Abstract
We report a case of histologically confirmed biliary hamartomatosis with calcifications studied by CT.
The appearance of biliary hamartomatosis on ultrasonography, CT and MRI is well established. Numerous publications have reported the behaviour of these lesions in dynamic MRI studies. However, to our knowledge, calcifications in biliary hamartomatosis have yet to be reported. Awareness of this rare condition may help radiologists to make an accurate diagnosis.
Case report
A 56-year-old man underwent CT for prostate cancer staging in February 2007. He had a history of smoking, had been correctly treated for tuberculosis 8 years previously and had Type II diabetes with retinopathy and severe arteriosclerotic complications, including chronic renal failure, ischaemic cerebrovascular accidents, ischaemic heart disease and distal amputations. At unenhanced CT, the size and shape of the liver were normal but there were numerous punctiform calcifications, predominantly in the right hepatic lobe (Figure 1). No changes in these calcifications were observed in follow-up CT examinations. In April 2008, the patient died of severe sepsis from Escherichia coli and Candida after surgical amputation. The autopsy confirmed that the cause of death was acute myocardial infarction and revealed the cause of the tiny calcifications in the liver.
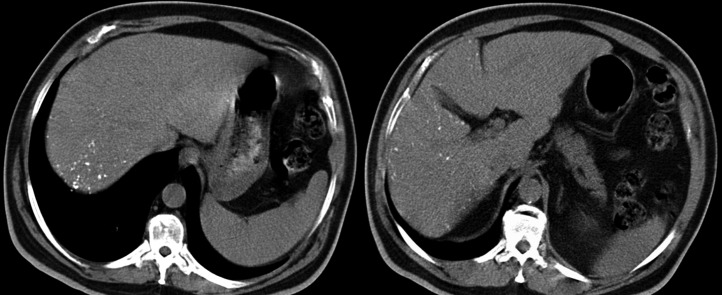
Figure 1.
Unenhanced abdominal CT with axial slices of the liver shows multiple punctiform calcifications of variable size with a clear predominance in the right lobe.
Macroscopic examination of the liver showed multiple white-grey nodules measuring 0.2–0.8 cm in diameter dispersed throughout the surface of both liver lobes (Figure 2). Microscopic examination showed multiple nodules composed of multiple bile ducts (some of which were small, irregular and/or dilated) enveloped in fibrous-hyalinised stroma (Figure 3). The lumina of these ducts were lined with simple or columnar cuboidal epithelium; a few had columnar cells with oval nuclei and mucous secretions which were positive after periodic acid–Schiff staining. Masson's trichrome stain for Type I collagen fibres revealed periductal fibrous stroma and some fibrous bridges between nodules. Although the growth pattern of the individual glands was irregular in places, the lesions had well-defined margins in the least magnified images. No cellular atypia was seen. Some ducts contained bile and others showed irregularly shaped and variably sized amphophilic or basophilic concretions that were positive at Von Kossa staining, specific for calcium salts (Figure 4).
Figure 2.
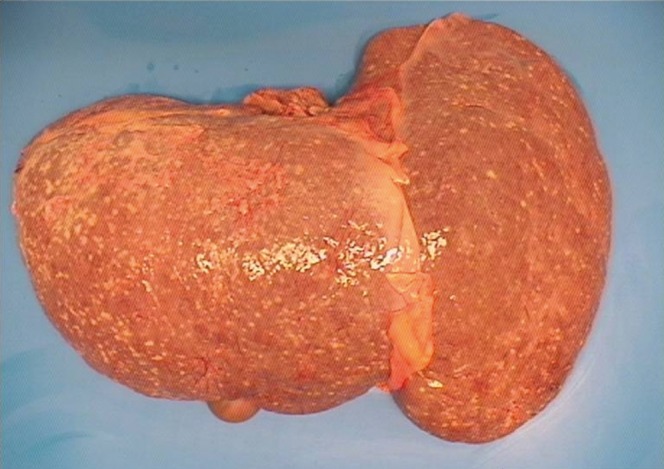
Gross histological image of the liver shows multiple white-grey nodules.
Figure 3.
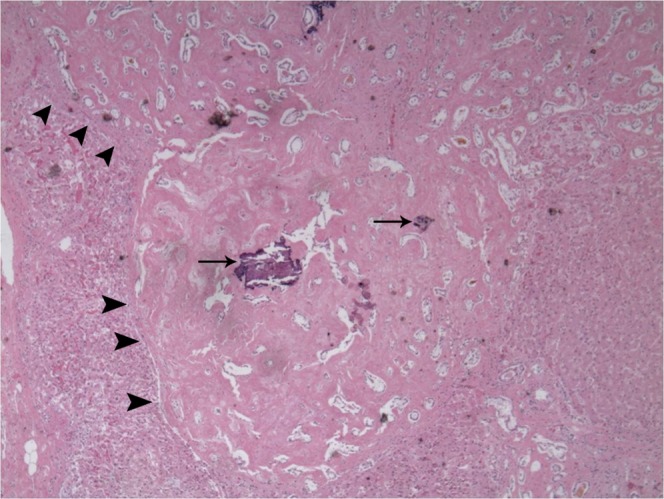
Haematoxylin and eosin stain of a biliary hamartoma. Nodular areas (arrowheads) with dense hyalinised fibrous stroma and hamartomatous proliferation with irregular ectatic lumens lined with biliary epithelium (original magnification×40). Note the multiple dystrophic calcifications (arrows).
Figure 4.
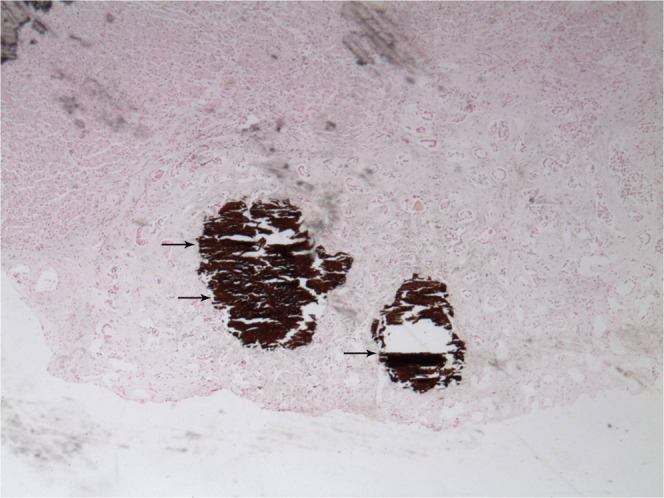
Homogeneous positivity of the calcium deposits after von Kossa staining (arrows), indicating with even more specificity the presence of calcium salts (original magnification ×40).
In summary, histological examination of the liver found multiple biliary hamartomas, many of which had intraluminal dystrophic calcifications.
Discussion
Biliary hamartomas are rare, benign malformations of the intrahepatic bile ducts [1]; they were first described by von Meyenburg in 1955 [2] and are also known as von Meyenburg complexes [3,4], microhamartomas, adenomas of the small bile ducts, cholangioadenomas, intracapsular aberrant bile ducts, fibroadenomatosis and liver hamartomatosis [5]. Biliary hamartomas are considered part of the spectrum of fibropolycystic liver disease arising from abnormal embryological development of the ductal plate [3,6] (the cylindrical layer of cells that surrounds the portal branch and then gives rise to the bile ducts), which also includes congenital liver fibrosis, Caroli's disease, mesenchymal hamartomas, dominant autosomal polycystic disease and choledochal cysts. Although hamartomas are considered benign lesions, a rare association with cholangiocarcinoma that follows the sequence hamartoma–hyperplasic lesionor adenomatous–cholangiocarcinoma has been reported, especially in patients with fibropolycystic disease [7].
Clinically, biliary hamartomas are usually asymptomatic and discovered incidentally at imaging, laparotomy or autopsy [3,4]. Tohme-Noun et al [1] found elevated serum levels of gamma-glutamyltranspeptidase (GGT) that could not be explained by another disease in 4 out of 11 patients with histologically proven hamartomatosis. The prevalence of biliary hamartomas has been estimated at 5.6% in adults and 0.9% in children [1,2]; the rate increases with age and chronic liver disease [7]. Biliary hamartomas can be confused with metastases, microabscesses, cysts, biliary adenomas, dilated bile ducts [4], cirrhosis [8,9], granulomatous hepatitis [8] and cystadenocarcinoma [10].
On macroscopic histological examination, biliary hamartomas are seen as white-grey nodular lesions [3,8] in a subcapsular location [1] or dispersed throughout the liver parenchyma [3]; they usually measure <5 mm in diameter [4,8] although they can also coalesce into larger cystic lesions [4]. Microscopic examination reveals that they are composed of a variable number of disorganised irregular tiny bile ducts immersed in fibrocollagenous stroma that may be hyalinised [11]. The ductal structures have a variable degree of dilation, can contain viscous bile [2] and do not communicate with the normal terminal bile ducts [5]. When the ducts dilate, they may coalesce in cystic cavities with intracavitary persistence of surrounding connective tissue forming endocystic polypoid projections [1]. Cholesterol crystals are often found in association with the dilated tiny bile ducts [9].
On ultrasonography, the presence of multiple biliary hamartomas gives the liver a heterogeneous granular echotexture similar to that seen in cirrhosis, with multiple small hyperechoic or hypoechoic spots with comet-tail artefacts [9,11]. In the Doppler study, a “twinkling” artefact, generated secondary to multiple reverberations from the cholesterol crystals inside the cystic ductal dilations, may be seen [9].
MRI is considered the best non-invasive technique for diagnosing biliary hamartomatosis [1]. Hamartomas are seen as nodular structures that are hypointense with respect to the adjacent parenchyma in T1 weighted sequences and very hyperintense in T2 weighted sequences; unlike in Caroli's disease, these structures show no communication with the bile tract in MRI cholangiography [3,10]. The signal intensity of the hamartomas increases characteristically with increases in echo time until it reaches that of cerebrospinal fluid [1]. Although enhancement is not usually seen in dynamic studies, some authors report homogeneous enhancement or peripheral ring enhancement owing to compression of the liver parenchyma and the inflammatory cells that surround the lesion [1,3,6]. Tohme-Noun et al [1] reported the presence of intracystic mural nodules that were isointense in T1 weighted sequences and had intermediate signal intensity in T2 weighted sequences and early, prolonged enhancement after the administration of intravenous contrast agents.
Unenhanced CT shows multiple hypodense liver nodules in both lobes; these nodules resemble cysts, although they usually measure <1.5 cm in diameter [3] and have more irregular margins [3,6]. In most cases, no enhancement is seen after the administration of iodinated contrast material [3,6].
In our case, microscopic examination revealed calcifications inside the hamartomas; these were also visible on CT as punctiform calcifications in the periphery of the liver and in the right lobe. We were unable to find any mention of calcifications in biliary hamartomatosis in the English-language literature. It may be that calcifications in hamartomas are extremely rare or that their non-specific appearance on CT results in them being confused with those of other origins (for example calcified granulomas).
Conclusion
It is important for radiologists to be aware that biliary hamartomas can calcify so that they do not attribute these calcifications to other causes.
Acknowledgment
The authors thank John Giba for help in translating the manuscript.
Reference
- 1.Tohme-Noun C, Cazals D, Noun R, Menassa L, Valla D, Vilgrain V. Multiple biliary hamartomas: magnetic resonance features with histopathologic correlation. Eur Radiol 2008;18:493–9 [DOI] [PubMed] [Google Scholar]
- 2.Song JS, Lee YJ, Kim KW, Huh J, Jang SJ, Yu E. Cholangiocarcinoma arising in von Meyenburg complexes: report of four cases. Pathol Int 2008;58:503–12 [DOI] [PubMed] [Google Scholar]
- 3.Mortele KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics 2001;21:895–910 [DOI] [PubMed] [Google Scholar]
- 4.Horton KM, Bluemke DA, Hruban RH, Soyer P, Fishman EK. CT and MR imaging of benign hepatic and biliary tumors. Radiographics 1999;19:431–51 [DOI] [PubMed] [Google Scholar]
- 5.Semelka RC, Hussain SM, Marcos HB, Woosley JT. Biliary hamartomas: solitary and multiple lesions shown on current MR techniques including gadolinium enhancement. J Magn Reson Imaging 1999;10:196–201 [DOI] [PubMed] [Google Scholar]
- 6.Mortele B, Mortele K, Seynaeve P, Vandevelde D, Kunnen M, Ros PR. Hepatic bile duct hamartomas (von Meyenburg complexes): MR and MR cholangiography findings. J Comput Assist Tomogr 2002;26:438–43 [DOI] [PubMed] [Google Scholar]
- 7.Jain D, Ahrens W, Finkelstein S. Molecular evidence for the neoplastic potential of hepatic von-Meyenburg complexes. Appl Immunohistochem Mol Morphol 2010;18:166–71 [DOI] [PubMed] [Google Scholar]
- 8.Mas A, Almirall J, Rodriguez A, Bella R, Corcuera A, Donoso L. Microhamartomatosis of the liver associated with autosomal dominant polycystic kidney disease: CT and US appearance. J Comput Assist Tomogr 1994;18:972–4 [DOI] [PubMed] [Google Scholar]
- 9.Jeon SJ, Yoon SE. Color Doppler twinkling artifact in hepatic bile duct hamartomas (von Meyenburg complexes). J Ultrasound Med 2006;25:399–402 [DOI] [PubMed] [Google Scholar]
- 10.Del Poggio P, Buonocore M. Cystic tumors of the liver: a practical approach. World J Gastroenterol 2008;14:3616–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luo TY, Itai Y, Eguchi N, Kurosaki Y, Onaya H, Ahmadi Y, et al. Von Meyenburg complexes of the liver: imaging findings. J Comput Assist Tomogr 1998;22:372–8 [DOI] [PubMed] [Google Scholar]