Abstract
Successful long-term preservation of Mycobacterium tuberculosis cells is important for sample transport, research, biobanking, and the development of new drugs, vaccines, biomarkers, and diagnostics. In this report, Mycobacterium bovis bacillus Calmette-Guérin and M. tuberculosis H37Ra were used as models of M. tuberculosis complex strains to study cryopreservation of M. tuberculosis complex cells in diverse sample matrices at different cooling rates. Cells were cryopreserved in diverse sample matrices, namely, phosphate-buffered saline (PBS), Middlebrook 7H9 medium with or without added glycerol, and human sputum. The efficacy of cryopreservation was quantified by microbiological culture and microscopy with BacLight LIVE/DEAD staining. In all sample matrices examined, the microbiological culture results showed that the cooling rate was the most critical factor influencing cell viability. Slow cooling (a few degrees Celsius per minute) resulted in much higher M. tuberculosis complex recovery rates than rapid cooling (direct immersion in liquid nitrogen) (P < 0.05). Among the three defined cryopreservation media (PBS, 7H9, and 7H9 plus glycerol), there was no significant differential effect on viability (P = 0.06 to 0.87). Preincubation of thawed M. tuberculosis complex cells in 7H9 broth for 20 h before culture on solid Middlebrook 7H10 plates did not help the recovery of the cells from cryoinjury (P = 0.14 to 0.71). The BacLight LIVE/DEAD staining kit, based on Syto 9 and propidium iodide (PI), was also applied to assess cell envelope integrity after cryopreservation. Using the kit, similar percentages of “live” cells with intact envelopes were observed for samples cryopreserved under different conditions, which was inconsistent with the microbiological culture results. This implies that suboptimal cryopreservation might not cause severe damage to the cell wall and/or membrane but instead cause intracellular injury, which leads to the loss of cell viability.
INTRODUCTION
Tuberculosis (TB) is the second leading cause of death from an infectious disease worldwide (after HIV/AIDS). Millions of people die from the disease every year (1.2 to 1.5 million deaths in 2010). A patient with active TB can infect 10 to 15 persons in a year without restriction or treatment. TB prevention and control, including diagnosis, treatment, and drug development, is one of the major tasks of the World Health Organization (WHO) and many governments, especially in developing countries (24).
Timely and correct diagnosis of TB is still a challenge. Often, collected samples must be shipped to centers with clinical laboratory facilities, well-trained personnel, and specialized working environments for biosafety. In this context, cryopreservation can be a useful option. Biobanking of Mycobacterium tuberculosis is also important in fundamental biological research and for the development of new drugs, vaccines, biomarkers, and diagnostic tests. Clinical and laboratory samples are often exchanged among institutions for comparative multicenter studies. Therefore, quality control of transported samples is a very important issue.
There have been few studies on the optimization of M. tuberculosis cryopreservation. Clinical M. tuberculosis samples, such as sputum, are stored at room temperature, but only for a few days (4, 10, 20). The viability of some bacteria, such as M. tuberculosis and Mycobacterium bovis, can be severely affected during shipping by storage conditions (14). Papers published a few decades ago demonstrated long-term preservation of M. tuberculosis samples at −70°C, but little information on optimization of the cryoprotective medium and freezing procedure was provided (9, 11–14). Therefore, optimization of M. tuberculosis cryopreservation remains an unfilled need, especially for situations requiring quantification of viable M. tuberculosis cells in samples with low cell density.
Since M. bovis bacillus Calmette-Guérin (BCG), a nonvirulent strain of the M. tuberculosis complex, is very close to M. tuberculosis in terms of cell physiology, it was used as the model to optimize the cryopreservation protocol in the first part of this study. Common cryopreservation media, the effect of a cryoprotective agent (glycerol), and the cooling rate were studied. It has been suggested that transient incubation of cells in broth medium after exposure to stress environments, such as heating, freezing/thawing, or UV light, helps to repair the injury for some cell types (1, 8, 15, 23). Therefore, the effect of transient incubation (preincubation) on cryopreserved BCG cells was also explored. To conclude the study, the optimized protocol was applied to M. tuberculosis H37Ra cells with which a natural, undefined sample matrix, namely, human sputum, was spiked.
MATERIALS AND METHODS
BCG cell preparation and concentration assessment.
BCG cells were cultivated to late log/early stationary phase in 15-ml conical tubes containing 5 ml Difco Middlebrook 7H9 broth with 10% albumin-dextrose-catalase (ADC) enrichment and 0.05% Tween 80 (BD Diagnostics, Sparks, MD) (henceforth referred to as 7H9) at 37°C without agitation for 3 to 4 weeks. Cells were harvested by centrifugation for 5 min at 5,000 rpm and then resuspended in an equal volume of fresh 7H9. The cell concentration was assessed by optical density measurement at 580 nm with a spectrophotometer (Spectramax Plus; Molecular Devices, Sunnyvale, CA). According to previously published growth measurements, an A580 of 0.1 unit is equivalent to 6.3 × 107 CFU Mycobacterium cells per ml (3).
BCG cryopreservation.
BCG cells were cryopreserved in three different media: phosphate-buffered saline (PBS), 7H9, and 7H9 plus glycerol (EMD Chemicals, Inc., Gibbstown, NJ). For PBS and 7H9, BCG cells were diluted in PBS or 7H9, respectively, to an estimated cell density of 1e8 CFU/ml (based on optical density). For 7H9 plus glycerol, BCG cells were first diluted with 7H9 to 5e8 CFU/ml, and then, 7H9 plus glycerol (precooled to 4°C) was slowly added dropwise to a final volume ratio of 4:1. The final glycerol concentration in the freezing sample was 4% (vol/vol). The cell suspension was agitated gently for osmotic equilibration during medium addition. After medium addition, the cell suspension was stored at room temperature for 15 min for equilibration before cryopreservation. For all three groups, the final cell concentration was 1e8 CFU/ml. This high cell density is typical of many cryopreserved samples, and it enabled LIVE/DEAD staining and microscopic analysis. Cryogenic freezing vials (2 ml; Fisher Scientific, Pittsburgh, PA) were used for cryopreservation, each containing 0.5 ml of the cell suspension.
For comparison between different cooling rates, two freezing methods were implemented. One was slow cooling in a “Box-in-Box” (BIB) system that was developed in our group, and the other was rapid cooling by direct immersion of samples in liquid nitrogen (LN2). In the BIB system (Fig. 1), a thermal insulation material made of polyethylene fills an aluminum enclosure. The thickness of the polyethylene layer was designed for a low cooling rate and then demonstrated empirically (21). For cryopreservation in BIB, vials were placed in the slots cut into the polyethylene foam. The system was then closed and placed into a −80°C freezer overnight. Dummy samples with only cryoprotective medium were treated the same way. T-type thermocouples (SA-1T; Omega, Stamford, CT) were inserted inside the dummy samples to record the temperature history during cooling. After equilibrium in the −80°C freezer overnight, the samples were transferred into LN2. The protocol for fast cooling was to immerse the sample vials in LN2 directly and record the temperature history via dummy samples.
Fig 1.
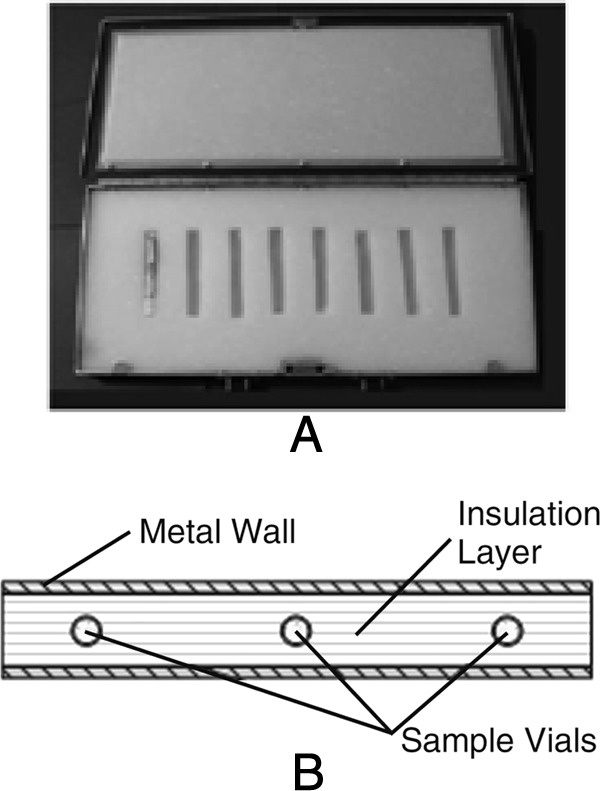
BIB system for slow cooling. (A) An opened BIB, in which sample vials are placed in one slot. (B) Cross-section of the BIB system.
Thawing of cryopreserved BCG cells.
For sample thawing, the frozen samples were removed from LN2 and quickly immersed in a 37°C water bath. They were agitated gently until no crystals remained. Then, the cells were assessed for viability by microbiological culture and LIVE/DEAD staining as described below.
Microbiological culturing, with and without preincubation.
The thawed cells were diluted with 7H9 broth to a concentration of 4,000 CFU/ml. Before culturing, the cells were divided into two groups. One group was plated on 7H10 agar directly (without preincubation), and the other was preincubated in 7H9 at 37°C with 5% CO2 and 100% humidity for 20 h before plating in order to study the preincubation effect. For plate culturing, Difco Middlebrook 7H10 agar with 10% (vol/vol) oleic acid-albumin-dextrose-catalase (OADC) enrichment (BD Diagnostics, Sparks, MD) (7H10) was used. A cell suspension of 250 μl with a predicted concentration of 4,000 CFU/ml was spread on each plate. The plates were sealed in plastic bags (BD GasPak EZ; BD Diagnostics, Sparks, MD) and incubated at 37°C with 5% CO2 and 100% humidity. After incubation for about 24 h, the petri dishes were inverted in order to prevent desiccation of the agar during extended culture.
These experiments were repeated three times with three separate batches of BCG cells. CFU were counted at several time points postinoculation.
LIVE/DEAD staining assessment.
A BacLight LIVE/DEAD staining kit (Invitrogen, Grand Island, NY) was used to assess the envelope integrity of cryopreserved cells. The staining was performed as specified by the user manual; briefly, 1.5 μl LIVE/DEAD staining reagent was added to 0.5 ml cell suspension, which was vortexed, incubated at room temperature for 15 min, and then observed under fluorescence microscopy (Nikon Instruments Inc., Melville, NY).
Cryopreservation of M. tuberculosis H37Ra cells in sputum.
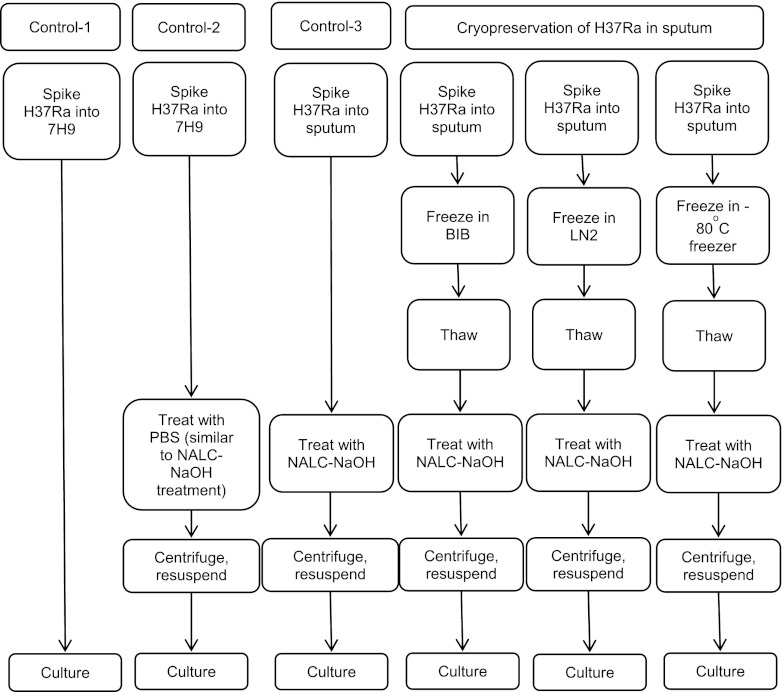
The experimental design of H37Ra cryopreservation in sputum is illustrated in Fig. 2. Sputum samples were spiked with H37Ra cells that had been collected for diagnostic purposes from anonymous human donors with no tuberculosis exposure (Bioreclamation Inc., Hicksville, NY). The estimated final cell concentrations were 1e7 CFU/ml. Then, the samples in cryogenic freezing vials (0.5 ml in each vial) were frozen by three different methods: BIB in a −80°C freezer, in LN2 directly, or in a −80°C freezer directly. After fast thawing in a 37°C water bath, the samples were treated with N-acetyl-l-cysteine and sodium hydroxide (NALC-NaOH), following the standard digestion-decontamination procedures for TB specimen processing (6). The samples were centrifuged at 3,000 × g for 20 min, and the pellets were resuspended in 7H9 for microbiological culturing as described above. The experiments were repeated twice.
Fig 2.
Experiment design of H37Ra cryopreservation in sputum.
In order to differentiate the effects of NALC-NaOH treatment and cryopreservation, three control experiments were conducted, as shown in Fig. 2. In control 1, 7H9 was spiked with H37Ra cells, and then the cells were cultured (without cryopreservation, NALC-NaOH treatment, or centrifugation). In control 2, 7H9 was spiked with H37Ra cells, and the samples were treated with PBS buffer following the procedure of NALC-NaOH treatment (with PBS in place of NALC-NaOH), centrifuged, and then cultured (without cryopreservation and chemical influence of NALC-NaOH). The difference between control 1 and control 2 is the effect of centrifugation on cell loss. In control 3, sputum was spiked with H37Ra cells, and the samples were treated with NALC-NaOH, centrifuged, and then cultured without cryopreservation. A comparison of control 2 and control 3 indicates the effect of NALC-NaOH treatment.
Statistical analysis.
The results are presented as averages ± standard deviations. The statistical analysis was performed with a two-way analysis of variance (ANOVA) test for the comparison of different conditions. The level of significance was set at a P value of <0.05.
RESULTS
Temperature record and cooling rate during freezing.
Typical temperature profiles in the cooling process were recorded for dummy samples in the BIB system, in LN2, and in a −80°C freezer directly, and the cooling rates were computed. In the BIB system, a low cooling rate of −1 to −3.5°C/min was observed. When samples were immersed in LN2 directly, the cooling rate ranged between −100 and −400°C/min. For samples in a −80°C freezer directly, the cooling rate ranged between −10 and −20°C/min. For freezing directly in the freezer, the cooling rate was variable and depended on the location of the samples and the heat transfer situation inside the freezer.
Viability of BCG cells after freezing and thawing.
CFU were counted at various time points after plating. After incubation for 2 weeks, colonies started emerging, while after 4 weeks, the CFU numbers reached stability. There was little or no additional colony formation between 4 and 8 weeks of culture.
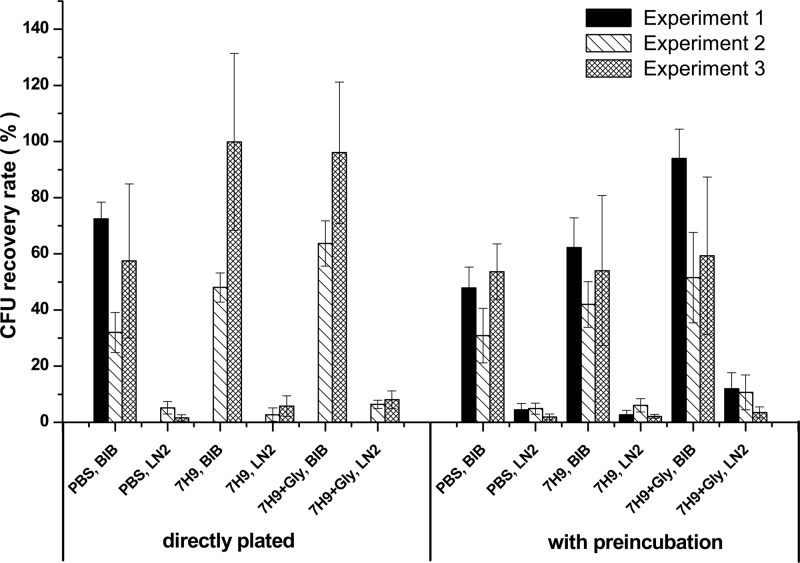
The CFU recovery rates compared to those of control samples are shown in Fig. 3. (In the first experiment cells were cultured for 3 weeks and in the second and third experiments for 4 weeks.) The results indicate that the cooling rate is one of the most critical factors for BCG cells to survive freezing and thawing. A low cooling rate enabled about 1 order of magnitude greater CFU recovery than a high cooling rate (P < 0.05) in all freezing media tested. There was no significant difference between any of the three freezing media (P = 0.06 to 0.87).
Fig 3.
Microbiological culture results for cryopreserved and thawed BCG cells. The error bars indicate standard deviations.
CFU counts of cryopreserved BCG with and without preincubation before plating are also shown in Fig. 3. For cryopreserved BCG cells, preincubation did not significantly enhance the cells' recovery (P = 0.14 to 0.71).
In conclusion, among the experimental conditions examined, only the cooling rate exhibited a significant and consistent effect on BCG cryopreservation.
LIVE/DEAD staining of BCG cells.
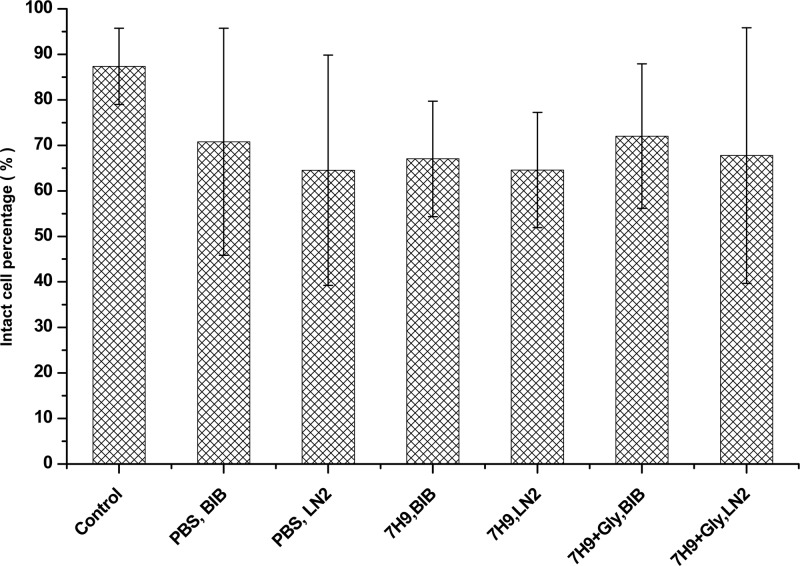
The BacLight LIVE/DEAD staining kit, which differentially stains bacteria with intact versus compromised cell envelopes, was used to assess the cell envelope integrity of cryopreserved cells. For all treatment groups, the percentage of intact cells after cryopreservation and thawing was evaluated with the BacLight LIVE/DEAD staining kit (Fig. 4). Among different freezing media and cooling rates, there was no significant difference in the percentage of intact (“live”) cells (P = 0.14 to 0.99). Compared to controls (fresh cells without cryopreservation), percentages of intact cells appeared high under all conditions despite the sharply reduced viability (assessed by culture) of cells that were rapidly frozen in LN2.
Fig 4.
Intact BCG cell percentages after cryopreservation assessed by LIVE/DEAD staining (means ± standard deviations; n = 14). Control, fresh cells.
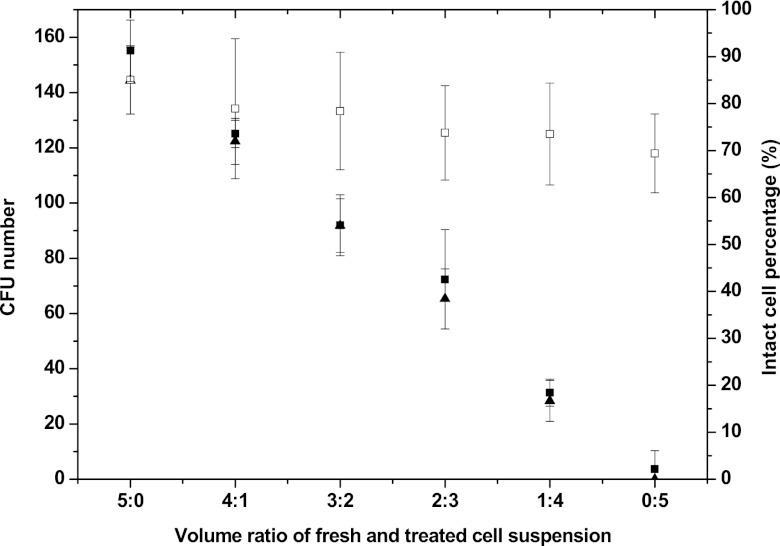
The LIVE/DEAD staining kit indirectly assesses viability in terms of cell envelope integrity. To validate the kit's performance on BCG cells, it was also applied to mixtures of fresh and heat-treated BCG cells and compared with the results of microbiological culturing. BCG cells were heated at 80°C for 35 min (inactivated cells), and then the treated cell suspension was mixed with fresh (viable) cells. The two cell suspensions had the same cell concentrations (estimated by optical density) and were mixed with various volume ratios (0:5, 1:4, 2:3, 3:2, 4:1, and 5:0). The mixtures were divided into two groups. One was assessed by BacLight LIVE/DEAD staining, and the other one was cultured on 7H10 agar. For microbiological culturing, each plate received 250 μl of cell suspension with a predicted starting concentration of 4,000 CFU/ml (i.e., 1,000 cells/plate, including both fresh and heat treated). The CFU numbers were counted after culture for 28 days. As shown in Fig. 5, LIVE/DEAD staining yielded results that were closely correlated with microbiological culturing results for heat-treated BCG cells. In contrast, a similar experiment of LIVE/DEAD staining for the mixtures of fresh and cryokilled BCG cells (fast cooled in LN2) was also conducted. However, the results did not show a significant difference among the mixtures of fresh and cryokilled cells with different volume ratios (0:5, 1:4, 2:3, 3:2, 4:1, and 5:0) (Fig. 5).
Fig 5.
Correlation between LIVE/DEAD staining and microbiological culturing results when applied to heat-treated (80°C for 35 min) and cryokilled (fast cooled in liquid nitrogen) BCG cells. ▲, CFU numbers for mixtures of fresh and heat-killed BCG cells; ■, intact-cell percentages for mixtures of fresh and heat-treated BCG cells; □, intact-cell percentages for mixtures of fresh and cryotreated BCG cells. The error bars indicate standard deviations.
Viability of M. tuberculosis H37Ra cells after cryopreservation in sputum.
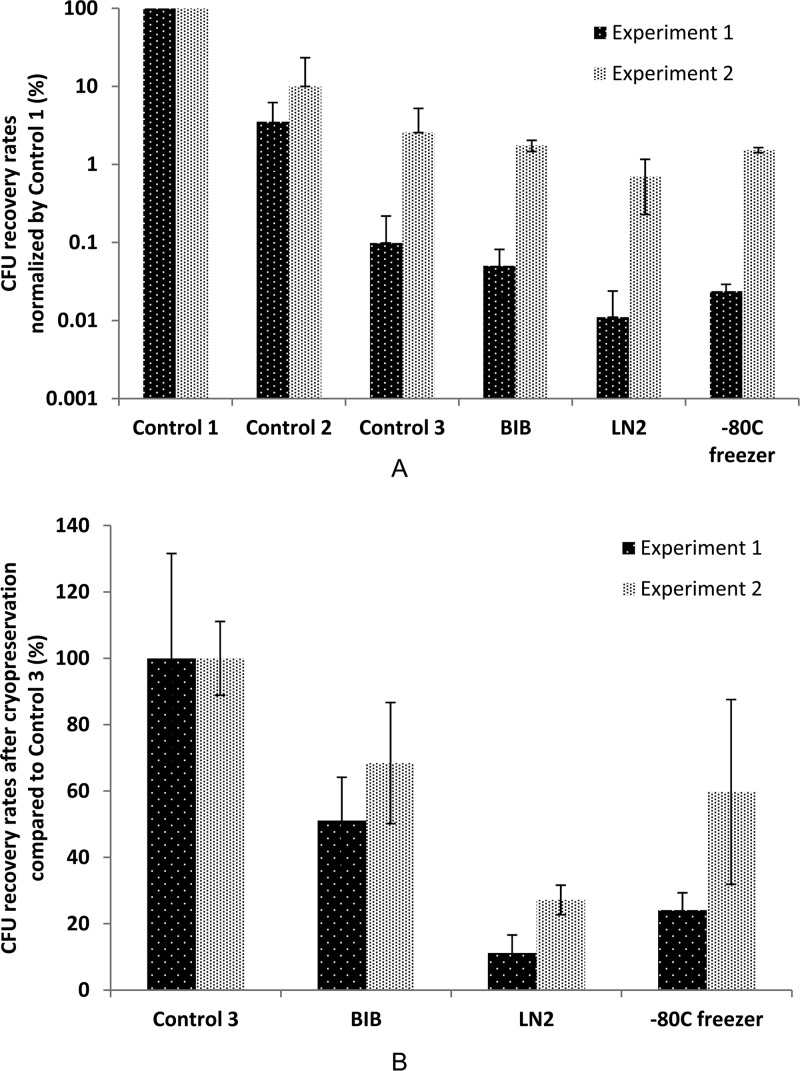
The CFU-counting results for cryopreserved H37Ra cells in sputum are presented in Fig. 6. The results show that treatment with NALC-NaOH, centrifugation, and freeze-thaw processing can result in viable-cell loss. Comparison of controls 1, 2, and 3 indicates that treatment with NALC-NaOH and centrifugation can each cause viable-cell loss by a factor of about 10-fold. As with the results of BCG cryopreservation in defined matrices, the cooling rate was a critical factor for M. tuberculosis cryopreservation in sputum. Fast cooling in LN2 reduced the viability of M. tuberculosis cells to a greater extent than slow cooling in BIB (P < 0.05).
Fig 6.
CFU results for cryopreserved and treated H37Ra cells. (A) CFU recovery rates (%) after cryopreservation, NALC-NaOH treatment, and centrifugation normalized by control 1. (B) Influence of the cooling rate on CFU recovery rates (%) after cryopreservation normalized by control 3. n = 6. The error bars indicate standard deviations.
Direct freezing of M. tuberculosis samples in a −80°C freezer has been used in clinics and research due to its low cost and convenience. The M. tuberculosis cell recovery rate after cryopreservation was compared between direct freezing in BIB and direct LN2 immersion, and greater survival was observed when BIB was used (P < 0.05). However, the difference between freezing in BIB and directly in the −80°C freezer was significant in the 1st experiment (P < 0.05), but not in the 2nd experiment (P = 0.73). This might be due to the fact that the freezing rates of samples in a −80°C freezer vary significantly with location inside the freezer, freezer operation, and heat transfer conditions. The BIB system can provide a more reproducible slow-cooling environment for cryopreservation.
DISCUSSION
Currently, there is no explicitly standardized protocol for the cryopreservation of clinical TB samples. Samples are often placed directly into a −80°C freezer. However, this practice leads to variable cooling rates dependent on many factors, including the sample container, volume of samples, and heat transfer conditions inside the freezer. Also, the cooling rate in the freezer is not optimally low for M. tuberculosis cryopreservation, as shown in the results. In this work, we employed a simple passive cooling device, “Box-in-Box,” which enables a consistent and reproducible low cooling rate. The BIB method is inexpensive, easy to perform, and reliable and delivers a reproducible cooling rate. The BIB device has been successfully used for cryopreservation of stem cells (21, 25, 26). The results in this study showed that it delivers the highest recovery of M. tuberculosis after cryopreservation.
In cryopreservation, according to the “two-factors” hypothesis, cryoinjury to cells during freezing consists of “ice injury” and “solution injury” (16, 17). Many parameters might influence the cell recovery rate after freezing and thawing, e.g., the cooling rate, the presence of a cryoprotective agent (CPA), CPA addition and removal, and the thawing process. The optimum procedure also depends on cell properties, such as the cell membrane permeability to water and CPA, the ratio of cell membrane area to cell volume (A/V), and the osmotically inactive intracellular volume fraction (Vb). The results of this work showed that slow cooling is much better than fast cooling for cryopreservation of M. tuberculosis cells. This may be explained by the properties of the cells. The Mycobacterium cell envelope has low permeability to most compounds, including water (“permeability barrier”), because its outer leaflet is composed of giant saturated fatty acids with extremely low fluidity (18, 19). During freezing, extracellular water is frozen first, which causes the osmolality of the extracellular solution to increase. Due to the imbalance of the water chemical potential between the intra- and extracellular environments, intracellular water is transported across the cell membrane and wall to the outside. This increases the osmolality of the intracellular solution, decreasing its freezing point and hindering intracellular ice formation (IIF). For M. tuberculosis cells, water may permeate across the cell envelope more slowly than the envelopes of other cell types. More time would be required to reach equilibrium between the inside and outside of the cells during freezing. Slow cooling might mitigate the intracellular ice injury in M. tuberculosis cryopreservation. Further research on M. tuberculosis cell membrane and wall properties, including quantitative cell membrane permeability to water, would be helpful for cooling protocol optimization and interpretation.
The cryopreservation medium and specific CPAs are additional important factors that may influence cell recovery. Generally, CPAs, such as glycerol, are added before freezing to reduce intracellular ice formation. The standard formulation of 7H9 broth contains glycerol, but at a very low concentration (0.2% [vol/vol]). Due to its widespread use in cryopreservation, glycerol was evaluated as the CPA in this study. However, the results revealed no significant benefits of glycerol (P = 0.11 to 0.87). In the future, additional CPAs (such as dimethyl sulfoxide) should to be tested.
Compared to PBS, 7H9 broth is a complex medium with differences in composition, pH, and osmolality. It contains many kinds of electrolytes, a low concentration of glycerol, and nutrients, with a pH of 6.8 and osmolality of about 168 mosmol/kg H2O. In contrast, PBS has a pH of 7.2 to 7.4, and its osmolality is about 290 mosmol/kg H2O. The osmolality was measured with a vapor pressure osmometer (Wescor Inc., Logan, UT). Despite these differences, we did not observe a significant difference between BCG cells cryopreserved in 7H9 and those cryopreserved in PBS (P = 0.11 to 0.84). Compared to the cooling rate, the cryopreservation medium and CPA had limited impacts. The results indicated that for convenience and simplicity, M. tuberculosis cells could be cryopreserved well in 7H9, PBS, or possibly other media, as long as the cooling rate is low (generally, recovery rates were >50%). This eliminates the steps of CPA addition and removal before and after cryopreservation, which add complexity and increase the risk of sample contamination.
When cells are exposed to stressful environments, e.g., cooling, heating, radiation, or desiccation, cellular functions may be impaired. It has been observed that for some cells, preincubation in broth or liquid medium for some time after exposure to the stress may help repair the injuries (1, 8, 15, 23); however, others doubt its effectiveness (7). In the present work, preincubation did not improve the recovery of cryopreserved BCG cells from cryoinjury.
The mechanism of cryoinjury during rapid cooling did not appear to involve severe damage to the cell envelope. By LIVE/DEAD staining, rapidly cooled cell suspensions with low viability did not significantly differ from slowly cooled suspensions with high viability. The BacLight LIVE/DEAD staining kit contains Syto 9 and PI. PI can penetrate only cells with compromised cell envelope integrity, while Syto 9 can penetrate both intact cells and cells with compromised cell envelopes. Thus, intact cells emit green fluorescence while compromised cells emit red fluorescence under fluorescence microscopy, i.e., the LIVE/DEAD staining kit indirectly assesses viability in terms of cell envelope integrity. After suboptimal (rapid) freezing and thawing, many BCG cells might retain intact walls and membranes while sustaining enough intracellular injury to compromise their ability to grow. This contrasts with BCG cells heated at 80°C for 35 min. For these heat-killed cells, LIVE/DEAD staining and microbiological culture results correlated with each other, consistent with cellular inactivation mechanisms that include cell envelope damage. The commercially available BacLight LIVE/DEAD staining kit was designed primarily for use on bacteria but lacks enough information on efficacy when applied to M. tuberculosis cells. It was previously reported that the staining pattern of the kit depends on the bacterium type and even the method of treatment of the bacteria (such as heating or UV exposure), especially for cells in intermediate states between viable and inactivated states (2, 5, 22). Additional evaluation of the kit should be conducted for M. tuberculosis viability assessment.
Conclusions.
Among the variables tested, the cooling rate was the most critical factor for the cryopreservation of M. tuberculosis complex cells. M. tuberculosis complex cells were well cryopreserved in PBS buffer, Middlebrook 7H9 with and without added glycerol, or sputum if a low cooling rate was applied. Preincubation of frozen/thawed BCG cells in 7H9 broth before culturing on solid 7H10 agar did not help the cells repair cryoinjury. Cell inactivation by fast cooling was not associated with a compromised cell envelope, as indicated by the results of microbiological culture and LIVE/DEAD staining.
ACKNOWLEDGMENT
We acknowledge a grant from the Catalysis Foundation for Health and NIH grant no. R01AI093418.
Footnotes
Published ahead of print 29 August 2012
REFERENCES
- 1.Ahmad M, Srivastava BS, Agarwala SC. 1978. Effect of incubation media on the recovery of Escherichia coli K12 heated at 52 degrees C. J. Gen. Microbiol. 107:37–44 [DOI] [PubMed] [Google Scholar]
- 2.Berney M, Hammes F, Bosshard F, Weilenmann HU, Egli T. 2007. Assessment and interpretation of bacterial viability by using the LIVE/DEAD BacLight Kit in combination with flow cytometry. Appl. Environ. Microbiol. 73:3283–3290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bloom BR. 1994. Tuberculosis: pathogenesis, protection, and control. ASM Press, Washington, DC [Google Scholar]
- 4.Bobadilla-del-Valle M, et al. 2003. Comparison of sodium carbonate, cetyl-pyridinium chloride, and sodium borate for preservation of sputa for culture of Mycobacterium tuberculosis. J. Clin. Microbiol. 41:4487–4488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davey HM. 2011. Life, death, and in-between: Meanings and methods in microbiology. Appl. Environ. Microbiol. 77:5571–5576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delta-Latta P. 2007. Mycobacteriology and antimycobacterial susceptibility testing, p 7.1.2.1–7.1.2.9 In Garcia L, Isenberg H. (ed), Clinical microbiology procedures handbook, 2nd ed,. ASM Press, Washington, DC [Google Scholar]
- 7.Duthie SJ, Pirie L, Jenkinson AM, Narayanan S. 2002. Cryopreserved versus freshly isolated lymphocytes in human biomonitoring: endogenous and induced DNA damage, antioxidant status and repair capability. Mutagenesis 17:211–214 [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara S, et al. 1986. Cryopreservation of human-lymphocytes for assessment of lymphocyte subsets and natural-killer cytotoxicity. J. Immunol. Methods 90:265–273 [DOI] [PubMed] [Google Scholar]
- 9.Grover AA, Kim HK, Wiegesha EH, Smith DW. 1967. Host-parasite relationships in experimental airborne tuberculosis. 2. Reproducible infection by means of an inoculum preserved at −70°C. J. Bacteriol. 94:832–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang TS, Chen YS, Lee SSJ, Tu HZ, Liu YC. 2005. Preservation of clinical isolates of Mycobacterium tuberculosis complex directly from MGIT culture tubes. Ann. Clin. Lab. Sci. 35:455–458 [PubMed] [Google Scholar]
- 11.Kim TH, Kubica GP. 1972. Long-term preservation and storage of Mycobacteria. Appl. Microbiol. 24:311–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim TH, Kubica GP. 1973. Preservation of Mycobacteria— 100 percent viability of suspensions stored at −70 C. Appl. Microbiol. 25:956–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubica GP, Gontijofilho PP, Kim T. 1977. Preservation of Mycobacteria at 70-degrees-C: persistence of key differential features. J. Clin. Microbiol. 6:149–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kubica GP, Kim TH. 1979. Preservation of Mycobacteria at −70-degrees-C—survival of unfrozen suspensions in transit. Tubercle 60:37–43 [DOI] [PubMed] [Google Scholar]
- 15.Lavoie ET, Grasman KA. 2005. Isolation, cryopreservation, and mitogenesis of peripheral blood lymphocytes from chickens (Gallus domesticus) and wild herring gulls (Larus argentatus). Arch. Environ. Contam. Toxicol. 48:552–558 [DOI] [PubMed] [Google Scholar]
- 16.Mazur P. 1977. Role of intracellular freezing in death of cells cooled at supraoptimal rates. Cryobiology 14:251–272 [DOI] [PubMed] [Google Scholar]
- 17.Mazur P. 1984. Freezing of living cells—mechanisms and implications. Am. J. Physiol. 247:C125–C142 [DOI] [PubMed] [Google Scholar]
- 18.Nikaido H. 1994. Prevention of drug access to bacterial targets—permeability barriers and active efflux. Science 264:382–388 [DOI] [PubMed] [Google Scholar]
- 19.Nikaido H. 2001. Preventing drug access to targets: cell surface permeability barriers and active efflux in bacteria. Semin. Cell Dev. Biol. 12:215–223 [DOI] [PubMed] [Google Scholar]
- 20.Selvakumar N, Sudhamathi S, Duraipandian M, Frieden TR, Narayanan PR. 2004. Reduced detection by Ziehl-Neelsen method of acid-fast bacilli in sputum samples preserved in cetylpyridinium chloride solution. Int. J. Tuberc. Lung Dis. 8:248–252 [PubMed] [Google Scholar]
- 21.Shu ZQ, et al. 2010. Development of a reliable low-cost controlled cooling rate instrument for the cryopreservation of hematopoietic stem cells. Cytotherapy 12:161–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stocks SM. 2004. Mechanism and use of the commercially available viability stain, BacLight. Cytometry 61:189–195 [DOI] [PubMed] [Google Scholar]
- 23.Wang SY, Hsu ML, Tzeng CH, Hsu HC, Ho CK. 1998. The influence of cryopreservation on cytokine production by human T lymphocytes. Cryobiology 37:22–29 [DOI] [PubMed] [Google Scholar]
- 24.WHO 2011. Global tuberculosis control 2011. http://www.who.int/tb/publications/global_report/2011/gtbr11_full.pdf [Google Scholar]
- 25.Zhou XM, et al. 2009. Cryopreservation of peripheral blood stem cells using a box-in-box cooling device. Biopreserv. Biobanking 7:107–114 [DOI] [PubMed] [Google Scholar]
- 26.Zhou XM, et al. 2011. Heat transfer analysis for the design and application of the passive cooling rate controlled device-box-in-box. Int. J. Heat Mass Transfer 54:2136–2143 [Google Scholar]