Abstract
Background
As the prevalence and severity of obesity among adolescents has increased, so has the number seeking bariatric surgery. Little is known about the opinions and referral behaviors of primary care physicians regarding bariatric surgery among adolescents. Therefore, the objective of this study was to assess primary care physicians’ opinions regarding referral of obese adolescents for bariatric surgery.
Methods
In spring of 2007, a two-page survey was fielded to a national randomsample of physicians (375 pediatricians and 375 family physicians). The survey explored physicians’ opinions about: (1) whether they would ever refer an adolescent for bariatric surgery, (2) the minimum age at which bariatric surgery should be considered, and (3) prerequisites to bariatric surgery. Chi-square tests were used to examine associations in responses.
Results
The response rate was 67%. Nearly one-half of physicians (48%) would not ever refer an obese adolescent for bariatric surgery. The most frequently endorsed minimum age at which physicians would make a referral for bariatric surgery was 18 years (46%). Almost all respondents endorsed the need for participation in a monitored weight management program prior to bariatric surgery (99%). However, the recommended duration of treatment varied from 3 months to over 5 years, with almost half recommending 12 months of monitored treatment prior to surgery.
Conclusion
Some severely obese adolescents may desire and potentially benefit from bariatric surgery, but referral for the procedure may depend heavily on the attitudes of their primary care physicians.
Keywords: Obesity, Adolescents, Bariatric surgery, Referrals, Primary care physicians
Introduction
The prevalence of childhood obesity has increased dramatically since the 1970s and currently remains high [1–5]. National Health and Nutrition Examination Survey data from 2007 to 2008 estimate the overall prevalence of childhood obesity at 16.9% [5]. Moreover, a significant proportion of children are extremely obese (i.e., BMI≥99th percentile for age and sex), documented at 4% of children in 2004 [6]; this is similar to the proportion of extremely obese adults in the same year (4.8%) [7]. The public health ramifications of this epidemic are significant as obese adolescents are more likely to suffer from a number of comorditities including type 2 diabetes, hypertension, nonalcoholic steatohepatitis, sleep apnea, and cholelithiasis [8–12]. In addition, extremely obese adolescents will very likely become extremely obese adults, putting them at risk not only for a host of obesity-related comorbidities but also premature death [13–18].
As the prevalence and severity of obesity among adolescents has increased, so has the number seeking bariatric surgery [19]. The number of US adolescents undergoing bariatric surgery has increased, from 51 cases in 1997 to 282 case in 2003 [20]. Among adults, bariatric surgery has been shown to be an effective means of producing sustained weight loss, improving obesity-related conditions, and reducing premature mortality [21, 22]. Fewer longitudinal studies exist that address the benefits and risks of bariatric surgery in adolescents. However, early data suggests that bariatric surgery may have positive physiologic outcomes among adolescent patients, with similar surgical risks as among adults [20, 23].
Primary care physicians (pediatricians (PDs) and family physicians (FPs)) who care for adolescents are faced with making treatment decisions for obesity. Currently, little is known about the opinions of primary care physicians regarding bariatric surgery for adolescents. Therefore, the objective of this study is to assess pediatricians’ and family physicians’ opinions regarding referral of obese adolescents (13–17 years old) for bariatric surgery.
Methods
Sample A national random sample of 375 pediatricians and 375 family physicians was drawn from the American Medical Association (AMA) Masterfile, a comprehensive listing of licensed US physicians, including AMA members and non-members. The sampling frame included all allopathic and osteopathic physicians self-described as a general pediatrician or family physician, in office-based direct patient care. Excluded were physicians with any specialty board listing, physicians 70 years of age or older, and resident physicians. Along with names and addresses, the AMA Masterfile also includes demographic information such as physician specialty, gender, year of medical school graduation, and board certification.
Instrument
The investigators developed a self-administered, two-page, 30-item survey instrument with fixed choice, Likert scale, and open-ended questions. The survey explored physicians’ opinions about the management of obese adolescents, including usual practice for referrals of obese adolescents and factors that impact those referrals patterns. Specifically, in relation to bariatric surgery for adolescents, questions probed physicians’ opinions about: (1) whether they would ever refer an adolescent for bariatric surgery, (2) the minimum age at which they would consider bariatric surgery for their patients, the minimum BMI at which bariatric surgery should be considered for adolescents, and (3) prerequisites to bariatric surgery. The survey instrument was pilot tested with a convenience sample of physicians to ensure clarity and ease of administration; refinements were made based on pilot test feedback.
Survey Administration
During spring 2007, the survey, along with a cover letter explaining the purpose of the study, were mailed to the full sample. Two subsequent mailings were sent to non-respondents at 3-week intervals. Data Analysis After verification of data entry, univariate frequencies were generated for each variable. Bivariate analyses using chi-square test, t test, and ANOVA were performed to examine the association between physician opinions and physician specialty, years since medical school graduation (≤10 years, 11–20 years, and >20 years), physician gender, and history of board certification. All analyses were conducted using STATA 8.0 (Stata Corporation; College Station, TX, USA). This study was approved by the Institutional Review Board of the University of Michigan Medical School.
Results
Of the 750 physicians in this national sample, 78 were excluded because the mailing materials were returned as undeliverable. Of the remaining sample, 451 completed surveys were returned, resulting in an overall response rate of 67% (pediatricians 76%, family physicians 58%). Seventy of these respondents were determined to be ineligible for the study because they reported that they did not provide care for adolescents. Thus, 381 surveys remained for final analysis giving an eligible response rate of 63%. There were no significant differences between non-respondents and respondents based on demographic characteristics (gender, years since graduation, and board certification) from the AMAMasterfile.
The characteristics of eligible respondents are presented in Table 1. Pediatricians and family physicians in this sample did not differ significantly in years since graduation or percentage with board certification. However, a higher percentage of pediatricians than family physicians were female.
Table 1.
Sample Characteristics
| Pediatricians (%) | Family physicians (%) | p value |
|---|---|---|
| Gender | ||
| Female 57 | 37 | <0.001 |
| Male 43 | 63 | |
| Years since graduation | ||
| ≤10 years 22 | 23 | 0.5 |
| 11–20 years 39 | 43 | |
| >20 years 39 | 34 | |
| History of board certification | ||
| Yes 88 | 85 | 0.4 |
| No 12 | 15 | |
Regarding physicians’ perceptions about referrals for bariatric surgery, nearly one-half of physicians (48%) surveyed stated they would not ever refer an obese adolescent for bariatric surgery. Results were not significantly different by specialty (pediatricians 47% vs. family physicians 50%; p=0.53), physicians’ gender (female 45% vs. male 52%; p=0.18), history of board certification (certified 47% vs. not certified 60%; p=0.1), or years in practice (≤10 years 48%, 11–19 years 52%, and ≥20 years 49%; p=0.42).
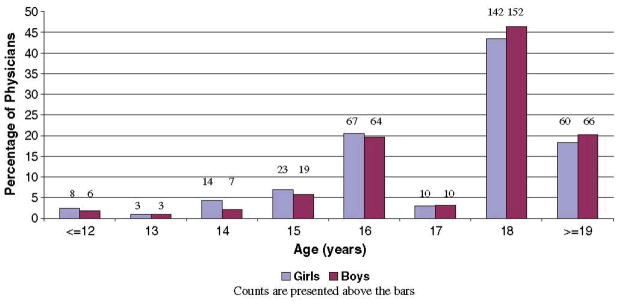
With regard to the minimum age at which physicians believe bariatric surgery should be considered for adolescents, the mean and median age for boys and girls combined was 18 years old (Fig. 1). Few physicians felt that bariatric surgery should be considered for adolescents younger than 15 years. The mean minimum age varied by whether physicians indicated they themselves would vs. would not refer adolescents for bariatric surgery (16.9 vs. 19.6 years; p<0.01).
Fig. 1.
Physicians’ opinions regarding the minimum age at which bariatric surgery should be considered in boys and girls
Of note, only 17% of physicians indicated different minimum ages for boys vs. girls. In this subgroup, the average age at which physicians would consider bariatric surgery for girls was 1.5 years younger than for boys (16.3 vs. 17.8 years; p<0.01). These physicians were more likely to state that they would refer adolescents for bariatric surgery, compared to those that indicated the same minimum age for boys and girls (69% vs. 50%; p<0.01).
Among those providers who indicated a level of obesity severity at which bariatric surgery should be considered for adolescents, the most common minimum levels suggested were a BMI of 40 (45% FPs vs. 16% PDs), a BMI of 35 (25% FPs vs. 17% PDs), and a minimum BMI percentile of 95 (6% FPs vs. 16% PDs).
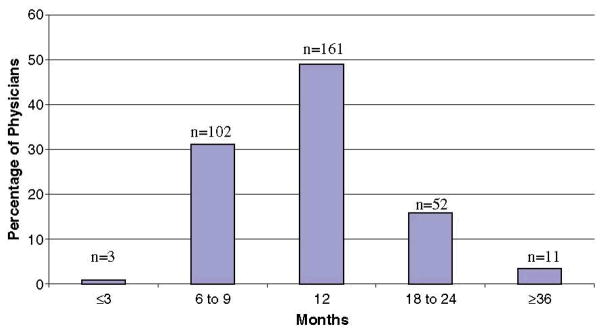
Almost all respondents endorsed participation in a monitored weight loss program as a prerequisite to bariatric surgery (99%). However, physicians’ preferences for the minimum duration of treatment in such weight loss programs prior to bariatric surgery varied from 3 months to over 5 years, with 96% recommending a duration between 6 and 24 months (Fig. 2). Overall, the mean recommended minimum treatment duration was 13.4 months. On average, pediatricians, compared to family physicians, recommended a minimum treatment duration that was 2.4 months longer (pediatricians 14.4 months vs. family physicians 12.0 months, p<0.05). Findings did not differ by physician gender, board certification, or years in practice.
Fig. 2.
Physicians’ opinions regarding the length of time adolescents should participate in a monitored weight management program prior to undergoing bariatric surgery
Beyond a monitored weight loss program, physicians were asked to state other prerequisites for surgery. The most frequent responses indicated that patients should have: passed a psychological evaluation (n=65), co-morbid conditions (n=43), demonstrated commitment/compliance with lifestyle changes (n=42), individual/family counseling (n=23), and family support (n=23).
Discussion
This study is the first to document primary care physicians’ perceptions regarding referral of obese adolescents for bariatric surgery. The most important finding of this study is that nearly half of primary care physicians would not ever refer obese adolescents for bariatric surgery, and that most thought patients should be at least 18 years old in order to be considered for bariatric surgery. Few physicians made distinctions regarding this minimum age based on patient gender. In addition, we found that virtually all physicians felt adolescents should participate in a monitored weight loss program prior to undergoing bariatric surgery and the majority thought that the minimum duration of participation in such a program should be 12 months or longer.
Previous studies suggest that bariatric surgery can improve obesity-related conditions in adolescents and can result in sustained weight loss [23, 24]. However, physicians appear reticent to refer obese adolescents for bariatric surgery. The reasons for this reluctance are unknown but physicians were likely uncertain about the long-term consequences of bariatric surgery. As long-term outcomes data for adolescents are currently limited, physicians could have concerns regarding potential problems for patients in the future. Without these data they may wonder whether the benefits of weight loss surgery outweigh the risks at this age. Furthermore, they may believe that a decision of this magnitude is best left until patients are old enough to give consent and have a better understanding of the ramifications of this significant procedure. However, the adolescent years can be difficult socially and emotionally for extremely obese youth [25–27]. In addition, studies indicate that obesity in adolescents has long-term health effects even if the patient ultimately loses weight, lending support for early intervention [17]. Indeed, a recent study showed that BMI prior to gastric bypass surgery is a strong predictor of an adolescent’s nadir BMI following surgery [28]. Thus suggesting that delays in referrals for weight loss surgery that result in a higher BMI at the time of surgical intervention may impact the likelihood of obese adolescents achieving a BMI within the normal range post-operatively. These health and quality of life considerations make the decision of whether or not to refer a particularly thorny one. Although the number of adolescents undergoing bariatric surgery is increasing rapidly, these surgical patients are still infrequently encountered by primary care physicians. With greater surgical volumes and experiences with patients who have undergone bariatric surgery, primary care physicians’ perceptions and practice may well change.
The majority of physicians indicated that adolescents should participate in a monitored weight loss program for at least 1 year prior to being considered for surgical weight loss interventions. Whether participation in such programs is helpful by providing time for adolescents to make a stable decision regarding surgery and for them to adopt healthy habits that will improve their post-operative course, or whether this delay in surgery leads to further weight gain and poor long-term outcomes, is a question requiring further study. Furthermore, it is unknown whether such programs are widely available for adolescents to attend. The most generally available weight loss program for pediatrics is ShapeDown [29]. However, this program is typically only 10–20 weeks long. This often leaves only commercial programs such as Weight Watchers, which are generally targeted to adults. Whether such programs represent an appropriate effort for adolescents prior to undergoing bariatric surgery is a compelling clinical question, but beyond the scope of this study.
This study did not explore whether physicians discuss surgical options with their obese patients. However, the fact that many would not ever refer an adolescent for bariatric surgery suggests that surgery is likely broached infrequently with obese patients. Further work should examine this issue; with the increasing media presentations of surgeries for weight loss among the general public and Hollywood celebrities, more obese adolescents and their parents are likely to consider it as an option. Efforts may be needed to ensure that primary care physicians are prepared to help obese adolescents consider the expanding range of treatment options. Fortunately, a growing number of articles addressing the issue of bariatric surgery for adolescents are now available, which might help inform physicians’ discussions with patients and their decisions about referrals [30, 31].
Limitations
This study’s response rate of 67% is favorable to many other published national physician surveys [31–34]. However, respondents may not be representative of all pediatricians and family physicians. It may be that those physicians who responded to the survey hold stronger opinions about adolescents undergoing bariatric surgery compared with pediatricians and family physicians in general. However, we are unable to determine the direction of these potential differences in opinion. Also, we examined physicians’ perceptions; actual referral patterns may differ significantly.
Conclusions
Some extremely obese adolescents may benefit from bariatric surgery, but whether they will be referred for the procedure may depend strongly on the opinions of their primary care physicians about this treatment option. Further work should explore primary care physicians’ knowledge regarding the risks and benefits of bariatric surgery for adolescents and the basis upon which they make referral decisions regarding bariatric surgery for their obese patients.
Footnotes
The authors declare that they have no conflict of interest.
Financial Disclosure None to disclose.
Contributor Information
Susan J. Woolford, Email: swoolfor@med.umich.edu, Pediatric Comprehensive Weight Management Center; Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics, University of Michigan, Ann Arbor, MI, USA, 300 NIB, Room 6D20, Campus Box 0456, Ann Arbor, MI 48109-5456, USA
Sarah J. Clark, Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics, University of Michigan, Ann Arbor, MI, USA
Achamyeleh Gebremariam, Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics, University of Michigan, Ann Arbor, MI, USA.
Matthew M. Davis, Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics; Division of Internal Medicine; The Gerald R. Ford School of Public Policy, University of Michigan, Ann Arbor, MI, USA
Gary L. Freed, Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics, University of Michigan, Ann Arbor, MI, USA
References
- 1.Ogden CL, Flegal KM, Carroll MD, et al. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 2.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286(22):2845–8. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 3.Troiano RP, Flegal KM, Kuczmarski RJ, et al. Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149(10):1085–91. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 4.Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 6.Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa heart study. J Pediatr. 2007;150(1):12–7. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 7.Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000. Int J Obes Relat Metab Disord. 2004;28(1):4–9. doi: 10.1038/sj.ijo.0802421. [DOI] [PubMed] [Google Scholar]
- 8.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25. [PubMed] [Google Scholar]
- 9.Must A, Strauss R. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23:S2–11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 10.Steinberger J, Moorehead C, Katch V, et al. Relationship between insulin resistance and abnormal lipid profile in obese adolescents. J Pediatr. 1995;126:690–5. doi: 10.1016/s0022-3476(95)70394-2. [DOI] [PubMed] [Google Scholar]
- 11.Rhodes SK, Shimoda KC, Waid LR. Neurocognitive deficits in morbidly obese children with obstructive sleep apnea. J Pediatr. 1995;127:741–4. doi: 10.1016/s0022-3476(95)70164-8. [DOI] [PubMed] [Google Scholar]
- 12.Ciba I, Widhalm K. The association between non-alcoholic fatty liver disease and insulin resistance in 20 obese children and adolescents. Acta Paediatr. 2007;96(1):109–12. doi: 10.1111/j.1651-2227.2007.00031.x. [DOI] [PubMed] [Google Scholar]
- 13.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srinivasan SR, Bao W, Wattigney WA, et al. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors. The Bogalusa heart study. Metabolism. 1996;45:235–40. doi: 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 15.Guo SS, Roche AF, Chumela WC, et al. The predictive value of childhood body mass index values for overweight at age 35 y. Am J Clin Nutr. 1994;59:810–9. doi: 10.1093/ajcn/59.4.810. [DOI] [PubMed] [Google Scholar]
- 16.Serdula MK, Ivery D, Coates RJ, et al. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–77. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 17.Must A, Jacques P, Dallal G, et al. Long-term morbidity and mortality of overweight adolescents. N Engl J Med. 1992;327:1350–5. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 18.Gunnell DJ, Frankel SJ, Nanchahal K, et al. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr. 1998;67(6):1111–8. doi: 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- 19.Davis MM, Slish K, Chao C, et al. National trends in bariatric surgery, 1996–2002. Arch Surg. 2006;141(1):71–4. doi: 10.1001/archsurg.141.1.71. [DOI] [PubMed] [Google Scholar]
- 20.Schilling P, Davis Albanese CT, Dutta S, et al. National trends in adolescent bariatric surgical procedures and implications for surgical centers of excellence. J Am Coll Surg. 2008;206(1):1–12. doi: 10.1016/j.jamcollsurg.2007.07.028. Epub 2007 Oct 18. [DOI] [PubMed] [Google Scholar]
- 21.Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 22.Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 23.Lawson ML, Kirk S, Mitchell T, et al. One-year outcomes of Roux-en-Y gastric bypass for morbidly obese adolescents: a multicenter study from the Pediatric Bariatric Study Group. J Pediatr Surg. 2006;41(1):137–43. doi: 10.1016/j.jpedsurg.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Sugerman HJ, Sugerman EL, DeMaria EJ, et al. Bariatric surgery for severely obese adolescents. J Gastrointest Surg. 2003;7(1):102–7. doi: 10.1016/S1091-255X(02)00125-7. [DOI] [PubMed] [Google Scholar]
- 25.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157:746–52. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 26.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 27.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 28.Inge TH, Jenkins TM, Zeller M, et al. Baseline BMI is a strong predictor of Nadir BMI after adolescent gastric bypass. J Pediatr. 2010;156:103–8. doi: 10.1016/j.jpeds.2009.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]; OBES SURG. 2010;20:937–942. 941. doi: 10.1007/s11695-010-0152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. [Accessed on January 13th, 2008];ShapeDown. Available online at http://www.shapedown.com.
- 30.Pratt JS, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity. 2009;17(5):901–10. doi: 10.1038/oby.2008.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caniano DA. Ethical issues in pediatric bariatric surgery. Semin Pediatr Surg. 2009;18(3):186–92. doi: 10.1053/j.sempedsurg.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 32.Asch DA, Jedriewski K, Christakis DA. Response rates to mailed surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–36. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 33.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35:1347–55. [PMC free article] [PubMed] [Google Scholar]
- 34.Cull WL, O’Connor KG, Sharp S, et al. Response rates and response bias for 50 surveys of pediatricians. Health Serv Res. 2005;40:213–26. doi: 10.1111/j.1475-6773.2005.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]