Abstract
Although lithium has been the first line agent in the treatment of bipolar disorder (BD), few studies have evaluated lithium's efficacy in mania with psychosis and its association with later response. Furthermore, given the widespread concern about antipsychotic side effects, answering a question about whether lithium alone can manage to treat both psychotic and non-psychotic mania seems a very relevant one. The present study addresses the antipsychotic efficacy of lithium monotherapy in acute mania and early improvement of psychotic symptoms as a predictor of later response of manic symptoms. Forty-six patients presenting a manic episode (32 with psychotic features and 14 subjects without psychotic features) were treated for 4 weeks with lithium monotherapy and evaluated weekly using the Young Mania Rating Scale (YMRS). Subjects with rapid cycling, substance abuse/dependence, or mixed episodes were excluded. The overall antimanic efficacy of lithium in psychosis vs. non-psychosis groups was evaluated. In addition, early improvement of psychotic symptoms and its prediction of subsequent response (>50% decrease in total YMRS scores) or remission were evaluated. Lithium showed a similar efficacy in both psychosis and non-psychosis mania. Early improvement of psychotic symptoms was associated with clinical response and remission at endpoint.
Keywords: Psychosis, Mania, Bipolar disorder, Lithium, Early improvement, Monotherapy
1. Introduction
Psychotic symptoms are present in about half of the manic episodes in bipolar disorder (BD) (Pope and Lipinski, 1978; Coryell et al., 2001; Keck et al., 2003). Psychosis in BD has been associated with poorer cognitive functioning (Bora et al., 2010), longer periods of active illness (Coryell et al., 2001), and higher relapse rates (Tohen et al., 1990). Although lithium is considered a first line agent for treating acute mania (Yatham et al., 2009), only a few studies have systematically evaluated lithium's efficacy for the treatment of mania with psychosis (Prien et al., 1972; Small et al., 1995; Swann et al., 2004) and none have addressed the time course of action onset. This seems to be mostly due to the widespread practice of combining antipsychotics with mood stabilizer agents within the first weeks of treatment (McElroy et al., 1996), which has been recommended for both psychosis and non-psychosis mania (Goodwin, 2009; Malhi et al., 2009; Yatham et al., 2009).
Few studies have evaluated early improvement in bipolar mania as a predictor of outcome (Houston et al., 2010; Kemp et al., 2011a; Ketter et al., 2010). It has been shown that improvement of psychotic (Ketter et al., 2010) and manic symptoms (Houston et al., 2010; Kemp et al., 2011a) in the first week predicts later response with second-generation antipsychotics. However, only a few predictors of response with lithium are available (Grandjean and Aubry, 2009) and no study has evaluated early improvement of psychotic symptoms with lithium and its potential role as a predictor of later response.
The present study aims to evaluate: 1) lithium's efficacy in mania with psychosis. Results were subsequently compared with a comparison group of concurrently-recruited, mania without psychosis treated with lithium; 2) whether or not lithium induces early improvement of psychotic symptoms, and 3) whether early improvement of psychotic features of mania is associated with later response and remission.
2. Materials and methods
This study is a post-hoc analysis from a larger 4-week, randomized, double-blind, trial in bipolar mania comparing the efficacy of lithium plus placebo vs. lithium plus other drugs (Machado-Vieira et al., 2008). The present analysis is performed in the lithium plus placebo arm of the original trial. Forty-six inpatients, aged 18–65 years, with a diagnosis of manic episode with psychosis (n = 32) or without psychotic features (n = 14; comparison group) by means of the Structured Clinical Interview for Axis I DSM-IV-TR Disorders, Research Version, Patient Version (First et al., 2001) were evaluated. All patients were enrolled between September 2003 and September 2006 at the Bipolar Disorder Research Center, Espirita Hospital of Porto Alegre, Brazil. Subjects were required to present a score of greater than or equal to 22 on YMRS (Young et al., 1978) at baseline. All subjects were in good physical health (determined by medical history, physical examination and blood tests) and free of comorbid substance abuse or dependence for at least 5 weeks prior to screen. Patients had not taken any psychopharmacologic treatment for at least 4 weeks before admission. Other exclusion criteria included rapid cycling, mixed episode, previous history of refractoriness to lithium, or other current axis I psychiatric disorder.
On the first day, patients were started on lithium carbonate 600 mg/day, and subsequent dosage adjustments were allowed at a flexible fashion, aiming to achieve therapeutic levels in the plasma (0.6–1.2 mmol/L), and then adjusted according to clinical improvement. Diazepam up to 20 mg/day was allowed as supplementary medication for agitation during the 4-week study period, except for the day prior to clinical assessment with the YMRS; physical restraint was used when necessary. In accordance with the Declaration of Helsinki, the local institutional review board approved the study and all subjects and/or family members provided written informed consent before entry into the study.
2.1. Outcome measures
Subjects were assessed with the YMRS on a weekly basis from baseline to week 4. Statistical analyses were made for baseline, 1-week, and 4-week (endpoint) measures, using the last observation carried forward (LOCF) or linear mixed model when data were missing. Psychosis in mania was defined as the presence of delusions and hallucinations, i.e., YMRS item-8 (Content) score = 8 (maximum score). Early improvement in psychotic symptoms (early improvers) was defined as improvement of delusions and hallucinations after 1 week of treatment, based on a decrease ≥25% in the YMRS item-8 (Content) score. Clinical response was defined as a decrease of 50% or more in the YMRS at the endpoint (week 4). Remitters were those who had YMRS ≤12 at endpoint. An additional analysis using a more stringent criterion at endpoint (YMRS score ≤7) was also performed.
2.2. Statistical analysis
Demographic and clinical characteristics of psychosis and non-psychosis mania at baseline were compared with the Chi-square test for categorical data. A linear mixed model was used to examine the time course of improvement with lithium treatment in mania with and without psychosis and to compare diazepam use between groups. Also, Student's t test (normal) or Manne-Whitney (non-normal distribution) tests were used for continuous variables. Wilcoxon signed ranks test was used to compare YMRS scores at baseline and endpoint. Spearman test was used to correlate decrease in the YMRS item-8 and total scores. Statistical significance was set at p < 0.05 (two-tailed). All statistical analyses were conducted in the SPSS 16.0 software. In the psychosis mania group, additional analyses were conducted in order to determine the prognostic value of early improvement in psychotic symptoms at week 1 in predicting endpoint (week 4) response or remission. Sensitivity, specificity, and positive and negative predictive values (see Kemp et al., 2011a for further details) were calculated.
3. Results
3.1. Clinical and demographical data
Demographic and clinical data for the psychosis and non-psychosis mania groups are summarized in Table 1. There were no differences between groups except for a larger number of women in the mania without psychosis group.
Table 1.
Demographic variables and clinical characteristics of psychosis and non-psychosis groups compared.
| YMRS item | Psychosis (n = 32) | Non-psychosis (n = 14) | p |
|---|---|---|---|
| Gender | |||
| Male/female, n (%) | 16(50)/16(50) | 1(7)/13(93) | 0.006*,a |
| Age | |||
| Age, year (SD) | 28.8 (8.5) | 30.7 (8.7) | 0.36 |
| Race | |||
| White, n (%) | 27 (84) | 11 (79) | 0.63a |
| Black, n (%) | 5 (15) | 3 (21) | |
| Age at onset, year (SD) | 22.7 (3.9) | 20.9 (3.8) | 0.16b |
| Duration of illness, year (SD) | 8 (7.7) | 7.9 (6.9) | 0.97b |
| Number of mood episodes, year (SD) | 4.5 (3.5) | 5.6 (3.2) | 0.35b |
| Number of manic episodes (SD) | 2.7 (2.2) | 4.1 (3) | 0.06c |
| Type of first episode | |||
| Mania, n (%) | 16 (50) | 9 (64) | 0.65a |
| Depression, n (%) | 12 (37) | 4 (29) | |
| Mixed, n (%) | 4 (13) | 1 (7) | |
| Number of past hospitalizations (SD) | 2.8 (2.7) | 3.5 (3) | 0.52c |
| Suicidal attempts (SD) | 1.6 (2.1) | 0.7 (1.6) | 0.17c |
| Familiar history of bipolar disorder | 16 (50) | 8 (57) | 0.65a |
| Present, n (%) | |||
| Serum lithium at endpoint, mEq/L (SD) | 0.96 (0.2) | 0.93 (0.19) | 0.91c |
| Diazepam use, mg (SD) | 184.7 (122) | 134.3 (127) | 0.81d |
YMRS – Young Mania Rating Scale. SD – standard deviation.
Significantly different.
Chi-square.
Student's T test.
Mann–Whitney test.
Linear mixed model.
3.2. Mania with and without psychosis has similar severity and also similar improvement with lithium treatment
YMRS total scores did not show significant differences between mania with and without psychosis (F = 0.27, df 1, 42, p = 0.87), nor significant interaction between group and time (F = 1.16, df = 3, 110, p = 0.33) (Fig. 1). When baseline was included as a time point in the mixed model, also no significant difference between YMRS total scores of mania with and without psychosis was found (F = 1.76, df = 1, 46, p = 0.19) and no significant interaction between group and time (F = 0.88, df = 4, 151, p = 0.48). There were no significant differences between psychosis and non-psychosis groups in YMRS single items, except for greater YMRS-item 11 scores in the psychosis group (data not shown).
Fig. 1.
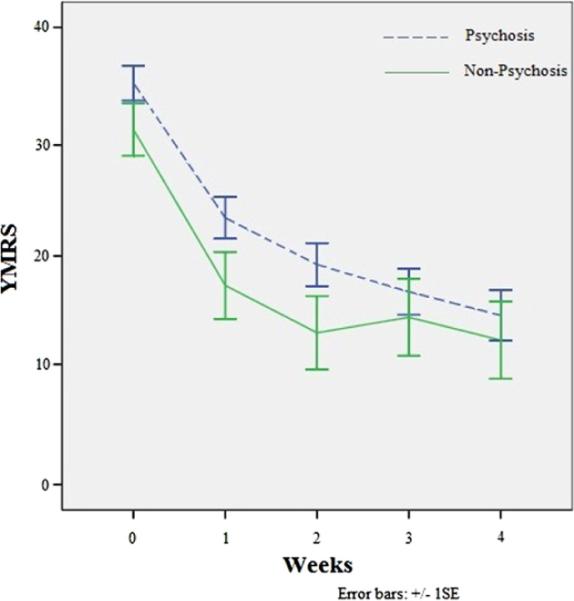
Course of overall manic symptoms (total YMRS) with lithium treatment in psychosis and non-psychosis mania.
Since there was a significant gender difference between psychosis and non-psychosis groups, additional linear mixed model analyses were performed in female patients and showed no significant differences in YMRS total scores between psychosis and non-psychosis groups, respectively (F = 0.21, df = 1, 27, p = 0.65 and F = 1.2, df = 1, 30, p = 0.28) and no significant interaction between group and time (F = 0.86, p = 0.46; F = 0.73 p = 0.57). Diazepam use and side effects were not significantly different between psychosis and non-psychosis groups (data not shown).
Lithium treatment was associated with a significant improvement of manic symptoms in the psychosis group from baseline to endpoint (YMRS: 35.1 ±8.6 vs. 14.8 ± 12.5, respectively, p < 0.001). At endpoint, in the psychosis mania group (n = 32), 63% achieved clinical response, and 50% remitted (YMRS ≤ 12). Also, 34% remitted using more stringent criteria (YMRS ≤ 7). In the non-psychosis group (n = 14), lithium also showed a significant improvement of manic symptoms from baseline to endpoint (YMRS: 31 ± 8.6 vs. 12.6 ± 12.7, respectively, p = 0.002). Sixty four percent showed both response and remission (YMRS ≤ 12) at the endpoint, while half of patients presented remission accordingly to the more stringent criteria.
Changes from baseline to endpoint of psychotic symptoms in YMRS item-8 (Content) correlated with improvement of YMRS total scores (p < 0.001) in psychotic mania (Fig. 2).
Fig. 2.
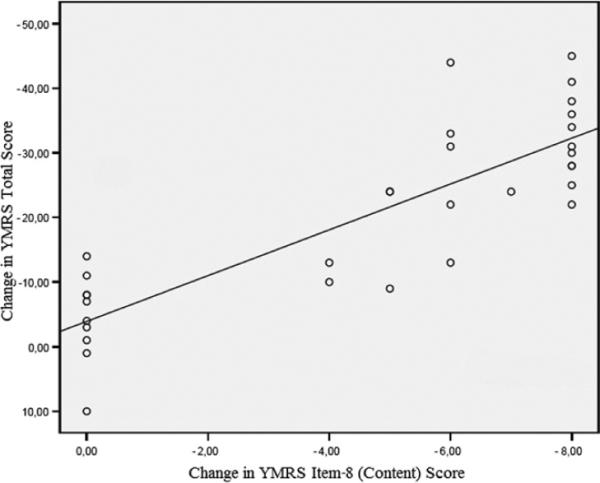
Relationship between change in YMRS item-8 (content) and YMRS total scores from baseline to endpoint in psychotic Mania. YMRS – Young Mania Rating Scale.
3.3. Early improvement in psychotic symptoms predicts later response and remission
Sixteen (50%) subjects in psychosis mania group presented an early improvement of delusions and hallucinations after one week of lithium treatment. Among early improvers, 15 achieved clinical response (PPV = 94%), 12 remitted (PPV = 75%, YMRS ≤ 12), and 8 presented remission (PPV = 50%) at endpoint with a more stringent criteria (YMRS ≤ 7) (Table 2). Among the 16 patients having no early improvement in psychotic symptoms after one week of treatment, 11 did not respond (NPV = 69%), 12 did not have remission (NPV = 75%, YMRS<13), while 13 failed to achieve remission with a more stringent criteria (NPV = 81%) at endpoint. Sensitivity, specificity, and positive and negative predictive values are summarized in the Table 2.
Table 2.
Analyses of early improvement in psychotic symptoms (delusions and hallucinations within the first week) in the psychosis group as a predictor of endpoint outcome.
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
|---|---|---|---|---|
| Response | 75 | 92 | 94 | 69 |
| Remission (YMRS ≤ 12) | 75 | 75 | 75 | 75 |
| Remission (YMRS ≤ 7) | 73 | 62 | 50 | 81 |
Values displayed as percentages. YMRS – Young Mania Rating Scale. Response is defined as ≥50% improvement in YMRS total score from baseline to endpoint.
4. Discussion
Lithium monotherapy showed similar efficacy in both mania with and without psychosis in patients without rapid cycling or mixed states. To the best of our knowledge, this is the first study showing that early improvement of psychotic symptoms predicts later outcome with lithium monotherapy. Our results are in line with other studies showing the efficacy of lithium or divalproex monotherapy (Swann et al., 2004), and lithium plus carbamazepine (Small et al., 1995) for treating psychotic symptoms in mania.
Specifically, the response rates found in our study for both psychosis (63%) and non-psychosis mania (64%) are slightly higher than those observed in previous studies with lithium monotherapy. Improvement of psychotic symptoms in bipolar mania with lithium monotherapy was studied by Swann et al. (2002), who found lithium treatment significantly better than placebo for improving mania in a psychotic subtype (derived from a previous cluster analysis). In addition, lithium was compared to first and second-generation neuroleptics in mania with psychosis. Prien et al. (1972) found chlorpromazine superior to lithium in suspiciousness measured by Brief Psychiatric Rating Scale (BPRS) and Keck et al. (2009) found aripiprazole, but not lithium, more effective than placebo in psychotic symptoms by Positive and Negative Syndrome Scale (PANSS) scale. Bowden et al. (2005) found lithium and quetiapine similarly effective and superior to placebo in the treatment of psychosis by PANSS positive subscale. In summary, the different results found may be explained by the use of different methodology and scales to compare lithium and antipsychotics for treating mania with psychosis.
In the present study, lithium monotherapy produced early improvement of psychotic symptoms in half of the patients after 1-week treatment. Early improvement of psychotic symptoms (delusions and hallucinations) in the first week of treatment yielded high specificity and positive predictive value for later clinical response at endpoint (week 4). Likewise, Ketter et al. (2010) found that early improvement (i.e., improvement after 4 days) on ziprasidone predicted remission at 21 days according to the Schedule for Affective Disorders and Schizophrenia-Change (SADS-C). Another study looked at early improvement of manic symptoms but did not evaluate improvement of psychosis. Kemp et al. (2011a) found that patients without improvement in overall manic symptoms at week 1 (<25% decrease in YMRS total score) with risperidone and olanzapine were less likely to reach response and remission at week 3.
Furthermore, our results are in agreement with other studies in different psychiatric conditions. Early improvement was found to predict later outcome in studies with atypical antipsychotics in schizophrenia (Kinon et al., 2008), antidepressants in unipolar depression (Szegedi et al., 2009), and mood stabilizers and atypical antipsychotics in bipolar depression (Kemp et al., 2011b).
Limitations include the exclusion of subjects with mixed episodes and rapid cycling, gender differences between psychosis and non-psychosis groups, and the lack of a specific rating scale for quantifying psychotic symptoms (e.g., BPRS, PANSS).
In conclusion, lithium monotherapy showed similar efficacy in both mania with and without psychosis.
To our knowledge, this is the first report to describe early improvement of psychotic symptoms having a high positive predictive value and significant specificity for later response with lithium therapy. The present findings reinforce the role of lithium in the treatment of classic mania with psychotic features as well as the importance of assessing improvement of psychosis in the first week of treatment as a predictor of subsequent outcome. Further studies are necessary to confirm these preliminary findings.
Acknowledgments
This work was supported by a grant from the Stanley Medical Research Institute, 03T-356 to RMV. The authors gratefully acknowledge the staff and patients of the Espirita Hospital of Porto Alegre and B. dos Santos, Drs CI Viale, JR Hecktheuer and F Kapczinski.
Role of the funding source This work was supported by a grant from the Stanley Medical Research Institute (03T-356 to RMV), which had no role in study design or data analysis.
Footnotes
Contributors All authors contributed to manuscript writing or data analysis, and agreed to submit the final version for publication.
Conflict of interest None of the authors in this study have a possible conflict of interest, financial or otherwise.
References
- Bora E, Yücel M, Pantelis C. Neurocognitive markers of psychosis in bipolar disorder: a meta-analytic study. Journal of Affective Disorders. 2010;127:1–9. doi: 10.1016/j.jad.2010.02.117. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Grunze H, Mullen J, Brecher M, Paulsson B, Jones M, et al. A randomized, double-blind, placebo-controlled efficacy and safety study of quetiapine or lithium as monotherapy for mania in bipolar disorder. Journal of Clinical Psychiatry. 2005;66:111–21. doi: 10.4088/jcp.v66n0116. [DOI] [PubMed] [Google Scholar]
- Coryell W, Leon AC, Turvey C, Akiskal HS, Mueller T, Endicott J. The significance of psychotic features in manic episodes: a report from the NIMH collaborative study. Journal of Affective Disorders. 2001;67:79–88. doi: 10.1016/s0165-0327(99)00024-5. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV TR axis I disorders, research version, patient edition (SCID-I/P) New York State Psychiatric Institute; New York: 2001. Biometrics Research. [Google Scholar]
- Goodwin GM, Consensus Group of the British Association for Psychopharmacology Evidence-based guidelines for treating bipolar disorder: revised second edition – recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology. 2009;23:346–88. doi: 10.1177/0269881109102919. [DOI] [PubMed] [Google Scholar]
- Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part I: clinical efficacy in bipolar disorder. CNS Drugs. 2009;23:225–40. doi: 10.2165/00023210-200923030-00004. [DOI] [PubMed] [Google Scholar]
- Houston JP, Gatz JL, Degenhardt EK, Jamal HH. Symptoms predicting remission after divalproex augmentation with olanzapine in partially nonresponsive patients experiencing mixed bipolar I episode: a post-hoc analysis of a randomized controlled study. BMC Research Notes. 2010;3:276. doi: 10.1186/1756-0500-3-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keck PE, Jr, McElroy SL, Havens JR, Altshuler LL, Nolen WA, Frye MA, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Comprehensive Psychiatry. 2003;44:263–9. doi: 10.1016/S0010-440X(03)00089-0. [DOI] [PubMed] [Google Scholar]
- Keck PE, Orsulak PJ, Cutler AJ, Sanchez R, Torbeyns A, Marcus RN, et al. CN138–135 Study Group. Aripiprazole monotherapy in the treatment of acute bipolar I mania: a randomized, double-blind, placebo- and lithium-controlled study. Journal of Affective Disorders. 2009 Jan;112:36–49. doi: 10.1016/j.jad.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Kemp DE, Johnson E, Wang WV, Tohen M, Calabrese JR. Clinical utility of early improvement to predict response or remission in acute mania: focus on olanzapine and risperidone. Journal of Clinical Psychiatry. 2011a;72:1236–41. doi: 10.4088/JCP.09m05874yel. [DOI] [PubMed] [Google Scholar]
- Kemp DE, Ganocy SJ, Brecher M, Carlson BX, Edwards S, Eudicone JM, et al. Clinical value of early partial symptomatic improvement in the prediction of response and remission during short-term treatment trials in 3369 subjects with bipolar I or II depression. Journal of Affective Disorders. 2011b;130:171–9. doi: 10.1016/j.jad.2010.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketter TA, Agid O, Kapur S, Loebel A, Siu CO, Romano SJ. Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. Journal of Psychiatric Research. 2010;44:8–14. doi: 10.1016/j.jpsychires.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Kinon BJ, Chen L, Ascher-Svanum H, Stauffer VL, Kollack-Walker S, Sniadecki JL, et al. Predicting response to atypical antipsychotics based on early response in the treatment of schizophrenia. Schizophrenia Research. 2008;102:230–40. doi: 10.1016/j.schres.2008.02.021. [DOI] [PubMed] [Google Scholar]
- Machado-Vieira R, Soares JC, Lara DR, Luckenbaugh DA, Busnello JV, Marca G, et al. A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. Journal of Clinical Psychiatry. 2008;69:1237–45. doi: 10.4088/jcp.v69n0806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi GS, Adams D, Lampe L, Paton M, O'Connor N, Newton LA, et al. Northern Sydney Central Coast mental health drug & alcohol; NSW Health Clinical Redesign Program; CADE Clinic, University of Sydney. Clinical practice recommendations for bipolar disorder. Acta Psychiatrica Scandinavica. 2009;439(Supplementum):27–46. doi: 10.1111/j.1600-0447.2009.01383.x. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Keck PE, Jr, Strakowski SM. Mania, psychosis, and antipsychotics. Journal of Clinical Psychiatry. 1996;57(Suppl. 3):14–26. [PubMed] [Google Scholar]
- Pope HG, Jr, Lipinski JF., Jr Diagnosis in schizophrenia and manic-depressive illness: a reassessment of the specificity of `schizophrenic' symptoms in the light of current research. Archives of General Psychiatry. 1978;35:811–28. doi: 10.1001/archpsyc.1978.01770310017001. [DOI] [PubMed] [Google Scholar]
- Prien RF, Caffey EM, Jr, Klett CJ. Comparison of lithium carbonate and chlorpromazine in the treatment of mania. Report of the Veterans Administration and National Institute of Mental Health collaborative study group. Archives of General Psychiatry. 1972;26:146–53. doi: 10.1001/archpsyc.1972.01750200050011. [DOI] [PubMed] [Google Scholar]
- Small JG, Klapper MH, Marhenke JD, Milstein V, Woodham GC, Kellams JJ. Lithium combined with carbamazepine or haloperidol in the treatment of mania. Psychopharmacological Bulletin. 1995;31:265–72. [PubMed] [Google Scholar]
- Szegedi A, Jansen WT, van Willigenburg AP, van der Meulen E, Stassen HH, Thase ME. Early improvement in the first 2 weeks as a predictor of treatment outcome in patients with major depressive disorder: a meta-analysis including 6562 patients. Journal of Clinical Psychiatry. 2009;70:344–53. doi: 10.4088/jcp.07m03780. [DOI] [PubMed] [Google Scholar]
- Swann AC, Bowden CL, Calabrese JR, Dilsaver SC, Morris DD. Pattern of response to divalproex, lithium, or placebo in four naturalistic subtypes of mania. Neuropsychopharmacology. 2002 Apr;26:530–6. doi: 10.1016/S0893-133X(01)00390-6. [DOI] [PubMed] [Google Scholar]
- Swann AC, Daniel DG, Kochan LD, Wozniak PJ, Calabrese JR. Psychosis in mania: specificity of its role in severity and treatment response. Journal of Clinical Psychiatry. 2004;65:825–9. doi: 10.4088/jcp.v65n0614. [DOI] [PubMed] [Google Scholar]
- Tohen M, Waternaux CM, Tsuang MT. Outcome in Mania. A 4-year prospective follow-up of 75 patients utilizing survival analysis. Archives of General Psychiatry. 1990;47:1106–11. doi: 10.1001/archpsyc.1990.01810240026005. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, Schaffer A, Parikh SV, Beaulieu S, O'Donovan C, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disorders. 2009;11:225–55. doi: 10.1111/j.1399-5618.2009.00672.x. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. British Journal of Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]


