Abstract
Study design:
Retrospective clinical study of patients treated for subaxial cervical spine trauma (SCST) at a tertiary medical center.
Purpose:
Evaluate the validity of the Subaxial Injury Classification (SLIC) system in surgical versus non-surgical decision making for SCST.
Inclusion criteria:
Age >12 years, presence of SCST with complete clinical and radiological (CT and MRI) data.
Exclusion criteria:
Patients with incomplete radiographic or clinical data, pathological fractures, isolated upper cervical trauma (occiput to C2), isolated transverse process or spinous process fractures, chronic or age indeterminate fractures, isolate MRI findings, and severe systemic trauma with death prior to either surgical or non-surgical treatment.
Results:
Fourteen patients were treated non-surgically (C), whereas 24 were treated surgically (S). In the C group, the SLIC score ranged from 0 to 5 points (standard deviation [SD] = 1.20 points; mean 1.07; median 1). Just 1 patient had an SLIC score greater than 2 (7.1% of the patients). In the S group, the SLIC score ranged from 1 to 10 points (standard deviation [SD] = 2.03 points; mean 5.6; median 6). Just 2 patients had an SLIC score smaller than 4 (both with 1 point each, 8.3% of the total group). All the other 22 (accounting for 91.6%) patients had an SLIC of 4 or more points.
Conclusions:
Our study suggests that the SLIC classification looks to be a promising system to aid spinal surgeons in the decision-making process of subaxial cervical trauma, but a large prospective cohort study is required.
Keywords: Cervical spine trauma, classification, injurity severity score, spinal cord injury
INTRODUCTION
Many classification schemes have been developed to guide clinical and surgical treatment of subaxial cervical spine trauma (SCST). Many of these systems represent milestones in the understanding of cervical trauma including the Holdsworth classification, the first comprehensive system for spinal column injuries.[1] Subsequent schemes like by Allen and Ferguson, in 1982, and its modified version proposed by Harris et al. in 1986, were also important advancements.[2,3] However, despite the comprehensive nature of these systems, their ultimate use has been limited because they are based on a presumed mechanism of injury based on plain radiographs without consideration of the supporting ligaments to maintain spine stability or the patient's neurological status.
Due to this fundamental deficiency, the systems lack practicality and clinical relevance and the associated terminology has been ineffective in describing precise traumatic conditions of the subaxial spine. With limitations in the classification of cervical trauma, it is difficult to standardize or compare different treatment approaches.
Treatment of SCST is based on a number of variables, including fracture pattern, suspected mechanism of injury, spinal alignment, neurologic injury, and expected long-term stability. Based on this, the Spine Trauma Study group proposed the Subaxial Injury Classification (SLIC) scoring system.[4] This scoring system proposes 3 major injury characteristics as indicators, which would direct the treatment of subaxial injuries.[5,6] These 3 characteristics are: (1) injury morphology as determined by the pattern of spinal column disruption on available imaging studies, (2) integrity of the discoligamentous soft tissue complex (DLC) represented by both anterior and posterior ligamentous structures as well as the intervertebral disc, and (3) neurologic status of the patient. These 3 injury characteristics are widely recognized as predictors of clinical outcome and influence treatment recommendations. Within each of the 3 categories, subgroups have been identified and graded from least to most severe. The SLIC classification divides injury morphology into 3 main categories referenced to the relationship of the vertebral bodies with each other (anterior support structures): (0) no abnormality, (1) compression, (2) distraction, and (3) translation or rotation. The components of the DLC include the intervertebral disc, anterior and posterior longitudinal ligaments, interspinous ligaments, facet capsules, and ligamentum flavum. The integrity of these soft tissue constraints is directly proportional to spinal stability and is classified within the SLIC system as disrupted, intact, or indeterminate. Neurologic injury is the third component of the SLIC system and is inherently an important indicator of the severity of spinal column injury and may be the single most influential predictor of treatment. As such, the presence of an incomplete neurologic injury, particularly in the presence of ongoing root or cord compression leads to the highest point score. Additionally, confounding factors can influence the treatment decision including the presence of ankylosing spondylitis, diffuse idiopathic hyperostosis, osteoporosis, previous surgery, and degenerative disease.[4]
Surgical versus non-surgical treatment is suggested by a threshold value of the SLIC severity score. If the total score is <4 (that is, 1-3), non-operative treatment is recommended.[4] If the total is ≥5, operative treatment is recommended. This treatment may consist of realignment, neurological decompression (if indicated), and stabilization.[4] Cases with a total score of 4 may be treated either operatively or non-operatively based upon surgeon and patient preferences.
Given the potential benefits of this new system, clinical assessment of the SLIC system is needed. The purpose of this study is to evaluate the safety of the SLIC system in surgical versus non-surgical decision-making for subaxial cervical trauma.
MATERIALS AND METHODS
A retrospective review of the trauma database at the University of Utah, from 2000 to 2010 was performed. The institution is a tertiary, level 1 trauma center that treats over 1500 trauma patients a year. Patients treated either surgically or non-surgically for acute, subaxial cervical spine trauma (from C3 to C7) were identified by ICD-9 codes for cervical injuries or spinal cord injury. Inclusion criteria included patient's age (>12), presence of subaxial cervical injury, and complete radiological and clinical data. The medical records and radiological data were considered adequate when the 3 injury characteristics of the SLIC could be scored, with a CT scan or a CT and MRI. Age criterion (>12 years old) was determined by the lower age limit of the University trauma database. Exclusion criteria included: incomplete radiographic or clinical data, pathological fractures (infection, cancer), isolated upper cervical trauma (occiput to C2), isolated transverse process or spinous process fractures, chronic or age indeterminate fractures, isolate MRI findings, and severe systemic trauma with death prior to either surgical or non-surgical treatment.
Demographic data including age and gender were recorded. Initial injury details were recorded including trauma etiology, injury level, and neurological status. The injuries were classified according to the SLIC system at the most severely injured level. The SLIC was scored by two of the authors (AFJ, AAP), a board-certified neurosurgeon and board-certified orthopedic surgeon, respectively. Among patients with uncertain SLIC classification, consensus was obtained. The patients were classified according to neurological status, the injury morphology, integrity of the discoligamentous complex, and the total SLIC score. Neurological status was scored as complete, incomplete, or intact as well as according to the American Spinal Injury Association (ASIA) score. Patients with severe myelopathy and/or acute central cord syndrome were classified as having incomplete spinal cord injuries. Confounding factors (e.g., ankylosing spondylitis, diffuse idiopathic hyperostosis, osteoporosis, previous surgery, and degenerative disease) were noted if present. Cases examples are shown in Figure 1 and 2
Figure 1.
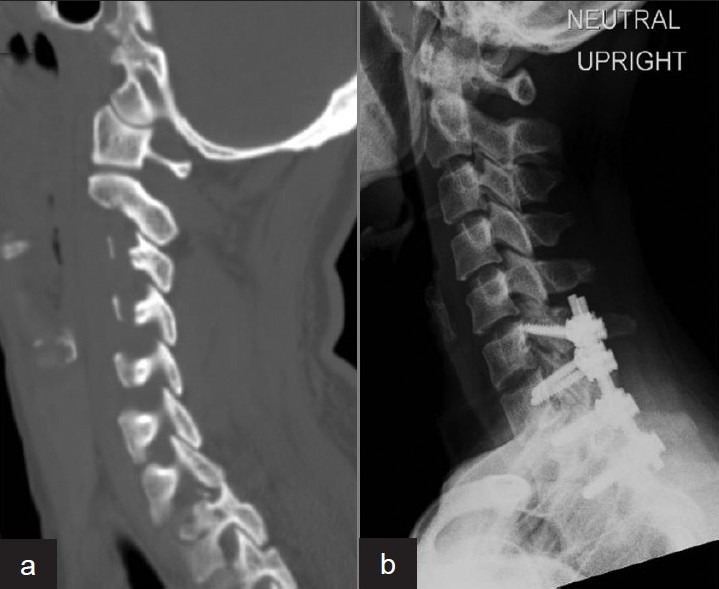
A 36-year-old woman presented after a motor vehicle collision. A unilateral locked facet at C7-T1 is demonstrated in the CT reconstruction (a). The patient had no neurological injury. SLIC score: 4 points for injury morphology (translation/rotation); 2 points for disruption of the discoligamentous complex and 0 points for neurological status; total of 6. Surgical treatment was chosen, with a posterior instrumentation and fusion C6 to T2 (b)
Figure 2.
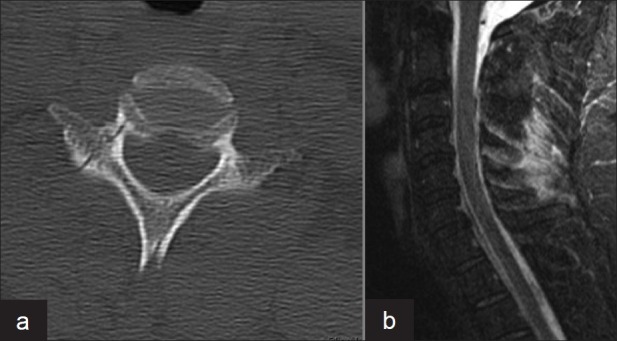
A 44-year-old man presented after a motor vehicle accident. A unilateral right C7 pedicle fracture is seen on the CT scan (a). The patient is neurologically intact. The MRI showed a hyper-intense signal at the region of the interspinous and supraspinous posterior ligaments suggesting potential ligamentous injury (b). SLIC score: 0 points for injury morphology; 1 point for suspect injury of the discoligamentous complex and 0 points for neurological status; total of 1. Non-surgical treatment was chosen
Retrospective outcomes of treatment during follow-up were recorded as well as complications (neurological deficit, conversion to operative treatment, surgical complications). Institutional review board committee approval was obtained prior to initiation of the study. There was no external funding source for this study.
RESULTS
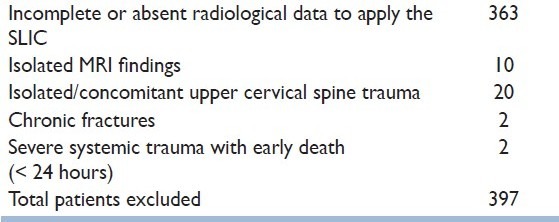
From an initial database of 435 patients, we included only 38 patients in our study excluding 397 patients [Table 1]. Most of the patients were excluded (363) due to incomplete or absent radiological data, which precludes obtaining the SLIC score. Of those patients who were included, 14 were treated conservatively (C), whereas 24 were treated surgically (S). Although the SLIC system was published in 2007, there was no mention in the medical records about its direct use by any surgeon in the decision-making process.
Table 1.
Patient distribution according to the criteria of exclusion
Non-surgical treatment group
Of the 14 patients in the non-surgical group, age ranged from 20 to 79 years (standard deviation [SD] = 15.64 years; mean 41.1; median 43) with a mean follow-up of 4.6 months (range, 1.5-15 months). Twelve (85.7%) were male, and 92.8% of the trauma was caused by motor vehicle accidents with one case of a snowboarding accident. The characteristics of the patients according to age, sex, site (as distraction and translational lesions involved 2 levels, we described the superior one as the injured level), and ASIA and SLIC scores are shown in Table 2.
Table 2.
Characteristics of 14 patients with cervical fractures treated conservatively according to age, sex, location of the injury, ASIA, and SLIC
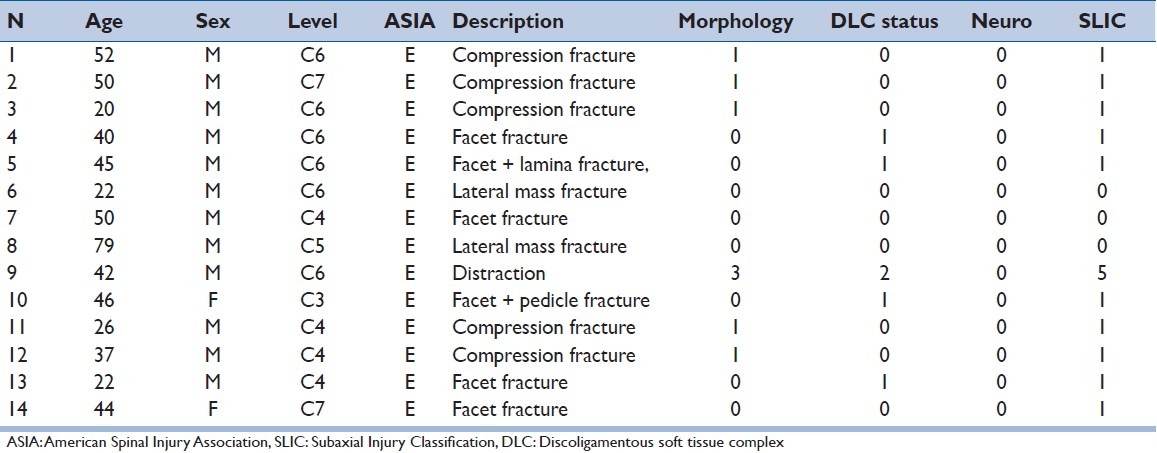
The SLIC score ranged from 0 to 5 points (standard deviation [SD] = 1.20; mean 1.1; median 1). Of the 14 patients, just 1 had an SLIC score greater than 3. The other 13 patients (accounting for 92.9%) had an SLIC of 0 or 1 points, matching with the reported SLIC algorithm. Most of these patients had small, non-displaced fractures in the facet joints, lateral mass or small vertebral body fractures. No confounding factors were identified in this group. Of the 14 patients, all 14 were ASIA E. All patients were treated with a rigid cervical orthosis between 6 and 12 weeks. There were no changes in the ASIA score at the latest follow-up. The only patient with score greater than 3 had a translational injury (“perched” facet) with an SLIC score of 5. His severe, but survivable, head injury precluded surgical management. He was maintained in a cervical orthosis for 6 weeks. Follow-up radiographs revealed persistent translational deformity. The patient demonstrated no improvement from his head injury and was discharged 1 month after the injury in a persistent vegetative state without subsequent surgical treatment of his cervical spine injury.
Of the 14 patients, 9 (64.2%) had follow-up after hospital discharge, with a mean follow-up of 4.7 months (median of 3 months).
The SLIC system accurately predicted treatment in 92.8% of the patients in this group. The only divergence (SLIC score of 5) was associated with a severe concomitant injury precluding surgical management, an important factor in the decision-making process.
Surgically treated group
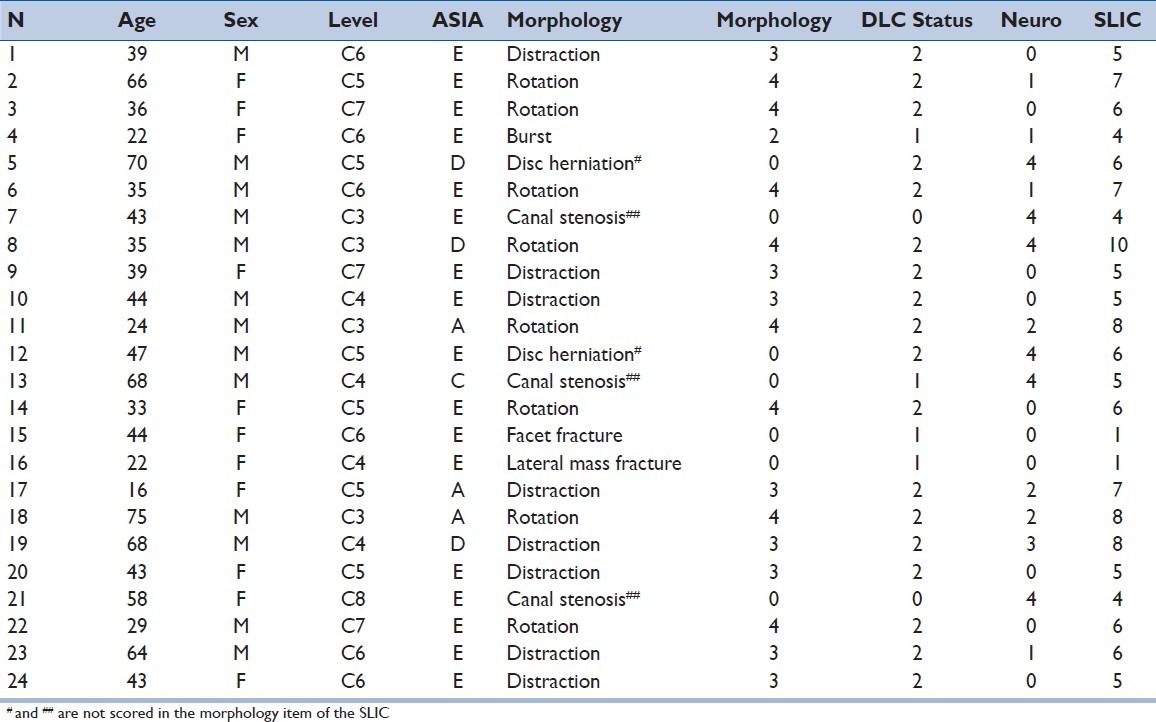
Of the 24 patients in the surgical group, age ranged from 16 to 75 years (standard deviation [SD] = 17 years; mean 44.3; median 43) with a mean follow-up of 7.7 months (range, 2–60 months). Eleven (45.8%) were male and the main cause of the trauma was motor vehicle accidents. The characteristics of the patients according to age, sex, location of the injured level (as distraction and translational lesions involved 2 levels, we described the superior one as the injured level), ASIA grade, and SLIC score are shown in Table 3.
Table 3.
Characteristics of 24 patients with cervical fractures treated surgically according to age, sex, location and morphology of the injury, and ASIA and SLIC score system
Six patients (5 neurologically intact and 1 with a complete neurological deficit) underwent closed traction reduction before surgery, all with a successful closed reduction. No changes in neurological status were seen after traction reduction in any of the patients. Fourteen (58.3%) had surgery within the first 24 hours after the trauma; 12 were treated by an anterior approach, 9 by a posterior, and 3 by a combined approach.
The SLIC score in this group ranged from 1 to 10 points (standard deviation [SD] = 2.03; mean 5.6; median 6). Twenty-two (91.7%) patients had an SLIC score of 4 or more points, matching proposed treatment with actual treatment. Of the 24 patients, only 2 (8.3%) had an SLIC score less than 4. One patient sustained a non-displaced facet fracture (SLIC score of 1) and 1 patient had a non-displaced lateral mass fracture (SLIC score of 1); both patients were neurologically intact. Three patients had evidence of severe spondylotic disease with spinal stenosis, a significant confounding factor. Two patients (5 and 12 in Table 3) with traumatic disc herniations were reported with a DLC score of 2 (i.e., disrupted).
Of the 24 patients, 19 (79.1%) had follow-up after hospital discharge, with a mean follow-up of 7.8 months (median of 3 months).
Preoperatively, 3 (12.5%) patients were ASIA A, 1 was ASIA C (4.1%), 3 were ASIA D (12.5%), and 17 were ASIA E (70.8%). Four patients [5, 7, 13, and 21 in Table 3] labeled as ASIA E (no sensation or motor function impairment) had neurological symptoms on presentation: bilateral numbness, neuropathic pain and tingling in both arms in 3 patients, and additional loss of dexterity and gait imbalance in 1 patient. All 4 patients were over 40 years with 3 having concomitant cervical degenerative disease and spinal stenosis. Despite their ASIA E status, these patients were assigned a neurological injury score of 4 (incomplete spinal cord injury 3 points plus 1 point for continuous cord compression in the setting of a neurological deficit). After treatment, all the patients maintain their ASIA status, except 1 patient who improved from D to E after 3 months of follow-up.
Complications in this group included postoperative wound infection after instrumented posterior cervical fusion in 2 patients (both neurologically intact). Two patients with complete tetraplegia required tracheostomy and developed systemic infection (sepsis) from non-spinal sources. One of these patients also had a deep venous thrombosis. There was no death in this group of patients.
DISCUSSION
As noted by the system creators,[4] the SLIC severity scale attempts to provide a utilitarian classification for the treatment of the subaxial cervical trauma, by accounting for the injury morphology, injury to the intervertebral disc and supporting ligaments, and the patient's neurological status. Our series demonstrates that the SLIC-proposed treatment matches the actual treatment administered in 92.1% of the patients. Among the 14 patients in the non-surgical group, considering a score of 4 or less as concordant with closed treatment, a 92.9% rate of concordance was reached. The sole outlier was an individual with an SLIC score of 5 who was treated conservatively due to the presence of severe traumatic brain injury. The surgical group, including patients with an SLIC score of 4 points or more, also demonstrated a very high concordance rate of 91.7%.
While the SLIC score demonstrated high agreement with both surgical and non-surgical management, there were noted limitations in its application. At the extreme ends of the spectrum of injury, such as compression and translational morphologies, the SLIC system is readily applied. However, certain injury patterns can be more difficult to classify. For example, in this series, 3 patients presented with acute injury in the setting of pre-existing cervical spondylosis and stenosis. We additionally noted 2 patients with traumatic disc herniations. The current SLIC injury morphology category does not specifically score these patterns. While the DLC and neurological status categories may allow for patient classification, this may be a point of confusion. Another limitation was identified with regard to details of the DLC injury. Specific MRI findings were often influential in the surgical decision process: the locality of compression (anterior or posterior), the extent and cause (traumatic disc herniation versus degenerative spondylolisthesis). In circumstances where the injury morphology was lacking, details of the DLC injury are not sufficiently documented to guide treatment.
We summarize these and other situations to exemplify these problems, suggesting that a more precise description score is needed for them, possibly leading to a more reproducible pattern between surgeons.
Neurological deficit score
As previously stated in the Methods section, we suggested that all the patients with signs of spinal cord dysfunction, such as bilateral paresthesias, loss of motor dexterity, balance problems but without traditional measures of impairment in motor strength or sensorial function should be scored as having an incomplete spinal cord injury. These individuals would be identified as ASIA E (“intact”) but nonetheless have a functional neurological impairment. These patients, therefore, are more deserving of a higher weighted score. Given the lack of high-quality evidence in the treatment of central cord injury and acute myelopathy, classifying these individuals with a lower neurological score may be historically consistent but, nonetheless, inaccurate.
Traumatic disc herniation
We suggest that patients with extruded traumatic disc herniation with signs of spinal cord dysfunction should receive a score of 6 (0 for morphology, 2 for DLC disrupted, 3 for incomplete neurological deficit, and + 1 for ongoing cord compression). This is in line with the aforementioned discussion of central cord injury/acute myelopathy as well as the DLC disruption that goes along with this injury pattern. Patients with a disc protrusion may be considered to have an indeterminate DLC injury and, as such, receive a score of 1.
Cervical spinal stenosis without evident fracture
Patients with cervical stenosis in the setting of new neurological deficits and with evidence of spinal cord compression on MRI but without evidence of fracture, distraction, or translational injury can be assessed as SLIC 4 (0 for morphology, 3 for incomplete deficit, and + 1 for persistent cord compression). This is the typical clinical picture of an individual with central cord syndrome or acute myelopathy. A score of 4 identifies that either surgical or non-surgical options may be a choice with treatment individualized to the patient and physician. This is concordant with the current uncertainty in the acute management of central cord syndrome and acute myelopathy.
Degenerative spondylolisthesis
Degenerative spondylolisthesis suspected by the presence of facet joint arthritis or osteophytes and without signs of acute fracture or translational injury should be scored as 0 for morphology. At times it may be difficult to distinguish chronic from acute spondylolisthesis. Older patients and those with degenerative findings may suggest a chronic condition. Younger patients, those without degenerative changes, and those with CT or MRI evidence of acute ligamentous injury or pre-vertebral edema suggest an acute condition.
Nondisplaced, unilateral facet fracture
Another important limitation of the score is with regard to small unilateral facet fractures without instability. Most of these lesions, when isolated, will be scored in the SLIC as non-operative (no injury morphology, intact DLC, intact neurology). Details of the facet fracture (fracture height, percent of surface area, percent of lateral mass), not addressed by the SLIC system, have been suggested to predict outcome of non-surgical management. Furthermore, there is some evidence that these lesions can have better outcomes when surgically treated when considering pain and disability than when conservative treatment is performed.[7] The SLIC system, therefore, may incompletely classify this injury pattern.
Magnetic resonance imaging
Lastly, the SLIC system does include MRI as part of the classification and can influence the decision-making process by inferring the status of the DLC. Until recently, there has been no good evidence to clarify its role. Recently, the correlation between the MRI and the intraoperative status of the posterior portion of the DLC was investigated in a well-designed, prospective study comparing the surgical findings, during posterior cervical approaches to treat cervical spine injuries, and preoperative MRI findings. The authors concluded that MRI may overestimate the injury of the DLC, possibly leading to unnecessary surgery.[8] Malham et al., in 2009, retrospectively evaluated 31 consecutive patients who underwent anterior surgery for stabilization after traumatic discoligamentous injury of the cervical spine.[8] The authors attempted to establish a correlation between MRI findings and surgically verified disruption of the anterior longitudinal ligament (ALL), intervertebral disc, and posterior longitudinal ligament (PLL). The kappa values for ALL, intervertebral disc, and PLL disruption measured 0.22, 0.25, and 0.31, respectively. Although MRI provided reasonable sensitivity to disc disruption (0.81), it had only poor sensitivity to ALL (0.48) and PLL (0.50) injury. The specificity obtained for ALL and PLL disruption was 1.00 and 0.87, respectively, but 0.00 for disc disruption. The authors concluded that the ability of cervical MRI to detect surgically verified injury to the ALL, intervertebral disc, and PLL varied according to the structure evaluated. They also demonstrated high false-negative rates for ALL and PLL injury and high false-positive rates for disc disruption.[9] The literature would therefore suggest that MRI be used cautiously in the medical decision-making process.
Limitations
Our study is limited by its sample size, single center, retrospective nature, and the limited clinical follow-up of the subjects. While we can demonstrate some validity of the SLIC system in predicting surgical decision-making, safety and efficacy still cannot be defined because of these limitations. Loss of follow-up could result in under-reporting of failures in the conservative treatment or complications in the surgical group. Once the SLIC was scored by both authors together, inter-rater reliability between observers was not conducted.
Another limitation of our study is the potential influence of the SLIC system on care of the patients in this study. While there was no mention of the SLIC in the medical records, a small number of patients were treated after the 2007 publication of the SLIC. Furthermore, one of the authors (AAP) was a co-author of the 2007 publication. As such, it is possible that this may bias results of the study. Unfortunately, the number of patients treated after 2007 is insufficiently small to allow for a comparison within our study population.
Despite the aforementioned limitations, the SLIC classification looks to be a promising system to aid spinal surgeons in the decision-making process of subaxial cervical trauma. Reliability of the SLIC had already been reported,[10] and our current study suggests that the SLIC system can be promising. Nonetheless, a large study with a prospective application of the SLIC system is still needed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534–51. [PubMed] [Google Scholar]
- 2.Allen BL, Jr, Ferguson RL, Lehmann TR. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976) 1982;7:1–27. doi: 10.1097/00007632-198200710-00001. [DOI] [PubMed] [Google Scholar]
- 3.Harris JH, Edeiken-Monroe B, Kopansiky DR. A practical classification of acute cervical spine injuries. Orthop Clin North Am. 1986;17:15–30. [PubMed] [Google Scholar]
- 4.Vaccaro AR, Hulbert RJ, Patel AA, Fischer C, Dvorak M, Lehman RA, et al. Spine Trauma Study Group. The subaxial cervical spine injury classification system: A novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32:2365–74. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 5.Dvorak MF, Fisher CG, Fehlings MG, Rampersaud R, Oner FC, Aarabi B, et al. The surgical approach to subaxial cervical spine injuries: An evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976) 2007;32:2620–9. doi: 10.1097/BRS.0b013e318158ce16. [DOI] [PubMed] [Google Scholar]
- 6.Patel AA, Dailey A, Brodke DS, Daubs M, Anderson PA, Hurlbert RJ, et al. Spine Trauma Study Group. Subaxial cervical spine trauma classification: The Subaxial Injury Classification system and case examples. Neurosurg Focus. 2008;25:E8. doi: 10.3171/FOC.2008.25.11.E8. [DOI] [PubMed] [Google Scholar]
- 7.Dvorak MF, Fisher CG, Aarabi B, Harris MB, Hurbert RJ, Rampersaud YR, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine (Phila Pa 1976) 2007;32:3007–13. doi: 10.1097/BRS.0b013e31815cd439. [DOI] [PubMed] [Google Scholar]
- 8.Rihn JA, Fisher C, Harrop J, Morrison W, Yang N, Vaccaro AR. Assessment of the posterior ligamentous complex following acute cervical spine trauma. J Bone Joint Surg Am. 2010;92:583–9. doi: 10.2106/JBJS.H.01596. [DOI] [PubMed] [Google Scholar]
- 9.Malham GM, Ackland HM, Varma DK, Williamson OD. Traumatic cervical discoligamentous injuries: Correlation of magnetic resonance imaging and operative findings. Spine (Phila Pa 1976) 2009;34:2754–9. doi: 10.1097/BRS.0b013e3181b6170b. [DOI] [PubMed] [Google Scholar]
- 10.Patel AA, Hurlbert RJ, Bono CM, Bessey JT, Yang N, Vaccaro AR. Classification and surgical decision making in acute subaxial cervical spine trauma. Spine (Phila Pa 1976) 2010;35:S228–34. doi: 10.1097/BRS.0b013e3181f330ae. [DOI] [PubMed] [Google Scholar]


