Abstract
Purpose
This article represents the use of inferiorly based nasolabial flap in reconstruction of various intraoral and extraoral defects.
Patients and Methods
Nasolabial flaps were performed in 40 patients, for reconstruction of buccal mucosa, gingivobuccal sulcus, commissure, lower lip, floor of mouth, upper lip and lower alveolar defects.
Results
The most common defect site in the oral cavity was the buccal mucosa. Partial flap necrosis occurred in five patients. Out of 40 cases of carcinoma of lip, commissure and floor of the mouth, all the patients had good speech after complete healing of the wound. None of the patients who had lip or commissure reconstruction developed drooling of saliva due to lip incompetence.
Conclusion
The inferiorly based nasolabial flap provides reliable coverage of intermediate-sized oral cavity defects when used alone. Minimal donor morbidity is associated with its use. It is especially useful in elderly patients with facial skin laxity and where esthetics is not a major concern.
Keywords: Nasolabial flap, Oral cavity defects, Local flaps, Alveolar defects
Introduction
With the increasingly widespread application of reliable microvascular free tissue transfer techniques for oral cavity reconstruction, the routine need for a variety of local and regional flaps has decreased. However, a number of such flaps remain quite useful and should be included in the modern armamentarium of the reconstructive surgeon. Often, a combination of local and distant flaps is required to optimize the functional outcome after oral resection. In this article, the focus is on the utility of the pedicled nasolabial flap to achieve this goal.
The subcutaneous pedicled nasolabial flap appears to have been originally described in the works of Sushruta in 600 BC [1]. For centuries thereafter it was used primarily in external nasal reconstruction.
Thiersch [2] was the first to use a transbuccal transfer of this flap for closure of an oral cavity defect. Subsequently, Esser [3] reported use of a cutaneous nasolabial flap transferred in two stages to increase its reliability. Wallace [4] and Rose [5] later reported modifications of the basic flap, allowing for single-stage transfer. Several authors have reported favorable outcomes when this flap was used to cover various oral cavity defects [6–9].
Patients and Methods
We retrospectively studied 40 patients (male 26 and 14 female) who had undergone excision of oral cancer and reconstruction using nasolabial flaps. The data were generated from the operation register and the case files of the patients and were supplemented by the postal enquiries. The age of the patients ranged from 23 to 73.
Patients profile
| S. no | Age/Sex | Diagnosis | Treatment done |
|---|---|---|---|
| 1 | 73/M | SCC BM | WE + MM + NLF |
| 2 | 50/F | SCC lower GBS | WE + NLF |
| 3 | 58/F | SCC lower GBS | WE + MM + NLF |
| 4 | 49/F | SCC BM | WE + NLF |
| 5 | 60/M | SCC commissure + BM | WE + NLF |
| 6 | 33/M | SCC BM | WE + NLF |
| 7 | 55/M | SCC lower lip | WE + NLF |
| 8 | 50/M | SCC Lt commissure + BM | WE + NLF |
| 9 | 60/F | SCC Lt BM | WE + NLF |
| 10 | 62/M | BCC Rt commissure | WE + NLF |
| 11 | 55/M | SCC Rt lower lip | WE + NLF |
| 12 | 40/F | SCC lower lip | WE + NLF |
| 13 | 48/M | SCC FOM | WE + MM + NLF |
| 14 | 60/F | SCC lower lip | WE + NLF |
| 15 | 70/M | SCC lower lip | WE + NLF |
| 16 | 55/M | SCC FOM | WE + MM + NLF |
| 17 | 50/M | SCC Rt BM + commissure | WE + NLF |
| 18 | 58/M | SCC FOM | WE + NLF |
| 19 | 60/F | SCC Rt commisure | WE + NLF |
| 20 | 50/F | SCC Rt BM + commissure | WE + NLF |
| 21 | 52/F | SCC lower lip | WE + NLF |
| 22 | 45/F | SCC Rt commisure | WE + NLF |
| 23 | 50/F | BCC Rt nose | WE + NLF |
| 24 | 55/M | SCC FOM | WE + NLF |
| 25 | 45/M | OSMF B/L BM | WE + NLF |
| 26 | 65/M | SCC lower lip | WE + NLF |
| 27 | 60/M | ACC Rt BM | WE + NLF |
| 28 | 40/F | SCC upper lip | WE + NLF |
| 29 | 64/M | SCC FOM | WE + MM + NLF |
| 30 | 47/M | SCC lower alveolus | MM + NLF |
| 31 | 60/M | SCC Lt BM + FOM | WE + MM + NLF |
| 32 | 45/M | SCC Lt BM | WE + NLF |
| 33 | 23/F | SCC Lt BM | WE + NLF |
| 34 | 60/F | SCC Lt BM + lower lip | WE + NLF |
| 35 | 55/M | SCC lower lip | WE + NLF |
| 36 | 45/M | SCC Lt BM | WE + BM |
| 37 | 50/M | SCC Rt BM | WE + BM |
| 38 | 55/M | SCC Rt upper lip | WE + NLF |
| 39 | 60/M | SCC Rt BM | WE + NLF |
| 40 | 28/M | SCC Lt lower lip + BM | WE + NLF |
SCC Squamus cell carcinoma, Rt right, Lt left, BM buccal mucosa, WE wide excision, MM marginal mandibulectomy, NLF nasolabial flap, GBS gingivobuccalsulcus, ACC adenoid cystic carcinoma, FOM floor of mouth, BCC basal cell carcinoma, OSMF oral submucous fibrosis
Results
A total number of 40 cases were evaluated who underwent reconstruction with nasolabial flap. The most common defect site in the oral cavity was the buccal mucosa followed by commissure and lower lip. Post operatively all patients had good speech after complete healing of the wound. Hypertrophied scar occurred in four patients and in five patients there was partial necrosis at the site where the flap pedicled was divided. Three flap developed infection which was controlled by the local measures, and systemic antibiotic therapy. Failure of the flap occurred in four patients. Drooling of saliva due to lip incompetence was the most common complication (Fig. 1a, b, c, d, e).
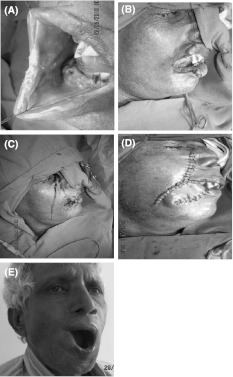
Fig. 1.
a SCC of right commissure and lower lip. b Wide excision done. c Outlined NLF. d NLF done. e Post operative view
Discussion
The idea of using the spare skin of the nasolabial fold to reconstruct nearby defects dates back to 1830 when Dieffenbach used superiorly based nasolabial flaps to reconstruct defects of the ala of the nose. In 1917 Esser used inferiorly based nasolabial flaps to repair palatal fistulae. Since then, modifications of the flaps have been described by several surgeons, ranging from the conventional pedicled flap (superiorly or inferiorly based) to subcutaneously pedicled flaps and facial-artery island flaps [10].
The skin of the nasolabial fold is nourished by multiple small branches from the alar branch of the superiorlabial artery, which is a branch of the facial artery, and by the terminal branches of the facial artery, which is called the angular artery near the dorsum of the nose. Further superolaterally the skin is nourished by the infraorbital artery (a branch of the ophthalmic artery) and the transverse facial artery. Hence, it is possible to design both an inferiorly based nasolabial flap, with the facial artery as its pedicle, and a superiorly based nasolabial flap with the infraorbital and transverse facial arteries as its pedicle [10]. Retrograde flow from the terminal parts of the facial artery and vein also contribute to the blood supply.
The lips and the floor of the mouth can also be reconstructed with nasolabial flaps, using techniques already described in the plastic surgery literature [11]. A limited full-thickness defect of the lips, commissure and buccal mucosa can also be reconstructed by folding the flap [10]. In addition to the superior cosmetic and functional result, the nasolabial flap has the added advantages of providing hairless skin to the defect and reducing the donor-site morbidity associated with other flaps. It provides adequate bulk at the recipient site, making postoperative rehabilitation easier. The flap is easily accessible in the same surgical field, and easy and quick to harvest, thus reducing operating time.
Even relatively small defects of the anterior floor of the mouth often require reconstruction to avoid loss of tongue mobility that results in a serious disturbance of function. The inferiorly based nasolabial flap, used bilaterally to cover defects of the anterior floor of the mouth, is the only two-stage technique that should be considered part of mainstream reconstruction [10, 11]. This is because it is reliable and predictable. This technique is well suited to repair defects of the floor of the mouth up to 4 to 5 cm in diameter. Reconstruction options for smaller defects of the oral cavity are ranging from primary closure, secondary healing from mucosalisation, or covering the defect site with split thickness skin grafts. Most of these techniques may result in speech and swallowing problems. Intraoral reconstruction with the nasolabial flap is a simple and fast procedure and minimizes the morbidity relating to speech and swallowing impairment to a great extent [12, 13]. Adequate oral function and esthetic results following reconstruction of smaller defects of the anterior floor of mouth were confirmed by Hofstra et al. [14]. In their series of 26 patients with intraoral reconstruction using a nasolabial flap, Maurer et al. [15] reported that 23 patients (88%) underwent successful prosthetic rehabilitation and they concluded that the nasolabial flap is a functional and esthetically satisfactory alternative compared to free tissue transfer.
Varghese et al. [12] published the largest series of nasolabial flaps for intraoral reconstruction with 224 patients. An inferiorly based nasolabial flap was used in 198 patients, whereas 24 patients were reconstructed using an superiorly based flap. The authors reported significantly more complications in post-irradiated cases than in primary cases (P = 0.03).
The use of nasolabial flaps in patients with limited defects of the anterior floor of mouth after tumor resection showed adequate functional and esthetic results [14]. Intraoral reconstruction using nasolabial flaps is a simple and fast procedure and can be recommended in particular in patients with medical comorbidities who are not candidates for time-consuming operations including microsurgical reconstructions.
It may be concluded from this study that the nasolabial flap is a simple and viable option in the reconstruction of selected oral defects in a low-resource setting where microvascular expertise is not available. The procedure can be performed with minimal complications in postirradiated patients. Preservation of the facial artery is desirable when the neck also has to be dissected as part of the same procedure. Reconstruction options for smaller defects of the oral cavity are ranging from primary closure, secondary healing.
Conclusion
The nasolabial flap provides the surgeon with another technique for effective reconstruction of select intraoral and extraoral defects. Minimal donor morbidity is associated with its use. It is especially useful in elderly patients with facial skin laxity. The tunneled random nasolabial flap should be kept in mind as a reliable option when reconstructing intraoral defects, especially where pliable thin tissue can be used to cover a moderately sized defects.
References
- 1.Pers M. Cheek flaps in partial rhinoplasty. Scand J Plast Reconstr Surg. 1967;1:37. doi: 10.3109/02844316709006558. [DOI] [Google Scholar]
- 2.Thiersch C. Verschluss eines loches im harten gaumen durch dic weichtheile der wange. Arch Heilkunde. 1868;9:159. [Google Scholar]
- 3.Esser JFS. Deckung von gaumendefekten mittels gestielter naso-labial-haultlappen. Deutsch Zeitschrift fur Chirurgie. 1918;147:128. doi: 10.1007/BF02798064. [DOI] [Google Scholar]
- 4.Wallace AF. Esser’s skin flap for closing large palatal fistulae. Br J Plast Surg. 1966;19:322. doi: 10.1016/S0007-1226(66)80073-5. [DOI] [PubMed] [Google Scholar]
- 5.Rose EH. One staged arterialised nasolabial island flap for floor of mouth reconstruction. Ann Plast Surg. 1981;6:71. doi: 10.1097/00000637-198101000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Morgan RF, Chambers RG, Jaques DA, et al. Nasolabial flap in intraoral reconstruction. Am J Surg. 1981;142:448. doi: 10.1016/0002-9610(81)90372-X. [DOI] [PubMed] [Google Scholar]
- 7.Gewirtz HS, Eilber FR, Zaram HA. Use of the nasolabial flap for reconstruction of the floor of the mouth. Am J Surg. 1981;136:508. doi: 10.1016/0002-9610(78)90271-4. [DOI] [PubMed] [Google Scholar]
- 8.Ioannides C, Fossion E. Nasolabial flap for the reconstruction of defects of the floor of mouth. Int J Oral Maxillofac Surg. 1991;20:40. doi: 10.1016/S0901-5027(05)80694-0. [DOI] [PubMed] [Google Scholar]
- 9.Mutimer KL, Poole MD. A review of nasolabial flaps for intraoral defects. Br J Plast Surg. 1987;40:472. doi: 10.1016/s0007-1226(87)90075-0. [DOI] [PubMed] [Google Scholar]
- 10.Cornmck GC, Lamberty BGH. The Arterial Anatomy of Skin Flaps. 2. Edinburgh: Churchill Livingstone; 1994. [Google Scholar]
- 11.Ariyan S, Chicarilli ZN. Cancer of the upper aerodigestive system. In: McCarthy JG, editor. Plastic Surgery. Philadelphia: WB Saunders Company; 1990. pp. 3412–3477. [Google Scholar]
- 12.Varghese BT, Sebastian P, Cherian T, Mohan PM, Ahmed I, Koshy CM, Thomas S. Nasolabial flaps in oral reconstruction: an analysis of 224 cases. Br J Plast Surg. 2001;54:499–503. doi: 10.1054/bjps.2001.3651. [DOI] [PubMed] [Google Scholar]
- 13.Wijk MP, Damen A, Nauta JM, Lichtendahl DHE, Dhar BK. Reconstruction of the anterior floor of the mouth with the inferiorly based nasolabial flap. Eur J Plast Surg. 2000;23:200–203. doi: 10.1007/s002380050250. [DOI] [Google Scholar]
- 14.Hofstra EI, Hofer SOP, Nauta JM, Roodenburg JLN, Lichtendahl DHE. Oral functional outcome after intraoral reconstruction with nasolabial flaps. Br J Plast Surg. 2004;57:150–155. doi: 10.1016/j.bjps.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Maurer P, Eckert AW, Schubert J. Functional rehabilitation following resection of the floor of the mouth: the nasolabial flap revisited. J Craniomaxillofac Surg. 2002;30:369–372. doi: 10.1054/jcms.2002.0325. [DOI] [PubMed] [Google Scholar]