Abstract
Introduction. Women diagnosed with breast cancer at a young age are more likely to carry a cancer predisposing genetic mutation. Per the current NCCN recommendations, women diagnosed under age 50 should be referred to cancer genetic counseling for further risk evaluation. This study seeks to assess patient-reported barriers and facilitators to receiving genetic counseling and risk assessment among a community-based population of young breast cancer survivors (YBCS). Methods. Through the Michigan Cancer Surveillance Program, a state-based cancer registry, 488 women diagnosed with breast cancer before age 50 in 2006-2007 were identified. They received a mail survey regarding family history and facilitators and barriers to receiving genetic counseling and risk assessment. Results. Responses were received from 289 women (59.2%). One hundred twenty-two (42.2%) reported having received cancer genetic counseling. The most frequent reason identified for receiving services was to benefit their family's future. The top reasons for not attending were “no one recommended it” and “medical insurance coverage issues.” Discussion. This study is the first published report using a state cancer registry to determine facilitators and barriers to receiving genetic counseling and risk assessment among YBCS. These findings demonstrate the need for additional awareness and education about appropriate indications for genetic services.
1. Introduction
Breast cancer diagnosed at a young age is an indication of a higher likelihood for an inherited cancer syndrome, such as hereditary breast and/or ovarian cancer syndrome (HBOC) or rarer genetic conditions such as Cowden syndrome and Li-Fraumeni syndrome [1–3]. According to the 2011 National Comprehensive Cancer Network (NCCN) Guidelines entitled “Genetic/Familial High-Risk Assessment: Breast and Ovarian,” women diagnosed with breast cancer prior to age 50 should be referred for further risk assessment, genetic counseling, and possible genetic testing [3]. Individuals diagnosed with breast cancer prior to age 50 are commonly referred to as young breast cancer survivors (YBCS) [4]. YBCS remain an understudied survivor population who have unique needs and challenges compared to the traditional cancer survivors because of young ages at diagnosis and associated family and societal roles [5, 6]. Even less is known about factors motivating this young population to attend a familial/high risk genetic counseling clinic.
According to the recent cancer genetic counseling recommendations published by the National Society of Genetic Counselors (NSGC), “genetic counseling and risk assessment is the process of identifying and counseling individuals at increased risk of developing cancer and distinguishing between those at high risk (highly penetrant hereditary cancer syndrome), those at modestly increased risk (multifactorial etiology or low penetrance allele), and those at average risk” [7]. Genetic counseling and risk assessment are often obtained through referral to a qualified cancer genetic professional [8]. Recent studies have found that referring providers are not able to consistently recognize appropriate referral indications for hereditary breast and ovarian cancer risk assessment and genetic counseling [2, 9–11].
As recommended by the NSGC and others, the essential components of the hereditary cancer risk assessment and genetic counseling visit include: (1) patient intake, including personal medical and 3-4 generation family history; (2) cancer genetic risk assessment using the personal history, family history, and physical examination to determine average, moderate, or increased cancer risk; (3) the offer of genetic testing when appropriate conditions apply; (4) an informed consent process is necessary and, in Michigan, legally required; and (5) disclosure of test results, including personalized interpretation of results, cancer risk reassessment, and identification of at-risk family members regardless of whether the test is positive, negative, or inconclusive [3, 7, 9, 12]. Qualified cancer genetics professionals guide patients through these essential components as well as encourage women at high risk to adopt appropriate screening and preventive strategies, since individuals with HBOC may benefit from earlier detection or more intense cancer screening or intervention [3, 7, 12, 13].
Six key prior studies have been published on motivators, facilitators, and/or barriers to patients attending familial/high risk cancer clinics, genetic counseling, and risk assessment using varying populations and recruitment methods [13–19]. Four of these studies took place outside the United States. Brain et al. conducted the largest study to date, using questionnaires from 833 Welsh women, all with a family history of breast cancer, to identify self-reported reasons for attending a familial breast cancer clinic; among the reasons identified for attending, personal risk was ranked highest, followed by risk to family members, to gain reassurance, and interest in genetic testing. Chin et al. (2005) looked specifically at female breast cancer survivors and evaluated responses to a hypothetical question about willingness to attend breast cancer genetic risk assessment clinic. Among 164 Singaporean female breast cancer survivors of all ages from a clinical population, the top facilitator identified was “the information may help my family understand their cancer risk”; the top barriers identified were the perception of no benefit, since this population was already affected, and the cost of such services [13]. A national multicenter study in England conducted by Fraser et al. surveyed 162 men and women, both affected and unaffected with cancer, who were referred to one of five regional cancer genetics centers. They found clear differences in personal motivation for referral follow-through between those with and those without cancer and found the main motivation for attending clinic in those with a personal history of cancer was altruistic concern for their family members and children [17]. A unique study by Wakefield et al. recruited 39 adult family members of all ages with a family history of hereditary breast and ovarian cancer syndrome (HBOC) due to a genetic mutation in BRCA genes [14]. In this Australian study, the top facilitators for cancer genetic referrals were the desire for BRCA testing and having a strong family history of breast and/or ovarian cancer. The top barriers were lack of awareness of the BRCA mutation in their family and appropriateness of referral [14].
Two studies were conducted within the United States. Morgan et al. recruited 69 adult women of all ages at risk for HBOC who had received genetic counseling and risk assessment in Maine. In this US study, the top facilitators to receiving genetic counseling and risk assessment were having a family history of breast and/or ovarian cancer and having a personal history of cancer [15]. Barriers to services were not evaluated in this study. Pal et al. (2011) worked with the Florida state cancer registry to recruit 82 young black breast cancer survivors for genetic counseling and BRCA 1 and 2 genetic testing to demonstrate that young black women are interested in participating in genetic studies [18].
None of the studies above were carried out strictly on young women with breast cancer (under age 50 at diagnosis). Despite study efforts to obtain surveys prior to attendance at familial/high risk cancer clinics, the studies above used data from women who had already been referred for genetic risk assessment except for one study that used a hypothetical referral situation. None of these studies were able to evaluate the facilitators and barriers to accessing genetic services in a general patient population with unknown genetic referral status.
To our knowledge, this study is the first to look at the facilitators and barriers to referral for and receipt of genetic counseling and risk assessment in YBCS. It is also the largest of its kind to look at issues related to YBCS utilizing a US state cancer registry. For our study, facilitators are defined as internal and external motivating factors to receiving services, and barriers are defined as internal and external inhibiting factors to receiving services. The objective of this study is to examine the number of YBCS who self-report having been referred for genetic services (genetic counseling and risk assessment) and to determine the self-reported barriers and facilitators to receiving these services, within a representative state cancer registry sample.
2. Methods
2.1. Selection Process
The sampling frame included women between the ages 18–49 who were diagnosed with invasive and noninvasive breast cancer in the years 2006 or 2007 in the state of Michigan. The eligible population was selected from the Michigan Cancer Surveillance Program (MCSP) registry, which has a mandate to collect data from local reporting facilities on cases of cancer and other specified tumorous and precancerous diseases that occur in the state. The study team worked with MCSP to exclude women who were known to be deceased from the state vital records. Of the 3,911 YBCS diagnosed in 2006 and 2007, 500 women were selected by simple random selection from the eligible population. Prior to implementation, the Michigan Department of Community Health's Institutional Review Board and the MCSP's Scientific Advisory Board reviewed and approved the study.
2.2. Consent Process
The consent process consisted of three steps based on an existing standard method used by MCSP (Figure 1). The first step was MCSP notifying the local reporting facility regarding the YBCS survey and requesting information regarding the physician on record. MCSP then contacted the physician on record regarding the YBCS survey. Both were provided with the potential study participant's name and the physician on record was asked whether they knew of any reason that the selected participant should not be contacted such as death, mental illness, or illness due to current cancer treatments. If the local reporting facility and diagnosing physician confirmed their case and the physician did not indicate any medical contraindications, to MCSP contacting their patient, the participant was mailed the survey making up to three attempts to obtain a response.
Figure 1.
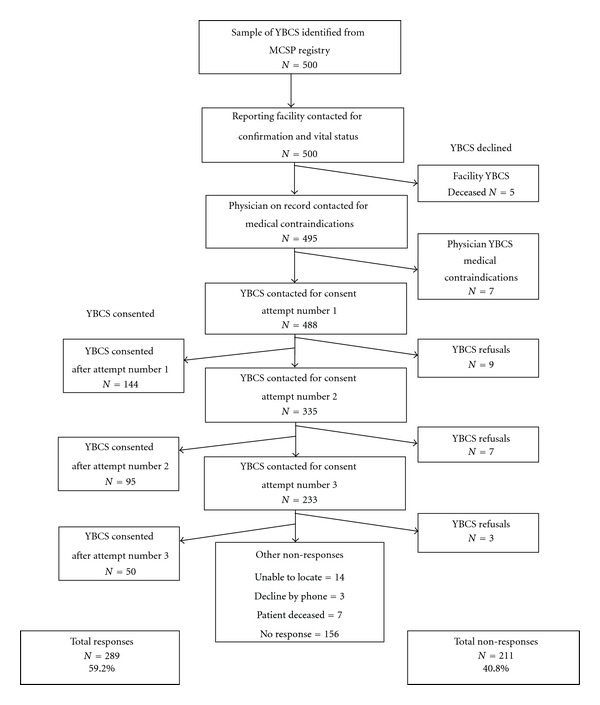
Flow chart of the selection and consent process.
The survey mailings included a personalized cover letter inviting participation and a postage-paid reply envelope. Due to budget constraints, the survey was in English only and was self-administered. The respondent was asked to sign an informed consent attached to the survey. Participants who returned a signed consent form and survey were mailed a $10 gift card. At all times, the participant's identifiable information was unavailable to the study team; only MCSP staff could identify the participants.
2.3. Survey Development
A review of available surveys was performed, and six surveys were obtained from several principle investigators of prior studies [20–25]. It was determined that no single prior tool was appropriate for our study in its entirety given the state-based, young survivor population and need for a self-administered mail survey; thus, a new tool was developed. Validated demographic questions from the National Behavioral Risk Factor Survey were used. The remaining questions were both adapted from the cited tools and created to fit our study methodology as a paper-based mail survey for young women that have survived a breast cancer diagnosis and to fulfill our study objectives.
The survey contained 31 questions, including fixed-choice and write-in response items. Within the survey “cancer genetic services” were defined for the patient (Box 1); this description was generated from several brochures and definitions and was meant to be a general description so that a patient might recognize whether they have had genetic counseling and risk assessment [26–29]. Respondents were asked if anyone had ever suggested that they go to cancer genetics services and if they ever received cancer genetic services. Based on this self-report, women who stated they had received services were asked about facilitators for receiving services (“please tell us why you decided to go for cancer genetics services?” and “please tell us what factors made it easier for you to go for cancer genetics services?”). The first question included fixed-choice responses related to psychological responses (to benefit my family, to reduce my cancer risk, etc.) and the second question addressed physical facilitators making it easier to go (e.g., time off work, transportation, and medical coverage). Women who stated they had not received services were asked about barriers to receipt (“Please tell us why you have not had cancer genetics services”). The main questions used to assess barriers and facilitators to receiving services were written by the study team; these questions and the fixed-choice response items for these questions are shown in the Appendix. Items included in the fixed-choice responses for both the barriers and facilitators were a collection of choices from the literature, expert opinion from the project steering committee members, and cancer survivors' input on the survey pilot (see below).
Box 1.
The definition of “cancer genetics services” provided to the YBCS in the survey instrument.
2.4. Survey Pilot
Survey drafts were extensively reviewed by the experts at MDCH Cancer Prevention and Control Section, the Centers for Disease Control Prevention Office of Public Health Genomics, MDCH Health Disparities, MDCH Disabilities, and the MDCH Project Steering Committee comprised of clinical geneticists, oncologists, genetic counselors, a health plan specialist, patient advocates, an advanced practice nurse, and epidemiologists.
The survey was piloted with four YBCS and one individual with a BRCA mutation. Pilot participants were asked to complete the survey in one sitting and track the length of time it took to complete. Following completion, they were asked to comment on any sections, questions, or answer choices that were unclear/unnecessary, uncomfortable, require different phrasing, require an alternative answer choice, or should be changed in some way. Several changes were made to question wording and survey format based on pilot responses, but overall survey length and content were retained.
2.5. Analysis
Response frequencies were assessed for differences between groups defined by demographic characteristics, socioeconomic characteristics, and family history of cancer. Two-sided Pearson chi-square tests were used to determine significant differences between subpopulations; P-values of <.05 were considered statistically significant. Multivariable logistic regression analysis was conducted to assess associations between demographic predictors and receipt of genetic counseling and risk assessment by using adjusted odds ratios with 95% confidence intervals. Likelihood chi-square tests were used to detect bivariate associations; P-values of <.05 were considered statistically significant. Demographic predictors in the analysis were employment, education, insurance, race, family history, and age at breast cancer diagnosis; all variables were categorical. Forward stepwise selection was used to populate the model. All analyses were conducted using PASW Statistics version 18.0 (IBM Corporation, NY, 2009).
3. Results
3.1. Sample Population
Five hundred women were sampled from the eligible population of 3,911 by MCSP. There were no statistically significant differences in age and racial characteristics between the sample and eligible population (Table 1). Based on local cancer registries and provider responses, 12 women were determined to be ineligible for the study, including five who were deceased and seven who had medical contraindications preventing contact (Figure 1).
Table 1.
Demographics of the young breast cancer survivors from the registry and the random sample that was selected for the study.
| YBCS population |
Sample population |
Respondent population |
Nonrespondent population | |
|---|---|---|---|---|
| N = 3,911 | N = 500 | N = 289 | N = 211 | |
| Age | 44.62 (20–49) | 43.02 (20–49) | 43.04 (26–49) | 43.01 (20–49) |
| Race | ||||
| White | 3,218 (82.3%) | 399 (79.8%) | 249 (86.2%) | 150 (71.1%) |
| Black | 531 (13.6%) | 69 (13.8%) | 24 (8.3%) | 45 (21.3%) |
| Other | 103 (2.6%) | 32 (6.4%) | 16 (5.5%) | 16 (7.6%) |
| Cancer stage | ||||
| Invasive | 2,915 (74.5%) | 358 (71.6%) | 204 (70.6%) | 154 (73.0%) |
| Noninvasive | 996 (25.5%) | 142 (28.4%) | 85 (29.4%) | 57 (27.0%) |
Surveys and consent documents were sent to the remaining 488 women in the sample. In total, 199 women who were sent surveys did not respond; 22 declined by phone or mail, 14 were unable to be located by mail, 7 were deceased, and 156 had no response, Figure 1. Surveys and signed consents were received from 289 women, for a response rate of 59.2%. The response rate from the black population (35.8%) was much lower than the response rate from the white population (64.0%) (data not shown).
Age, race, and cancer stage reported in the MCSP database was used to compare the respondent and nonrespondent populations. The racial distribution between these two populations was significantly different (P < .001) with blacks having a lower response rate than whites.
3.2. Demographics among Respondents
Respondents were primarily white (86.2%), employed for wages (56.1%), had private insurance (75.4%), had a college degree or higher (50.2%), and had a family history of breast and/or ovarian cancer in a first or second degree relative (53.3%) (Table 2). Mean age at breast cancer diagnosis was 43 years with a range of 26–49 years. Almost three-quarters of the YBCS had been diagnosed with invasive breast cancer in 2006 or 2007 (70.6%) (Table 1). Forty-three YBCS had more than one cancer diagnosis and 34 of them had a second breast cancer diagnosis (data not shown).
Table 2.
Demographics of YBCS respondents.
| Study population | Received genetic counseling | Did not receive genetic counseling | ||
|---|---|---|---|---|
| N = 289 (100%) | N = 122 (42.2%) | N = 158 (54.7%) | ||
| Age at diagnosis (yrs) | ||||
| 20–34 | 22 (7.6%) | 17 (13.9%) | 5 (3.2%) | P = .002 |
| 35–49 | 266 (92.0%) | 105 (86.1%) | 152 (96.2%) | |
| Race | ||||
| White | 249 (86.2%) | 110 (90.2%) | 132 (83.5%) | P = .205 |
| Black | 24 (8.3%) | 5 (4.1%) | 17 (10.8%) | P = .075 |
| Other | 16 (5.5%) | 7 (5.7%) | 9 (5.7%) | P = .995 |
| Employment* | ||||
| Employed for wages | 162 (56.1%) | 70 (57.4%) | 88 (55.7%) | P = .845 |
| Self-employed | 14 (4.8%) | 6 (4.9%) | 7 (4.4%) | P = .893 |
| Out of work | 15 (5.2%) | 5 (4.1%) | 10 (6.3%) | P = .503 |
| Unable to work | 32 (11.1%) | 11 (9.0%) | 18 (11.4%) | P = .383 |
| Other | 37 (12.8%) | 21 (17.2%) | 16 (10.1%) | P = .566 |
| Insurance (time of dx)** | ||||
| Private | 218 (75.4%) | 102 (83.6%) | 112 (70.9%) | P = .175 |
| Government | 15 (5.2%) | 5 (4.1%) | 9 (5.7%) | P = .660 |
| None | 11 (3.8%) | 2 (1.6%) | 7 (4.4%) | P = .173 |
| Multiple | 14 (4.8%) | 3 (2.5%) | 10 (6.3%) | P = .112 |
| Education | ||||
| High school diploma or less | 57 (19.7%) | 13 (10.7%) | 40 (25.3%) | P = .003 |
| Some college | 83 (28.7%) | 39 (32.0%) | 41 (25.9%) | P = .222 |
| College degree | 102 (35.3%) | 47 (38.5%) | 53 (33.5%) | P = .576 |
| Graduate degree | 43 (14.9%) | 21 (17.2%) | 22 (13.9%) | P = .351 |
| Family history of cancer*** | ||||
| Yes | 154 (53.3%) | 79 (64.8%) | 71 (44.9%) | P = .001 |
| No | 135 (46.7%) | 43 (35.2%) | 87 (55.1%) |
*Data missing for 29 respondents.
**Data missing for 31 respondents.
***Family history of breast or ovarian cancer in a first or second degree relative.
One hundred twenty-two respondents (42.2%) reported receiving genetic counseling and risk assessment. Compared to those who did not receive genetic counseling and risk assessment (n = 158), the women who received services were of a younger age (P = .002), higher education (P = .033), and were more likely to report having a family history of breast and/or ovarian cancer (P = .001) (Table 2).
Over half of the women (51.6%) who received genetic counseling and risk assessment perceived that the risk for breast cancer in their family was higher than other families, compared to 35.4% of women who did not receive genetic services (data not shown). Trouble keeping follow-up cancer treatment appointments was more frequent among women who did not receive genetic counseling and risk assessment (14.6%) than women who did receive genetic counseling and risk assessment (8.2%) (data not shown).
3.3. Predictors and Facilitators to Receiving Genetic Counseling and Risk Assessment
Among the 122 women who received genetic counseling and risk assessment, the most frequently cited reasons for going to genetic counseling and risk assessment were “benefit my family's future” (86.1%), followed by “wanted to know my future risk of cancer” (50.8%), “my doctor recommended that I go” (41.0%), and “may alter my cancer treatment” (39.3%) (Table 3).
Table 3.
Reasons for going to genetic counseling and risk assessment and factors that made it easier.
| n = 122 (42.2%) | |
|---|---|
| Reasons for going* | |
| Benefit my family's future | 105 (86.1%) |
| Wanted to know my future risk of cancer | 62 (50.8%) |
| My doctor recommended that I go | 50 (41.0%) |
| May alter my cancer treatment | 48 (39.3%) |
| Going seemed very important | 41 (33.6%) |
| Family members wanted me to go | 21 (17.2%) |
| Already knew of a familial mutation | 3 (2.5%) |
| Factors that made it easier to go** | |
| My medical insurance covered the visit | 83 (68.0%) |
| Clinic was close to home | 49 (40.2%) |
| Have available transportation | 49 (40.2%) |
| Clinic hours were flexible and fit my schedule | 30 (24.6%) |
| Have available childcare | 11 (9.0%) |
| I was able to obtain these services by phone | 2 (1.6%) |
*Among the 122 respondents who answered the question “please tell us why you decided to go for cancer genetics services”.
**Among the 122 respondents who answered the question “please tell us what factors made it easier for you to go for cancer genetics services?”.
On average YBCS reported 2.7 reasons that they went.
On average these women reported 1.8 reasons that made it easier for them to go.
Of the women who received services and mentioned that genetic counseling and risk assessment would benefit their family's future, 54.1% had a reported family history of breast and/or ovarian cancer.
Among women who received genetic counseling and risk assessment, the top three reported factors that made it easier to go for genetic counseling and risk assessment were “medical insurance covered the visit” (68.0%), “the clinic was close to home” (40.2%), and “have available transportation” (40.2%) (Table 3). Due to small sample sizes, it was not possible to explore differences in demographics.
Importantly, of the 122 women who received the genetic counseling and risk assessment, 121 were told or recommended by a health care professional or family member to go and one was never told about these services. The majority were told by an oncologist (48.4%) or surgeon (19.7%). A small number of women were told by their OB/GYN (4.9%), genetic counselor (4.9%), or family member (4.9%).
Of the 289 respondents, 50 were excluded from the multivariate logistic regression analysis due to missing data, leaving 239 cases in the analysis. In the final logistic regression model, family history of breast and/or ovarian cancer (odds ratio = 2.308, P-value = .002) and young age at the time of breast cancer diagnosis (odds ratio = 5.008, P-value = .006) were associated with receiving genetic services (Table 4). No further variables were added to the model because the parameter estimates changed by less than .001. The goodness of fit for this final model had a chi-square score of .001 with a P-value equal to .975, and the model accounted for 55.6% of the variation in the outcome.
Table 4.
Final logistic regression model for receiving genetic counseling and risk assessment.
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| B | P | Odds ratio | 95% CI | B | P | Odds ratio | 95% CI | |
| Family history | .860 | .001 | 2.362 | 1.399–3.988 | .837 | .002 | 2.308 | 1.353–3.938 |
| Age 20–34 | 1.627 | .006 | 5.088 | 1.607–16.108 | ||||
Hosmer and Lemeshow chi-square test = 0.001, P value = .975.
3.4. Barriers to Receiving Genetic Counseling and Risk Assessment
Among the 158 women who did not receive genetic counseling and risk assessment, the top barriers reported were “no one ever recommended it” (58.2%), “medical insurance coverage issues” (23.4%), “did not know they existed” (10.8%), and “worried a genetic test could be used against me” (9.5%) (Table 5). Among the 37 women who reported that medical insurance coverage issues were at least one reason they did not receive genetic counseling and risk assessment, 62.2% had private insurance, 13.5% were self-insured, 10.8% had no insurance, 5.4% had Medicare, and 2.7% had Medicaid coverage (data not shown). As mentioned above, when asked “Has anyone ever suggested that you should go for cancer genetics services?” 72.9% of women who did not receive genetic counseling and risk assessment reported that no one had recommended they do so. Yet only 58.2% of the women that did not receive genetic counseling and risk assessment reported it as a barrier when asked to list the reasons for not having cancer genetic counseling and risk assessment later in the survey.
Table 5.
Reasons for not having genetic counseling and risk assessment*.
| n = 158 (54.7%) | |
|---|---|
| No one ever recommended it | 92 (58.2%) |
| Medical insurance coverage issues | 37 (23.4%) |
| Did not know they existed | 17 (10.8%) |
| Worried a genetic test could be used against me | 15 (9.5%) |
| Too nervous | 6 (3.8%) |
| A doctor told me not to go | 5 (3.2%) |
| Lack of transportation | 4 (2.5%) |
| Other life arise that are more important | 4 (2.5%) |
| Too busy | 3 (1.9%) |
| Disability makes it difficult to carry out daily activities | 2 (1.3%) |
| Family members wouldn't want me to go | 2 (1.3%) |
*Among the 158 respondents who answered the question “please tell us why you have not had cancer genetics services?”.
The average number of barriers reported among these women was 1.2.
4. Discussion
This project marks the largest published report using a US state cancer registry to survey YBCS (diagnosed under age 50). This study documents patient-reported referral history for genetic counseling and risk assessment and facilitators and barriers to receiving those services. The use of a state cancer registry as a sampling frame is a unique method to recruiting YBCS and surveying them on their referral history for genetic counseling and risk assessment. This method provided results representative of a cancer survivor population, and the MCSP procedures proved to be effective, with nearly 60% of those contacted responding to a mail survey. We speculate that our strong response rate might be due to this population being so personally invested in the survey topic; several comments were written on the surveys with one woman stating, “Thank you. This is a very important topic.”
Previously published studies have used varying populations and survey methods to examine facilitators and barriers to receiving genetic counseling and risk assessment [13–17, 19]; however, our study that included 289 YBCS is the largest US study to date. Although Pal et al. (2011) used a similar sampling frame and found the same primary factor for being interested in cancer genetic counseling and testing among their 82 young black female participants (for the sake of their family members), their use of the state cancer registry in Florida was somewhat different than our use of the MCSP registry. Due to the nature of the Pal study with the involvement of DNA collection, recruitment methods were more extensive, involving eventual telephone contact to enroll patients and trained staff time [18]. For the purposes of data collection, the mail-only methods of our survey produced a higher response rate and would be easier and more economical for replication at other state cancer registries throughout the country.
4.1. Facilitators to Receiving Genetic Counseling and Risk Assessment
A common theme in Michigan and other studies was the role of the survivor's family in the decision to receive genetic counseling and risk assessment [13–18]. Michigan women reported “benefit my family's future” as their top reason for receiving genetic counseling and risk assessment. Other studies found similar motivating factors, including “helping the family understand their cancer risk” [13], “helping the family make better health decisions” [13], and “to better understand the risk of cancer in family members” [18].
“Wanting to know future risk of cancer” was the second most noted facilitator in this Michigan study, which is similar to previous studies [13, 16, 17]. Chin et al. found that the top reasons listed as motivators to attend breast cancer genetic clinics were “learning what to do to detect cancer early”, “learning how to reduce cancer risk”, and “understanding cancer risk” [13]. Brain et al.'s top motivator for attending a familial breast cancer clinic was “to find out about my risk” [16]. Identifying individuals at risk of developing a future cancer can have dramatic effects on early detection and cancer outcomes, which is one reason why genetic counseling and risk assessment are becoming a standard of care [9].
In previous studies, having a family history of breast and ovarian cancer was identified as a common reason for women with a personal or family history of breast cancer to go to genetic counseling and risk assessment [14, 15]. Our study was able to expand upon these findings to show that significantly more women with a family history of breast or ovarian cancer reported receiving genetic counseling and risk assessment than those that that did not have a family history. Based on our survey responses, it is unknown whether this family history was ever shared with a healthcare provider. This is an area for possible future exploration.
The role of a healthcare provider has been shown to be a strong facilitator for receiving genetic counseling and risk assessment [13, 15] and was seen in our study as the third most noted facilitator. Approximately three-quarters of the Michigan YBCS who were told to go to genetic counseling and risk assessment followed through with this recommendation. Chin et al. reported that 85% of breast cancer patients cited “if the doctor asked me to” would be an important motivator [13].
Given the influential role of healthcare providers in motivating patients to receive genetic counseling and risk assessment, there is a need for additional provider education regarding appropriate indications for cancer genetic referrals. A recent survey of primary care physicians showed that 87% were aware of BRCA genetic testing and 25% reported ordering a test in the last year; however, less than one-fifth correctly identified the low and high risk clinical scenarios they were given [9]. All of our study participants are appropriate for referral to genetic counseling based on age at diagnosis alone (under age 50 with breast cancer). However, over 40% report that their provider never recommended that they go. Our study clearly reinforces the need to educate providers regarding the potential benefits of genetic counseling and risk assessment for appropriate patients such as YBCS.
4.2. Barriers to Receiving Genetic Counseling and Risk Assessment
The most frequently reported barrier among the study population was that “no one had ever recommended” genetic counseling and risk assessment to the YBCS. Similarly, Fraser and colleagues reported that more than half of their patients were the first to raise the issue of their family history of cancer to their provider [17]. Lack of provider recognition of high risk family history is an important concern identified in this and other studies. Trivers et al. (2011) surveyed 3,200 US family physicians, general internists, and OB/GYNs and found that among high risk women, only 41% of physicians self-reported recognizing high risk women and adhering to referral recommendations for genetic counseling or testing. Providers have a harder time correctly identifying high-risk women (41% of the time they assess the patient risk correctly) compared to average-risk women (71% of the time they assess the patient risk correctly) [10]. Provider understanding and awareness can be improved through promotion of current evidence-based and nationally accepted practice guidelines on hereditary breast and ovarian cancer [3].
Our study found that YBCS without a family history of breast and/or ovarian cancer were less frequently receiving a referral for genetic counseling and risk assessment, although they are appropriate for referral based solely on age at diagnosis [3, 8, 28]. Additionally, YBCS in the 35–49-year-old age group were the most likely age group to be missed. It appears that being a YBCS of a younger age and/or having a family history of breast and/or ovarian cancer is more obvious to providers and more likely to prompt identification of a need for referral. It is not known if this is related to provider and/or patient motivators; this is another area in need of future research. It is possible that providers are more aware of indications for HBOC testing and are not aware of the broader indications for appropriate referral for cancer genetic counseling.
Medical insurance coverage issues were another factor influencing referral and receipt of genetic counseling in this study, both as a facilitator to receiving services and a barrier for not attending. Although the recent passage of the Affordable Care Act provides coverage by health insurers for those with a family history of breast and/or ovarian cancer [30], another potential area of future research is to compare our findings to countries with national health insurance for cancer survivors to receive genetic counseling and risk assessment.
With the success of reducing cancer mortality, there is now an increasing number of YBCS; this population has a unique and complex set of roles (i.e., patient, mother, worker, caregiver) with personal barriers such as lack of time due to family responsibilities and appointment fatigue [8]. In our study, it appears that the population who did not make it to genetic counseling and risk assessment also had a harder time making it to their cancer-related follow-up appointments. The use of a patient navigator model in cancer genetic referral has been suggested by Rahm et al. and could help to address this barrier and increase utilization [31].
The fourth most reported barrier to genetic counseling and risk assessment was “worried a genetic test could be used against me.” In 2008, the Genetic Information Non-Discrimination Act (GINA) was passed as a federal law and is currently enforced by various federal agencies [32]. GINA provides protection against discrimination in health coverage and employment on the basis of genetic information [32]. In order to address this barrier, additional patient and provider education about this federal protection would be of importance.
4.3. Limitations
Although the random sample was representative of Michigan YBCS, the response rate was significantly lower among blacks than whites (35.8% and 64.0% resp.), meaning that the generalizability of the results to other black YBCS women may be poor.
We do not have an explanation for this reduced response rate in our black population. According to Wendler et al. (2006), who carried out an extensive literature review of racial and ethnic minorities and their willingness to participate in health research, there are very small differences in the willingness of minorities to participate [33]. However, according to Simon and Petrucelli (2009), the literature suggests the presence of a number of barriers to the use of genetic services in the African American community, including lack of knowledge of genetics, adverse attitudes regarding genetics, and fears of racial discrimination [34]. MDCH will therefore be examining additional details about the non-respondents and the racial differences in the response rate in the future.
This study was meant to address all women with YBCS. However, 12 women were deceased and could not participate in our study. It is not known if referral for cancer genetic counseling and risk assessment was ever received.
Another limitation was that the survey was only offered in English. However, in Michigan, the number of individuals who do not speak and understand English is lower than the national average (Michigan 3.2% of population versus US 8.1% of population) [35].
A batch of surveys was mailed out that was missing a page of the survey. That page included questions on employment, insurance, and race. These women were sent the missing page asking them to return it. However, 29 women did not return it; therefore, the demographic information is missing on several women.
Due to the cross-sectional nature of the survey, there may have been response bias wherein women who had been to cancer genetic services prior to taking the survey were more likely to participate. In addition, women who had a family history of cancer may have been more likely to remember having received cancer genetic services. A prospective study starting at the time of diagnosis would be the best method to examine YBCS' perception of the importance of cancer genetic services and the facilitators and barriers to receipt of such services. Also, an analysis that includes likelihood for HBOC based on pathology and extensive family history would be beneficial for future studies.
5. Conclusions
This is the first study that provides community-based information about barriers and facilitators to obtaining genetic counseling and risk assessment among YBCS. Results point to the need for promotion and education outreach to providers about the national guidelines and the importance for referral to genetic counseling and risk assessment. Provider practice could also be enhanced through policies that encourage appropriate genetic counseling and risk assessment referrals and through creation and dissemination of patient and provider cancer genetic resources and tools for risk assessment and referral. The results also indicate a need for increased service promotion to YBCS on what is available to them and how the cost of the services can be covered. Policies to improve use and access to genetic counseling and risk assessment need to be explored and initiated to help detect cancer earlier and reduce mortality.
Acknowledgments
The authors would like to thank Donna Genei of the Michigan Cancer Surveillance Program at the Michigan Department of Community Health for her assistance in this project. This work was supported by Cooperative Agreement no. 5U38GD000054 from the Centers for Disease Control and Prevention (CDC), Office of Public Health Genomics. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
Appendix
Survey Instrument Questions Used in This Article Related to Receiving Genetic Counseling and Risk Assessment
-
Has anyone ever suggested that you should go for cancer genetics services?
-
□Yes
-
□No
-
□Don't know
-
□
-
Have you ever had cancer genetics services?
-
□Yes
-
□No
-
□Don't know
-
□
-
Please tell us why you have not had cancer genetics services? (Check all that apply)
-
□No one ever recommended it
-
□Too busy
-
□Cannot get time off from work
-
□Disability makes it difficult to carry out daily activities
-
□Lack of transportation
-
□Lack of child care
-
□Clinic hours do not fit my schedule
-
□Medical insurance coverage issues (no coverage or out-of-pocket cost is too high)
-
□Other life issues that come up are more important than an appointment
-
□Worried a genetic test result could be used against me (i.e., by employer or for future health insurance, etc.)
-
□Clinics are too far away
-
□Feeling sick from cancer treatments
-
□Too nervous (i.e., don't want to know the risk of inherited cancer)
-
□Family members would not want me to go
-
□Cultural and/or religious beliefs do not support genetic testing
-
□Did not know they existed
-
□A doctor told me not to go
-
□Other: …
-
□
-
Please tell us why you decided to go for cancer genetics services? (Check all that apply)
-
□Benefit my family's future
-
□May alter my cancer treatment (preventive surgery, chemotherapy, etc.)
-
□Wanted to know my future risk of cancer
-
□Already knew someone in my family has a cancer causing gene-change
-
□Going seemed very important
-
□Family members wanted me to go
-
□My doctor recommended that I go
-
□Other: …
-
□
-
Please tell us what factors made it easier for you to go for cancer genetics services? (Check all that apply)
-
□Clinic was close to home
-
□Have available transportation
-
□Have available childcare
-
□Clinic hours were flexible and fit my schedule
-
□I was able to obtain these services by phone
-
□My medical insurance covered the visit (minimal charge to me)
-
□Other: …
-
□
References
- 1.Ruddy KJ, Gelber S, Shin J, et al. Genetic testing in young women with breast cancer: results from a Web-based survey. Annals of Oncology. 2009;21(4):741–747. doi: 10.1093/annonc/mdp355. [DOI] [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Annals of Internal Medicine. 2005;143(5):355–361. doi: 10.7326/0003-4819-143-5-200509060-00011. [DOI] [PubMed] [Google Scholar]
- 3.National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. Genetic/Familial High-Risk Assessment: Breast and Ovarian. 2011, http://www.nccn.org/index.asp.
- 4.Centers for Disease Control and Prevention Division of Cancer Prevention and Control. 2012, http://www.cdc.gov/cancer/dcpc/about/
- 5.Miedema B, Easley J. Barriers to rehabilitative care for young breast cancer survivors: a qualitative understanding. Supportive Care in Cancer. 2011:1–9. doi: 10.1007/s00520-011-1196-7. [DOI] [PubMed] [Google Scholar]
- 6.Pronzato P, Mustacchi G, De Matteis A, et al. Biological characteristics and medical treatment of breast cancer in young women — A featured population: results from the NORA study. International Journal of Breast Cancer. 2011 doi: 10.4061/2011/534256.534256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riley BD, Culver JO, Skrzynia C, et al. Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. Journal of Genetic Counseling. 2012;21:151–161. doi: 10.1007/s10897-011-9462-x. [DOI] [PubMed] [Google Scholar]
- 8.American College of Surgeons Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient-Centered Care. 2012, http://www.facs.org/cancer/coc/cocprogramstandards2012.pdf.
- 9.Bellcross CA, Kolor K, Goddard KAB, Coates RJ, Reyes M, Khoury MJ. Awareness and utilization of BRCA1/2 testing among U.S. Primary Care Physicians. American Journal of Preventive Medicine. 2011;40(1):61–66. doi: 10.1016/j.amepre.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 10.Trivers KF, Baldwin LM, Miller JW, et al. Reported referral for genetic counseling or BRCA 1/2 testing among United States physicians: a Vignette-Based Study. Cancer. 2011;117(23):5334–5343. doi: 10.1002/cncr.26166. [DOI] [PubMed] [Google Scholar]
- 11.Sweet KM, Bradley TL, Westman JA. Identification and referral of families at high risk for cancer susceptibility. Journal of Clinical Oncology. 2002;20(2):528–537. doi: 10.1200/JCO.2002.20.2.528. [DOI] [PubMed] [Google Scholar]
- 12.Robson ME, Storm CD, Weitzel J, Wollins DS, Offit K. American Society of Clinical Oncology Policy Statement update: genetic and genomic testing for cancer susceptibility. Journal of Clinical Oncology. 2010;28(5):893–901. doi: 10.1200/JCO.2009.27.0660. [DOI] [PubMed] [Google Scholar]
- 13.Chin TM, Tan SH, Lim SE, et al. Acceptance, motivators, and barriers in attending breast cancer genetic counseling in Asians. Cancer Detection and Prevention. 2005;29(5):412–418. doi: 10.1016/j.cdp.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Wakefield CE, Ratnayake P, Meiser B, et al. ‘For all my family’s sake, i should go and find out’: an Australian report on genetic counseling and testing uptake in individuals at high risk of breast and/or ovarian cancer. Genetic Testing and Molecular Biomarkers. 2011;15(6):379–385. doi: 10.1089/gtmb.2010.0158. [DOI] [PubMed] [Google Scholar]
- 15.Morgan D, Sylvester H, Lucas FL, Miesfeldt S. Cancer prevention and screening practices among women at risk for hereditary breast and ovarian cancer after genetic counseling in the community setting. Familial Cancer. 2009;8(4):277–287. doi: 10.1007/s10689-009-9242-z. [DOI] [PubMed] [Google Scholar]
- 16.Brain K, Gray J, Norman P, et al. Why do women attend familial breast cancer clinics? Journal of Medical Genetics. 2000;37(3):197–202. doi: 10.1136/jmg.37.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraser L, Bramald S, Chapman C, et al. What motivates interest in attending a familial cancer genetics clinic? Familial Cancer. 2003;2(3-4):159–168. doi: 10.1023/b:fame.0000004621.38109.16. [DOI] [PubMed] [Google Scholar]
- 18.Pal T, Rocchio E, Garcia A, Rivers D, Vadaparampil S. Recruitment of black women for a study of inherited breast cancer using a cancer registry-based approach. Genetic Testing and Molecular Biomarkers. 2011;15(1-2):69–77. doi: 10.1089/gtmb.2010.0098. [DOI] [PubMed] [Google Scholar]
- 19.Rolnick SJ, Rahm AK, Jackson JM, et al. Barriers in identification and referral to genetic counseling for familial cancer risk: the perspective of genetic service providers. Journal of Genetic Counseling. 2011;20(3):314–322. doi: 10.1007/s10897-011-9351-3. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. National Health Interview SurveyQuestionnaire: Cancer Control Module (Healthy People 2010). Hyattsville, MD. 2000, ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2000/qcancerx.pdf.
- 21.Michigan Department of Community Health, Children's Special Health Care Services, Region 4 Genetics Collaboration. Clinical Genetic Services: A View from Michigan's Children's Special Health Care Services' (CSHCS) Families Questionnaire. Michigan. 2009.
- 22.Michigan Chronic Disease Epidemiology Section. Michigan Behavioral Risk Factor Survey (MiBRFS) Demographic content. Obtained through personal communication, 2010.
- 23.University of Maryland Survey Research Center. Genetic Technology and Health. Project #1389 Questionnaire. January. 2001 Obtained through personal communication.
- 24.Informed Medical Decisions. Breast Cancer Questionnaire. Draft. Obtained through personal communication, 2010.
- 25.Michigan Public Health Institute, Michigan Department of Community Health, and Michigan Cancer Consortium Prostate Cancer Action Committee. Prostate Cancer Survivors Follow-Back Study [Ph.D. thesis] Personal Communication; 20092010. [Google Scholar]
- 26.Michigan Cancer Genetics Alliance & Michigan Cancer Consoritum. Position Paper for Health Care Providers: Testing for Hereditary Cancer Predisposition Syndromes and Genetic Counseling. 2011, https://www.migeneticsconnection.org/cancer/MCGAPositionStatement2009.pdf.
- 27.Michigan Cancer Genetics Alliance. Guide to the Genetic Counseling Process. 2011, http://www.migeneticsconnection.org/cancer/intro_2.html.
- 28.National Cancer Institute. Cancer Genetics Risk Assessment and Counseling. 2011, http://www.cancer.gov/cancertopics/pdq/genetics/risk-assessment-and-counseling/HealthProfessional/page1.
- 29.Facing Our Risk of Cancer Empowered. Assessing your Risk/Genetic Counseling. 2011, http://www.facingourrisk.org/info_research/hereditary-cancer/risk/index.php.
- 30.Patient Protection, Affordable Care Act of 2010. public law 111-148, 111th Cong., 2d session, 2010.
- 31.Rahm AK, Sukhanova A, Ellis J, Mouchawar J. Increasing utilization of cancer genetic counseling services using a patient navigator model. Journal of Genetic Counseling. 2007;16(2):171–177. doi: 10.1007/s10897-006-9051-6. [DOI] [PubMed] [Google Scholar]
- 32.Genetic Information Non-Discrimination Act of 2008. H.R. 493, 110th Cong. 2007–2008.
- 33.Wendler D, Kington R, Madans J, et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Medicine. 2006;3(2):201–210. doi: 10.1371/journal.pmed.0030019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simon MS, Petrucelli N. Hereditary breast and ovarian cancer syndrome: the impact of race on uptake of genetic counseling and testing. Methods in Molecular Biology. 2009;471:487–500. doi: 10.1007/978-1-59745-416-2_25. [DOI] [PubMed] [Google Scholar]
- 35.United States Census Bureau. Language Use and English-Speaking Ability: 2000 Census. 2000, http://www.census.gov/prod/2003pubs/c2kbr-29.pdf.