Abstract
BACKGROUND
Although many studies have indicated that psychosocial factors contribute to hypertension, and that early childhood adversity is associated with long-term adverse mental and physical health sequelae, the association between early adversity and later hypertension is not well studied.
METHOD
Data from 10 countries participating in the World Health Organization (WHO) World Mental Health (WHM) Surveys (N = 18,630) were analyzed to assess the relationship between childhood adversity and adult-onset hypertension, as ascertained by self-report. The potentially mediating effect of early-onset depression-anxiety disorders, as assessed by the WHM Survey version of the International Diagnostic Interview (WMH-CIDI), on the relationship between early adversity and hypertension was also examined.
RESULTS
Two or more early childhood adversities, as well as early-onset depression-anxiety, were significantly associated with hypertension. A range of specific childhood adversities, as well as early-onset social phobia and panic/agoraphobia, were significantly associated with hypertension. In multivariate analyses, the presence of 3 or more childhood adversities was associated with hypertension, even when early-onset depression-anxiety or current depression-anxiety was included in the model.
CONCLUSIONS
Although caution is required in the interpretation of self-report data on adult-onset hypertension, the results of this study further strengthen the evidence base regarding the role of psychosocial factors in the pathogenesis of hypertension.
INTRODUCTION
Research has found that psychosocial factors, in particular depression, anxiety, and anger, contribute to the etiology of hypertension.1,2 Psychological trauma has been hypothesized to be an especially important contributor to hypertension.3 Such a relationship would be consistent with research that has found chronic adverse psychobiological sequelae of early childhood adversity,4,5 and with an increasingly sophisticated and integrative approach to understanding mental-physical comorbidity.6
Nevertheless, studies on psychosocial contributors to hypertension have important limitations.1,2 Most of these studies have been conducted in only a few countries. The relationship between childhood adversity and hypertension has received relatively little attention, with sparse data available on the contribution of different types of childhood adversity. Further, despite evidence that childhood adversity is a risk factor for depression and anxiety disorders,7 there has been no research assessing whether the association of depression and anxiety with subsequent hypertension might be explained by exposure to childhood adversity.
Using data from cross-national population surveys, this paper reports on the relationships between childhood adversity, early-onset depression-anxiety disorders, and adult-onset hypertension. Based on prior research, we hypothesized that exposure to significant childhood adversity is associated with adult-onset hypertension. To assess the potential mediation of early-onset depression-anxiety disorders on the association between childhood adversity and hypertension, we evaluated (1) whether such early-onset conditions are associated with an increased risk of adult-onset hypertension, and (2) whether childhood adversity and early-onset depression-anxiety disorders predict adult-onset hypertension independently of each other.
METHODS
Samples
Ten surveys were carried out in the Americas (Colombia, Mexico, and the United States), Europe (Belgium, France, Germany, Italy, the Netherlands, and Spain), and Asia (Japan). All surveys were based on multistage, clustered, area probability household samples. All interviews were carried out face-to-face by trained lay interviewers. Sample sizes ranged from 2372 (Netherlands) to 9282 (United States). Response rates ranged from 45.9% (France) to 87.7% (Colombia), with an average response rate of 66.7%.
Internal subsampling was used to reduce respondent burden and average interview time and cost by dividing the interview into 2 parts. Part 1 included the core diagnostic assessment of mental disorders. Part 2 included additional information relevant to a wide range of survey aims, including assessment of chronic physical conditions. All respondents completed part 1. All part 1 respondents who met criteria for any mental disorder as well as a probability sample of other respondents were administered part 2. Part 2 respondents were weighted by the inverse of their probability of selection for part 2 of the interview to adjust for differential sampling. Analyses in this article were based on the weighted part 2 subsample (n = 18,303). Additional weights were used to adjust for differential probabilities of selection within households, to adjust for nonresponse, and to match the samples to population sociodemographic distributions.
Training and field procedures
The central World Mental Health (WMH) staff trained bilingual supervisors in each country. The World Health Organization (WHO) translation protocol was used to translate instruments and training materials. Some surveys were conducted in bilingual form (Belgium). Other surveys were conducted exclusively in the country’s official language. Persons who could not speak these languages were excluded. Quality control protocols, described in more detail elsewhere,8 were standardized across countries to check on interviewer accuracy and to specify data cleaning and coding procedures. The institutional review board of the organization that coordinated the survey in each country approved and monitored compliance with procedures for obtaining informed consent and protecting human subjects.
Mental disorder status
All surveys used the WMH Survey version of the WHO Composite International Diagnostic Interview (WMH-CIDI, now CIDI 3.0),8 a fully structured diagnostic interview, to assess disorders. Clinical calibration studies have supported the reliability and validity of both the original CIDI9 and the WMH-CIDI.10 Disorders were assessed using the definitions and criteria of the DSM-IV.11 CIDI organic exclusion rules were imposed (the diagnosis was not made if the respondent indicated that the episode of depressive or anxiety symptoms was due to physical illness or injury or the use of medication, drugs, or alcohol).
This article includes anxiety disorders (generalized anxiety disorder, panic disorder and/or agoraphobia, posttraumatic stress disorder, and social phobia) and depressive disorders (major depressive disorder). Anxiety and depressive disorders were aggregated into a single category, on the basis of prior WMH Survey findings that both anxiety disorders and depressive disorders have similar relationships with a wide range of chronic physical conditions.12 For each disorder present at any time in a respondent’s lifetime, the age of onset was determined using standard CIDI questions. Persons were classified as having an early-onset depression/anxiety disorder if the earliest age of onset for any lifetime disorder was less than 21 years of age. In analyses for each mental disorder singly, early onset was also defined as age of onset prior to age 21.
Hypertension
In a series of questions about chronic conditions adapted from the US Health Interview Survey, respondents were asked about the lifetime presence of select chronic conditions. Respondents were asked, “Did a doctor or other health professional ever tell you that you had any of the following illnesses…hypertension?” Respondents were also asked how old they were when the condition began. Only those reporting hypertension onset after the age of 20 were included in the current analyses.
Childhood adversity
The following types of childhood adversity were included in the present report: physical abuse; sexual abuse; neglect; parental death, parent divorce, other parental loss; parental mental disorder; parental substance use; parental criminal behavior; family violence; and family economic adversity. The aim was to assess the occurrence of childhood adversity within the context of the family rather than all possible childhood adversities. Thus, natural disasters or exposure to war were not assessed in this section. Those respondents who reported that the experience occurred before age 18 and who met the criteria specified for a given adversity (described below) were coded as having experienced childhood family adversity.
Physical abuse
Respondents were classified as having experienced physical abuse when they indicated that, when they were growing up, their father or mother (includes biological, step, or adoptive parents) slapped, hit, pushed, grabbed, shoved, or threw something at them, or that they were beaten as a child by the persons who raised them.
Sexual abuse
For sexual abuse, the following questions were asked:
“The next 2 questions are about sexual assault. The first is about rape. We define this as someone either having sexual intercourse with you or penetrating your body with a finger or object when you did not want them to, either by threatening you or using force, or when you were so young that you didn’t know what was happening. Did this ever happen to you?”
“Other than rape, were you ever sexually assaulted or molested?”
Sexual abuse was the only adversity for which information was not collected that would distinguish whether the perpetrator was a family member or someone else. However, previous research that used a similar measure but did allow such a distinction showed that a good indirect way to distinguish family vs nonfamily sexual abuse is to ask about the number of instances of victimization, with cases involving 1 or 2 instances typically perpetrated by a stranger and those involving 3 or more instances typically perpetrated by a family member.13 In the WMH surveys, therefore, respondents who reported that they had had any of these experiences 3 times or more were coded as having experienced sexual abuse (within the family context).
Neglect
For the assessment of neglect, 2 scales were created. These were based on responses to the neglect items:
“How often were you made to do chores that were too difficult or dangerous for someone your age?”
“How often were you left alone or unsupervised when you were too young to be alone?”
“How often did you go without things you need like clothes, shoes, or school supplies because your parents or caregivers spent the money on themselves?”
“How often did your parents or caregivers make you go hungry or not prepare regular meals?”
“How often did your parents or caregivers ignore or fail to get you medical treatment when you were sick or hurt?”
The serious neglect scale was the sum of the number of neglect items in which the respondent replied “often” or “sometimes,” plus 1 if the respondent rated either of his or her parents as having spent little or no effort in watching over them to ensure they had a good upbringing. The severe neglect scale is the sum of the number of neglect items where respondents replied “often” plus 1 if the respondent rated either of his or her parents as having spent no effort in watching over them to ensure they had a good upbringing. Both the serious and severe neglect scales ranged from 0 to 6. For the final definition of neglect, the respondent had to have a score of at least 1 on the severe neglect scale and at least 2 on the serious neglect scale. The coding of the neglect domain was determined empirically on the basis of frequency distributions to derive estimates in keeping with existing literature on the prevalence of these experiences in the general population.
Parental death, parental divorce, or other parental loss
Respondents were first asked whether they lived with both of their parents when they were brought up. If respondents replied in the negative, they were asked:
“Did your biological mother or father die, were they separated or divorced, or was there some other reason?”
According to their answers to these questions, respondents were classified as having experienced parental death (when they indicated that one or both parents had died), parental divorce (when they indicated that their parents had divorced), and other parental loss (when respondents replied that they had either been adopted, had gone to boarding school, had been in foster care, or had left home before age 16).
Parental mental disorder
Parental depression was assessed by the following diagnostic items:
“During the years you were growing up, did [woman/man who raised the respondent] ever have periods lasting 2 weeks or more where [she/ he] was sad or depressed most of the time?”
“During the time when [her/his] depression was at its worst, did [she/he] also have other symptoms like low energy, changes in sleep or appetite, and problems with concentration?”
A positive response to item 1 was followed up with a frequency question:
“Was this during all, most, some, or only a little of your childhood?”
Parental generalized anxiety disorder (GAD) was assessed as follows:
“During the time you were growing up, did [woman/man who raised the respondent] ever have periods of a month or more when [she/he] was constantly nervous, edgy, or anxious?” and
“During the time [her/his] nervousness was at its worst, did [she/he] also have other symptoms, like being restless, irritable, easily tired, and difficulty falling asleep?”
A positive response to GAD item 1 was followed up with a frequency question:
“Was this during all, most, some, or only a little of your childhood?”
Parental panic disorder was assessed by the following item:
“Did [woman/man who raised the respondent] ever complain about anxiety attacks where all of a sudden [she/he] felt frightened, anxious, or panicky?”
Respondents who replied positively to both diagnostic items for depression and who replied “all or most of the time” to the frequency item and who reported that their parents got professional help for depression or that depression interfered a lot with their parents’ lives or activities were coded as respondents with parental depression. A similar logic applied to characterizing respondents whose parents had GAD. Respondents who responded positively to the single parental panic disorder item were coded as having parents with panic disorder.
Parental substance disorder
Similarly, parental substance disorder was assessed with the following items:
(criterion a) “Did [woman/man who raised the respondent] ever have a problem with alcohol or drugs” and
(criterion b) “Did [she/he] have this problem during all, most, some, or only a little of your childhood?”
Respondents who replied positively on the first and “all” and “most” on the second item were then asked whether the problem interfered a lot with life or activities of the woman or man who raised the respondent (criterion c), or whether they had sought professional help for this problem (criterion d). Those respondents who replied affirmatively on criteria a and b, and on either c or d were coded as having had parents with a substance disorder.
Parental criminal behavior
Parental criminal behavior was assessed by the following questions:
“Was [woman/man who raised the respondent] ever involved in criminal activities like burglary or selling stolen property?” and
“Was [woman/man who raised the respondent] ever arrested or sent to prison?”
Respondents who replied positively on either question were classified as having experienced criminal behavior in the family.
Family violence
Respondents were coded as having experienced family violence when they indicated that they
“were often hit, shoved, pushed, grabbed, or slapped while growing up” or
“witnessed physical fights at home, like when your father beat up your mother?”
Family economic adversity
Respondents were coded positive for family economic adversity if there was a positive response to either of the 2 following items:
“During your childhood and adolescence, was there ever a period of 6 months or more when your family received money from a government assistance program like Welfare, Aid to Families with Dependent Children, General Assistance, or Temporary Assistance for Needy Families?” (This item was modified to be relevant to the welfare programs in each country where the survey was administered.) Or,
If there was no male head of the family and the female head did NOT work all or most of the time during respondent’s childhood; or if there was no female head of the family and the male head did NOT work all or most of respondent’s childhood, or if there was no female head and no male head of the family.
Statistical analysis
The association of childhood adversity and early-onset mental disorders with adult-onset asthma was studied with discrete-time survival analyses, using retrospective self-report of age of onset of hypertension (reported in whole years). The start of the period at risk for adult-onset hypertension was set at age 20.
Cox proportional hazards models were constructed to estimate risk of adult-onset hypertension as a function of number of childhood adversities and early-onset depression-anxiety disorder status while adjusting for potential confounders (sex and current age). Country was included in the analyses as a stratifying variable, which allows each country to have a unique hazard function. This was necessary because of large differences in prevalence rates of childhood adversity, mental disorders, and chronic physical disorders between countries, and to allow for the slight differences in measurement of childhood adversities between countries (ie, measurement of neglect and parental divorce).
In the Cox proportional hazards regression analyses, time to age of onset of hypertension from age 20 was the dependent variable. Persons who had not developed hypertension were censored at their current age. The associations are expressed as hazard ratios (HRs) measuring relative risk (RR). Childhood adversities were analyzed in 4 categories of number of adversities (none, 1, 2, ≥3), with no adversities as the reference group. Childhood adversity and early-onset mental disorders were included in the models both separately and simultaneously. We screened for interaction of childhood adversity and early-onset depression-anxiety, but the interaction was nonsignificant; therefore, only main effects are reported in this article. To account for the possibility of differential recall of childhood adversity among those with a current mood or anxiety disorder, we performed an additional analysis that adjusted for current (12-month) anxiety or mood disorder. We performed yet another analysis, including educational attainment, to assess whether any associations between the risk factors of primary interest (childhood adversity and early-onset depression/anxiety) were explained by differences in educational level.
The assumption of proportional hazards was assessed by inspecting log-minus-log plots of the survival functions. Standard errors were calculated for all HRs. The statistical significance level was set at .05 for a 2-sided test. The analyses were performed using the SURVIVAL procedure in SUDAAN statistical software.14 In all multivariate models, a complete-case approach was used, but the WMH survey used multiple imputation methods to impute missing values for the childhood adversities. The survival analyses employed sample weights to adjust for differences in probability of selection. Estimates were made using SUDAAN software to account for the complex sample design.
RESULTS
Characteristics of the sample are presented in TABLE 1, and prevalence of self-reported adult-onset hypertension, childhood adversity, and early-onset depression-anxiety disorders are presented in TABLE 2. Overall, 17.3% of the respondents reported hypertension, of whom almost half (48.6%) noted a history of childhood adversity, and about a fifth of whom (18.5%) were found to have early onset of depression-anxiety disorder. Prevalence of childhood adversity varied across countries, ranging from 30% in Spain to 65% in Colombia.
TABLE 1.
Characteristics of total and adult onset hypertension samples
| CHARACTERISTIC | TOTAL CROSS-NATIONAL SAMPLE (N = 18,600) | ADULT-ONSET HYPERTENSION (AGE ≥21) SAMPLE (N = 3215) | |
|---|---|---|---|
| Unweighted, N | Weighted, % | Weighted, % | |
| Age (21 to 98) | |||
| 21 to 44 | 9827 | 52.5 | 18.0 |
| ≥45 | 8803 | 47.5 | 82.0 |
| Female | 11,092 | 52.8 | 55.6 |
| Adult onset of hypertension (≥21 years) | 18,600 | 3215 | 17.3 |
| Country | |||
| Colombia | 2122 | 11.5 | 8.0 |
| Belgium | 989 | 5.3 | 4.6 |
| France | 1359 | 7.3 | 6.4 |
| Germany | 1273 | 6.9 | 7.9 |
| Italy | 1699 | 9.1 | 6.8 |
| Netherlands | 1052 | 5.6 | 5.2 |
| Spain | 2015 | 10.8 | 9.6 |
| Japan | 873 | 4.7 | 4.4 |
| Mexico | 2059 | 11.0 | 6.6 |
| United States | 5189 | 27.8 | 23.6 |
TABLE 2.
Early-onset depressive/anxiety disorders and childhood adversities in total and adult-onset hypertension samples
| CHARACTERISTIC | TOTAL CROSS-NATIONAL SAMPLE (N = 18,600) | ADULT-ONSET HYPERTENSION (AGE ≥21) SAMPLE (N = 3215) |
|---|---|---|
| Weighted, % | Weighted, % | |
| Early-onset (prior to age 21) mental disorders | ||
| Any depressive/anxiety disorder | 10.2 | 18.5 |
| Major depressive disorder | 4.5 | 9.0 |
| Generalized anxiety disorder | 1.3 | 2.5 |
| Social phobia | 4.8 | 8.3 |
| Posttraumatic stress disorder | 1.7 | 2.7 |
| Panic disorder/agoraphobia | 1.8 | 3.3 |
| Number of childhood adversities | ||
| 0 | 56.1 | 51.4 |
| 1 | 25.6 | 25.8 |
| 2 | 10.0 | 11.6 |
| ≥3 | 8.3 | 11.2 |
| Type of childhood adversity | ||
| Physical abuse | 9.6 | 12.9 |
| Sexual abuse | 2.6 | 3.9 |
| Neglect | 6.5 | 8.2 |
| Parent died | 12.8 | 12.7 |
| Parents divorced | 9.8 | 10.6 |
| Other loss of parent | 5.3 | 6.2 |
| Parental mental disorder | 7.2 | 10.0 |
| Parental substance use disorder | 5.0 | 6.5 |
| Violence in family | 9.4 | 11.9 |
| Parental criminal behavior | 3.3 | 4.4 |
| Family economic adversity | 5.8 | 6.3 |
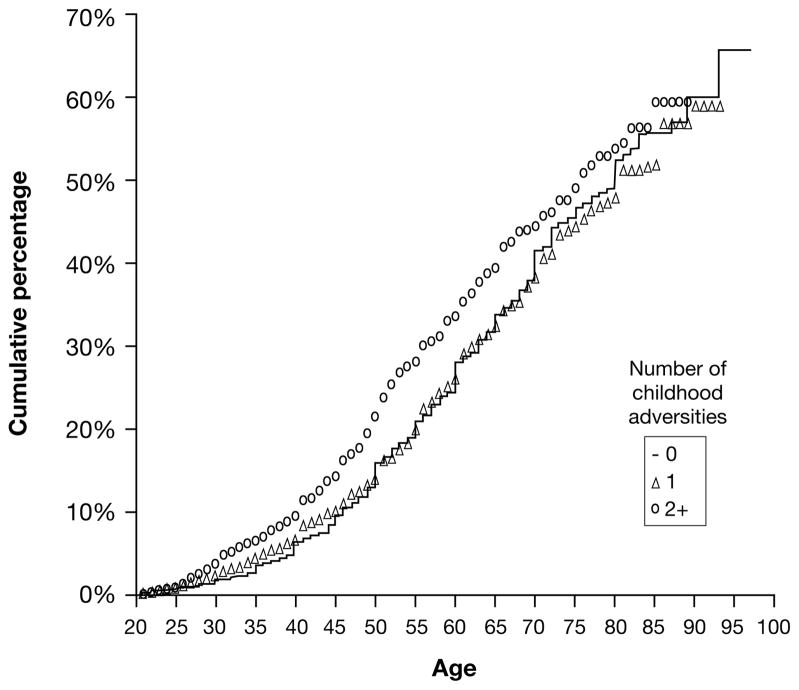
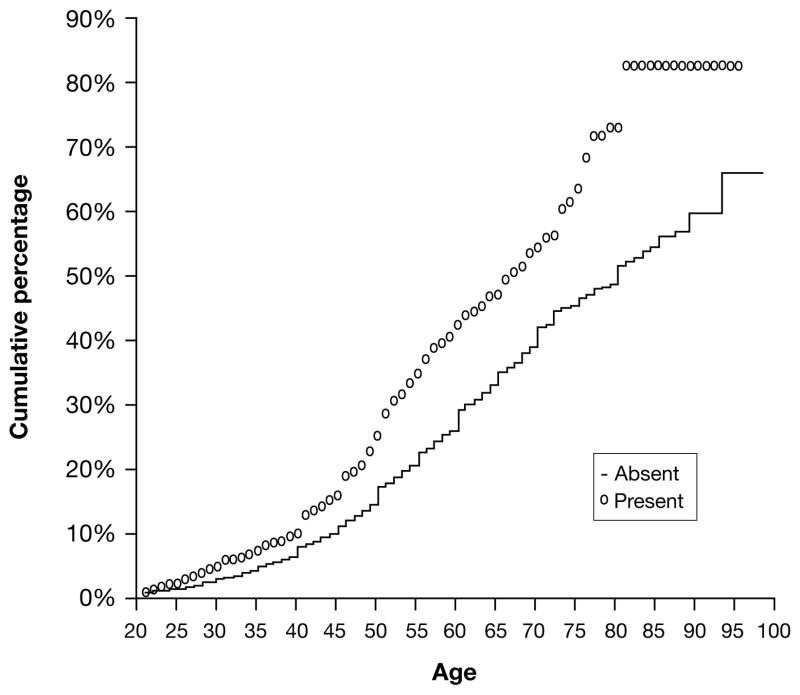
Kaplan-Meier curves for the cumulative percentage of hypertension by age for persons with 0, 1, or ≥2 childhood adversities (FIGURE 1) and for persons with vs without early-onset depression-anxiety disorders (FIGURE 2) were plotted; these curves indicate crude associations between hypertension and both childhood adversity and early-onset depression-anxiety disorders.
FIGURE 1.
Kaplan-Meier curve for the cumulative percentage of onset of hypertension by age for persons with 0, 1, or 2+ childhood adversities
FIGURE 2.
Kaplan-Meier curve for the cumulative percentage of hypertension onset by age for persons with vs without early-onset depression-anxiety disorders
TABLE 3 provides HRs for the relationship between childhood adversity, early-onset depression-anxiety disorder, and adult-onset hypertension. The unadjusted HR for adult-onset hypertension for persons with early-onset depression-anxiety (relative to those without) was 1.34 (P < .001). After adjusting for number of childhood adversities, this HR was essentially unchanged, at 1.29 (P < .001). Unadjusted HRs for number of childhood adversities (relative to persons with no childhood adversity) were 1.03 for persons with 1 adversity (P = ns), 1.19 for persons with 2 adversities (P < .05), and 1.28 for persons with 3 or more adversities (P < .01), prior to adjusting for early-onset depression-anxiety disorder status. After adjusting for depression-anxiety disorder status, the HRs for number of childhood adversities were somewhat reduced but remained significantly greater than 1.0 for persons with 3 or more adversities (P < .05), as shown in the second column of TABLE 2. Adjusting for current depression-anxiety disorder status rather than early-onset depression-anxiety disorder status changed the HRs for number of childhood adversities only slightly, suggesting that effects of current mood on recall of childhood adversities or hypertension status does not explain their association.
TABLE 3.
Association between early-onset depression-anxiety disorders, childhood adversities, and hypertension
| RISK FACTOR | HAZARD RATIOS (95% CONFIDENCE INTERVAL) | ||
|---|---|---|---|
| Main effect for hypertension | Adjusted for early-onset depression/anxiety | Adjusted for current depression/anxiety | |
| Depression/anxiety onset before age 21 | 1.34 (1.20 to 1.48; P < .001) | ||
| 1 childhood adversity | 1.03 (0.92 to 1.16; ns) | 1.03 (0.91 to 1.15; ns) | 1.02 (0.91 to 1.15, ns) |
| 2 childhood adversities | 1.19 (1.01 to 1.41; P < .05) | 1.17 (1.00 to 1.38; ns) | 1.17 (1.00 to 1.38; P < .01) |
| ≥3 childhood adversities | 1.28 (1.07 to 1.53; P < .01) | 1.22 (1.02 to 1.46; P < .05) | 1.21 (1.01 to 1.44; P < .001) |
HRs for each of the specific childhood adversities, adjusted for gender, age, and country are shown in TABLE 4. Of the 11 childhood adversities ascertained, 6 were significantly associated with adult-onset hypertension (with odds ratios [ORs] ranging from 1.17 to 1.53). Among the 5 specific DSM-IV mental disorders assessed, early-onset social phobia and panic disorder/agoraphobia were significantly associated with increased risk of adult-onset hypertension, whereas early-onset major depressive disorder, generalized anxiety disorder, and posttraumatic stress disorder were not (TABLE 4).
TABLE 4.
Effect of early-onset (prior to age 21) depressive/anxiety disorders and specific childhood adversities on adult- onset of hypertension (21 years and over)
| Early-onset (prior to age 21) mental disorder | Hazard ratio (95% CI) for adult-onset hypertension (adjusted for age, sex, country) |
|---|---|
| Major depressive disorder | 1.15 (0.96 to 1.39; ns) |
| Generalized anxiety disorder | 1.16 (0.91 to 1.47; ns) |
| Social phobia | 1.36 (1.19 to 1.57; P < .001) |
| Posttraumatic stress disorder | 1.15 (0.89 to 1.48; ns) |
| Panic disorder/agoraphobia | 1.53 (1.19 to 1.97; P < .001) |
| Childhood adversity | |
| Physical abuse | 1.23 (1.04 to 1.46; P < .05) |
| Sexual abuse | 1.14 (0.84 to 1.54; ns) |
| Neglect | 1.10 (0.90 to 1.34; ns) |
| Parent died | 1.02 (0.89 to 1.18; ns) |
| Parents divorced | 0.96 (0.79 to 1.16; ns) |
| Other loss of parent | 1.26 (1.05 to 1.52; P < .05) |
| Parental mental disorder | 1.29 (1.11 to 1.50; P < .01) |
| Parental substance use disorder | 1.30 (1.07 to 1.56; P < .01) |
| Violence in family | 1.17 (1.02 to 1.34; P < .05) |
| Criminal behavior in family | 1.33 (1.09 to 1.62; P < .01) |
| Family economic adversity | 1.03 (0.83 to 1.27; ns) |
CI: confidence interval.
DISCUSSION
It is important to emphasize several limitations of this study. Blood pressure levels can be directly measured in epidemiological studies, but the current study relied on self-report and provided only a categorical measure of hypertension. At the same time, epidemiological studies of hypertension are rarely able to obtain detailed data on mental illness and psychological stressors. Partial reassurance is obtained from data that self-reported hypertension is moderately associated with objective data on hypertensive status.15,16 Nevertheless, although estimates of sensitivity of self-report of hypertension range from 64% to 91% in several Western countries, it may be lower in other locations.17 A second crucial limitation is that the focus of this study was childhood family adversity rather than a range of other possible early traumas, and the study relied on retrospective reports of childhood stressors. False-negative childhood reports may lead to underestimation of associated effects. Some reassurance is obtained from a recent review of the validity of retrospective report of childhood adversities; this review found that although false-negative reports are common, false-positive reports are rare, and concluded that retrospective case-control studies of major, easily defined adversities are potentially valid.18 Finally, retrospective reports of age of onset of both hypertension and mental disorders are subject to bias.
Given these limitations, we view the results reported in this article as exploratory findings that would need to be replicated with more rigorous ascertainment of hypertension and hypertension onset, along with prospective studies of subjects exposed to early adversity. The main findings of the current study were that (1) the presence of 2 or more early childhood adversities was significantly associated with adult-onset hypertension, (2) early-onset depression-anxiety disorder was also significantly associated with increased risk of hypertension, and (3) in multivariate analyses, 3 or more childhood adversities, as well as early-onset depression-anxiety disorder, continued to be significantly associated with increased risk of hypertension.
The observed HRs suggest a “dose-response” relationship between early childhood adversity and subsequent hypertension. The extent and number of childhood adversities may be more important than the specific type of adversity experienced. There was no increased risk of adult-onset hypertension among persons who reported only 1 childhood adversity, and the HRs for the relationship between early adversity and subsequent hypertension were relatively low. However, given that 22.8% of the respondents with adult-onset hypertension experienced 2 or more childhood adversities, the potential impact of these exposures on hypertension risk has potential importance.
Although childhood adversity is associated with an increased risk of early-onset depression-anxiety disorders, controlling for number of childhood adversities did not explain the association of early depression-anxiety disorders with adult-onset hypertension. Effect sizes for the association of psychosocial factors and hypertension have been modest to date,2 and the findings here underscore previous recommendations that genetic, early environmental, and later environmental effects on hypertension and other cardiovascular conditions all require further delineation.19,20 Effects sizes for behavioral treatments for hypertension are quite variable,21 and this parallel area of research requires additional attention.
Additional work is needed to understand the specific psychobiological mechanisms that mediate the relationships between childhood adversity, early-onset depression and anxiety disorders, and subsequent adult-onset hypertension. Although the current data do not directly address these mechanisms, it is relevant to note the research documenting how both early trauma and depression-anxiety disorders alter the autonomic system, potentially contributing to increased allostatic load.7,22–24 In addition to chronic sympathetic nervous system dysregulation, monoamine abnormalities and endothelial dysfunction might play a role.2
In conclusion, the WMH Survey provides a unique opportunity to assess the relationship between childhood adversity, early-onset depression-anxiety disorders, and adult-onset hypertension in a large, multinational sample. The data are consistent with prior literature on the role of psychosocial factors in the pathogenesis of hypertension and call attention to the potential role of both early childhood adversity and early-onset depression-anxiety disorders as risk factors for hypertension. These exploratory results suggest the need for prospective studies assessing the independent and joint effects of childhood adversity and early-onset emotional disorders in influencing risk of developing hypertension as an adult.
Acknowledgments
The surveys included in this report were carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the US National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01-DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, the Eli Lilly & Company Foundation, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. A complete list of WMH publications can be found at www.hcp.med.harvard.edu/wmh.
The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection.
The ESEMeD project is funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, Instituto de Salud Carlos III (CIBER CB06/02/0046, RETICS RD06/0011 REM-TAP), and other local agencies and by an unrestricted educational grant from GlaxoSmithKline.
The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013) from the Japan Ministry of Health, Labour, and Welfare.
The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONA-CyT-G30544-H), with supplemental support from the Pan American Health Organization (PAHO).
The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust.
Footnotes
DISCLOSURES: Dr. Stein has received research grants and/or consultancy honoraria from AstraZeneca, Eli Lilly, GlaxoSmithKline, Jazz Pharmaceuticals, Johnson & Johnson, Lundbeck, Orion, Pfizer Inc, Pharmacia, Roche, Servier, Solvay, Sumitomo, Takeda, Tikvah, and Wyeth.
Dr. Kessler has been a consultant for GlaxoSmith-Kline Inc., Kaiser Permanente, Pfizer Inc, sanofi-aventis, Shire Pharmaceuticals, and Wyeth-Ayerst; has served on advisory boards for Eli Lilly & Company and Wyeth-Ayerst; and has had research support for his epidemiological studies from Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Johnson & Johnson Pharmaceuticals, Ortho-McNeil Pharmaceuticals Inc., Pfizer Inc, and sanofi-aventis.
Dr. Haro Abad receives grant/research support from the Spanish government, the European Commission, Eli Lilly and Company, Lundbeck, and AstraZeneca and is a consultant to and speaker for Eli Lilly and Company and AstraZeneca.
Drs. Scott, Aguilar-Gaxiola, Alonso, Angermeyer, Demytteneare, de Girolamo, Iwata, Posada-Villa, Kovess, Lara, Ormel, and Von Korff report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Contributor Information
Dan J. Stein, Department of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa.
Kate Scott, Department of Psychological Medicine, Wellington School of Medicine and Health Sciences, Otago University, Wellington, New Zealand.
Josep M. Haro Abad, Sant Joan de Déu-SSM, Fundació Sant Joan de Déu, Sant Boi de Llobregat, Barcelona, Spain.
Sergio Aguilar-Gaxiola, Center for Reducing Health Disparities, Sacramento, CA, USA.
Jordi Alonso, Health Services Research Unit, Institut Municipal d’Investigació Mèdica (IMIM-Hospital del Mar), CIBER en Epidemiología y Salud Pública (CIBERESP), Barcelona, Spain.
Matthias Angermeyer, Center for Public Mental Health, Gösing, Austria.
Koen Demytteneare, Department of Neurosciences and Psychiatry, University Hospitals Gasthuisberg, Leuven, Belgium.
Giovanni de Girolamo, IRCCS Centro S. Giovanni di Dio-Fatebenefratelli, Brescia, Italy.
Noboru Iwata, Department of Clinical Psychology, Hiroshima International University, Hiroshima, Japan.
José Posada-Villa, Medico Psiquiatra, U. Javerina, Centro Medico de la Sabana, Bogota, Colombia.
Viviane Kovess, Fondation MGEN pour la Santé Publique, Paris, France.
Carmen Lara, National Institute of Psychiatry, Puebla, Mexico.
Johan Ormel, Department of Psychiatry, University Medical Center, Groningen, The Netherlands.
Ronald C. Kessler, Department of Health Care Policy, Harvard University, Boston, MA, USA.
Michael Von Korff, Group Health Center for Health Studies, Seattle, WA, USA.
References
- 1.Kaplan MS, Nunes A. The psychosocial determinants of hypertension. Nutr Metab Cardiovasc Dis. 2003;13:52–59. doi: 10.1016/s0939-4753(03)80168-0. [DOI] [PubMed] [Google Scholar]
- 2.Rutledge T, Hogan BE. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosom Med. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 3.Mann SJ, Delon M. Improved hypertension control after disclosure of decades-old trauma. Psychosom Med. 1995;57:501–505. doi: 10.1097/00006842-199509000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Felitti VJ, Anda RF, Nordernberg D, et al. Relationship of child abuse to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prevent Med. 1998;14:245–248. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 5.Gluckman PD, Hanson MA. Living with the past: evolution, development, and patterns of disease. Science. 2004;305:1733–1736. doi: 10.1126/science.1095292. [DOI] [PubMed] [Google Scholar]
- 6.Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 10.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 12.Scott KM, Bruffaerts R, Tsang A, et al. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007;103:113–120. doi: 10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SUDAAN: Software for the statistical analysis of correlated data [program] Research Triangle Park, NC: Research Triangle Institute; 1999. [Google Scholar]
- 15.Alonso A, Beunza JJ, Delgado-Rodriguez M, et al. Validation of self reported diagnosis of hypertension in a cohort of university graduates in Spain. BMD Public Health. 2005;5:94. doi: 10.1186/1471-2458-5-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tormo MJ, Navarro C, Chirlaque MD, et al. Validation of self diagnosis of high blood pressure in a sample of the Spanish EPIC cohort: overall agreement and predictive values. J Epidemiol Community Health. 2000;54:221–226. doi: 10.1136/jech.54.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldman N, Lin IF, Weinstein M, et al. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol. 2003;56:148–154. doi: 10.1016/s0895-4356(02)00580-2. [DOI] [PubMed] [Google Scholar]
- 18.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 19.Eisen SA, Neuman R, Goldberg J, et al. Contribution of emotionally traumatic events and inheritance to the report of current physical health problems in 4042 Vietnam era veteran twin pairs. Psychosom Med. 1998;60:533–539. doi: 10.1097/00006842-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110:1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 21.Linden W, Moseley JV. The efficacy of behavioral treatments for hypertension. Appl Psychophysiol Biofeedback. 2006;31:51–63. doi: 10.1007/s10484-006-9004-8. [DOI] [PubMed] [Google Scholar]
- 22.Grippo AJ, Lamb DG, Carter CS, et al. Social isolation disrupts autonomic regulation of the heart and influences negative affective behaviors. Biol Psychiatry. 2007;62:1162–1170. doi: 10.1016/j.biopsych.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bedi US, Arora R. Cardiovascular manifestations of posttraumatic stress disorder. J Natl Med Assoc. 2007;99:642–649. [PMC free article] [PubMed] [Google Scholar]
- 24.Evans GW, Kim P, Ting AH, et al. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol. 2007;43:341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]