Abstract
Background and Objective:
Studies have documented that deviations in skeletal components such as the cranial base, the mid-facial complex and the mandible may be associated with morphological factors in patients with class III skeletal malocclusion. Furthermore, deviations in head and neck posture may be associated with the class III skeletal malocclusion. The purpose of this study was to compare cervical vertebrae morphology in patients with class III skeletal malocclusion and adults with normal occlusion.
Materials and Methods:
This case-control study assessed 30 patients with class III skeletal malocclusion (aged 17-30 yrs, with normal vertical growth pattern and ANB<0) were compared with 46 controls (aged 17-30 years, with normal vertical growth pattern, ANB=3+1). Cervical vertebrae anomalies (fusion anomalies and posterior arch deficiency) were assessed via evaluation of their lateral cephalograms. The t- test and Fisher's exact test were used for statistical analysis.
Results:
In the study group, 73.3% had fusion of the body of the cervical vertebrae, while in the control group only 32.6% showed fusion. The fusion in the control group was between C2 and C3 in all cases; whereas, in the study group, fusion was seen between C2-C3, C3-C¬4 or C4-C¬5. Additionally, cervical column deviations occurred significantly more often in the study group compared to the control group (P<0.001).
Conclusion:
Class III skeletal malocclusion may be associated with fusion of cervical vertebrae and deviation of the cervical column.
Keywords: Cervical column morphology, class III skeletal malocclusion, fusion
INTRODUCTION
Studies have demonstrated that deviations in skeletal components such as the cranial base, mid-facial complex and mandible may be seen in patients with class III skeletal malocclusion.[1–3] Additionally, deviations in head and neck posture can also be associated with this type of malocclusion.[4] Studies are indicative of the relationship between orthopedic and orthodontic findings. Several of these studies have evaluated the correlation between head posture and cervical inclination.[4–11] Festa and colleagues evaluated the relationship between mandibular length and cervical lordosis.[5] D’Attilio noticed a significant relationship between the position and length of mandible and cervical.[8] Lippold confirmed the correlation between the position of mandible and cervical vertebrae morphology.[4] Sonnesen et al. evaluated the morphology of cervical column in class III skeletal malocclusion.[12] Such studies have not been performed in the Iranian population. This study sought to evaluate the correlation between class III skeletal malocclusion and cervical vertebrae anomalies such as vertebral fusion altered intervertebral space and spinal deviation in the Iranian population.
MATERIALS AND METHODS
In this case-control study, 76 subjects aged 17-30 yrs referred to several private clinics in Tehran were selected based on the selection criteria and were divided into two groups: study group (30 patients with class III malocclusion) and controls (46 subjects with normal growth pattern and mild class I malocclusion). The inclusion criteria were as follows:
No history of previous orthodontic treatment or orthognathic surgery
No underlying syndrome, respiratory disease, neuromuscular disease or temporomandibular joint disorder
No wound, burns, or scarring in the head and neck
Normal vertical growth pattern (Y axis=61.4±2.9, SN-MP=31.8±5.2, MM=23.6±4.5 and Jarabak Index=62-65%)
ANB<0 for the case group and ANB=3±1 for the control group
All patients in cervical stage 6 (CS6) of cervical vertebral maturation.[13]
The 2 groups were matched in terms of age and sex [Table 1]. Cervical vertebrae morphology was evaluated from lateral cephalograms.[14] In a subject with normal cervical vertebrae, intervertebral spaces were radiolucent [Figure 1].
Table 1.
Frequency distribution of patients with class III skeletal malocclusion (cases) and controls based on age and sex
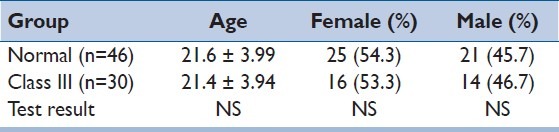
Figure 1.

Normal cervical vertebrae as seen on a cephalogram
The under study anomalies assessed included:
Fusion: When articular surfaces in transverse processes of the vertebrae are skeletally fused to each other [Figure 2]. Block fusion: Severe type of fusion where the intervertebral space is completely lost [Figure 3]. Posterior arch deficiency: Is the absence of cortical layer inside the posterior arch. The cortical surface inside the posterior arch of atlas is seen as a smaller than normal opacity [Figure 4].
Figure 2.

Fusion between C2 and C3
Figure 3.

Block fusion between the body of C2, C3 and C4
Figure 4.

Deficient posterior arch of C1
In order to detect fusion, the distance between the articular surfaces of the vertebrae was measured. If the radiolucency between these surfaces was greater than 1 mm, the vertebra was considered normal with no fusion. If the mentioned radiolucency did not exist, the patient was considered as a case of fusion. If the articular surfaces were seen as separate opaque bony structures, the patient would be considered as a case of discontinuous fusion.[14]
For posterior arch deficiency, absence of internal cortical layer of the posterior arch was our diagnostic criterion. Owing to this absence, the internal cortical surface of the posterior arch of atlas is seen as a smaller than normal opacity.[14]
In order to minimize errors, all lateral cephalograms were controlled again 2 weeks later and then the correlation coefficient was calculated for them.
Statistical analyses
T-test and Fisher's exact tests were used for the comparison of cephalometric indices related to cervical vertebrae anomalies.
RESULTS
No significant differences were detected between the two groups in terms of sex or age [Table 1].
A total of 23.3% of cases and 67.4% of controls had normal cervical vertebrae morphology. This difference between cases and controls was statistically significant (P<0.001, Table 2).
Table 2.
Incidence of deviations in cervical vertebrae morphology of patients with skeletal class III malocclusion and controls
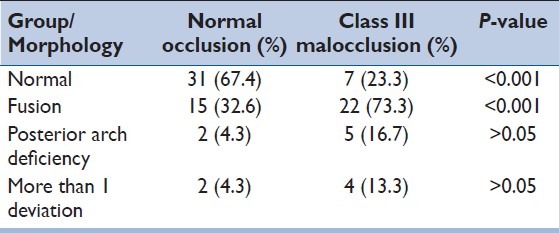
Incidence of fusion was 73.3% in cases and 32.6% in controls which was statistically significant (P<0.001). In the control group, fusion was only observed between C2 and C3. In the majority of the case group, the fusion was between C2 and C3. However, some cases of fusion between C3 and C4 or C4 and C5 were also detected.
Incidence of posterior arch deficiency was 16.7% in the case and 4.3% in the control group. This difference was not statistically significant (P>0.05).
DISCUSSION
The cervical vertebrae assessed were:
C1 (Atlas): The first cervical vertebra has no body or spinous process. Its anterior tubercle is eminent and is close to the posterior wall of nasopharynx. The posterior tubercle is 8-10 mm from the base of skull. C2 (Axis): The second cervical vertebrae of the spine has an odontoid process seen as a cone-shaped process with a rounded apex. C3 to C6: Are similar to each other and clearly visible on radiography.
The present study showed that the incidence of cervical vertebrae anomalies was higher in patients with class III skeletal malocclusion compared to those with normal occlusion. This incidence rate was 73.3% in cases and 32.6% in controls.
Kjaer and Sonnesen in their study conducted in 2007 in Denmark on cervical column morphology in class III malocclusion patients showed higher rates of fusion in class III skeletal malocclusion cases (61.4%) compared to those with normal occlusion (14.3%). In their study, total incidence of cervical column anomalies was higher in skeletal class III malocclusion cases than in those with normal occlusion but incidence of posterior arch deficiency was not significantly different between the 2 groups.[12] Incidence of cervical column anomalies among the Iranian population in both the study group and controls was greater than in the Danish population.
In the Kjaer and Sonnesen study, most cases of fusion were observed to be between C2and C3 (except for 2 cases). In the control group all fusions were also between C2 and C3 (12). These findings were in accord with those of ours.
Sonnesen et al. in their study in 2007 on cervical vertebrae body fusions in patients with skeletal deep bite and controls revealed that incidence of fusion in cervical vertebrae of skeletal deep bite patients was significantly higher than in subjects with normal occlusion. Fusion was mostly reported to be between C2 and C3. Incidence of posterior arch deficiency was also greater in skeletal deep bite patients when compared to normal occlusion in controls.[15]
Kjaer and Sonnesen in their study in 2008, on cervical column morphology in skeletal open bite patients found that incidence of cervical vertebrae deviations was significantly higher in skeletal open bite cases compared to controls.[16]
Kjaer et al. in their study in 2007 entitled “Cervical column morphology related to head posture, cranial base angle and condylar malformation” showed that incidence of cervical anomalies was greater in skeletal malocclusion patients than in normal occlusion subjects.[17]
The basilar part of the occipital bone guides the formation of the cervical vertebrae.[18] Studies show that the notochord through its signaling induces the formation and development of body of the cervical vertebrae and basilar part of the occipital bone. Via some other signals, the notochord affects the paraxial mesoderm and induces the formation of spinal curve and parts of the occipital bone.[19–22]
Results from our study and similar researches highlight the need for further investigations in the fields of genetics and primary stages of fetal development for better understanding of factors influencing the formation of skeletal malocclusions. Such studies may help in better recognition of phenotypic differences in patients with skeletal malocclusions especially class III skeletal malocclusion (which are due to different genotypes) and their relationship to cervical anomalies.
CONCLUSIONS
According to our study results and those of similar researches, a significant correlation exists between cervical vertebrae anomalies and skeletal malocclusions. Therefore, genetic studies relevant to the formation and development of the head and neck during embryonic and fetal periods may help to better understand this correlation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Singh GD. Morphologic determinants in the etiology of Class III malocclusions: A review. Clin Anat. 1999;12:382–405. doi: 10.1002/(SICI)1098-2353(1999)12:5<382::AID-CA9>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 2.Hong SX, Yi CK. A classification and characterization of skeletal Class III malocclusion on etio-pathogenic basis. IntJ Oral Maxillofac Surg. 2001;30:264–71. doi: 10.1054/ijom.2001.0088. [DOI] [PubMed] [Google Scholar]
- 3.Bui C, King T, Proffit W, Frazier-Bowers S. Phenotypic characterization of Class III patients. A necessary background for genetic analysis. Angle Orthod. 2006;76:564–9. doi: 10.1043/0003-3219(2006)076[0564:PCOCIP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Lippold C, Danesh G, Hoppe G, Drerup B, Hackenberg L. Sagittal spinal posture in relation to craniofacial morphology. Angle Orthod. 2006;76:625–31. doi: 10.1043/0003-3219(2006)076[0625:SSPIRT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Festa F, Tecco S, Dolci M, Ciufolo F, Di Meo S, Filippi MR, et al. Relationship between cervical lordosis and facial morphology in Caucasian women with skeletal class II malocclusion: A cross sectional study. Cranio. 2003;21:121–9. doi: 10.1080/08869634.2003.11746240. [DOI] [PubMed] [Google Scholar]
- 6.Gresham H, Smithells PA. Cervical and mandibular posture. Dent Rec. 1954;74:261–4. [Google Scholar]
- 7.Korbmacher H, Eggers-Stroeder G, Koch L, Kahl-Nieke B. Correlations between anomalies of the dentition and pathologies of the locomotor system—a literature review. J Orofac Orthop. 2004;65:190–203. doi: 10.1007/s00056-004-0305-3. [DOI] [PubMed] [Google Scholar]
- 8.D’Attilio M, Epifania E, Ciuffolo F, Salini V, Filippi MR, Dolci M, et al. Cervical lordosis angle measured on lateral.cephalograms; findings in skeletal class II female subjects with and without TMD: A cross sectional study. Cranio. 2004;22:27–44. doi: 10.1179/crn.2004.005. [DOI] [PubMed] [Google Scholar]
- 9.Lippold C, van den Bos L, Hohoff A, Danesh G, Ehmer U. Interdisciplinary study of orthopedic and orthodontic findingsin pre-school infants. J Orofac Orthop. 2003;64:330–40. doi: 10.1007/s00056-003-0236-4. [DOI] [PubMed] [Google Scholar]
- 10.Michelotti A, Manzo P, Farella M, Martina R. Occlusion andposture: Is there evidence of correlation? Minerva Stomatol. 1999;48:525–34. [PubMed] [Google Scholar]
- 11.Huggare JA, Cooke MS. Head posture and cervicovertebral anatomy as mandibular growth predictors. Eur J Orthod. 1994;16:175–80. doi: 10.1093/ejo/16.3.175. [DOI] [PubMed] [Google Scholar]
- 12.Sonnesen L, Kjaer I. Cervical Column morphology in patients with skeletal Class III malocclusion and mandibular overjet. Am J Orthod Dentofacial Orthop. 2007;132:427–el2. doi: 10.1016/j.ajodo.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebralmaturation (CVM)methodfor the assessment of optimal treatmenttiming in dentofacial orthopedics. Semin Orthod. 2005;11:119–29. [Google Scholar]
- 14.Sandham A. Cervical Vertebral anomalies in cleft lip and palate. Cleft Palate J. 1986;23:206–14. [PubMed] [Google Scholar]
- 15.Sonnesen L, Kjaer I. Cervicalvertebral body fusionsin patients with skeletaldeepbite. Eur J Orthod. 2007;29:404–7. [Google Scholar]
- 16.Sonnesen L, Kjaer I. Cervical Column morphology in patients with skeletal openbite. Orthod Craniofac Res. 2008;11:17–23. doi: 10.1111/j.1601-6343.2008.00409.x. [DOI] [PubMed] [Google Scholar]
- 17.Sonnesen L, Pedersen CE, Kjaer I. Cervical Column Morphology related to head posture, Cranial base angle and condylar malformation. Eur J Orthod. 2007;24:398–403. doi: 10.1093/ejo/cjm010. [DOI] [PubMed] [Google Scholar]
- 18.Sonnesen L, Nolting D, Kjaer KW, Kjaer I. Association between the development of the Body Axis and the Craniofacial Skeleton Studied by Immunohistochemical Analyses Using Collagen II, Pax9, Paxl, and Noggin Antibodies. Spine. 2008;33:1622–6. doi: 10.1097/BRS.0b013e31817b61d1. [DOI] [PubMed] [Google Scholar]
- 19.Kjaer I. Neuro - osteology. Crit Rev Oral Biol. 1998;9:224–44. doi: 10.1177/10454411980090020501. [DOI] [PubMed] [Google Scholar]
- 20.Kjaer I. Human prenatal craniofacial development related to brain development under normal and pathologic conditions. Actaodont Scand. 1995;3:135–43. doi: 10.3109/00016359509005963. [DOI] [PubMed] [Google Scholar]
- 21.Sadler TW. Embryology of neural tube development. Am J Genet C Semin Med Genet. 2005;135:2–8. doi: 10.1002/ajmg.c.30049. [DOI] [PubMed] [Google Scholar]
- 22.Giampietro PF, Dunwoodie SL, Kusumi K, Pourquie O, Tassy O, Offiah AC, et al. Progress in the understanding of the genetic etiology of vertebral segmentation disorders in humans. Ann N Y Acad Sci. 2009;1151:38–67. doi: 10.1111/j.1749-6632.2008.03452.x. [DOI] [PubMed] [Google Scholar]


