Abstract
Background
Osteomas are benign neoplasm often associated with facial asymmetry, pain and surface ulceration. Peripheral osteomas are more common in the cranio-maxillofacial region. It is prevalent at younger age but maximum seen in the sixth decade, with a female to male ratio is 1:2. The aim of this study was to review the clinical presentations and management protocol of such lesions in cranio-maxillofacial region.
Materials and Methods
The study was conducted at Command Military Dental Centre (EC) during May 2004 to May 2007. Six serving soldiers and their families (four males, two females), age group ranging between 13 and 56 years, mean age 34.5 years were recruited in this study. The tumors were excised using extra oral, intra oral and combined approaches; no complications were reported during post op period.
Results
All the cases were operated under GA through extra oral, intra oral and combined approaches with satisfactory results. HPE report was benign in all our cases with no post operative complications reported during follow up.
Conclusion
Cranio-maxillofacial osteomas are exclusively benign tumors and not very common entities. Proper diagnosis and precision management alleviates symptoms without any post surgical complications. In our series of six cases the tumors were diagnosed and managed as per standard surgical protocol with excellent result.
Keywords: Osteoma, Benign, Surgical excision
Introduction
Osteoma is a benign neoplasm characterized by proliferation of either compact or cancellous bone usually in an endosteal or periosteal location. It can be central, peripheral, or extra skeletal. Central osteomas arise from the endosteum, peripheral osteoma from the periosteum, and extraskeletal soft tissue osteoma within a muscle [1]. Osteomas are exclusively found in membranous bones such as skull, facial, and jaw bones. Though asymptomatic in most cases, it is often associated with swelling, facial asymmetry and pain. In the jawbones, the majority of solitary osteomas reported in the literature have been of the peripheral variant, involving the mandible more often than the maxilla. Although osteomas are more common in young adults, it can be noted at any age and children are almost never affected unless they have Gardner syndrome. There is no sex predilection but men seem to be affected more frequently than women [2, 3].
Peripheral osteomas typically present as mushroom shaped hard radiopaque masses which are often pedunculated but may also have a broad-base by which they are attached to the cortical plates. The lesion is usually slow growing. Peripheral osteomas in most cases are fairly easy to recognize and diagnose, because of their unique presentation as radiopaque masses protruding from the periphery of the jawbone [4]. The etiology of these lesions remain unclear. The possibility of reactive mechanism, triggered by trauma [5], infection or muscle traction has been suggested.
Multiple peripheral osteomas with impacted supernumerary teeth of the jaws are typical in Gardner syndrome, as well as multiple central radiopaque lesions, which resemble exostosis or dense bone islands rather than central osteoma, because they seldom if ever cause expansion or continue to grow [6, 7]. The purpose of this article was to review the clinical presentations and management protocol of such lesions and analysis of the literature.
Materials and Methods
Six cases (four males and two females) of army personnel and their families were included in this study. Age group ranges between 13 and 56 years with an average age of 34.5 years. All the patients had reported with complaints of facial asymmetry as common findings (Fig. 1). Pain, surface ulceration, limitation of mouth opening, sinusitis and difficulty in speech were reported as per the location of tumors in the study sample. The size of the lesions in their greatest diameter ranged from 1 to 4 cm with a mean of 1.86 cm. The average duration of lesion was 6 months to 2 years.
Fig. 1.

Swelling at angle of mandible (L)
Routine evaluation of other long bones of the body did not show any abnormality in any of our cases. Two of our cases who presented with multiple supernumerary teeth were investigated for colorectal polyp and the colonoscopy findings were negative. Pre anesthetic check up was done as per protocol and all the patients were operated under GA. Three cases were managed through extra oral submandibular approach; two were operated via intra oral vestibular approach (Cald-Well-Luc for maxillary sinus), whereas one case was dealt with both extra oral as well as intra oral approach. Complete excision as one piece or by sectioning as per requirement of cases was performed to avoid recurrence and jaw fracture. Excised specimen was sent routinely for HPE. Residual bone smoothening, wound toileting with copious saline irrigation was done and vacuum drain was placed as per indication. Tissues closed in layers. Antibiotics were administered as per institute protocol and average period of hospitalization was for 5–7 days. All the cases were followed up for an average period of 2 years.
Results
Six patients with peripheral osteoma (PO) were included in the study. The clinical features are tabulated in Table 1. Five patients had lesion in mandible and one in the maxillary sinus. Radiographic findings in routine radiographs and CT scan showed well circumscribed radio-opaque mass in all our cases (Fig. 2). No soft tissue spread was seen in any of our cases. The most common indication of surgery was facial asymmetry. Colonoscopy was performed in two cases and the results were negative. Surgical excision was performed in the cases through extra oral (Fig. 3), intra oral and a combination of extra oral and intra oral approaches. Excision was done using high speed saw and bur. The histological picture in our cases was mature bone which was either compact, cancellous or a combination of both (Fig. 6). Two cases with supernumerary teeth were referred for evaluation of Gardner’s syndrome and the results were negative. There were no post surgical complications or recurrence reported in our cases during periodic clinico-radiological follow up for an average period of 2 years (Fig. 4, 5).
Table 1.
Clinical data of patients with osteomas in the maxillofacial region
| Patient | Age (years)/sex | Location | Size (cm) | Clinical Symptoms |
|---|---|---|---|---|
| 1. | 13/M | Mandible body (R) lingual side, floor of mouth. | 2 | Difficulty in speech & deglutition, recurrent mucosal ulcers. |
| 2. | 45/M | Mandible body (L) in the lower border | 2.5 | Facial asymmetry, pain |
| 3. | 39/M | Mandible angle (L) | 3 | Facial asymmetry, pain reduction in mouth opening |
| 4. | 25/F | Maxillary sinus (R) | 1 | Pain, sinusitis. |
| 5. | 29/F | Mandible body (L) buccal surface | 3.5 | Facial asymmetry, local sensitivity. |
| 6. | 56/M | Angle of Mandible (L) | 4 | Facial asymmetry, limited mouth opening & local sensitivity. |
Fig. 2.
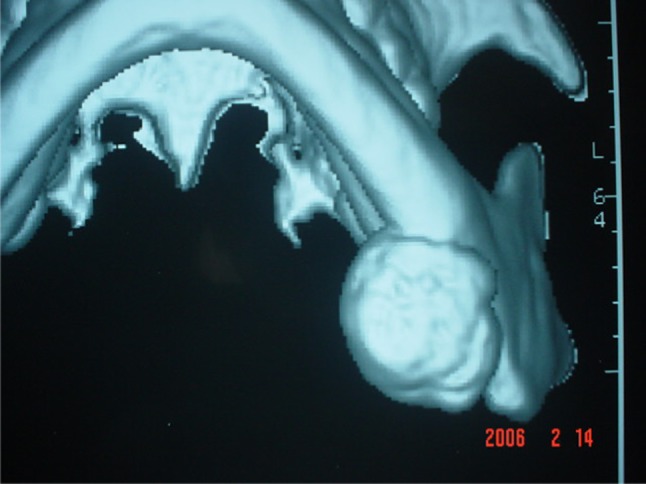
3-D reformatted view of the tumour
Fig. 3.
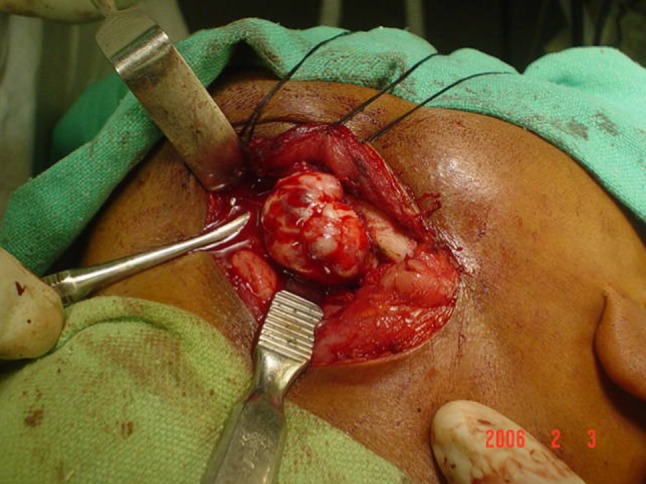
Extra-oral exposure
Fig. 6.
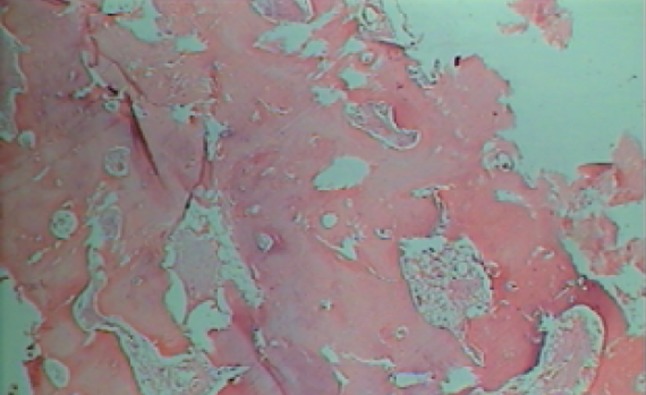
Histopathological view
Fig. 4.

Post-op view
Fig. 5.
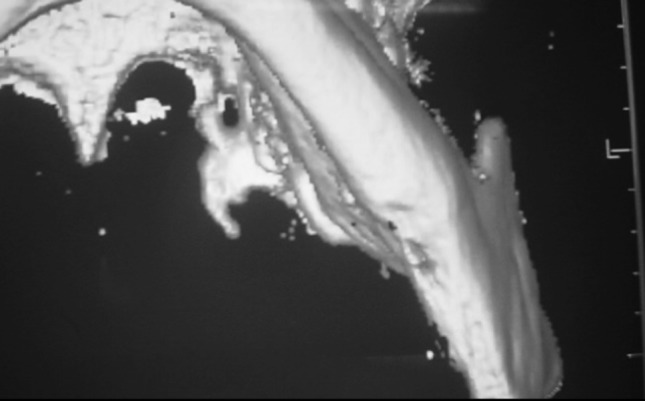
3-D post-op view
Discussion
Osteomas are often referred to as benign osteogenic lesions [4] arising from compact or cancellous bone. Clinically they appear circumscribed, usually rounded and protuberant [8], and are characterized by very slow, continuous growth [5]. Osteomas, are usually asymptomatic, often remain undetected unless incidentally found on a routine radiographic survey or until they cause facial asymmetry or functional impairment [9]. They produce symptoms by compression, rather than by invasion or destruction [8]. Depending on the location, they might cause headaches, facial pain or swelling, surface ulcerations and/or limited mandibular movements [8]. In all six cases in the study, patients presented with clinical symptoms like pain, facial asymmetry, limited mouth opening, local sensitivity, difficulty in speech and deglutition, recurrent mucosal ulcers or sinusitis.
Peripheral osteomas occur mainly in the head and neck region. Osteomas are the most frequent benign tumors of the paranasal sinuses, occurring most commonly in the frontal sinus. [10] Peripheral osteomas of the jaws are uncommon [9] and more often found in the mandible than in the maxilla [5]. Lingual aspect of the mandibular body and the inferior border of the angle are the most common sites affected in the mandible. [5] In the maxilla there have been reports of osteomas arising from the maxillary sinus [11], from the outer plate in the molar region, from the tuberosity, and from the anterior or posterior parts of the maxilla. Although an osteoma can arise at any age, it seems to be more common among young adults. It is generally seen in the third and fourth decades of life [9]. It has been reported by some authors that osteomas have no sex predilection [5, 12], while Kaplan et al. [4] in their case series have found a male-to-female ratio of 2:1. Four of our six cases occurred in male patients with most common region of occurrence being the body of the mandible. One case involved the maxillary sinus. Three of our six cases occurred in the third or fourth decades of life.
Though the exact etiology and pathogenesis of osteoma is still unknown, traumatic, congenital, inflammatory, and endocrine causes have been considered as possible etiological factors. Varboncoeur et al. [11] considered osteomas to arise either from embryological cartilaginous rests or from persistent embryological periosteum. According to the developmental or embryological theory [13], osteomas would then originate from the suture between bones with different embryological derivatives (membranous/enchondral), but this seems rather unlikely as in most cases they develop in adults and not during childhood or adolescence. The inflammatory theory suggests that chronic infections could stimulate the proliferation of the periosteum-related osteogenetic cells. According to other investigators [1], osteoma is a reactive condition triggered by trauma (even minor that is unlikely to be remembered by the patient, years later), because peripheral osteomas are generally located on the lower border or buccal aspect of the mandible, which often get traumatized during daily routine. Kaplan et al. [4] suggested that a combination of trauma and muscle traction may play a role in its development; however, a clear history of trauma is reported only in a few cases. Our patients could not recall any trauma in the area of the lesion.
Traditional radiographic imaging is generally sufficient to diagnose an osteoma [9]. It appears as a radiopaque mass with a density similar to normal bone. A panoramic radiograph, lateral oblique view of the mandible, Water’s view, or a tomogram usually shows the position and benign nature of the lesion. Computed tomography (CT) scanning makes it possible to achieve a better resolution and a more precise localization, especially with 3D reconstruction [8, 14]. All our cases showed a well circumscribed radiopaque mass.
The differential diagnosis should include several pathologic entities both inflammatory and neoplastic, such as exostosis, chronic focal sclerosing osteomyelitis, cemento-osseous dysplasia, osteoblastoma, ossifying fibroma, chondroma, osteosarcoma, Paget’s disease, fibrous dysplasia, and odontoma although it has been stated that at its typical site, the lesion cannot be confused with other tumours or tumour like lesions.
Osteoma and benign osteoblastoma (OB) are closely related entities and pose a challenge in the clinical diagnosis. OB is more common in jaw than osteoma [15]. Osteoblastomas occur predominantly on the left side of the posterior mandible and are generally larger than osteoma, exhibit rapid rate of growth and are associated with pain, tenderness, and discomfort [16]. Radiographically, osteoma is a thick radiopaque mass with reactive sclerosis of bone and sometimes with thick periosteal reaction. In contrast the OB is radiolucent and of larger size, located in medullary bone and causing expansion of affected bone [17]. Microscopically, osteoblastoma is characterized by a proliferation of osteoblasts forming bone trabeculae set in a vascularized fibrous connective tissue stroma, often with osteoblastic rimming [18]. Because the background of vascularized fibrous connective tissue is absent in osteoma, this feature should make the distinction between osteoma and osteoblastoma uncomplicated.
Patients with osteoma and supernumerary or impacted teeth should undergo a work-up for Gardner’s syndrome [19]. The triad of colorectal polyposis, skeletal abnormalities and multiple impacted or supernumerary teeth is consistent with this syndrome. Because osteomas often develop before the colorectal polyposis, early recognition of syndrome may be in some cases, a life saving event. The colonic polyps of Gardner syndrome have a 100% risk of undergoing malignant transformation; consequently, early identification and surgical therapy of the disease are critical [20]. Therefore, the patient with a diagnosis of mandibular osteoma, suspected to have Gardner’s syndrome, should be further examined to rule out colorectal carcinoma. In our cases colonoscopy ruled out any polyposis and other triad of Gardner’s syndrome.
Treatment of the osteoma consists of complete surgical removal at the base where it unites with the cortical bone [4, 5]. We preferred surgical excision for the treatment of osteomas. An intra oral approach is always preferable when possible (as in the case of tumour on the lingual aspect of the body or ramus), because it avoids external scar and injury to facial nerve is minimal, whereas the extra oral approach usually affords better access and visibility when the tumours are very large or in an unfavourable position [21]. There are no reports of osteomas undergoing malignant transformation. One recurrence 9 years after surgical excision was reported by Bosshardt et al. [22]. Therefore, it is appropriate to provide both periodic clinical and radiographic follow up after surgical excision of a peripheral osteoma.
Conclusion
Peripheral osteomas of the jaw bone are uncommon. Early diagnosis and precise surgical excision of the lesion helps in alleviating pain, swelling, limited mandibular movements and subsequent facial asymmetry. The post operative follow up should include periodic clinical and radiological studies. The recurrence of these lesions is rare. Patients of osteoma with multiple impacted supernumerary teeth should be evaluated for the Gardner’s syndrome.
References
- 1.Bodner L, Gatot A, Sion-Vardy N, et al. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998;56:1446–1449. doi: 10.1016/S0278-2391(98)90414-1. [DOI] [PubMed] [Google Scholar]
- 2.Sayan NB, Ucok C, Karasu HA, Gunhan O. Peripheral osteoma of the oral and maxillofacial region. J Oral Maxillofac Surg. 2002;60:1299–1301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 3.Marx RE, Stern D. Oral and maxillofacial pathology: A rationale for diagnosis and treatment. Hanover Park: Quintessence Publishing; 2003. p. 771. [Google Scholar]
- 4.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–470. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 5.Cutilli BJ, Quinn PD. Traumatically induced peripheral osteoma: Report of a case. Oral Surg Oral Med Oral Pathol. 1992;73:667. doi: 10.1016/0030-4220(92)90006-C. [DOI] [PubMed] [Google Scholar]
- 6.Wijn MA, Keller JJ, Giardiello FM, Brand HS. Oral and maxillofacial manifestations of familial adenomatous polyposis. Oral Dis. 2007;13:360–365. doi: 10.1111/j.1601-0825.2006.01293.x. [DOI] [PubMed] [Google Scholar]
- 7.Ida M, Nakamura T, Utsunomiya J. Osteomatous changes and tooth abnormalities found in the jaws of patients with adenomatosis coli. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1981;52:2–11. doi: 10.1016/0030-4220(81)90164-x. [DOI] [PubMed] [Google Scholar]
- 8.Chalain T, Tan B. Ivory osteoma of the craniofacial skeleton. J Craniofac Surg. 2003;14:729–735. doi: 10.1097/00001665-200309000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Longo F, Califano L, Maria G, Ciccarelli R. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001;59:698–700. doi: 10.1053/joms.2001.23408. [DOI] [PubMed] [Google Scholar]
- 10.Becelli R, Santamaria S, Saltarel A, Carboni A, Iannetti G. Endo-orbital osteoma: two case reports. J Craniofac Surg. 2002;13:493–496. doi: 10.1097/00001665-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Varboncoeur P, Vanbelois HJ, Bowen LL. Osteoma of the maxillary sinus. J Oral Maxillofac Surg. 1990;48:882–883. doi: 10.1016/0278-2391(90)90351-2. [DOI] [PubMed] [Google Scholar]
- 12.Swanson KS, Guttu RL, Miller ME. Gigantic osteoma of the mandible: report of a case. J Oral Maxillofac Surg. 1992;50:635–638. doi: 10.1016/0278-2391(92)90449-A. [DOI] [PubMed] [Google Scholar]
- 13.Seward MHE. An osteoma of the maxilla. Br Dent J. 1965;5:27–30. [PubMed] [Google Scholar]
- 14.Kashima K, Rahman OIF, Sakoda S, Shiba R. Unusual peripheral osteoma of the mandible: report of 2 cases. J Oral Maxillofac Surg. 2000;58:911–913. doi: 10.1053/joms.2000.8223. [DOI] [PubMed] [Google Scholar]
- 15.Weinberg S, Katsikeris N, Pharoah M. Osteoblastoma of the mandibular condyle: review of the literature and report of a case. J Oral Maxillofac Surg. 1987;45:350–355. doi: 10.1016/0278-2391(87)90359-4. [DOI] [PubMed] [Google Scholar]
- 16.Rawal YB, Angiero F, Allen CM, Kalmar JR, Sedghizadeh PP, Steinhilber AM. Gnathic osteoblastoma: clinicopathologic review of seven cases with long-term follow-up. Oral Oncol. 2006;42:123–130. doi: 10.1016/j.oraloncology.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Smith RA, Hansen LS, Resnick D, Chan W. Comparison of the osteoblastoma in gnathic and extragnathic site. Oral Surg Oral Med Oral Pathol. 1982;54:285–298. doi: 10.1016/0030-4220(82)90098-6. [DOI] [PubMed] [Google Scholar]
- 18.Jones AC, Prihoda TJ, Kacher JE, Odingo NA, Freedman PD. Osteoblastoma of the maxilla and mandible: a report of 24 cases, review of the literature, and discussion of its relationship to osteoid osteoma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:639–650. doi: 10.1016/j.tripleo.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Lew D, Witt A, Hicks RJ, Cavalcanti MG. Osteomas of the condyle associated with Gardner’s syndrome causing limited mandibular movement. J Oral Maxillofac Surg. 1999;57:1004–1009. doi: 10.1016/S0278-2391(99)90026-5. [DOI] [PubMed] [Google Scholar]
- 20.Bilkay U, Erdem O, Ozek C, Helvaci E, Kilik K, Ertan Y, Gurler T. Benign osteoma with Gardner syndrome: review of the literature and report of a case. J Craniofac Surg. 2004;15:506–509. doi: 10.1097/00001665-200405000-00032. [DOI] [PubMed] [Google Scholar]
- 21.Chen YK, Lin LM, Lin CC. Osteoma of the mandibular coronoid process: Report of a case. Int J Oral Maxillofac Surg. 1998;27:222. doi: 10.1016/S0901-5027(98)80016-7. [DOI] [PubMed] [Google Scholar]
- 22.Bosshardt L, Gordon RC, Westerberg M, et al. Recurrent peripheral osteoma of mandible: Report of a case. J Oral Surg. 1971;29:446. [PubMed] [Google Scholar]


