Abstract
The role of pyrazinamide in the current treatment of multidrug-resistant (MDR) tuberculosis (TB) is uncertain. From a territory-wide registry of MDR-TB cases diagnosed between 1995 and 2009, we assembled a cohort of 194 patients with MDR pulmonary TB given fluoroquinolone-containing regimens. Stratified by pyrazinamide use and susceptibility, there were 83 users with pyrazinamide-susceptible MDR-TB (subgroup A), 24 users with pyrazinamide-resistant MDR-TB (subgroup B), 40 nonusers with pyrazinamide-susceptible MDR-TB (subgroup C), and 47 nonusers with pyrazinamide-resistant MDR-TB (subgroup D). We estimated the adjusted risk ratio (ARR) of early sputum culture conversion (ARR-culture) that occurred within 90 days posttreatment and that of cure or treatment completion (ARR-success) that occurred by 2 years posttreatment due to pyrazinamide use with susceptibility. In comparison with subgroup B, ARR-culture and ARR-success were 1.38 (95% confidence interval [CI], 0.89 to 2.12) and 1.38 (95% confidence interval [CI], 0.88 to 2.17), respectively. Corresponding findings were 0.99 (95% CI, 0.81 to 1.22) and 0.99 (95% CI, 0.78 to 1.26) in comparison with subgroup C and 1.09 (95% CI, 0.84 to 1.42) and 0.94 (95% CI, 0.74 to 1.20) in comparison with subgroup D. Early culture conversion significantly increased the incidence proportion of cure or treatment completion by 71% (95% CI, 26% to 133%). Selection bias among pyrazinamide nonusers might have underestimated the role of pyrazinamide. Comparison of pyrazinamide users showed that pyrazinamide increased the incidence proportion of early culture conversion and that of cure or treatment completion by a best estimate of 38% for both. This magnitude of change exceeded the 15 to 20% increase in the 2-month culture conversion rate of drug-susceptible TB that results from adding pyrazinamide to isoniazid and rifampin. Pyrazinamide is likely important in fluoroquinolone-based treatment of MDR-TB.
INTRODUCTION
First chemically synthesized by Dalmer and Walter in 1934 (4), pyrazinamide has probably attracted as much attention as rifampin in the treatment of tuberculosis (TB). By targeting ribosomal protein S1, thereby inhibiting trans-translation of nonreplicating persisters in an acidic microenvironment rather than actively multiplying tubercle bacilli (30), pyrazinamide has demonstrated sterilizing activity comparable to that of rifampin, when given together with streptomycin and isoniazid (9). Synergism between rifampin and pyrazinamide has been demonstrated by a reduction in the proportion of positive 2-month cultures and relapse rates (11). While there is clinical evidence for using fluoroquinolones (21, 41), second-line injectable drugs (SLIDs) (1, 20), and streptomycin (15) in the treatment of multidrug-resistant (MDR) tuberculosis (TB), corresponding evidence about the role of pyrazinamide in the treatment of MDR-TB is scarce (10, 24). The less favorable treatment outcomes among MDR-TB cases with resistance to all first-line TB drugs than those among other MDR-TB cases that harbored bacillary strains susceptible to ethambutol, streptomycin, or pyrazinamide might allude to a potentially important role of pyrazinamide in the treatment of pyrazinamide-susceptible MDR-TB (19). A recent study that reported the use of a gatifloxacin-based regimen among treatment-naïve MDR-TB patients (36) and our recent report on the feasibility of giving shorter treatment for selected MDR-TB patients to achieve cure (16) might also suggest a treatment-shortening role of pyrazinamide in pyrazinamide-susceptible MDR-TB. Despite the unparalleled effectiveness of pyrazinamide as a scavenger of persisters (22, 30), it remains uncertain whether pyrazinamide may add much to the treatment of MDR-TB in the presence of active drugs such as fluoroquinolones. Thus, it appears to be necessary to better delineate the role of pyrazinamide in MDR-TB treatment, especially when the unrivaled activity of pyrazinamide may be harnessed in the formulation of novel regimens that contain diarylquinoline (TMC207) (38) or nitroimidazo-oxazine (PA-824) (26).
In terms of drug use and drug susceptibility, there can be only four subgroups of patients: drug users with drug-susceptible disease, drug users with drug-resistant disease, drug nonusers with drug-susceptible disease, and drug nonusers with drug-resistant disease. As the effect of a drug must be exerted through use of a drug with in vivo activity, which is indirectly evaluated by drug susceptibility testing (DST), the role of a drug can be evaluated in an observational study by examining either drug susceptibility among drug users or drug use in comparison with nonuse. Selection for pyrazinamide use or nonuse may be biased by DST results and other clinical factors. Routinely done in Lowenstein-Jensen medium, DST results for pyrazinamide and second-line drugs in Hong Kong are often available at least 1 to 2 months after starting MDR-TB treatment. Pyrazinamide is commonly given alongside second-line drugs in the treatment of MDR-TB. Pyrazinamide nonuse might suggest selection bias due to favorable clinical factors. Thus, the role of pyrazinamide may be better evaluated by examining the association between treatment outcomes and pyrazinamide susceptibility among pyrazinamide users, rather than pyrazinamide use in comparison with nonuse. In fact, the same approach has been used to demonstrate the roles of fluoroquinolones (21, 41), second-line injectable agents (1, 20), and streptomycin (15) in the treatment of MDR-TB. Using updated data for a published MDR-TB cohort (16) that had been studied with prior approval from the Ethics Committee in the Department of Health in Hong Kong, this study aimed at evaluating the role of pyrazinamide in fluoroquinolone-based treatment of MDR-TB by estimating the adjusted risk ratio (ARR) of treatment outcome due to pyrazinamide use with susceptibility.
MATERIALS AND METHODS
By searching a territory-wide TB registry of 359 MDR-TB patients diagnosed between September 1996 and December 2009, we assembled a cohort of 194 MDR-TB patients given fluoroquinolone-containing regimens. Data collection was facilitated by a well-established health infrastructure with support from a World Health Organization (WHO)-designated supranational TB reference laboratory. Treatment outcome was evaluated by two endpoints: sputum culture conversion within 90 days after commencement of second-line treatment (early sputum culture conversion) and cure or treatment completion by 2 years after commencement of second-line treatment (treatment success). Sputum culture conversion was defined by the occurrence of two consecutive negative cultures of samples taken at least 30 days apart with no subsequent recurrence of a positive culture (39). In accordance with WHO guidelines (39), cure was defined as completion of treatment according to the program protocol with at least five consecutive negative cultures from sputum samples collected at least 30 days apart in the last 12 months of treatment, and treatment completion was defined as completion of treatment with fewer than five consecutive negative cultures in the last 12 months of treatment. Second-line treatment referred to the use of a treatment regimen comprising one or more drugs listed in groups 2 to 5 according to classification by WHO (39), except for streptomycin. Unfavorable treatment outcome included death from any cause during treatment, default, treatment failure, relapse, or inability to allocate to a treatment outcome that has been defined by WHO guidelines (36, 39). Only drug use exceeding 1 month was counted. Data were extracted by review of clinical records.
To optimize inclusion of major confounders and exclusion of nonconfounding variables, we followed basic principles in epidemiological studies with emphasis on the strength of association rather than statistical significance (27). We screened potential confounders by examining risk ratios in univariate analysis rather than P values from the chi-square test (with or without Yates' correction for continuity) or Fisher's exact test. A potential confounder must meet two criteria (27). First, it must be at least weakly associated with both the exposure factor (pyrazinamide use with susceptibility) and outcome (treatment success or early sputum culture conversion). Risk ratios of ≥1.2 or ≤0.9 were used to denote at least a weak association (25). Second, a potential confounder must individually cause at least a 10% change in the coefficient of the exposure factor upon inclusion in robust Poisson regression, which is probably the best available method for estimating adjusted risk ratios (44). Before multivariable analysis, multicollinearity was examined using the variance inflation factor, which was considered unacceptable when its value exceeded 1.4.
Statistical analysis was done in SPSS, version 15.0.
RESULTS
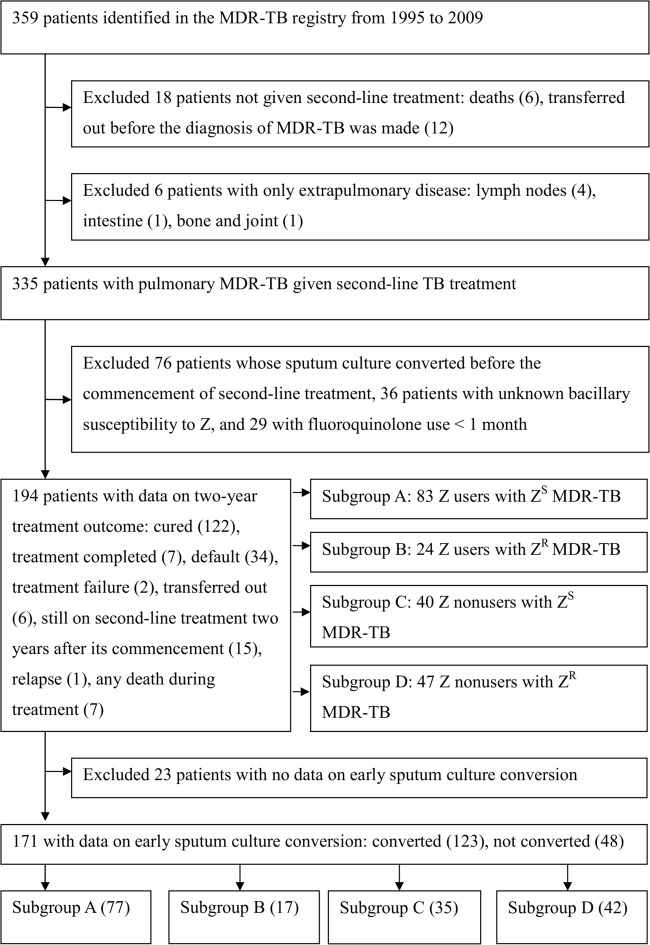
Figure 1 shows how we assembled a cohort of 194 MDR-TB patients treated with fluoroquinolone-containing regimens. Stratified by pyrazinamide use and susceptibility, there were 83 users with pyrazinamide-susceptible MDR-TB (subgroup A), 24 users with pyrazinamide-resistant MDR-TB (subgroup B), 40 nonusers with pyrazinamide-susceptible MDR-TB (subgroup C), and 47 nonusers with pyrazinamide-resistant MDR-TB (subgroup D).
Fig 1.
Flowchart of enrollment for cohort analyses. Numbers in parentheses show the number of subjects with the condition. Abbreviations: ZR, pyrazinamide resistant; ZS, pyrazinamide susceptible.
Table 1 shows a comparison between subgroup A and each of the other three subgroups. Compared with subgroup A, each of the three other subgroups showed comparable patient and disease characteristics. Subgroup A differed significantly from subgroup B as well as subgroup D in terms of drug susceptibility pattern and drug use. Respective proportions with bacillary susceptibility to ofloxacin, SLIDs, ethionamide, pyrazinamide, and cycloserine were significantly higher in subgroup A than subgroup B. The proportion that used cycloserine was significantly lower in subgroup A than subgroup B. The proportion of patients using fewer than four drugs with activity in vitro was significantly lower in subgroup A than subgroup B. The respective proportions with early sputum culture conversion and treatment success were both significantly higher in subgroup A than subgroup B. A similar pattern was observed in the comparison between subgroups A and D. The respective proportions with bacillary susceptibility to ofloxacin, SLIDs, ethionamide, pyrazinamide, and ethambutol were significantly higher in subgroup A than subgroup D. The proportion with use of ethambutol was significantly higher in subgroup A than subgroup D, whereas the respective proportions with use of cycloserine and para-aminosalicylic acid (PAS) were significantly lower in subgroup A than subgroup D. The proportion of patients using fewer than four drugs with activity in vitro was significantly lower in subgroup A than subgroup D. The proportion with early sputum culture conversion was significantly higher in subgroup A than subgroup D, but proportions with treatment success were comparable. Subgroups A and C (the two subgroups with pyrazinamide-susceptible MDR-TB) had comparable drug susceptibility patterns, but the proportion that used cycloserine and PAS was significantly higher among pyrazinamide nonusers (subgroup C). The respective proportions with early sputum culture conversion and treatment success were comparable between subgroups A and C.
Table 1.
Comparison of subgroup A and each of the other three subgroupsa
| Variable | No. (%) of subjects |
P |
|||||
|---|---|---|---|---|---|---|---|
| Subgroup A (n = 83) | Subgroup B (n = 24) | Subgroup C (n = 40) | Subgroup D (n = 47) | Subgroup B vs A | Subgroup C vs A | Subgroup D vs A | |
| Female | 21 (25) | 8 (33) | 8 (20) | 13 (28) | 0.60 | 0.67 | 0.769 |
| Age >44 yearsb | 41 (49) | 10 (42) | 22 (55) | 29 (62) | 0.50 | 0.56 | 0.176 |
| Non-Chinese | 9 (11) | 2 (8) | 5 (13) | 3 (6) | 1.00 | 0.77 | 0.534 |
| Nonpermanent resident | 17 (20) | 6 (25) | 8 (20) | 4 (9) | 0.85 | 1.00 | 0.125 |
| Ever a smoker | 50 (63) | 13 (57) | 26 (67) | 28 (64) | 0.78 | 0.66 | 0.900 |
| Adverse social factorsc | 23 (28) | 10 (42) | 15 (38) | 12 (26) | 0.29 | 0.27 | 0.788 |
| Comorbidityd | 43 (52) | 9 (38) | 19 (48) | 23 (49) | 0.22 | 0.65 | 0.753 |
| Second-line drug naïve and <1 mo of first-line drugs | 40 (48) | 10 (42) | 22 (55) | 21 (45) | 0.57 | 0.48 | 0.700 |
| Positive initial sputum smear | 59 (71) | 20 (83) | 28 (72) | 38 (81) | 0.35 | 0.94 | 0.219 |
| Disease on initial chest radiograph more than RUL/equivalent | 35 (43) | 13 (54) | 18 (46) | 20 (43) | 0.32 | 0.72 | 0.989 |
| Cavitation on initial chest radiograph | 42 (51) | 15 (63) | 20 (50) | 24 (51) | 0.30 | 0.95 | 0.960 |
| >50% treatment supervised by trained personnel | 64 (78) | 19 (79) | 31 (79) | 39 (83) | 1.00 | 1.00 | 0.657 |
| Use of: | |||||||
| SLIDs | 47 (57) | 16 (67) | 31 (78) | 31 (66) | 0.52 | 0.02 | 0.297 |
| Thioamide | 73 (88) | 19 (79) | 35 (88) | 37 (79) | 0.32 | 1.00 | 0.251 |
| Pyrazinamide | 83 (100) | 24 (100) | 0 (0%) | 0 (0) | NA | <0.001e | <0.001e |
| Streptomycin | 18 (22) | 5 (21) | 7 (18) | 7 (15) | 1.00 | 0.76 | 0.476 |
| Ethambutol | 53 (64) | 13 (54) | 24 (60) | 16 (34) | 0.53 | 0.68 | 0.001e |
| Cycloserine | 27 (33) | 15 (63) | 36 (90) | 39 (83) | 0.02e | <0.001e | <0.001e |
| PAS | 23 (28) | 9 (38) | 26 (65) | 37 (79) | 0.50 | <0.001e | <0.001e |
| Linezolid | 1 (1) | 0 (0) | 1 (3) | 2 (4) | 1.00 | 0.55 | 0.30 |
| Hepatotoxicity complicating TB treatment | 14 (17) | 1 (4) | 8 (20) | 5 (11) | 0.18 | 0.86 | 0.48 |
| Use of <4 drugs with activity in vitro | 13 (16) | 10 (42) | 7 (18) | 26 (55) | 0.01e | 1.00 | <0.001e |
| Susceptible to: | |||||||
| Ofloxacin | 77 (93) | 17 (71) | 34 (85) | 31 (66) | 0.01e | 0.20 | <0.001e |
| SLIDs | 78 (95) | 19 (79) | 37 (93) | 37 (79) | 0.03e | 0.68 | 0.010e |
| Ethionamide | 78 (94) | 19 (79) | 37 (93) | 36 (77) | 0.04e | 0.71 | 0.01e |
| Pyrazinamide | 83 (100) | 0 (0) | 40 (100) | 0 (0) | <0.001e | NA | <0.001e |
| Streptomycin | 26 (31) | 7 (29) | 12 (30) | 10 (21) | 1.00 | 0.88 | 0.22 |
| Ethambutol | 56 (67) | 12 (50) | 28 (70) | 18 (38) | 0.19 | 0.78 | 0.001e |
| Cycloserine | 81 (99) | 21 (88) | 40 (100) | 43 (91) | 0.04e | 1.00 | 0.06 |
| Treatment success | 59 (71) | 11 (46) | 28 (70) | 31 (66) | 0.04e | 0.90 | 0.54 |
| Early sputum culture conversion | 61 (79) | 9 (53) | 27 (77) | 26 (62) | 0.03e | 1.00 | 0.04e |
Less than 5% of the data were missing, except for smoking status among subgroup C (6.4% of data on smoking status were missing). Unless otherwise specified, use of drugs refers to use for >1 month. Abbreviations: CI, confidence interval; NA, not applicable; PAS, para-aminosalicylic acid; RUL, right upper lobe; SLIDs, second-line injectable drugs; TB, tuberculosis.
The median age of the cohort of 194 patients was 45 years.
Adverse social factors refer to financial difficulty that meets social security criteria, history of imprisonment, or history of drug addiction.
Comorbidity refers to diabetes mellitus, renal impairment, lung cancer, other malignancy, obstructive/restrictive lung disease, use of cytotoxic or steroids, liver disease, or HIV infection. The prevalence of HIV infection was less than 1%.
P < 0.05.
Table 2 shows the results of univariate analysis of factors that may confound the association between early sputum culture conversion and pyrazinamide use with susceptibility. Table 3 summarizes the procedures and results of robust Poisson regression analysis of early sputum culture conversion. A total of 11 factors showed at least a weak association with both early sputum culture conversion and pyrazinamide use with susceptibility. Eight factors resulted in a change of at least 10% in the coefficient of pyrazinamide use with susceptibility when they were individually included in the robust Poisson regression analysis. Excluding four factors by consideration of multicollinearity left four factors that may potentially confound the association between early sputum culture conversion and pyrazinamide use with susceptibility: use of ethambutol, use of PAS, and bacillary susceptibility to ofloxacin and ethionamide. Taking into account these four factors, robust Poisson regression analysis showed that the adjusted risk ratio of early sputum culture conversion due to pyrazinamide use with susceptibility was 1.38 (95% CI, 0.89 to 2.12) in comparison with pyrazinamide use with resistance (subgroup B), 0.99 (95% CI, 0.81 to 1.22) in comparison with pyrazinamide nonuse with susceptibility (subgroup C), and 1.09 (95% CI, 0.84 to 1.42) in comparison with pyrazinamide nonuse with resistance (subgroup D) (see footnotes in Table 3).
Table 2.
Univariate analysis of factors that may confound the association between early sputum culture conversion and pyrazinamide use with susceptibilitya
| Factor | Total no. of subjects for row | Z use with susceptibility |
Early sputum culture conversion |
||||
|---|---|---|---|---|---|---|---|
| No. (%) of subjects | RR | P | No. (%) of subjects | RR | P | ||
| Sex | |||||||
| Male | 129 | 59 (46) | 0.94 | 0.75 | 91 (71) | 1.08 | 0.48 |
| Female | 42 | 18 (43) | 32 (76) | ||||
| Age group (yr)b | |||||||
| ≤44 | 81 | 40 (49) | 0.83 | 0.28 | 60 (74) | 0.95 | 0.55 |
| >44 | 90 | 37 (41) | 63 (70) | ||||
| Ethnicity | |||||||
| Chinese | 155 | 69 (45) | 1.05 | 1.00 | 113 (73) | 0.82 | 0.37 |
| Others | 15 | 7 (47) | 9 (60) | ||||
| Permanent resident | |||||||
| No | 143 | 62 (43) | 1.24 | 0.32 | 104 (73) | 0.93 | 0.77 |
| Yes | 28 | 15 (54) | 19 (68) | ||||
| Ever a smoker | |||||||
| No | 59 | 26 (44) | 1.04 | 0.84 | 46 (78) | 0.87 | 0.16 |
| Yes | 105 | 48 (46) | 71 (68) | ||||
| Adverse social factorc | |||||||
| No | 115 | 54 (47) | 0.87 | 0.47 | 88 (77) | 0.82 | 0.06 |
| Yes | 56 | 23 (41) | 35 (63) | ||||
| Comorbidityd | |||||||
| No | 85 | 35 (41) | 1.19 | 0.31 | 59 (69) | 1.07 | 0.47 |
| Yes | 86 | 42 (49) | 64 (74) | ||||
| Second-line drug naïve and <1 mo of first-line drugs | |||||||
| No | 90 | 41 (46) | 0.98 | 0.88 | 56 (62) | 1.33 | 0.003 |
| Yes | 81 | 36 (44) | 67 (83) | ||||
| Initial sputum smear | |||||||
| Negative | 40 | 21 (53) | 0.82 | 0.30 | 29 (73) | 0.99 | 0.91 |
| Positive | 130 | 56 (43) | 93 (72) | ||||
| Disease on initial chest radiograph more than RUL/equivalent | |||||||
| No | 92 | 42 (46) | 0.97 | 0.85 | 66 (72) | 1.00 | 0.96 |
| Yes | 77 | 34 (44) | 55 (71) | ||||
| Cavitation on initial chest radiograph | |||||||
| No | 80 | 36 (45) | 1.00 | 0.99 | 57 (71) | 1.02 | 0.85 |
| Yes | 91 | 41 (45) | 66 (73) | ||||
| >50% treatment supervised by trained personnel | |||||||
| No | 33 | 16 (48) | 0.91 | 0.65 | 23 (70) | 1.03 | 0.96 |
| Yes | 136 | 60 (44) | 98 (72) | ||||
| Use of SLIDs | |||||||
| No | 61 | 34 (56) | 0.70 | 0.04 | 44 (72) | 1.00 | 0.97 |
| Yes | 110 | 43 (39) | 79 (72) | ||||
| Use of thioamide | |||||||
| No | 27 | 10 (37) | 1.26 | 0.36 | 16 (59) | 1.25 | 0.17 |
| Yes | 144 | 67 (47) | 107 (74) | ||||
| Use of streptomycin | |||||||
| No | 138 | 60 (43) | 1.18 | 0.40 | 99 (72) | 1.01 | 1.00 |
| Yes | 33 | 17 (52) | 24 (73) | ||||
| Use of ethambutol | |||||||
| No | 73 | 28 (38) | 1.30 | 0.13 | 47 (64) | 1.20 | 0.06 |
| Yes | 98 | 49 (50) | 76 (78) | ||||
| Use of cycloserine | |||||||
| No | 65 | 50 (77) | 0.33 | <0.001 | 53 (82) | 0.81 | 0.03 |
| Yes | 106 | 27 (25) | 70 (66) | ||||
| Use of PAS | |||||||
| No | 86 | 55 (64) | 0.40 | <0.001 | 66 (77) | 0.87 | 0.16 |
| Yes | 85 | 22 (26) | 57 (67) | ||||
| Use of linezolid | |||||||
| No | 167 | 76 (46) | 0.55 | 0.63 | 120 (72) | 1.04 | 1.00 |
| Yes | 4 | 1 (25) | 3 (75) | ||||
| Hepatotoxicity complicating TB treatment | |||||||
| No | 146 | 65 (45) | 1.08 | 0.75 | 103 (71) | 1.13 | 0.47 |
| Yes | 25 | 12 (48) | 20 (80) | ||||
| Use of <4 drugs with activity in vitro | |||||||
| No | 125 | 64 (51) | 0.55 | 0.01 | 100 (80) | 0.63 | <0.001 |
| Yes | 46 | 13 (28) | 23 (50) | ||||
| Susceptible to ofloxacin | |||||||
| No | 29 | 6 (21) | 2.42 | 0.004 | 12 (41%) | 1.89 | <0.001 |
| Yes | 142 | 71 (50) | 111 (78) | ||||
| Susceptible to SLIDs | |||||||
| No | 20 | 4 (20) | 2.40 | 0.03 | 9 (45) | 1.67 | 0.01 |
| Yes | 150 | 72 (48) | 113 (75) | ||||
| Susceptible to ethionamide | |||||||
| No | 22 | 5 (23) | 2.13 | 0.04 | 10 (45) | 1.67 | 0.007 |
| Yes | 149 | 72 (48) | 113 (76) | ||||
| Susceptible to streptomycin | |||||||
| No | 122 | 53 (43) | 1.13 | 0.51 | 86 (70) | 1.07 | 0.51 |
| Yes | 49 | 24 (49) | 37 (76) | ||||
| Susceptible to ethambutol | |||||||
| No | 69 | 26 (38) | 1.33 | 0.11 | 43 (62) | 1.26 | 0.02 |
| Yes | 102 | 51 (50) | 80 (78) | ||||
| Susceptible to cycloserine | |||||||
| No | 6 | 1 (17) | 2.74 | 0.23 | 5 (83) | 0.86 | 1.00 |
| Yes | 164 | 75 (46) | 117 (71) | ||||
| Z use with susceptibility | |||||||
| Yes | 77 | NA | NA | NA | 61 (79) | 0.83 | 0.06 |
| Others | 94 | NA | 62 (66) | ||||
Less than 5% of data were missing. Unless otherwise specified, use of drugs refers to use for >1 month. Factors with risk ratios of ≥1.2 or ≤0.9 in both exposure factor and outcome are shown in bold. Abbreviations: NA, not applicable; PAS, para-aminosalicylic acid; RR, risk ratio; RUL, right upper lobe; SLIDs, second-line injectable drugs; TB, tuberculosis; Z, pyrazinamide.
The median age of the cohort of 194 patients was 45 years.
Adverse social factors refer to financial difficulty that meets social security criteria, history of imprisonment, or history of drug addiction.
Comorbidity refers to diabetes mellitus, renal impairment, lung cancer, other malignancy, obstructive/restrictive lung disease, use of cytotoxic or steroids, liver disease, or HIV infection. The prevalence of HIV infection was less than 1%.
Table 3.
Procedures and results of robust Poisson regression analysis of the association between early sputum culture conversion and pyrazinamide use with susceptibilitya
| Factor | Change in coefficient of Z use with susceptibility (%) | Reason for exclusion from multivariable analysis | Adjusted risk ratio (95% CI) |
|---|---|---|---|
| Adverse social factor | −4.9 | <10% change in coefficient | |
| Use of thioamide | −5.5 | <10% change in coefficient | |
| Use of ethambutolb | −10.4 | 1.08 (0.89–1.30) | |
| Use of cycloserine | −42.6 | Multicollinearity | |
| Use of PASb | −15.8 | 1.02 (0.84–1.24) | |
| Use of <4 drugs with activity in vitro | −39.3 | Multicollinearity | |
| Susceptible to ofloxacinb | −44.8 | 1.68 (1.08–2.62) | |
| Susceptible to SLIDs | −27.3 | Multicollinearity | |
| Susceptible to ethionamideb | −25.1 | 1.35 (0.84–2.16) | |
| Susceptible to ethambutol | −13.1 | Multicollinearity | |
| Susceptible to cycloserine | 3.3 | <10% change in coefficient | |
| Z use with susceptibilityb,c | Reference | ||
| Z use with resistance (subgroup B) | 0.727 (0.469–1.127)d | ||
| Z nonuse with susceptibility (subgroup C) | 1.008 (0.823–1.234)e | ||
| Z nonuse with resistance (subgroup D) | 0.914 (0.703–1.190)f |
See footnote a of Table 2 for definitions of abbreviations.
These five factors were included in robust Poisson regression analysis to estimate the adjusted risk ratios of early sputum culture conversion in the presence of pyrazinamide use with susceptibility in comparison with each of the other alternatives.
In univariate analysis, this factor was evaluated as a binary variable comprising pyrazinamide use with susceptibility as the reference subgroup versus the others. After identifying potential factors that may confound the association between this factor and early sputum culture conversion, “others” was expanded into three subgroups, namely, pyrazinamide use with resistance, pyrazinamide nonuse with susceptibility, and pyrazinamide nonuse with resistance.
Taking subgroup B (pyrazinamide use with resistance) as the reference group, the adjusted risk ratio becomes 1.38 (95% CI, 0.89 to 2.12), which is the reciprocal of 0.727 (95% CI, 0.469 to 1.127).
Taking subgroup C (pyrazinamide nonuse with susceptibility) as the reference group, the adjusted risk ratio becomes 0.99 (95% CI, 0.81 to 1.22), which is the reciprocal of 1.008 (95% CI, 0.823 to 1.234).
Taking subgroup D (pyrazinamide nonuse with resistance) as the reference group, the adjusted risk ratio becomes 1.09 (95% CI, 0.84 to 1.42), which is the reciprocal of 0.914 (95% CI, 0.703 to 1.190).
Tables 4 and 5 summarize the results of univariate and multivariable analyses of factors that may confound the association between treatment success and pyrazinamide use with susceptibility. Taking into account adverse social factors and the total number of drugs used with activity in vitro, robust Poisson regression analysis showed that the adjusted risk ratio of treatment success due to pyrazinamide use with susceptibility was 1.38 (95% CI, 0.88 to 2.17) in comparison with pyrazinamide use with resistance (subgroup B), 0.99 (95% CI, 0.78 to 1.26) in comparison with pyrazinamide nonuse with susceptibility (subgroup C), and 0.94 (95% CI, 0.74 to 1.20) in comparison with pyrazinamide nonuse with resistance (subgroup D) (see footnotes in Table 5).
Table 4.
Univariate analysis of factors that may confound the association between treatment success and pyrazinamide use with susceptibilitya
| Factor | Total no. of subjects for row | Z use with susceptibility |
Treatment success |
||||
|---|---|---|---|---|---|---|---|
| No. (%) of subjects | RR | P | No. (%) of subjects | RR | P | ||
| Sex | |||||||
| Male | 144 | 62 (43) | 0.98 | 0.90 | 96 (67) | 0.99 | 0.93 |
| Female | 50 | 21 (42) | 33 (66) | ||||
| Age group (yr)b | |||||||
| ≤44 | 92 | 42 (46) | 0.88 | 0.44 | 60 (65) | 1.04 | 0.72 |
| >44 | 102 | 41 (40) | 69 (68) | ||||
| Ethnicity | |||||||
| Chinese | 174 | 73 (42) | 1.13 | 0.83 | 122 (70) | 0.45 | 0.002 |
| Others | 19 | 9 (47) | 6 (32) | ||||
| Permanent resident | |||||||
| No | 159 | 66 (42) | 1.17 | 0.45 | 109 (69) | 0.83 | 0.20 |
| Yes | 35 | 17 (49) | 20 (57) | ||||
| Ever a smoker | |||||||
| No | 69 | 30 (43) | 0.98 | 0.92 | 47 (68) | 0.95 | 0.66 |
| Yes | 117 | 50 (43) | 76 (65) | ||||
| Adverse social factorc | |||||||
| No | 134 | 60 (45) | 0.86 | 0.40 | 95 (71) | 0.80 | 0.05 |
| Yes | 60 | 23 (38) | 34 (57) | ||||
| Comorbidityd | |||||||
| No | 100 | 40 (40) | 1.14 | 0.42 | 64 (64) | 1.08 | 0.45 |
| Yes | 94 | 43 (46) | 65 (69) | ||||
| Second-line drug naïve and <1 mo of first-line drugs | |||||||
| No | 101 | 43 (43) | 1.01 | 0.95 | 63 (62) | 1.14 | 0.21 |
| Yes | 93 | 40 (43) | 66 (71) | ||||
| Initial sputum smear | |||||||
| Negative | 48 | 24 (50) | 0.81 | 0.26 | 29 (60) | 1.13 | 0.32 |
| Positive | 145 | 59 (41) | 99 (68) | ||||
| Disease on initial chest radiograph more than RUL/equivalent | |||||||
| No | 106 | 47 (44) | 0.92 | 0.61 | 69 (65) | 1.04 | 0.73 |
| Yes | 86 | 35 (41) | 58 (67) | ||||
| Cavitation on initial chest radiograph | |||||||
| No | 93 | 41 (44) | 0.94 | 0.73 | 58 (62) | 1.13 | 0.24 |
| Yes | 101 | 42 (42) | 71 (70) | ||||
| >50% treatment supervised by trained personnel | |||||||
| No | 39 | 18 (46) | 0.91 | 0.63 | 23 (59) | 1.17 | 0.22 |
| Yes | 153 | 64 (42) | 106 (69) | ||||
| Use of SLIDs | |||||||
| No | 69 | 36 (52) | 0.72 | 0.05 | 44 (64) | 1.07 | 0.55 |
| Yes | 125 | 47 (38) | 85 (68) | ||||
| Use of thioamide | |||||||
| No | 30 | 10 (33) | 1.34 | 0.26 | 18 (60) | 1.13 | 0.41 |
| Yes | 164 | 73 (45) | 111 (68) | ||||
| Use of streptomycin | |||||||
| No | 157 | 65 (41) | 1.18 | 0.42 | 102 (65) | 1.12 | 0.35 |
| Yes | 37 | 18 (49) | 27 (73) | ||||
| Use of ethambutol | |||||||
| No | 88 | 30 (34) | 1.47 | 0.03 | 53 (60) | 1.19 | 0.09 |
| Yes | 106 | 53 (50) | 76 (72) | ||||
| Use of cycloserine | |||||||
| No | 77 | 56 (73) | 0.32 | <0.001 | 49 (64) | 1.07 | 0.49 |
| Yes | 117 | 27 (23) | 80 (68) | ||||
| Use of PAS | |||||||
| No | 99 | 60 (61) | 0.40 | <0.001 | 68 (69) | 0.93 | 0.51 |
| Yes | 95 | 23 (24) | 61 (64) | ||||
| Use of linezolid | |||||||
| No | 190 | 82 (43) | 0.58 | 0.64 | 125 (66) | 1.52 | 0.30 |
| Yes | 4 | 1 (25) | 4 (100) | ||||
| Hepatotoxicity complicating TB treatment | |||||||
| No | 166 | 69 (42) | 1.20 | 0.40 | 109 (66) | 1.09 | 0.70 |
| Yes | 28 | 14 (50) | 20 (71) | ||||
| Use of <4 drugs with activity in vitro | |||||||
| No | 138 | 70 (51) | 0.46 | <0.001 | 101 (73) | 0.68 | 0.002 |
| Yes | 56 | 13 (23) | 28 (50) | ||||
| Susceptible to ofloxacin | |||||||
| No | 35 | 6 (17) | 2.82 | 0.001 | 19 (54) | 1.27 | 0.09 |
| Yes | 159 | 77 (48) | 110 (69) | ||||
| Susceptible to SLIDs | |||||||
| No | 22 | 4 (18) | 2.51 | 0.03 | 13 (59) | 1.14 | 0.60 |
| Yes | 171 | 78 (46) | 115 (67) | ||||
| Susceptible to ethionamide | |||||||
| No | 24 | 5 (21) | 2.20 | 0.02 | 15 (63) | 1.07 | 0.83 |
| Yes | 170 | 78 (46) | 114 (67) | ||||
| Susceptible to streptomycin | |||||||
| No | 139 | 57 (41) | 1.15 | 0.43 | 92 (66) | 1.02 | 0.89 |
| Yes | 55 | 26 (47) | 37 (67) | ||||
| Susceptible to ethambutol | |||||||
| No | 80 | 27 (34) | 1.46 | 0.03 | 50 (63) | 1.11 | 0.32 |
| Yes | 114 | 56 (49) | 79 (69) | ||||
| Susceptible to cycloserine | |||||||
| No | 8 | 1 (13) | 3.50 | 0.14 | 6 (75) | 0.88 | 0.72 |
| Yes | 185 | 81 (44) | 122 (66) | ||||
| Z use with susceptibility | |||||||
| Yes | 83 | NA | NA | NA | 59 (71) | 0.89 | 0.24 |
| Others | 111 | NA | 70 (63) | ||||
Table 5.
Procedures and results of robust Poisson regression analysis of association between treatment success and pyrazinamide use with susceptibilitya
| Factor | Change in coefficient of Z use with susceptibility (%) | Reason for exclusion from multivariable analysis | Adjusted risk ratio (95% CI) |
|---|---|---|---|
| Adverse social factorb | −10.0 | 0.81 (0.64–1.03) | |
| Use of linezolid | 6.7 | <10% change in coefficient | |
| Use of <4 drugs with activity in vitrob | −65.0 | 0.68 (0.51–0.91) | |
| Susceptible to ofloxacin | −31.7 | Multicollinearity | |
| Susceptible to cycloserine | 3.3 | <10% change in coefficient | |
| Z use with susceptibilityb,c | Subgroup A as reference | ||
| Z use with resistance (subgroup B) | 0.723 (0.460–1.135)d | ||
| Z nonuse with susceptibility (subgroup C) | 1.006 (0.792–1.278)e | ||
| Z nonuse with resistance (subgroup D) | 1.062 (0.832–1.355)f |
See footnote a of Table 2 for definitions of abbreviations.
These three factors were included in robust Poisson regression analysis to estimate the adjusted risk ratios of treatment success in the presence of pyrazinamide use with susceptibility in comparison with each of the other alternatives.
In univariate analysis, this factor was evaluated as a binary variable comprising pyrazinamide use with susceptibility as the reference subgroup versus the others. After identifying potential factors that may confound the association between this factor and treatment success, “others” was expanded into three subgroups, namely, pyrazinamide use with resistance, pyrazinamide nonuse with susceptibility, and pyrazinamide nonuse with resistance.
Taking subgroup B (pyrazinamide use with resistance) as the reference group, the adjusted risk ratio becomes 1.38 (95% CI, 0.88 to 2.17), which is the reciprocal of 0.723 (95% CI, 0.460 to 1.135).
Taking subgroup C (pyrazinamide nonuse with susceptibility) as the reference group, the adjusted risk ratio becomes 0.99 (95% CI, 0.78 to 1.26), which is the reciprocal of 1.006 (95% CI, 0.792 to 1.278).
Taking subgroup D (pyrazinamide nonuse with resistance) as the reference group, the adjusted risk ratio becomes 0.94 (95% CI, 0.74 to 1.20), which is the reciprocal of 1.062 (95% CI, 0.832 to 1.355).
The adjusted risk ratio of treatment success due to early sputum culture conversion was 1.71 (95% CI, 1.26 to 2.33). Subgroup analysis showed similar estimates for the adjusted risk ratio: 1.63 (95% CI, 1.14 to 2.34) for subgroups A and D, 1.66 (95% CI, 1.10 to 2.50) for subgroups A and C, and 1.78 (95% CI, 1.13 to 2.78) for subgroups A and B.
DISCUSSION
It was the primary objective of this observational study to focus on the strength of association rather than statistical significance. By following basic epidemiological principles in controlling for major confounders, this study suggests that pyrazinamide use with susceptibility among pyrazinamide users considerably increases the incidence proportion of early sputum culture conversion and that of treatment success by a best estimate of 38% for both. As this magnitude of change exceeds the 15 to 20% increase in the 2-month culture conversion rate of drug-susceptible TB that results from adding pyrazinamide to isoniazid and rifampin (5–8), our study suggests that pyrazinamide has an important role in fluoroquinolone-based treatment of MDR-TB. Furthermore, we found that early sputum culture conversion significantly increased the incidence proportion of treatment success by 71% (95% CI, 26% to 133%). This finding corroborated a previous study of MDR-TB patients (41), which showed that negative sputum cultures after 2 and 3 months of therapy with ofloxacin- or levofloxacin-containing regimens were 100% predictive of cure.
Selection bias is a major problem in observational studies. While restriction, stratification, and regression analysis may help control for major confounding factors, selection bias is often not amenable to correction at the analysis stage. The much attenuated estimates of adjusted risk ratios based on a comparison that involved pyrazinamide nonusers (subgroups C and D) might be attributable to selection bias.
Our findings corroborate the latest WHO recommendation regarding the use of pyrazinamide in the treatment of MDR-TB alongside a minimum of 4 second-line drugs that are likely to be effective (10). The WHO recommendation is weakly based on a slightly added benefit due to pyrazinamide found in one analysis included in the literature review (10). Only one small retrospective study of MDR-TB has suggested that including both pyrazinamide and ethambutol in the treatment regimen substantially reduced the odds of treatment failure or death (24).
The current study may underline the importance of routinely ascertaining pyrazinamide susceptibility to facilitate the treatment of MDR-TB, as we have recently proposed in a review article (42a). Baseline pyrazinamide resistance among MDR-TB patients is by no means uncommon. A systematic review shows that the prevalence of pyrazinamide resistance for culture isolates of MDR M. tuberculosis is considerably higher than that for culture isolates susceptible to isoniazid and rifampin (medians, 51% versus 5%; ranges, 31% to 89% versus 0% to 9%) (3). This may be anticipated, as pyrazinamide is probably the only drug with activity against tubercle bacilli inhibited by acidic pH (23). The WHO recommendation regarding pyrazinamide use has made no reference to pyrazinamide susceptibility testing, probably because of the technical challenges in testing pyrazinamide susceptibility in phenotypic assays (42, 42a). With recent advances in and the significantly reduced cost of DNA sequencing (28), it is hoped that this problem may be solved in the near future by molecular tests based on detection of pncA mutations (29), which is reasonably reliable for predicting pyrazinamide susceptibility in the context of MDR-TB (3). Pyrazinamide use is not without a considerable risk of hepatotoxicity (2), although a retrospective study has recently suggested that hepatotoxicity may not adversely affect the outcome of treatment for MDR-TB (14). If reliable pyrazinamide susceptibility testing results are not available, it may be prudent to weigh pyrazinamide use against treatment efficacy, tolerance, and safety.
The therapeutic effect of pyrazinamide in the treatment of MDR-TB is biologically plausible. One Russian study has suggested in vitro synergistic effects between levofloxacin and pyrazinamide (31). It has been demonstrated in the murine TB model that a companion drug, which can be bacteriostatic (18) or preferably bactericidal (17), is required to elicit the therapeutic benefit of pyrazinamide. In the treatment of tuberculosis with bacillary resistance to streptomycin and isoniazid, a few studies demonstrated high cure rates from combination therapy with pyrazinamide, ethionamide, and cycloserine (32, 35, 43). By virtue of its bactericidal effect, a fluoroquinolone may be the key component in the current MDR-TB treatment regimen that elicits the therapeutic benefit of pyrazinamide. Although it remains to be proven whether bactericidal synergism between pyrazinamide and PA-824 (34), TMC207 (13, 33), clofazimine (33), and possibly, thioridazine (37) in the murine TB model may translate into better treatment of MDR-TB in clinical trials, our findings suggest that the therapeutic benefit of pyrazinamide in the treatment of MDR-TB should be further evaluated in randomized controlled trials with special consideration of routine pyrazinamide susceptibility testing plus a shorter treatment duration with pyrazinamide use.
The current study, based on a retrospective analysis of data collected in a TB program setting, has limitations inherent to the study design. First, our sample size was insufficient for demonstrating statistical significance. Our focus was on the estimation of the adjusted risk ratio, with meticulous consideration and careful identification of major confounders. Second, some misclassification bias in sputum culture conversion would be inevitable. Similar bias would also apply to all analyzed data, including false-positive pyrazinamide resistance due to the intrinsic problems of phenotypic pyrazinamide susceptibility testing methods (42) and the inherent limitations of drug susceptibility testing for ethionamide, PAS, and cycloserine (40). However, such bias was probably nondifferential, with a tendency to diminish rather than inflate the strength of association (27). Third, our findings cannot be extrapolated to the combination of pyrazinamide and other novel drugs in the pipeline. Fourth, we have not examined the optimal duration of pyrazinamide use in the treatment of MDR-TB. Unlike the case in drug-susceptible TB, whereby the activity of pyrazinamide is largely confined to the first 2 months of treatment (12), the optimal duration of pyrazinamide use in MDR-TB may vary according to the potency of the given regimen, bacillary load, and host immunity.
In conclusion, our study suggests that pyrazinamide use with susceptibility increases the incidence proportion of early sputum culture conversion and that of treatment success by a best estimate of 38% for both. Taking into account the impact on the 2-month culture conversion rate of drug-susceptible TB by adding pyrazinamide to isoniazid and rifampin, pyrazinamide may be important in fluoroquinolone-based MDR-TB treatment.
ACKNOWLEDGMENTS
This study was not supported by any funding.
We acknowledge the contribution from all colleagues in the Tuberculosis and Chest Service for their great efforts in keeping good records and maintaining a territory-wide MDR-TB registry.
We have no conflicts to declare.
Footnotes
Published ahead of print 6 August 2012
REFERENCES
- 1. Chan ED, Strand MJ, Iseman MD. 2009. Multidrug-resistant tuberculosis (TB) resistant to fluoroquinolones and streptomycin but susceptible to second-line injection therapy has a better prognosis than extensively drug-resistant TB. Clin. Infect. Dis. 48:e50–e52 [DOI] [PubMed] [Google Scholar]
- 2. Chang KC, Leung CC, Yew WW, Lau TY, Tam CM. 2008. Hepatotoxicity of pyrazinamide: cohort and case-control analyses. Am. J. Respir. Crit. Care Med. 177:1391–1396 [DOI] [PubMed] [Google Scholar]
- 3. Chang KC, Yew WW, Zhang Y. 2011. Pyrazinamide susceptibility testing in Mycobacterium tuberculosis: a systematic review with meta-analyses. Antimicrob. Agents Chemother. 55:4499–4505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dalmer O, Walter E, Firma E. 1936. Merck in Darmstadt. Verfahren zur Herstellung von Abkömmlingen der Pyrazinmonocarbonsäure. Patentiert im Deutschen Reiche vom 8. Juli 1934 ab. German patent 632 257 Klasse 12 p Gruppe 6 M 127990 IV a/12 p [Google Scholar]
- 5. East African/British Medical Research Council 1974. Controlled clinical trial of four short-course (6-month) regimens of chemotherapy for treatment of pulmonary tuberculosis. Lancet ii:1100–1106 [PubMed] [Google Scholar]
- 6. East African/British Medical Research Council 1976. Controlled clinical trial of four 6-month regimens of chemotherapy for pulmonary tuberculosis. Second report. Second East African/British Medical Research Council Study. Am. Rev. Respir. Dis. 114:471–475 [DOI] [PubMed] [Google Scholar]
- 7. East African/British Medical Research Council 1978. Controlled clinical trial of four short-course regimens of chemotherapy for two durations in the treatment of pulmonary tuberculosis: first report: Third East African/British Medical Research Councils study. Am. Rev. Respir. Dis. 118:39–48 [DOI] [PubMed] [Google Scholar]
- 8. East African/British Medical Research Council 1980. Controlled clinical trial of four short-course regimens of chemotherapy for two durations in the treatment of pulmonary tuberculosis. Second report. Third East African/British Medical Research Council Study. Tubercle 61:59–69 [DOI] [PubMed] [Google Scholar]
- 9. East African/British Medical Research Councils 1973. Controlled clinical trial of four short-course (6-month) regimens of chemotherapy for treatment of pulmonary tuberculosis. Second report. Lancet i:1331–1338 [PubMed] [Google Scholar]
- 10. Falzon D, et al. 2011. WHO guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Eur. Respir. J. 38:516–528 [DOI] [PubMed] [Google Scholar]
- 11. Hong Kong Chest Service/British Medical Research Council 1979. Controlled trial of 6-month and 8-month regimens in the treatment of pulmonary tuberculosis: the results up to 24 months. Tubercle 60:201–210 [DOI] [PubMed] [Google Scholar]
- 12. Hong Kong Chest Service/British Medical Research Council 1991. Controlled trial of 2, 4, and 6 months of pyrazinamide in 6-month, three-times-weekly regimens for smear-positive pulmonary tuberculosis, including an assessment of a combined preparation of isoniazid, rifampin, and pyrazinamide. Results at 30 months. Am. Rev. Respir. Dis. 143:700–706 [DOI] [PubMed] [Google Scholar]
- 13. Ibrahim M, et al. 2007. Synergistic activity of R207910 combined with pyrazinamide against murine tuberculosis. Antimicrob. Agents Chemother. 51:1011–1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Keshavjee S, et al. 2012. Hepatotoxicity during treatment for multidrug-resistant tuberculosis: occurrence, management and outcome. Int. J. Tuberc. Lung Dis. 16:596–603 [DOI] [PubMed] [Google Scholar]
- 15. Kim DH, et al. 2010. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Am. J. Respir. Crit. Care Med. 182:113–119 [DOI] [PubMed] [Google Scholar]
- 16. Leung ECC, Yew WW, Leung CC, Leung WM, Tam CM. 2011. Shorter treatment duration for selected patients with multidrug-resistant tuberculosis. Eur. Respir. J. 38:227–230 [DOI] [PubMed] [Google Scholar]
- 17. McCune RM, Jr, Feldmann FM, Lambert HP, McDermott W. 1966. Microbial persistence. I. The capacity of tubercle bacilli to survive sterilization in mouse tissues. J. Exp. Med. 123:445–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McCune RM, Jr, McDermott W, Tompsett R. 1956. The fate of Mycobacterium tuberculosis in mouse tissues as determined by the microbial enumeration technique. II. The conversion of tuberculous infection to the latent state by the administration of pyrazinamide and a companion drug. J. Exp. Med. 104:763–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Migliori GB, et al. 2007. Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur. Respir. J. 30:623–626 [DOI] [PubMed] [Google Scholar]
- 20. Migliori GB, et al. 2008. Resistance to second-line injectables and treatment outcomes in multidrug-resistant and extensively drug-resistant tuberculosis cases. Eur. Respir. J. 31:1155–1159 [DOI] [PubMed] [Google Scholar]
- 21. Migliori GB, et al. 2008. Fluoroquinolones: are they essential to treat multidrug-resistant tuberculosis? Eur. Respir. J. 31:904–905 [DOI] [PubMed] [Google Scholar]
- 22. Mitchison D, Davies G. 2012. The chemotherapy of tuberculosis: past, present and future. Int. J. Tuberc. Lung Dis. 16:724–732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mitchison DA. 1998. How drug resistance emerges as a result of poor compliance during short course chemotherapy for tuberculosis. Int. J. Tuberc. Lung Dis. 2:10–15 [PubMed] [Google Scholar]
- 24. Mitnick C, et al. 2003. Community-based therapy for multidrug-resistant tuberculosis in Lima, Peru. N. Engl. J. Med. 348:119–128 [DOI] [PubMed] [Google Scholar]
- 25. Monson R. 1990. Occupational epidemiology, 2nd ed CRC Press Inc., Boca Raton, FL [Google Scholar]
- 26. Nuermberger E, et al. 2008. Powerful bactericidal and sterilizing activity of a regimen containing PA-824, moxifloxacin, and pyrazinamide in a murine model of tuberculosis. Antimicrob. Agents Chemother. 52:1522–1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rothman KJ. 2002. Epidemiology: an introduction. Oxford University Press, Oxford, United Kingdom [Google Scholar]
- 28. Schuster SC. 2008. Next-generation sequencing transforms today's biology. Nat. Methods 5:16–18 [DOI] [PubMed] [Google Scholar]
- 29. Scorpio A, Zhang Y. 1996. Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat. Med. 2:662–667 [DOI] [PubMed] [Google Scholar]
- 30. Shi W, et al. 2011. Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. Science 333:1630–1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sokolova GB, Semenova OV, Bogadel'nikova IV, Kunichan AD. 2002. Effect of levofloxacine on cell elements of the lung tissue and on the growth of drug resistant Mycobacteria tuberculosis. Antibiot. Khimioter. 47:12–17 (In Russian.) [PubMed] [Google Scholar]
- 32. Somner AR, Brace AA. 1966. Late results of treatment of chronic drug-resistant pulmonary tuberculosis. Br. Med. J. 1:775–778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tasneen R, et al. 2011. Sterilizing activity of novel TMC207- and PA-824-containing regimens in a murine model of tuberculosis. Antimicrob. Agents Chemother. 55:5485–5492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tasneen R, Tyagi S, Williams K, Grosset J, Nuermberger E. 2008. Enhanced bactericidal activity of rifampin and/or pyrazinamide when combined with PA-824 in a murine model of tuberculosis. Antimicrob. Agents Chemother. 52:3664–3668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tousek J, Jancik E, Zelenka M, Jancikova-Máková M. 1967. The results of treatment in patients with cultures resistant to streptomycin, isoniazid and PAS: a five-year follow-up. Tubercle 48:27–31 [DOI] [PubMed] [Google Scholar]
- 36. Van Deun A, et al. 2010. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am. J. Respir. Crit. Care Med. 182:684–692 [DOI] [PubMed] [Google Scholar]
- 37. van Soolingen D, et al. 2010. The antipsychotic thioridazine shows promising therapeutic activity in a mouse model of multidrug-resistant tuberculosis. PLoS One 5:e12640 doi:10.1371/journal.pone.0012640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Veziris N, et al. 2009. A once-weekly R207910-containing regimen exceeds activity of the standard daily regimen in murine tuberculosis. Am. J. Respir. Crit. Care Med. 179:75–79 [DOI] [PubMed] [Google Scholar]
- 39. World Health Organization 2008. Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. WHO/HTM/TB/2008.402 World Health Organization, Geneva, Switzerland [Google Scholar]
- 40. World Health Organization 2008. Policy guidance on drug-susceptibility testing (DST) of second-line antituberculosis drugs. WHO/HTM/TB/2008.392 World Health Organization, Geneva, Switzerland: [PubMed] [Google Scholar]
- 41. Yew WW, et al. 2000. Outcomes of patients with multidrug-resistant pulmonary tuberculosis treated with ofloxacin/levofloxacin-containing regimens. Chest 117:744–751 [DOI] [PubMed] [Google Scholar]
- 42. Zhang Y, Mitchison D. 2003. The curious characteristics of pyrazinamide: a review. Int. J. Tuberc. Lung Dis. 7:6–21 [PubMed] [Google Scholar]
- 42a. Zhang Y, et al. 2012. ‘ZS-MDR-TB’ versus ‘ZR-MDR-TB’: improving treatment of MDR-TB by identifying pyrazinamide susceptibility. Emerg. Microbes Infect. 1:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zierski M, Zachara A. 1970. Late results in re-treatment of patients with pulmonary tuberculosis. Tubercle 51:172–177 [DOI] [PubMed] [Google Scholar]
- 44. Zou G. 2004. A modified Poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159:702–706 [DOI] [PubMed] [Google Scholar]