaku Co., Ltd. (Kyoto, Japan), provided by Covidien Japan Co., Ltd. (Tokyo, Japan)).
An acrylic tube of 20 mm ID was vertically placed as an artificial trachea and the endotracheal tube inserted and fixed in the acrylic tube with the cuff inflated to 25 mmHg pressure. The ID of 20 mm of the artificial trachea was based on the model used in previous studies [11].
The present model, using a rigid artificial trachea, a fixed endotracheal tube and pouring liquid above the cuff, is similar to that used in a prior study of the TaperGuard-PU [8] and in other studies that evaluated cuff effectiveness [6, 9, 12,13,14].
The sealing effect of the cuffs was tested using the following protocol. Ten milliliters of water (viscosity was 1mPa • S) were placed above the inflated tube cuff and the amount of water that passed around the tube cuff within 5 minutes was measured.
If all of the initially placed water passed through the cuff, another 10 ml of water was added just before the prior aliquot was gone. This procedure was repeated 5 times for each endotracheal tube.
The amount of water that passed around the cuff was measured at 5 minutes for all tubes tested, and in addition at 4 hours and 8 hours for the TaperGuard-PVC. Each determination was repeated five times and the data pooled.
After testing with water, the endotracheal tubes were cleaned and dried. They were again placed in the artificial trachea and 10 ml of viscous fluid (viscosity 50-150mPa • S) applied above the inflated tube cuff. The amount of viscous fluid that passed around the tube cuff was measured at 5 minutes and 4 hours. If all of the initially placed viscous fluid passed through the cuff, another 10 ml of fluid was added just before the prior aliquot was gone. The experiment was repeated 5 times for each tube tested.
Statistical analysis. Data are expressed as median (range).
We compared the amount of fluid that leaked around each endotracheal tube with that for TaperGuard-PVC using Dunnett’s test.
This statistical technique uses the difference between the absolute value of the difference minus the least significant difference. This value was then converted to a p-value. The level of significance was set at p<0.05. JMP version 9.0.1 (SAS institute, NC, USA) was used for the analysis.
Results
In the first test, the amount of water leaking around each tube was measured over five minutes.
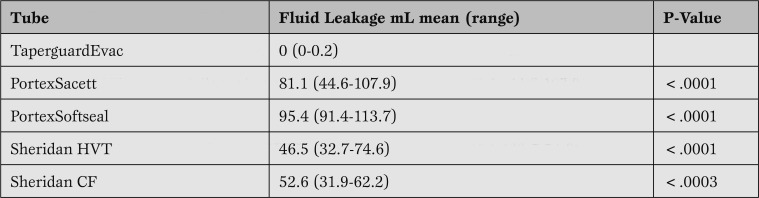
While leakage of water around the TaperGuard-PVC tube was 0 (0-0.2) ml, leakage around the other tubes was significantly (p<.05) higher, demonstrating the effectiveness in sealing the artificial trachea in this model compared to the other endotracheal tubes tested (Table 1).
Table 1.
The amount of water (ml (range)) leaking around the cuff at 5 minutes. Values are the mean of 5 determinations for each tube. P-values refer to the comparison of each tube to the Taperguard tube.
Given the high volume of drainage in just 5 minutes, testing at later time points was not conducted for all tubes studied.
However, drainage around the TaperGuard-PVC tube was tested at four hours and eight hours, and measured at 0.2 (0-4.2) ml and 0.2 (0-5.0) ml, respectively, thus maintaining an effective seal over a long time period when tested with water.
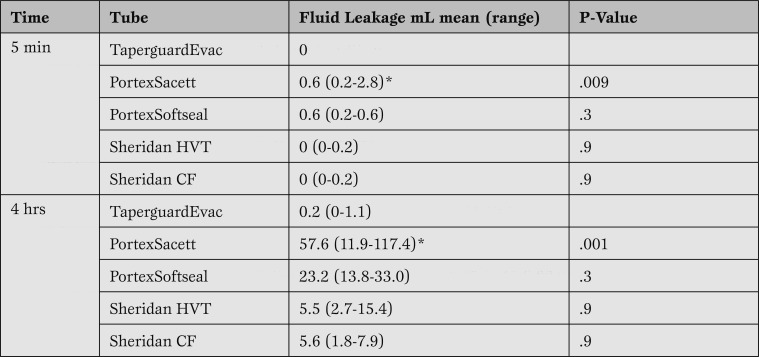
In the second test, leakage of a viscous fluid was measured around each tube, and very little of the viscous fluid passed around any tube at 5 minutes (Table 2).
Table 2.
The amount of viscous fluid (ml) leaking around the cuff measured at 5 minutes and 4 hours. Values shown are the mean of 5 determinations for each tube. P-values refer to the comparison of each tube to the Taperguard tube.
There was little or no leakage in the first 5 minutes with any tube while at 4 hours the median leakage of the viscous fluid around the TaperGuard-PVC tube was significantly less than the PortexSacett tube (Table 2).
Discussion
This study evaluated the effect of cuff shape on tracheal sealing by measuring the leakage of both water and a viscous fluid around an endotracheal tube using an in vitro model.
The model attempts to simulate the clinical situation in an ICU patient by testing with a viscous liquid as well as by testing over an extended time period.
These data show that the cuff of the TaperGuard-PVC tube allowed less drainage of fluid around the cuff compared to other tubes tested with water, and had an effective seal with a viscous liquid over a long time period. These results using a tapered cuff endotracheal tube water are consistent with a previous study, done with water alone [8].
Dave MH et al. concluded that the superiority was derived from both the shape and the PVC material of the cuff. The present study compared tubes all made of PVC demonstrating that the tapered cuff was a more effective seal compared to the cylindrical cuffs tested.
In addition to a prior in-vitro study using TaperGuard [8], two randomized clinical trials and one historically controlled clinical trial showed the association of reduced pneumonia with polyurethane (PU) cuffed tubes [15,16,17].
In these previous studies, the PVC cuffs tested were cylindrical in shape, rather than tapered and the investigators concluded that PVC was not effective.
On the contrary, an excellent sealing effect was seen with the PVC tapered cuff in the present study that evaluated the function of a tapered PVC cuff compared to cylindrical PVC endotracheal tube cuffs using not only water but also a viscous fluid and over a longer duration. These results demonstrate that a PVC cuff can be an effective tracheal seal in this in vitro model. These discordant findings may be attributed to the shape of the cuff, as previous studies used cylindrical PVC cuffs, rather than the tapered cylindrical cuff tested in this study.
Dave et al. suggested that the ratio of the cross sectional area (CSA) of the cuff to that of the trachea could also affect the fluid leakage around the cuff [8].
They concluded that a ratio of more than 1.5:1 facilitated the development of longitudinal folds in the cuff, which may allow the passage of fluid.
The TaperGuard has a smaller resting cuff diameter compared with other endotracheal tubes tested, except the Sheridan CF.
The artificial trachea used in this study was relatively small, which may have favorably affected the results obtained with the TaperGuard and Sheridan CF. However, only the TaperGuard demonstrated less fluid leakage. This also suggests that a tapered cuff has a better sealing effect compared with the conventional cuff shape. The ratio and the maximum resting cuff diameter are shown in Table 3, calculated from data provided by the manufacturers.
Table 3.
The ratio of the cross sectional area of the cuff (maximum resting diameter) to the inner diameter of the artificial trachea, and the size of the maximum resting cuff diameter of each endotracheal tube tested.
Although prior studies of cuff sealing effectiveness focused on short duration studies using water, other testing conditions may have more clinical relevance. The tapered cuff tube showed continued effectiveness up to 8 hours of testing, but tests beyond the initial 5 minutes were not possible with the other tubes due to their already high leakage rate.
In this study, the leakage of a viscous fluid was also tested to more closely simulate the clinical situation.
The viscosity of human saliva is reported in normal volunteers from 2.8-15.5 milliPascal-seconds (mPa • S) [18], but the exact value may depend on volume status or autonomic nerve activity. The viscosity of the fluid used in this study was higher than that of human saliva, and its relative viscosity can be seen in Figure 1 compared to a variety of other fluids.
Patients admitted to the ICU generally have different volume or autonomic status compared to normal volunteers, however, highly viscous saliva may be present in some clinical settings.
The relatively high viscosity of the fluid tested may have affected the results, but adds important information in comparison to testing with water alone, as performed in previous studies [6,7,8,9,10, 12,13,14]. ll tested PVC tubes showed less fluid leakage with the viscous fluid than with water suggesting that, in a viscous fluid model, tapered cuffs are not necessarily superior to cylindrical cuffs.
We acknowledge the following limitations of the present study: the exact thickness of the PVC cuff membranes was not available from the manufacturers; the tests were performed in vitro with no swallowing motion of the larynx no neck flexion and extension, no positive pressure ventilation and further studies are needed.
Furthermore, preventing leakage around any cuff may reduce the volume and rate of aspiration around the cuff but will not prevent the accumulation of secretions in the subglottic space: this pooled volume of colonized subglottic secretions is still present and therefore the potential for aspiration around the cuff still exists.
The present study in an in vitro model suggests that tapered PVC cuffs allow less drainage of water when compared with four different cylindrical PVC cuffs and that they perform well when tested with a viscous fluid in both short and long term tests.
The significant results of these in vitro studies suggest the need for clinical trials to study the role of tapered PVC cuffs to reduce the incidence of ventilatory associated pneumonia.
Footnotes
Source of Support Nil.
Conflict of interest None declared.
Cite as: Shiotsuka J, Lefor AT, Sanui M, Nagata O, Horiguchi A, Sasabuchi Y. A quantitative evaluation of fluid leakage around a polyvinyl chloride tapered endotracheal tube cuff using an in-vitro model. HSR Proceedings in Intensive Care and Cardiovascular Anesthesia 2012; 4(3): 169-175
References
- Chastre J, Fagon J Y. Ventilator-associated pneumonia. Am J RespirCrit Care Med. 2002;165:867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- Rello J, Ollendorf D A, Oster G. et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122:2115–2221. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- American Thoracic Society , Infectious Diseases Society of America . Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- Seegobin R D, van Hasselt G L. Aspiration beyond endotracheal cuffs. Can Anaesth Soc J. 1986;33:273–279. doi: 10.1007/BF03010737. [DOI] [PubMed] [Google Scholar]
- Guyton D, Banner M J, Kirby R R. High-volume, low-pressure cuffs. Are they always low pressure? Chest. 1991;100:1076–1081. doi: 10.1378/chest.100.4.1076. [DOI] [PubMed] [Google Scholar]
- Dullenkopf A, Gerber A, Weiss M. Fluid leakage past tracheal tube cuffs: evaluation of the new Microcuff endotracheal tube. Intensive Care Med. 2003;29:1849–1853. doi: 10.1007/s00134-003-1933-6. [DOI] [PubMed] [Google Scholar]
- Oikkonen M, Aromaa U. Leakage of fluid around low-pressure tracheal tube cuffs. Anaesthesia. 1997;52:567–569. doi: 10.1111/j.1365-2044.1997.149-az0153.x. [DOI] [PubMed] [Google Scholar]
- Dave M H, Frotzler A, Spielmann N. et al. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth. 2010;105:538–543. doi: 10.1093/bja/aeq202. [DOI] [PubMed] [Google Scholar]
- Zanella A, Cressoni M, Epp M. et al. A double-layer tracheal tube cuff designed to prevent leakage: a bench-top study. Intensive Care Med. 2008;34:1145–1149. doi: 10.1007/s00134-008-1016-9. [DOI] [PubMed] [Google Scholar]
- Asai T, Shingu K. Leakage of fluid around high-volume, low-pressure cuffs. A comparison of four tracheal tubes. Anaesthesia. 2001;56:38–42. doi: 10.1046/j.1365-2044.2001.01718.x. [DOI] [PubMed] [Google Scholar]
- Mehta S, Myat H M. The cross-sectional shape and circumference of the human trachea. Ann R Coll Surg Engl. 1984;66:356–358. [PMC free article] [PubMed] [Google Scholar]
- Young P J, Pakeerathan S, Blunt M C. et al. A low-volume, low-pressure tracheal tube cuff reduces pulmonary aspiration. Crit Care Med. 2006;34:632–639. doi: 10.1097/01.CCM.0000201406.57821.5B. [DOI] [PubMed] [Google Scholar]
- Blunt M C, Young P J, Patil A. et al. Gel lubrication of the tracheal tube cuff reduces pulmonary aspiration. Anesthesiology. 2001;95:377–381. doi: 10.1097/00000542-200108000-00019. [DOI] [PubMed] [Google Scholar]
- Dave M H, Koepfer N, Madjdpour C. et al. Tracheal fluid leakage in benchtop trials: comparison of static versus dynamic ventilation model with and without lubrication. J Anesth. 2010;24:247–252. doi: 10.1007/s00540-010-0871-z. [DOI] [PubMed] [Google Scholar]
- Lorente L, Lecuona M, Jiménez A. et al. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia. Am J Respir Crit Care Med. 2007; 176: 1079-83. 2007;176:1079–1083. doi: 10.1164/rccm.200705-761OC. [DOI] [PubMed] [Google Scholar]
- Poelaert J, Depuydt P, De Wolf A. et al. Polyurethane cuffed endotracheal tubes to prevent early postoperative pneumonia after cardiac surgery: a pilot study. J Thorac Cardiovasc Surg. 2008;135:771–776. doi: 10.1016/j.jtcvs.2007.08.052. [DOI] [PubMed] [Google Scholar]
- Miller M A, Arndt J L, Konkle M A. et al. A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia. J Crit Care. 2011;26:280–286. doi: 10.1016/j.jcrc.2010.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preetha A, Banerjee R. Comparison of Artificial Saliva Substitute. Trends Biomater Artif Organs. 2005;18:178–186. [Google Scholar]