Abstract
Bilateral Warthin’s tumours of parotid constitute a small proportion of all salivary gland tumours. We present a case report of surgical management of a prototype case.
Introduction
Papillary cystadenoma lymphomatosum is a benign hamartoma or reactive proliferation of ductal salivary gland cells and lymphoid elements; that is commonly referred as a Warthin’s tumor [1, 2]. They are most common in parotid glands and around 11% of all benign salivary gland tumors [3]. In 4–6% of cases Warthin’s tumors occur bilaterally or two or more tumors are known to occur in same gland [1]. Knowledge of clinical representation and management of bilateral Warthin’s tumor is based on the summary of knowledge present in the literature. Observation only [4, 5] and enucleation [4, 5] have been suggested in some articles besides the standard treatment, superficial parotidectomy [6]. However, a clear guideline of addressing the bilateral cases specifically is not yet outlined clearly in the texts.
Report of a Case
A 68-years-old male patient, reported with the complaint of bilateral parotid swellings. Patient had moderate cardiopulmonary conditions as well as allergic to penicillin.
The patient’s history revealed swelling in bilateral parotid regions, for 5 years. Condition was neglected and later alternate forms of medicines tried with no demonstrable result. There was gradual enlargement of the tumors. Three months before presentation, enlargement was quite rapid.
On palpation of bilateral parotid glands, the lesions were painless, smooth and mobile. An MRI scan showed bilateral, well circumscribed, heterogeneous masses located in the tails of parotid glands. Approximate dimensions—Right 6 cm × 4.5 × 2.5 cm3 and Left 6 × 5 × 2 cm3 (Figs. 1, 2, 3).
Fig. 1.

Bilateral parotid tumours
Fig. 2.

Closer view on lesions of both the sides
Fig. 3.
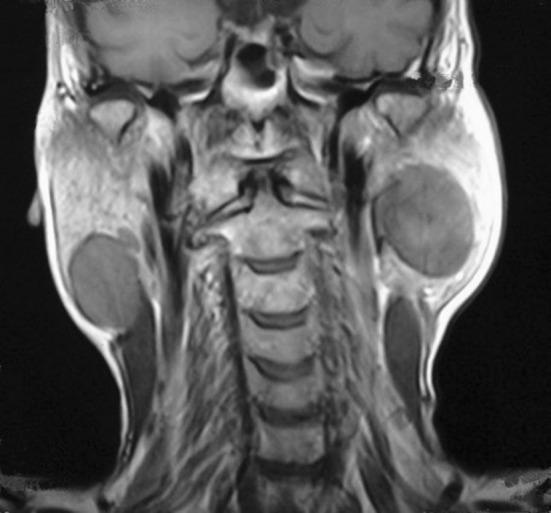
The MRI showing bilateral parotid swellings
There was no sign of facial nerve function disturbance.
No FNA was done as these were frankly benign parotid tumors and the plan was to proceed for bilateral superficial parotidectomy directly. In general, FNA has good overall accuracy for diagnosing salivary gland neoplasms (87–97%) [7], and it has been widely used for the diagnosis of Warthin’s tumors.
Management
As mentioned before, patient has moderate cardiopulmonary conditions. Stress echo test was conducted and concluded negative for evidence of provocable myocardial ischemia. Diagnosis was chronic obstructive pulmonary disease. Respiratory physician recommended pre-operative, Inj. Hydrocortisone 100 mg intravenous and Duolin inhaler TDS as well as oxygen (2 L/min) with nasal canula continuously.
Both sided superficial parotidectomy were done with all branches of facial nerve preserved (Figs. 4, 5, 6). Tumour capsules were maintained intact. The tumours were chocolate coloured and soft (almost cystic) and were not easily separable from the parotid tissue at their points of origin. There was no post operative complaints related to the facial nerves (Figs. 7, 8, 9).
Fig. 4.
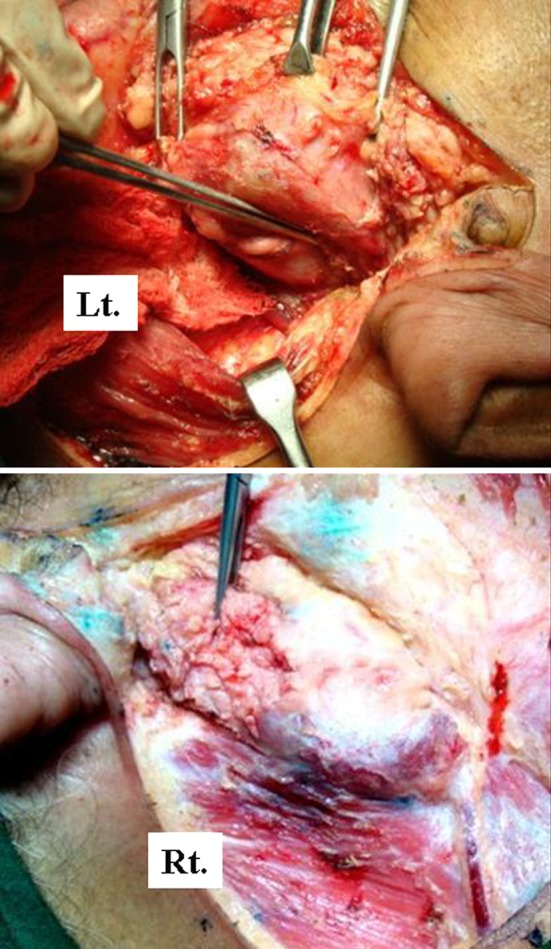
Exposure lesion exposed surgically
Fig. 5.
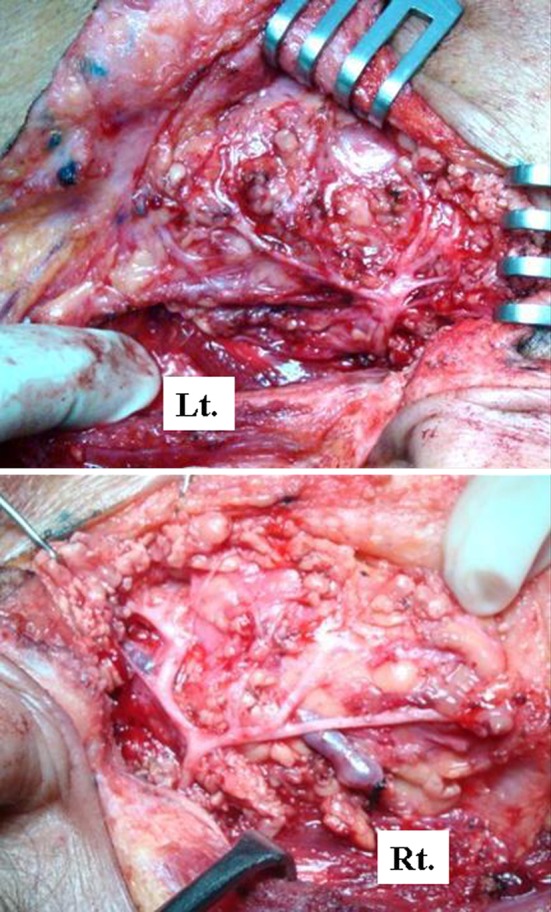
Facial nerves
Fig. 6.
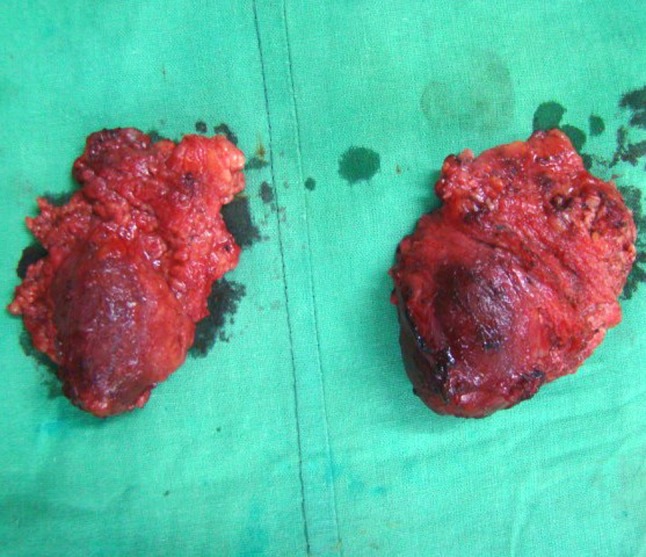
Excised specimens
Fig. 7.

Post operative
Fig. 8.
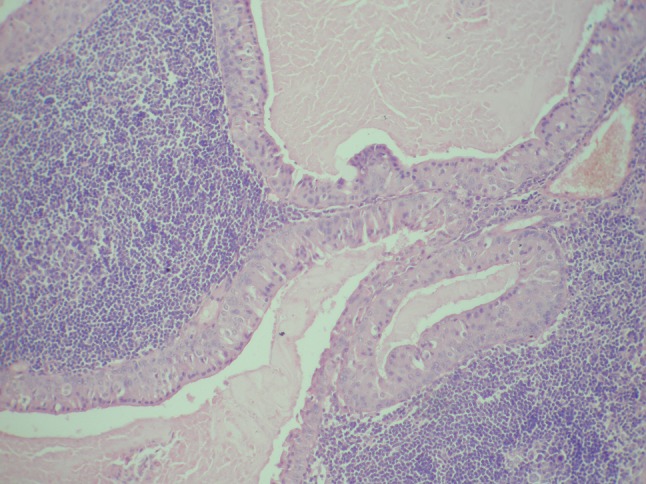
Histology of Right parotid tumour
Fig. 9.
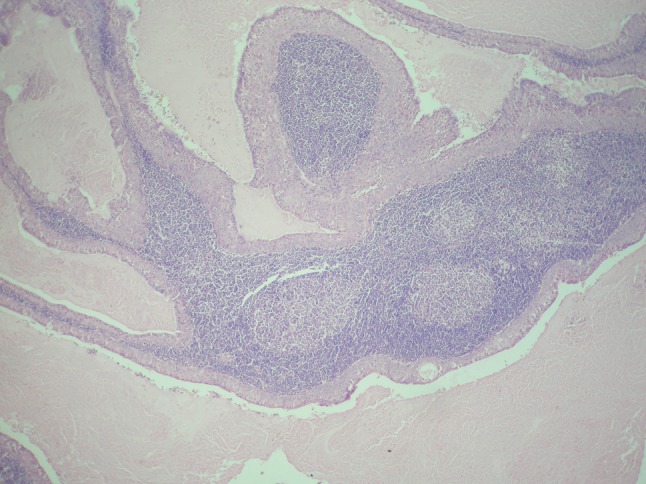
Histology of Left parotid tumour
Histopathology
Microscopy revealed thin, encapsulated tumor mass consisting of tall, columnar, finely granular, eosinophilic epithelial cells surrounding lymphoid tissues. The epithelium typically forms papillary projections into cystic spaces. Overall features were conclusive of Warthin’s tumors.
Discussion
Historically men are more frequently associated with Warthin’s tumor than females, with ratio of 2.5:1 [8]. It is common in elder age groups with the average age of 60 years [8, 9]. Recent reports state that females are also equally endangered due to the increasing smoking habit among women [8]. Smoking increases the risk of Warthin’s tumor by eight folds [10].
The common site for Warthin’s tumor is “Tail” of parotid glands, but there are cases reported in the upper lip, palates, nasopharynx [11, 12].
Warthin’s tumor is a hamartoma or reactive proliferation of ductal salivary gland cells and lymphoid elements. Though it is a benign condition, some reports of malignant transformation are also documented causing facial paralysis [13]. So, complete superficial parotidectomy is essential while resecting the tumor [6, 14].
Some controversies are present over treatment options. Some surgeons recommend conservative lines like observation only [4, 5], or tumour enucleation [4, 5], as this condition is benign and painless, by calculating risk to facial nerve branches. Though there are claims of Warthin’s tumour growth getting arrested at some stage, there are evidences of these tumours growing to massive sizes, infarcting, necrosing and affecting the facial nerve [15, 16].
References
- 1.Marx R, Stern D (2003) Oral maxillofacial pathology—a rationale for diagnosis and treatment, malignant soft tissue tumours of mesenchymal origin, 2nd edn. Quintessence, Illinois pp 475–477
- 2.Batsakis JG, El-Naggar AK. Warthin’s tumor. Ann Otol Rhinol Laryngol. 1990;99:588–591. doi: 10.1177/000348949009900719. [DOI] [PubMed] [Google Scholar]
- 3.Sirohi D, Sharma R, Sinha R, Menon S. Salivary gland neoplasms: an analysis of 74 cases. J Maxillofacial Oral Surg. 2009;8(2):164–166. doi: 10.1007/s12663-009-0040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo GH, Eisele DW, Askin FB, Driben JS, Johns ME. Warthin’s tumor: a 40-year experience at the Johns Hopkins Hospital. Laryngoscope. 1994;104:799–803. doi: 10.1288/00005537-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Reddy VM, Thangarajan T, Arango F, Panarese A. Conservative management of Warthin tumor. J Otolaryngol Head Neck Surg. 2008;37(5):744–749. [PubMed] [Google Scholar]
- 6.Ethunandan M, Pratt C, Higgins B, Morrison A, Umar T, Macpherson D, Wilson A. Factors influencing the occurrence of multicentric and recurrent Warthin’s tumor: a cross sectional study. Int J Oral Maxillofac Surg. 2008;37(9):831–834. doi: 10.1016/j.ijom.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Stewart CJ, MacKenzie K, McGarry GW, Mowat A. Fine-needle aspiration cytology of salivary gland: a review of 341 cases. Diagn Cytopathol. 2000;22:13. doi: 10.1002/(SICI)1097-0339(20000301)22:3<139::AID-DC2>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 8.Khan MA (2001) Salivary gland tumours. Basic oral and maxillofacial pathology, vol 1
- 9.Hatch RL, Shah S. Warthin tumor: a common, benign tumor presenting as a highly suspicious mass. J Am Board Fam Med. 2005;18:320–322. doi: 10.3122/jabfm.18.4.320. [DOI] [PubMed] [Google Scholar]
- 10.Chung Y, Khoo M, et al. Epidemiology of Warthin’s tumour of the parotid gland in an asian population. Br J Surg. 1999;86(5):661–664. doi: 10.1046/j.1365-2168.1999.01113.x. [DOI] [PubMed] [Google Scholar]
- 11.Almedia A, Hanemann J, Oliveria D. Warthin tumor of upper lip: an unusual location. Int J Surg Pathol. 2009 doi: 10.1177/1066896908331232. [DOI] [PubMed] [Google Scholar]
- 12.Low WK, Ng SB. Synchronous parotid and nasopharyngeal Warthin’s tumors: first report of a case. Korean ENT J. 2002;81:341–839. [PubMed] [Google Scholar]
- 13.Batsakis JG. Carcinoma ex papillary cystadenoma lymphomatosum malignant Warthin’s tumor. Ann Otol Rhinol Laryngol. 1987;96:234–235. doi: 10.1177/000348948709600221. [DOI] [PubMed] [Google Scholar]
- 14.Brown L, Jr, Aparicio S. Malignant Warthin’s tumor: an ultrastructural study. J Clin Pathol. 1984;37:170–175. doi: 10.1136/jcp.37.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maini S, Osborne JE. Ischaemic necrosis and facial palsy in Warthin’s tumour of the parotid gland. Int J ORL HNS. 2002;29(1):99–101. doi: 10.1016/s0385-8146(01)00120-1. [DOI] [PubMed] [Google Scholar]
- 16.Newman L, Loukata R, Bradley P. An infarcted Warthin’s tomour presenting with facial weakness. Br J Oral Maxillofac Surgery. 1993;31(5):311–312. doi: 10.1016/0266-4356(93)90067-7. [DOI] [PubMed] [Google Scholar]


