Abstract
The aim of this study was to determine whether there is superior diagnostic accuracy for the detection and exclusion of bronchiectasis using 16-slice CT of the chest (1 mm) compared with conventional high-resolution CT (HRCT) of the chest (10 mm). A prospective study was carried out in patients who were referred for chest CT by a chest physician for the investigation of bronchiectasis over a 1-year period. All scans were performed using a 16-slice CT scanner. In addition to contiguous 1 mm slices, conventional HRCT images (1 mm slice every 10 mm) were prepared. Both datasets were dual read. There were 53 patients with a median age of 62 years (range, 51.5–71.5 years), comprising 14 males and 39 females. 10 of 53 scans had no bronchiectasis in either dataset. 36 patients had bronchiectasis diagnosed on both HRCT and 1 mm scans. Two patients had tubular bronchiectasis on the HRCT scans, which was not confirmed on the 1 mm scans. Five patients had confirmed tubular bronchiectasis on the 1 mm scans, which was not identified on HRCT scans. 40 extra lobes demonstrated bronchiectasis on the 1 mm vs the HRCT scans; of these, half were labelled as definite bronchiectasis on the 1 mm scan. There was a 32% increased confidence with the 1 mm scans compared with conventional HRCT of the chest in the diagnosis of bronchiectasis (p < 0.001). In conclusion, there is improved diagnostic accuracy and confidence for diagnosis and exclusion of bronchiectasis using 16-slice chest CT (1 mm cuts) compared with conventional HRCT of the chest.
Bronchiectasis is a chronic disabling lung disease affecting between 1 in 1000 and 1 in 5000 of the general population. Pathologically, patients have irreversibly dilated and damaged bronchi. This leads to patients having a daily productive cough and recurrent chest infections.
High-resolution computed tomography (HRCT) of the chest is the gold standard for the diagnosis of bronchiectasis. For diagnosis, patients should have bronchial dilatation at least greater than the associated arterial vessel [1–5]. There may be associated bronchial wall thickening and mucus plugging. The extent of bronchiectasis is determined by the number of lobes involved and the severity of bronchiectasis, varying from mild tubular bronchiectasis to severe cystic bronchiectasis. There has been shown to be good interobserver agreement for the detection and assessment of the severity of bronchiectasis using HRCT [6], with good pathological correlation [7].
The aim of this study was to assess whether there is any difference in determining the extent and severity of bronchiectasis, and also if there is an improvement in the degree of confidence in diagnosis, using 16-slice CT of the chest using 1 mm contiguous slices compared with conventional HRCT using 1 mm slices every 10 mm.
Methods and materials
A prospective study was carried out over a one-year period in patients who were referred for chest CT by a chest physician for the investigation of bronchiectasis. The CT scans were all performed using a 16-slice CT scanner (Toshiba Aquilion scanner; Toshiba Medical Systems, Tokyo, Japan). Two sets of images were formed and saved individually onto discs. These were contiguous 1 mm slices (1 mm set) and 1 mm slices every 10 mm, analogous to conventional HRCT (10 mm set).
Each disc was interpreted randomly by two radiologists who have an interest in chest radiology, and a consensus reached. If there was no initial agreement in interpretation, then a third radiologist was used to help form a consensus. We used lung windows with a width of 1500 and depth of −750. Observers were blinded to the corresponding clinical information or report.
The CT scans were scored using six lobes: right upper lobe, right middle lobe, right lower lobe, left upper lobe, left lower lobe and the lingula, which was counted as a separate lobe in this study. They were graded as 0 for no bronchiectasis, 1 for tubular bronchiectasis, 2 for varicose bronchiectasis and 3 for cystic bronchiectasis, with one extra mark per lobe if central bronchiectasis was present. The score per scan could range from 0 (no bronchiectasis) to 24 (most severe case of bronchiectasis). When more than one type of bronchiectasis was present, the more severe type was recorded. The degree of confidence in the diagnosis of bronchiectasis was also recorded per lobe as “possible”, “probable” or “definite”. By assigning a value of 0 for possible bronchiectasis, 1 for probable bronchiectasis and 2 for either definite absence or presence of bronchiectasis, a confidence rating could be calculated.
Statistical analysis
The data were analysed using SPSS version 13 (SPSS Inc, Chicago, IL). The data are presented as the median (interquartile range). A Wilcoxon paired test was used to compare the two groups. Fisher's exact test was used to compare confidence ratings. A two tailed p-value <0.05 was considered statistically significant.
Results
A total of 53 patients were included. Their median age was 62 years (range, 51.5–71.5 years). 14 were male and 39 were female.
Concordance between HRCT (10 mm) and 1 mm scans — per patient
The concordance between scans is shown in Table 1. The 1 mm dataset therefore upgraded the diagnosis of bronchiectasis in 5 (9%) patients and downgraded the diagnosis in 2 (4%) patients.
Table 1. Presence of bronchiectasis in the HRCT (10 mm) vs the 1 mm data set.
| HRCT (10 mm) | 1 mm |
| Y _ 36 | Y _ 36 |
| Y _ 2 | N _ 0 |
| N _ 10 | N _ 10 |
| N _ 0 | Y _ 5 |
Y, bronchiectasis; N, no bronchiectasis; HRCT, high-resolution CT.
Total number of patients _ 53.
Concordance between HRCT (10 mm) and 1 mm scans — per lobe
The concordance between HRCT and 1 mm scans is shown in Table 2 for each lobe. In total, there were 318 lobes and bronchiectasis was diagnosed in 111 lobes on HRCT and 139 lobes on 1 mm scans. There was agreement between the scans in 262/318 (83%) lobes. The 1 mm scans downgraded from bronchiectasis to no bronchiectasis in 12/318 (4%) lobes and upgraded from no bronchiectasis to bronchiectasis in 40/318 (13%) (Table 2). Two examples are illustrated (Figures 1 and 2).
Table 2. Concordance in the diagnosis of bronchiectasis.
| RUL | RML | RLL | LUL | LING | LLL | |
| Yes | 13 | 21 | 17 | 14 | 19 | 15 |
| No | 31 | 21 | 27 | 34 | 23 | 31 |
| Downgraded | 1 | 6 | 4 | 0 | 0 | 1 |
| Upgraded | 8 | 5 | 5 | 5 | 11 | 6 |
RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe; LING, lingula.
Concordance is graded as yes (bronchiectasis in both scans); no (no bronchiectasis in either scan); downgraded (bronchiectasis on HRCT to no bronchiectasis on 1 mm); upgraded (no bronchiectasis on HRCT to bronchiectasis on 1 mm scans).
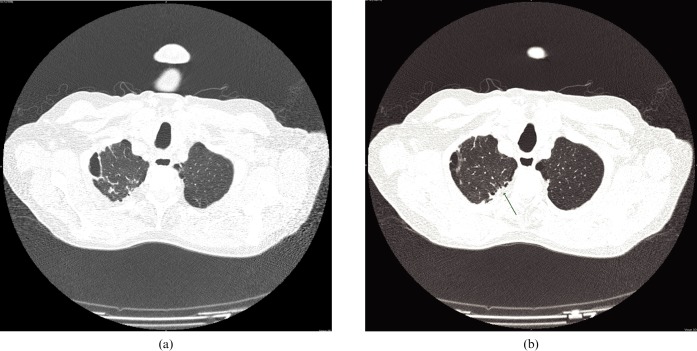
Figure 1.
(a) High-resolution CT of the chest (10 mm). (b) 16-slice chest CT (1 mm) — upgrading from no bronchiectasis (a) to tubular bronchiectasis (arrow).
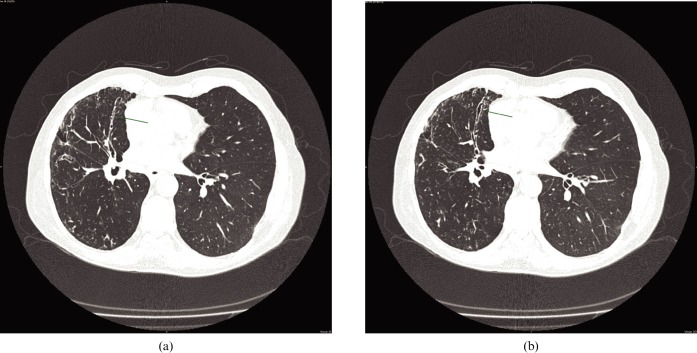
Figure 2.
(a) High-resolution CT of the chest (10 mm). (b) 16-slice chest CT (1 mm) — upgrading from tubular bronchiectasis (a) to varicose bronchiectasis (arrows).
CT scores in scans diagnosed with bronchiectasis
The median CT scores per patient were higher for the 1 mm dataset (5; range, 2.0–10.5) compared with the HRCT dataset (4; range, 2.0–7.5) (p _ 0.002).
Degree of confidence in diagnosing bronchiectasis
On those scans with bronchiectasis diagnosed on both HRCT and 1 mm scans, there was increased confidence of diagnosis (change from “possible” to “probable” or “definite”) in 32/99 (32%) of the 1 mm scans (Table 3) (p <0.001).
Table 3. Confidence in diagnosis of bronchiectasis using 1 mm scans.
| Confidence | RUL | RML | RLL | LUL | LING | LLL |
| No change | 10 | 15 | 13 | 8 | 9 | 9 |
| Decrease | 0 | 0 | 0 | 0 | 2 | 1 |
| Increase | 3 | 6 | 4 | 6 | 8 | 5 |
RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe; LING, lingula.
Change in confidence with 1 mm scans compared with HRCT for scans with bronchiectasis diagnosed on both HRCT and 1 mm scans.
Discussion
This study confirms improved diagnostic accuracy for the diagnosis and exclusion of bronchiectasis using 16-slice chest CT (1 mm cuts) compared with conventional HRCT of the chest. Reconstructed HRCT images generated from multidetector CT (MDCT) scanner data acquisition have been shown to be of comparable quality to images obtained using conventional HRCT [8], and so this approach was considered the best way to compare HRCT and MDCT, whilst limiting the radiation dose and not subjecting the patients to two scans.
The radiation dose for MDCT of the chest is known to be higher than that for HRCT [9, 10]. In our institution, the average effective dose for MDCT of the thorax is 7 mSv (dose–length product (DLP) _ 394 mGy cm), whereas HRCT of the thorax on the same 16-slice scanner gives a lower effective dose of 5 mSv (DLP _ 282 mGy cm).
The sensitivity of conventional HRCT, however, is limited owing to the 10 mm gaps between the non-contiguous slices and image degradation owing to motion artefact. The presence of data gaps on HRCT means that relatively small areas of bronchiectasis may be missed between sections [7]. This occurs particularly if the bronchiectatic segment runs in the axial plane, predominantly in the middle lobe and lingula. Misinterpretation of broncho-arterial ratio may also result if the scan plane lies close to bifurcations in the vessels or bronchi, as these two levels may not coincide.
The introduction of MDCT scanners has allowed assessment of the chest with thin-section collimation and rapid acquisition, often in a single breath-hold, thus improving spatial resolution [11]. Improved resolution also along the z-axis allows multiplanar reformatting, so that images can be interrogated in any plane [12]. These factors should reduce motion artefact, improve image quality and therefore increase sensitivity for the detection and exclusion of bronchiectasis. Dodd et al [13] confirmed that helical 16-slice MDCT was superior to HRCT in 10-mm intervals at showing the presence and extent of bronchiectasis, and Chooi et al [12] showed that the use of multiplanar image reconstruction further improves the confidence in diagnosing bronchiectasis. Despite having the capability in this study to use multiplanar reformatting to interrogate the 1 mm dataset, we opted not to use this function so that the two datasets were analysed and compared in the same axial plane. This study also showed improved confidence in the diagnosis of bronchiectasis with MDCT.
In conclusion, there is improved diagnostic accuracy and confidence for the diagnosis and exclusion of bronchiectasis using 16-slice chest CT (1 mm cuts) compared with conventional HRCT of the chest. The improved diagnostic accuracy therefore justifies the higher radiation dose incurred by performing a volume acquisition rather than performing the previously accepted gold standard HRCT of the thorax.
References
- 1.Naidich DP, McCauley DI, Khouri NF, Stitik FP, Siegelman SS, et al. Computed tomography of bronchiectasis. J Comput Assist Tomogr 1982;6:437–44 [DOI] [PubMed] [Google Scholar]
- 2.Grenier P, Maurice F, Musset D, Menu Y, Nahum H. Bronchiectasis: assessment by thin-section CT. Radiology 1986;161:95–9 [DOI] [PubMed] [Google Scholar]
- 3.Joharjy IA, Bashi SA, Adbullah AK. Value of medium-thickness CT in the diagnosis of bronchiectasis. AJR Am J Roentgenol 1987;149:1133–7 [DOI] [PubMed] [Google Scholar]
- 4.Phillips MS, Williams MP, Flower CD. How useful is computed tomography in the diagnosis and assessment of bronchiectasis? Clin Radiol 1986;37:321–5 [DOI] [PubMed] [Google Scholar]
- 5.Smith IE, Jurriaans E, Diederich S, Ali N, Shneerson JM, Flower CD. Chronic sputum production: correlations between clinical features and findings on high resolution computed tomographic scanning of the chest. Thorax 1996;51:914–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diederich S, Jurriaans E, Flower CD. Interobserver variation in the diagnosis of bronchiectasis on high-resolution computed tomography. Eur Radiol 1996;6:801–6 [DOI] [PubMed] [Google Scholar]
- 7.Kang EY, Miller RR, Muller NL. Bronchiectasis: comparison of preoperative thin-section CT and pathologic findings in resected specimens. Radiology 1995;195:649–54 [DOI] [PubMed] [Google Scholar]
- 8.Studler U, Gluecker T, Bongartz G, Roth J, Steinbrich W. Image quality from high resolution CT of the lung: comparison of axial scans and of sections reconstructed from volumetric data aquired using MDCT. AJR Am J Roentgenol 2005;185:602–7 [DOI] [PubMed] [Google Scholar]
- 9.Mayo JR, Jackson SA, Muller NL. High-resolution CT of the chest: radiation dose. AJR Am J Roentgenol 1993;160:479–81 [DOI] [PubMed] [Google Scholar]
- 10.Yi CA, Lee KS, Kim TS, Han D, Sung YM, Kim S. Multidetector CT of bronchiectasis: effect of radiation dose on image quality. AJR Am J Roentgenol 2003;181:501–5 [DOI] [PubMed] [Google Scholar]
- 11.Dawson P, Lees WR. Multislice technology in computed tomography. Clin Radiol 2001;56:302–309 [DOI] [PubMed] [Google Scholar]
- 12.Chooi WK, Matthews S, Bull MJ, Morcus SK. Multislice helical CT: the value of multiplanar image reconstruction in assessment of the bronchi and small airways disease. Br J Radiol 2003;76:536–40 [DOI] [PubMed] [Google Scholar]
- 13.Dodd JD, Souza CA, Muller NL. Conventional high-resolution CT versus helical high-resolution MDCT in the detection of bronchiectasis. AJR Am J Roentgenol 2006;187:414–20 [DOI] [PubMed] [Google Scholar]