Abstract
Objective
The aim of the study is to evaluate the usage of Dieffenbach’s modification of Weber–Fergusons approach in the treatment of lesions involving maxilla.
Study
In this study five different maxillary pathologies were approached through Dieffenbach’s modification of Weber–Fergusons approach. Partial and subtotal procedures were performed depending on the type of pathology and the extent of the lesion which was assessed both clinically and radiologically. The study evaluates the easy exposure of the site, post operative complications like scar formation and infra orbital nerve parasthesia.
Results
There were two subtotal maxillectomy procedures and three partial maxillectomy procedures approached through Dieffenbach’s modification of Weber–Fergusson’s approach. All the cases recovered well in the post operative healing period without noticeable scarring. There was parasthesia in three cases which subsided in 3 months.
Conclusion
The approach through Dieffenbach’s modification of Weber–Fergusons incision gave better visibility and accessibility to the lesions of maxilla. Because there is direct access to the pathology, the inadvertent resection of the un-involved structures is prevented thus minimizing the morbidity.
Keywords: Dieffenbach’s modification, Weber–Fergusson’s approach, Scarring, Parasthesia
Introduction
Out of many approaches to the maxillary region, the commonly used approaches are the Weber–Fergusson’s incision [1] and the Midface deglowing incision, [2]. A controversy exists regarding who described the incision first. Few authors consider it was first described by Gensoul 1893 later the technique was popularized by Weber & Fergusson. The others argue that it was first described by Weber in the German literature and was later modified by Fergusson in the English literature [3]. And some people believe that Sir William Fergusson was the person who described the technique and Weber. O has described the mandibular procedure. However the standard technique underwent various modifications depending on the extent of the tumor. This paper discusses the Dieffenbach’s modification of Weber Fergusson’s incision for treating maxillary pathologies and evaluates the surgical exposure to the lesion, post operative complications like scar formation and infraorbital nerve parasthesia.
Materials and Methods
The study included five cases of maxillary pathologies which were treated with Dieffenbach’s modification of Weber–Fergusson’s incision. The group consisted of 4 females and 1 male between 15 and 45 years of age. Demographic data was collected and the chief complaint was noted in the detailed case history. The incision biopsy was made prior to surgery. The cases were followed up to 18–24 months. The parameters considered in the study are formation of hypertrophic scar in the incision line, alar bulging which was compared with the normal side, ectropion, telecanthus, lower eye lid edema and parasthesia. The demographic data and the diagnosis were mentioned in the Table 1
Table 1.
Demographic data
| S. no | Age/sex | Diagnosis | Treatment |
|---|---|---|---|
| 1 | 45/F | Osteomyelitis | Subtotal maxillectomy |
| 2 | 28/F | CEOT | Partial maxillectomy |
| 3 | 15/F | Basal cell variant Ameloblastoma | Partial maxillectomy |
| 4 | 28/F | Cemento ossifying fibroma | Subtotal maxillectomy |
| 5 | 32/M | Ossifying fibroma | Partial maxillectomy |
Technique
Transfacial approaches incorporating lip splits attempt to use anatomical landmarks and good principles of incision design to hide the resultant scar line. However, the commonly used straight line incision across the lip skin and vermilion margin can be the most obvious section of the final scar, clearly indicating the surgical approach used [4].
The first step in the Weber–Fergusson’s incision is to mark the incision line on the face which begins as a vertical incision which is made through the upper lip in the philtrum from the nasolabial groove to the vermillion border. Lower end is extended to the midline and then vertically in the midline through the buccal mucosa to the gingivobuccal gutter. Upper lip is divided and labial arteries may be ligated. External skin incision is extended transversely from the upper end of the lip incision in the nasolabial groove to beyond the nasal ala and then superiorly along the nasofacial groove to the lower eyelid. The lateral nasal incision should be raised and placed in the nasal side wall at the junction of the nasal subunit. Once the medial canthal region is approached, the incision may be extended laterally inferior to the lower eyelid in one of the creases which is called the Dieffenbach’s modification. For better postoperative cosmesis, Hernandes Altemir [4] suggested a modification to the incision, in which the straight line incision in the lip is moved from the midline and placed on the philtrum.
Here we demonstrate two cases where the Dieffenbach’s modification of Weber Fergusson’s incision was used for the resection of the pathology.
Results
All the five cases were successfully treated with negligible scar in 4 of the cases and only one case had a scar in the operated site. Paraesthesia was present in 3 of the cases after the operation and it was cured within 6 months of the post operative follow up period. The results of these parameters are tabulated Table 2
Table 2.
Results
| S. no | Parameter | No of cases |
|---|---|---|
| 1 | Hypertrophic scar | 1 |
| 2 | Alar bulging | 0 |
| 3 | Ectropion | 0 |
| 4 | Telecanthus | 0 |
| 5 | Lower eye lid edema | 1 |
| 6 | Recurrence | 0 |
| 7 | Parasthesia | 3a |
aParasthesia was noted for 3 months in 2 patients and in 1 patient it lasted only for 1 month. During 6 months follow up, all the patients were recovered of the parasthesia
Discussion
Out of many reasons existing for the exposure of facial skeleton, surgical pathology remains to be the challenging task to approach. The choice of the approach is based not only on the extent of the lesion, and it’s the characteristics but also varies greatly with the skills, experience, bias and training of the surgeon and finally the patient’s choice. (Figs. 1, 2).
Fig. 1.
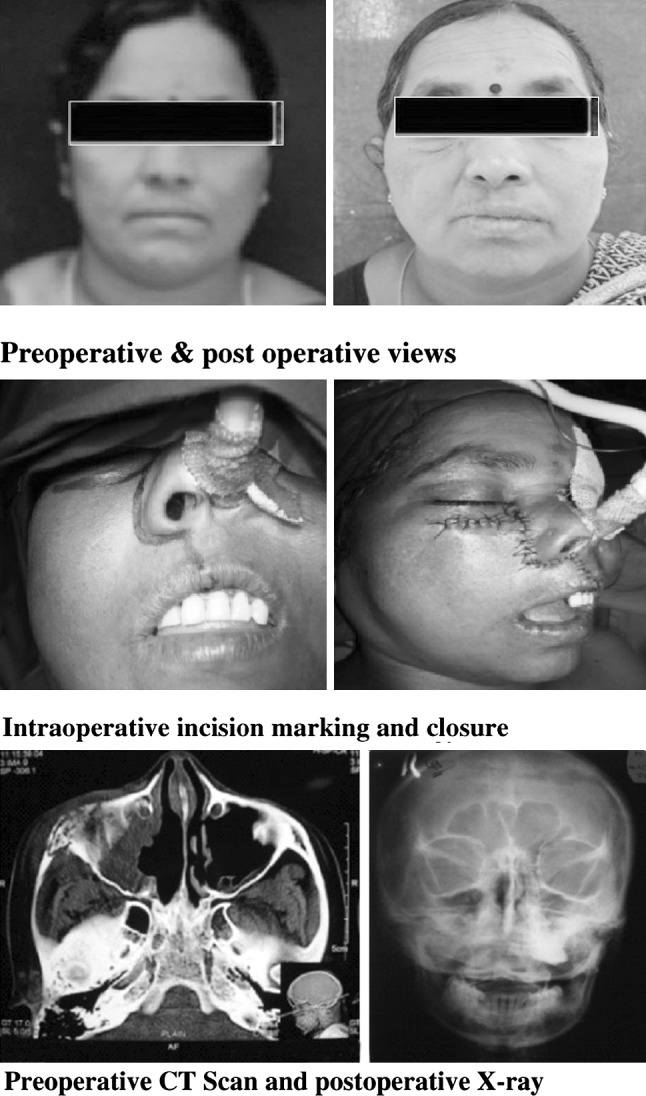
Case 1. Osteomyelitis of the maxilla
Fig. 2.
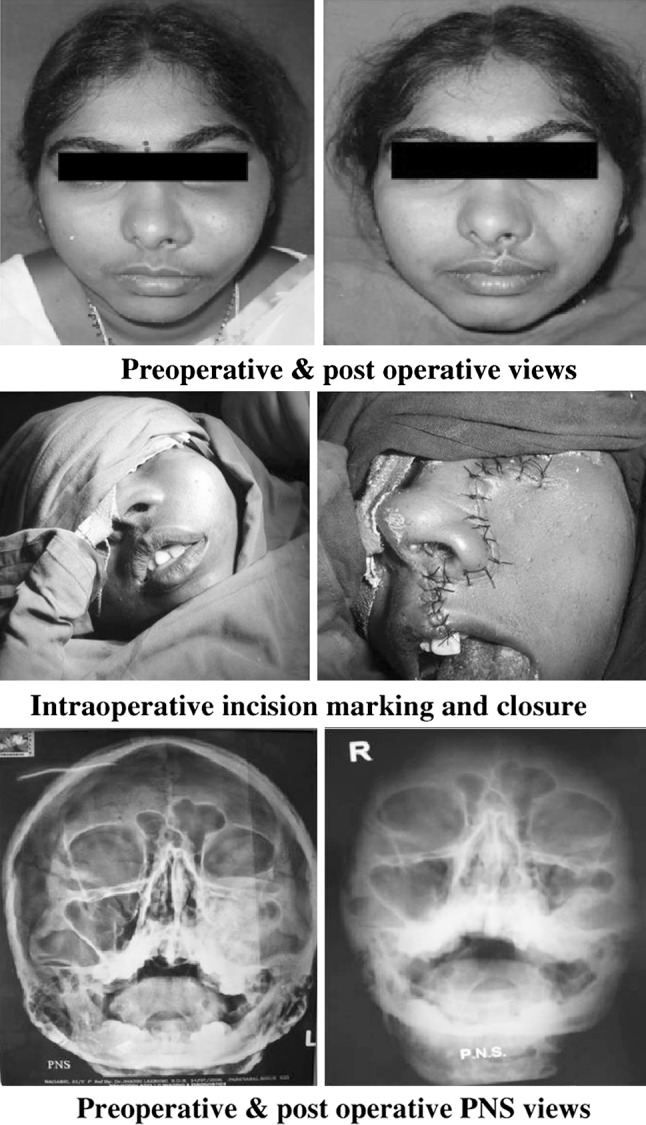
Case 2. Calcifying epithelial odontogenic tumor
The classical Weber–Fergusson’s approach may be modified depending on the extent and nature of the tumor. Once the medial canthal region is approached, the incision may be extended laterally inferior to the lower eyelid in one of the creases as in the Dieffenbach’s modification Fig. 3 or extended superiorly into a Lynch incision [5]. The incision is extended from the lateral canthus of the eye to the temporal region in the shape of a “question mark” when the reconstruction of the maxillectomy defect is planned with a temporalis muscle flap this is known as Borle’s extension. [6]. Infraorbital orbitotomy may be performed for the protection of the infraorbital neurovascular bundle during the surgical procedure [7]. Weber–Fergusson and lateral rhinotomy approaches provide excellent surgical access; however, they require a facial incision and lip split which is undesirable, particularly for extirpation of benign tumors [8]. Sometimes it may be combined with craniotomy for the intracranial extensions of the tumor [9]. Transpalatal approach may be combined with the Weber–Fergusson approach for massive nasopharyngeal tumors [10]. The upper lip split displays the maxilla and the maxilla may be swinged laterally through this approach. When the maxilla is pedicled to the cheek flap and swung laterally, the paranasal sinuses, the nasopharynx and the base of skull become readily accessible [11, 12]. The final cosmetic result is optimized by restoring the normal anatomical position of the maxilla and mandible with stable fixation and careful approximation of the soft tissues. The Dieffenbach’s modification of Weber–Fergusson’s approach may be combined with a lip-splitting mandibulotomy approach so that the posterior aspect of the tumor can be resected in a more direct fashion or the mandibulotomy can be performed alone [13].
Fig. 3.
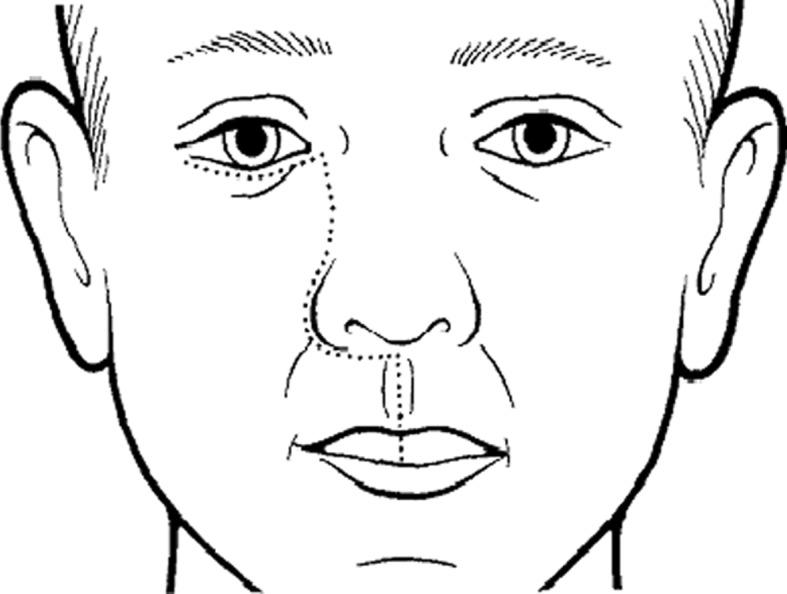
Dieffenbach’s modification of Weber Fergusson’s approach [4]
Dieffenbach’s modification of Weber–Fergusson’s approach provides a very good exposure of the maxillary region. This incision gives more direct access to the maxilla and allows for more unimpeded resection of tumors. This approach will avoid resection of the uninvolved structures owing to its direct access to the pathologies of the maxilla. The approach is more flexible with relatively minimum number of complications such as scar formation and lymphedema.
Hypertrophic scarring (Fig. 4) usually occurs within 4–8 weeks as a result of aberrations of physiologic wound healing eventually leading to flat scars with no further symptoms. Various factors influencing the hypertrophic scar formation include severity and the type of inflammatory response, fibrogenic response, excessive collagen formation and the genetic factors. Histologically, hypertrophic scars contain primarily type III collagen oriented parallel to the epidermal surface with abundant nodules containing myofibroblasts, large extracellular collagen filaments and plentiful acidic mucopolysaccharides [14]. Proper handling of the soft tissues suturing with less tension minimizes the scar formation.
Fig. 4.
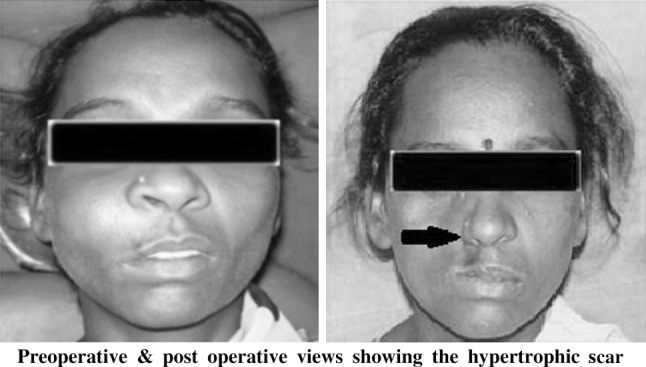
Preoperative and post operative views showing the hypertrophic scar
Care is to be taken to spare angular vein while placing the incision at the medial canthal ligament and also the lymphatic channels draining from the lateral parts of the eye are spared. The post operative facial fullness is not achieved due to resection of the maxillary pathology which is to be reconstructed with obturator. But the main disadvantage of the Dieffenbach’s modification of Weber Fergusson’s approach is that, it does not provide a better exposure to the tumors of cranial base and nasopharyngeal tumors and the tumors involving posterior wall of sinus, pterygoid process and pterygoid muscle [15].
Conclusion
Several approaches have been proposed for resection of tumors of maxilla. But each of them has got inherent advantages and disadvantages. Avoiding damage to vital structures and ease of operating technique remains the objectives of successful treatment which can be achieved with Dieffenbach’s modification of Weber-Fergusson’s approach. This approach provides better visibility and direct access to the tumor thus preventing the inadvertent resection of the uninvolved vital structures. This approach is very flexible and is suitable for the treatment of complex pathologies of mid face region. Adhering to the basic principles, good planning, execution of osteotomies and careful handling of the soft tissues will minimize the complications.
References
- 1.Chiodo AA, Strumas N, Gilbert RW, Birt BD. Management of odontogenic myxoma of the maxilla. Otolaryngol Head Neck Surg. 1997;117(6):S93–S96. doi: 10.1016/S0194-5998(97)70062-7. [DOI] [PubMed] [Google Scholar]
- 2.Zaghloul AS, Nouh MA, Fatah HA. Midfacial degloving approach for malignant maxillary tumors. J Egypt Natl Canc Inst. 2004;16(2):69–75. [PubMed] [Google Scholar]
- 3.Fernandes R, Ord R. Access surgery for oral cancer. Oral Maxillofac Surg Clin North Am. 2006;18:565–571. doi: 10.1016/j.coms.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Hayter JP, Vaughan ED, Brown JS. Aesthetic lip splits. Br J Oral Maxillofac Surg. 1996;34:432–435. doi: 10.1016/S0266-4356(96)90102-3. [DOI] [PubMed] [Google Scholar]
- 5.Carol R. Bradford and Mark E. Prince (2004) ACS Surgery, principles & Practice, Head and neck, Oral cavity procedures
- 6.Rai A, Bhola N, Datarkar A, Borle R. Modified Weber–Fergusson incision with Borle’s extension. Br J Oral Maxillofac Surg. 2010;48:e23–e24. doi: 10.1016/j.bjoms.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Andi KA, Holmes SB, Hutchison IL. Infraorbital orbitotomy: modification of the Weber–Ferguson approach. Br J Oral Maxillofac Surg. 2010;48:44–45. doi: 10.1016/j.bjoms.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Kademani D. Le Fort maxillary swing procedure for posterior maxilla tumor extirpation. J Oral Maxillofac Surg. 2007;65:1055–1058. doi: 10.1016/j.joms.2005.12.044. [DOI] [PubMed] [Google Scholar]
- 9.Pai SB, Harish K, Venkatesh MS, Udayshankar, Jermely D. Ethmoidal osteoid osteoma with orbital and intracranial extension—a case report. BMC Ear Nose Throat Disord. 2005;5(2):1–6. doi: 10.1186/1472-6815-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saha S, Saha VP, Chattopadhyay S. Orbital and para orbital tumors–clinicopathological profile and surgical management. Indian J Otolaryngol Head Neck Surg. 2002;54(2):117–122. doi: 10.1007/BF02968729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hassan S, Abdullah J, Abdullah B, Shah Jihan WD, Jaafar H, Abdullah S. Appraisal of clinical profile and management of juvenile nasopharyngeal angiofibroma in Malaysia. Malays J Med Sci. 2007;14(1):18–24. [PMC free article] [PubMed] [Google Scholar]
- 12.Honda K, Asato R, Tanaka S, Endo T, Nishimura K, Ito J. Vidian nerve schwannoma with middle cranial fossa extension resected via a maxillary swing approach. Head Neck. 2008;30(10):1389–1393. doi: 10.1002/hed.20793. [DOI] [PubMed] [Google Scholar]
- 13.Nair S, Sridhar KR, Shah A, Kumar B, Nayak K, Shetty P. Maxillectomy through mandibulotomy—a retrospective clinical review. J Oral Maxillofac Surg. 2011;69(7):2040–2047. doi: 10.1016/j.joms.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 14.Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Mol Med. 2011;17(1–2):113–125. doi: 10.2119/molmed.2009.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Umeda M, Minamikaw T, Komatsubara H, Ojima Y, Shibuya Y, Yokoo S, Komori T. En bloc resection of the primary tumour and cervical lymph nodes through the parapharyngeal space in patients with squamous cell carcinoma of the maxilla: a preliminary study. Br J Oral Maxillofac Surg. 2005;43:17–22. doi: 10.1016/j.bjoms.2004.10.003. [DOI] [PubMed] [Google Scholar]


