Abstract
Background
Obtaining the definitive data necessary to determine the safety and efficacy of using antiretroviral treatment (ART) to reduce the sexual transmission of HIV in heterosexual couples encountered an array of ethical challenges that threatened to compromise HPTN 052, the multinational clinical trial addressing this issue that has profound public health implications.
Purpose
To describe and analyze the major ethical challenges faced in HPTN 052.
Methods
The ethical issues and modifications of HPTN 052 in response to these issues were catalogued by the principal investigator, the lead coordinator, and the ethicist working on the trial. The major ethical issues that were unique to the trial were then described and analyzed, referring as appropriate to published literature and emerging guidance and policies. Ethical challenges that must be addressed in many clinical trials, such as those related to obtaining informed consent and making provisions for ancillary care, are not described.
Results
When HPTN 052 was being designed, ethical questions emerged related to the relevance of the research question itself given data from observational research and a range of beliefs about the appropriate means of preventing and treating HIV-infection and AIDS. Further, ethical challenges were faced regarding site selection since there was a scientific need to conduct the research in settings where HIV incidence was high, but alternatives to study participation should be available. As in most HIV prevention research, ethical questions surrounded the determination of the appropriate prevention package for all of those enrolled. During the course of the trial, guidance documents and policies emerged that were of direct relevance to the research questions, calling for a balancing of concerns for the research subjects and trial integrity. When the study results were made public, there was a need to ensure access to the treatment shown to be effective that in some cases differed from the guidelines used at the sites where the research was being conducted. In addition, questions were raised about whether there was an obligation to notify subjects about “unlinked’ transmissions of HIV, that is, infections acquired outside of the designated sexual partners enrolled in the study.
Limitations
The ethical issues described are limited to those discerned by the authors and not those of other stakeholders who may have identified additional issues or had a different perspective in analyzing them.
Conclusions
Understanding the ethical challenges faced in HPTN 052 promises to inform the design and conduct of future complex, long-term clinical trials aimed at addressing critical scientific and public health questions, where data and practice patterns emerge over the course of the trial.
Introduction
After years of speculation and debate, definitive data now indicate that the use of antiretroviral treatment (ART) in persons who are HIV-infected can reduce transmission of HIV to their heterosexual partners.1 This finding has profound global implications. While the publication of the results of HIV Prevention Trials Network (HPTN) 052, the multinational trial that demonstrated these salutary results, is widely heralded as a success, from its outset the trial faced a series of ethical challenges that threatened the ability to answer the primary research questions. These ethical challenges evolved over the course of the trial and necessitated deliberation and response, not only from the investigators, sponsors, community members, and oversight bodies, but also from those with expertise in ethics. Understanding these ethical challenges promises to inform the design and conduct of future complex, long-term clinical trials aimed at addressing critical scientific and public health questions where data and practice patterns continue to emerge over the course of the trial.
HPTN 052 was sponsored by the National Institute of Allergy and Infectious Diseases/National Institutes of Health (NIAID/NIH) and was designed to address two questions. First, can ART that suppresses HIV replication prevent sexual transmission of the virus to a sexual partner? Second, is earlier ART (offered at a high CD4 count) better for personal health? Accordingly, HPTN 052 involved random assignment to early versus delayed treatment of HIV. The logistical and practical aspects of designing and implementing the trial are detailed elsewhere1,2. Briefly the pilot phase (2005–7) enrolled 92 HIV serodiscordant couples, where the index subject was HIV-infected with a CD4 count between 300–500 cells/mm3 at recruitment and their designated sexual partner was HIV-uninfected; ART in the delayed arm was offered when the CD4 count fell below 200 cells/mm3, thereby allowing some time to demonstrate protection by ART in those in the immediate arm. By the time recruitment began for the full phase of the study (2007), the protocol was modified with respect to both the CD4 inclusion criteria and the timing for the initiation of ART. Specifically, upon enrollment, the infected partner was required to have a CD4 count of 350–550 cells/mm3; and ART was initiated in the delayed arm to when two consecutive CD4 counts below 250 cells/mm3 were observed. Given the medical importance of initiating ART before the CD4 count reached 200 cells/mm3, CD4 counts were repeated soon after an initial count was below 250 cells/mm3. These protocol modifications were made by the study team in response to recommendations from the Data and Safety Monitoring Board (DSMB) that was well aware of the potential health benefits of initiating ART at a higher CD4 count. Further, updated World Health Organization (WHO) guidelines were issued in early 2006, recommending that ART be initiated between 200 – 350 cells/mm3.3 Ultimately, 1763 serodiscordant couples were enrolled at 13 sites in 9 countries.
Initial Ethical Challenges: Study Design, Site Selection, and the Prevention Package
Study Design
Among others, necessary conditions for research to be ethically acceptable are that a study appropriately and rigorously designed to address relevant research questions.4 In randomized clinical trials, such research may rightly involve examining testing interventions for which there is a lack of expert consensus on whether one study arm is superior to another. Some scholars believe that such a state of affairs can be described as “clinical equipoise”,5 yet others find this notion to be problematic6. While it is beyond the scope of this paper to defend a particular conceptual approach, it seems fair to say that those on both sides of the conceptual debate would endorse the ethical requirements delineated above6,7.
As the HPTN 052 protocol was being developed, it was clear that there was a need to develop means for preventing the sexual transmission of HIV infection as well as to offer the best treatment for those infected with HIV. While limited data were available concerning the research questions the study addressed, some experts at the time believed that the primary research question regarding transmission to a sexual partner had already been answered based upon a single retrospective observational study that associated blood HIV viral load and transmission probability in Uganda.8 In other words, the strong biological plausibility of the idea combined with the observational data suggested to some that a randomized trial was not required. This belief had to be explicitly considered to ensure that conducting the proposed research would still be ethically appropriate This in part arguable involves whether there was clinical equipoise regarding each arm of the study in terms of the main outcome measures. Note that clinical equipoise permits particular individuals to disagree that uncertainty remains since under this approach the crucial assessment is whether there is uncertainty among experts all things considered. Accordingly, it was critical to recognize the limitations of the findings from the observational Uganda study. First, the Uganda study did not involve the use of ART, nor did it determine whether apparent HIV transmission events were virally linked. Since HIV can be acquired outside individual partnerships1, demonstrating viral linkage is critical. Most importantly, the observational data from Uganda could not provide insight about the magnitude or durability of benefit afforded by intervening with ART; however, such data are critical for developing sound prevention strategies. Ultimately, this information from HPTN 052 regarding the extent to which ART prevented HIV transmission became a catalytic event for establishing that ART can help prevent infection with HIV9; at its outset HPTN 052 was poised to help answer research questions about which there were substantial uncertainty.
Site Selection
In order to answer the primary research question, it was essential to conduct HPTN 052 at sites that were experiencing high incidence rates of HIV infection. Across much of the world at the time the study was being designed, high HIV incidence rates were commonplace in resource constrained settings. As a consequence, as the trial was being designed, ART was not generally available at most of the research sites, generating claims that the trial might be “coercive”, since participants would have access to life-saving drugs that otherwise would not be available to them. While the unavailability of ART at the research sites reflected longstanding issues of global justice, labeling the trial as coercive was misplaced since coercion implies a forced bad choice.10 Given what was known about the use of ART at the time, deciding whether to participate in HPTN 052 did not necessarily require making a forced bad choice. Similarly, offering enrollment in the trial would not be properly considered an undue inducement since the offer of participation including access to ART would not reasonably seem to adversely affect decision-making of potential subjects.11 However, if there was unavailability of ART at the research sites, enrollment would understandably be considered a strong incentive. Fortunately, the World Health Organization’s Three by Five Campaign12, the Global Fund to Fight AIDS, Tuberculosis, and Malaria13 and the President’s Emergency Plan for AIDS Relief (PEPFAR)14 made ART far more available than it had been before HPTN 052 fully started, so patients with low CD4 counts who unequivocally needed ART generally had access to treatment according to country guidelines without having to enroll in HPTN 052. It is important to note, however, that this typically meant that ART was available for those with very low CD4 counts who would de facto be ineligible for enrollment in the HPTN 052 study. In addition, in coordination with NIAID, a separate study (AIDS Clinical Trials Group 5175) was launched to offer the option of participating in a treatment clinical trial for potential participants who screened out of HPTN 052 due to CD4 count falling below the threshold required for study entry.15
The prevention package
Until quite recently, HIV prevention in adults depended entirely on reducing higher risk behavior through counseling and the provision of condoms. To provide ART without offering safer sex counseling and condoms in HPTN 052 would suggest that the investigators and sponsor were not concerned with the well-being of the participants and were willing to tolerate HIV transmission to address the research questions. Conversely, if HIV transmission was decreased greatly as a result of counseling and behavior change, the trial might well prove futile. This tension is commonplace in HIV-prevention trials, yet including a “prevention package” is ethically obligatory. As discussed in more detail elsewhere, developing a particular prevention package for a trial should be established with broad input and include interventions that are known to be effective, reasonably accessible, and practically achievable.16 In order to ensure the integrity of a trial, it should be powered appropriately to account for the anticipated prevention benefit from the package. In HPTN 052, couples and adherence counseling was optimized so that the intervention could reasonably be expected to be effective, accessible and achievable. In addition, the study was powered to anticipate the very low level of HIV transmission that was actually observed.1
Ethical Challenges during the Study: Evolving Guidelines and Policies
As HPTN 052 was ongoing, there was growing enthusiasm for using ART for prevention, as well as for initiation of earlier treatment (at a higher CD4 cell count). However, HPTN 052 was the only randomized clinical trial actually addressing these questions. While another study17 discussed below was organized to address the question of when to initiate ART, the actual enrollment and management led to the study of a different population. In order to generate the most orderly clinical and public health recommendations the World Health Organization has generated a strategy to weigh and employ the strength of evidence18. Based on available evidence of recognized moderate or low strength, HIV treatment guidelines were issued that called for changes in current ART practice.19 This evolving guidance brought into sharp focus the ethical tensions inherent to a moral obligation to intervene, and the sometimes conflicting need for gathering data to develop evidence-based practices. Given these guidelines, there was a clear need to deliberate about the protection of the research subjects, the appropriateness of the HPTN 052 research design including the continued existence of clinical equipoise, and the integrity of the trial itself. The nature of these emerging guidelines and policies and their implications for HPTN 052 with respect to prevention and time to initiate treatment over the course of the trial are discussed below.
ART and HIV transmission
Prior to the results from HPTN 052, two lines of evidence were used to examine the effects of ART on sexual transmission of HIV: analyses of HIV transmission among serodiscordant couples in observational studies,20, 21 and population-level ecological studies.22 While most observational studies support the idea that ART can decrease HIV transmission, not all population study results have reported a benefit from ART.23, 24 Further, there are clear limitations of observational and ecologic studies.25 Accordingly, although observational studies can be useful, the potential for confounding and systematic error should cause great pause when and if such studies are used to support changes in medical or public health policy. The randomized controlled trial method is used specifically to reduce many of these concerns, leading to a higher level of evidence18. Thus, despite biological plausibility, evolving data from population studies, and growing interest in using ART for prevention during the course of the HPTN 052, it remained unclear if this approach was truly safe and effective, warranting continuation of the trial. While it may seem intuitive that early initiation of ART might be desirable, untoward side effects in new populations always require consideration. In addition, the effects of ART on sexual behavior have long been a concern, with the fear that increased risk behavior might offset the prevention benefit provided by ART.26 Ultimately, he desire for rigorous data needed to be balanced against the interests of the subjects; accordingly HPTN 052 included not only plausible approaches to the prevention of HIV transmission, but also regular systematic monitoring by the DSMB.
When to start ART
At least five observational retrospective studies addressing the optimal time to initiate ART have been published.24, 27–30 These studies all suggest that ART started at a CD4 count higher than 200 cells/mm3 reduces morbidity and mortality from HIV infection, but to differing degrees depending on the methods and the cohorts. The greatest disagreements in these reports surface when ART is initiated at CD4 counts greater than 500 cells/mm3 where differences observed are smaller, and sometimes negligible. As the first of these reports surfaced as meeting abstracts or publications, many organizational (normative) treatment guidelines underwent review and were modified in response to them.3,31–33 The WHO guidelines were of greatest importance to HPTN 052 because of the multinational nature of the study.3,31 However, it should be emphasized that the countries that participated in HPTN 052 did not uniformly follow the evolving WHO Guidelines (see Table). The country decisions were predicated on their own expert response to the strength of evidence, and the general lack of availability of enough ART to follow WHO guidelines if they were put into place. In 2009, investigators working in Haiti reported that subjects initiating ART at a median CD4 count of 287 cells/mm3 did considerably better than those delaying ART until a median CD4 count of 160 cells/mm3.17 While the data from this Comprehensive International Program of Research on AIDS (CIPRA) Haiti study were compelling, understanding the potential implications of these data for HPTN 052 required considering a variety of questions, beginning with the external validity of the findings. Were the populations in the CIPRA Haiti and HPTN 052 studies so similar that the results applied to the HPTN 052 study? Were the study designs so similar that the CIPRA Haiti results addressed the “when to start” question in HPTN 052?
Table 1.
HPTN 052 Implementation Status of WHO 2009 Guidelines for ART Initiation*
| Site | Implementation Status |
|---|---|
| SOUTH AMERICA | |
| Brazil | Threshold is at CD4 <350 |
| ASIA | |
| India | Threshold is currently at CD4 <350 for HIV/TB (pulm) co-infected, and pregnant women with WHO stage 3 disease, and Stage 4 disease or HIV with extra-pulmonary TB initiate ART irrespective of CD4 cell count. General population threshold to increase to CD4 < 350 soon. |
| Thailand | Current CD4 threshold for the general population is <200. Threshold increase to CD4 <350 for asymptomatic HIV positive person will be reconsidered next year (2012). In order to initiate ART now at CD4 <350, a person needs to have some specific illnesses that are related to HIV/AIDS or WHO stage 4 diseases. |
| AFRICA | |
| Botswana | Threshold remains at CD4 <250. Botswana National Subcommittee on Clinical Guidelines is awaiting assurance of resources before considering increasing the threshold. |
| Kenya | Threshold increased to CD4 <350 in late 2010, and is currently being implemented at local clinics. |
| Malawi | Current CD4 threshold for the general population is <250. Threshold is currently at CD4 <350 for pregnant and breastfeeding women. Any person with WHO stage 3 or stage 4 disease is eligible regardless of CD4 count. |
| South Africa | Threshold remains at CD4 <350 for HIV/TB co-infected, and pregnant women with CD4 <350 or have WHO stage 3 or 4 disease. |
| Zimbabwe | Due to resource constraints, the MOH released guidelines in March 2011 for a phased-approach of implementation of ART initiation for CD4 <350 over next three years, starting 01 April 2011. |
Current as of April 2011
On careful examination it became clear that there were important differences in the two studies. In short, ART was initiated in subjects in HPTN 052 at higher CD4 counts than in the CIPRA Haiti study in both the immediate and delayed arm. Ultimately, in HPTN 052, the median CD4 count for the infected partner was 442 cells/mm3 in the immediate arm and 428 cells/mm3 in the delayed arm; ART was initiated in the delayed arm at a CD4 count median of 221 cells/mm3 (Range: 199–249 cells/mm3)1. Nevertheless, the CIPRA Haiti results and the anticipated changes in WHO guidelines expected to specify earlier initiation of ART, led NIAID to request an urgent DSMB meeting in July 2009 to consider the aggregate data. The primary purpose of this deliberation was to protect the well-being of the subjects enrolled in the trial; here was a secondary but critical obligation to protect the integrity of the trial, if appropriate. These deliberations emphasize the constant tension between the need for modification of clinical and public health guidelines in response the best available evidence, and the generation of better evidence: if randomized controlled trials were routinely discontinued because of observational data or changing expert belief, many critical trials would not come to completion. In other words, the opportunity to obtain a higher level of evidence to address critical questions would be foreclosed.
Upon review of all the internal and external data, the DSMB saw no evidence of harm to the HPTN 052 subjects and the study was permitted to continue without modification. However, in November of 2009, when new “Rapid Advice” WHO guidelines were released, which recommended that ART be initiated at or before a CD4 count falls below 350 cells/mm3,31 all couples enrolled in the study were provided information about the new guidelines.
Despite uniformity in this approach across the study sites, Kenya, one of the participating countries in HPTN 052 with a site in partnership with the Centers for Disease Control-sponsored Kenya Medical Research Institute, adopted the new WHO guidelines in late 2010. The CDC felt that a change in country guidelines to comport with the international guidelines should be endorsed, and that the study participants should be provided with ART to be consistent with these guidelines. Given the desire to maintain uniformity across all sites, consideration was given to discontinuation of the study site, but the CDC declined this option. As an alternative, participants at the site were given information about the WHO and country guidelines and index participants in the delayed arm were told how to obtain ART outside the study at the country-recommended CD4 count level should they choose to seek it. Eight (8) participants elected to do so; for purposes of analysis of data, those changes in treatment were considered protocol violations.
Ethical Challenges based on Trial Results: Delivering the Benefits
In April 2011, the DSMB observed that there was significant benefit to subjects in the early ART arm of HPTN 052 and recommended that the results be made public as soon as possible. Before this could transpire, decisions needed to be made about how to manage subjects in the delayed ART arm. Based on the results, the study team was challenged to initiate ART in delayed arm subjects at a CD4 count higher than in-country or WHO guidelines. In addition, it was recognized that if participants in HPTN 052 were initiating ART at a higher CD4 count than specified in country guidelines, there might be difficulty in transitioning subjects onto locally-provided ART at the end of the study. This was discussed with each site and country-by-country strategies to assure continued therapy after the trial were developed.
The time of initiation of ART in response to CD4 count in HPTN 052 was modified several times during the course of the study (See Figure), emphasizing the difficulty of guidance in the absence of higher level evidence. When the HPTN 052 study was being developed, several IRBs questioned the wisdom of initiating ART before the CD4 count fell below 200 cells/mm3, which was the standard of care for asymptomatic patients in 2002 when the safety of the earlier initiation of ART had not been well established34. As described earlier, by 2009 the belief about the ideal time to start treatment had evolved so much as to jeopardize the continuation of the trial, although no high level evidence to support this position had yet surfaced. The HPTN 052 trial results themselves demonstrated some degree of benefit at a higher CD4 count than recommended in 2009 WHO guidelines, and certainly beyond the resources of most countries participating in HPTN 052. But to allow the study subjects to realize the benefits of the trial the investigators and the sponsor were required to generate their own unique standard of care, hoping that guidelines and policies would follow suit. In fact, in 2011, PEPFAR announced new guidance consistent with the results of HPTN 052.35 Similarly, WHO conducted a consultation in 2011 and is expected to issue new ART guidelines in 201236).
Figure 1.
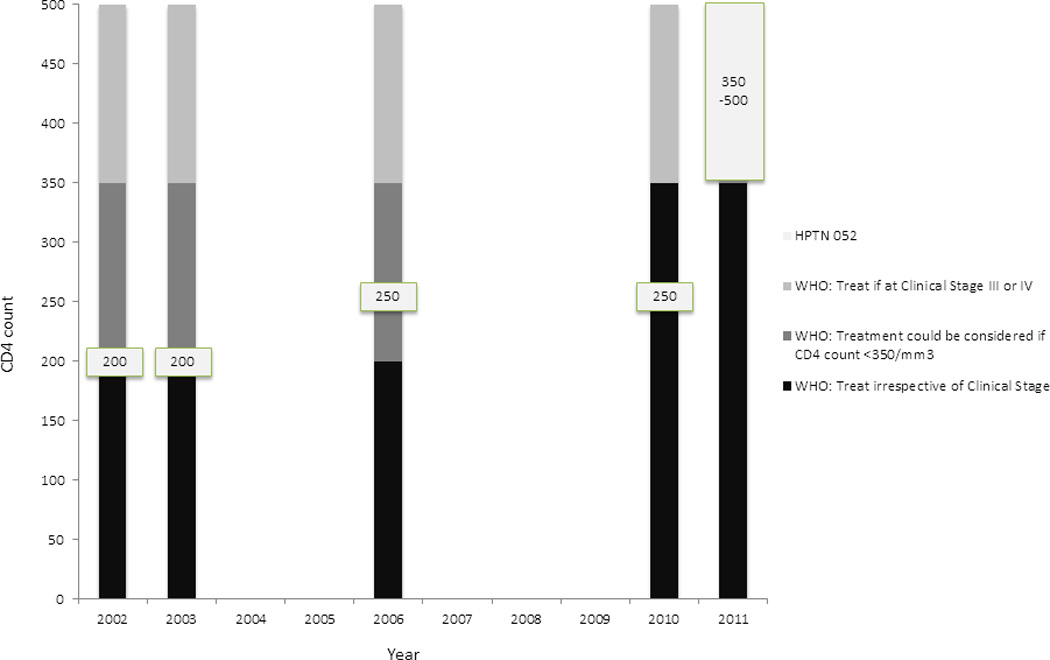
Initiation of ART over Time
Linked and Unlinked Transmission
The primary endpoint of HPTN 052 requires the establishment of virally linked and unlinked transmission events.1 While transmission linkage information is important in understanding the study results, whether to communicate such results to participants is another matter. After considering the merits of disclosing linkage information to participants, a decision was made to keep it confidential. The justification for doing so is based on the potential harms related to disclosure or non-disclosure. Any potential benefits for the disclosure to the index subject would derive from having information about sexual activity outside the partnership that would then translate into engaging in safer sexual practices to minimize the chance of sexually transmitted infections. Conversely, revealing an unlinked transmission could lead to harm and even physical violence to the newly infected subject. In addition, each member of the couples participating in the study gave individual consent, which stipulated that any information about sexual activity would be kept confidential from the other member of the couple. Parenthetically, couples with unlinked transmission were more likely to acknowledge multiple sexual partners.37, 38
Concluding Comments
In May 2011, results of HPTN 052 were made available to the sites, the study subjects, and the public after median 1.7 years of follow-up1. But as mentioned earlier, the study was designed to measure not only the magnitude, but also the durability of ART benefit. Regardless of accelerated use of ART in the delayed arm, the study has the statistical power to address these questions. In particular, will ART continue to offer a prevention benefit to an HIV negative partner with the reliability observed in the first two years of the study? Accordingly, the study will continue until 2015 as originally planned.
The HPTN 052 trial encountered a range of ethical challenges, some anticipated and some surprising. The investigators worked closely with the local IRBs to sort through the issues required for continuing approval of study implementation. The experience from HPTN 052 suggests that a prospective “ethics plan” comparable to a statistical analysis plan, anticipating the challenges and envisioning potential scenarios, is a good idea. Accordingly, HPTN appoints an ethics representative to each protocol team as the protocols are being developed to address ethical concerns that occur in real time.16 The most important ethics lesson from HPTN 052 was the constant threat to the study from observational and ecological results stemming from huge amounts of emerging data generated by investigators working on HIV, and the use of such data in guideline adjustments made by agencies and their experts based on the best available evidence. As these necessary changes were made, they threatened the very research that might support or refute the recommendations themselves. Certainly this concern is not unique to HPTN 052, and there is no way to abrogate this tension. Do ongoing studies that do not adhere to guideline revisions made during the course of the study de facto become unethical? Unfortunately, a definitive yes or no answer to this question in the abstract is impossible. So the ethical analysis hinges upon what circumstances should new evidence lead to the termination of a clinical trial. Making these determinations is largely the responsibility of a knowledgeable independent DSMB. In the case of HPTN 052 the DSMB (which met 11 times during the course of the study) played a central and critical role. We believe the system in place actually works as long as the investigators, IRBs and the DSMB maintain good communication39. We believe that the “ethical odyssey” of HTN 052 is a demonstration of the success of the current system of research oversight.
Acknowledgements
The authors appreciate the thoughtful and constructive comments by the peer-reviewers of earlier versions of this manuscript. Work on this document was supported by Grant Number U01 AI068619 from the National Institute of Allergy and Infectious Diseases (NIAID), with additional support from the National Institute on Drug Abuse (NIDA) and the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAID, NIDA, NIMH, or the National Institutes of Health.
Contributor Information
Myron S. Cohen, J. Herbert Bate Distinguished Professor, Medicine, Microbiology and Immunology, and Public Health Director, UNC Institute of Global Health and Infectious Disease, Chief, Division of Clinical Infectious Diseases, 130 Mason Farm Road, Suite 2115, CB#7030, UNC Chapel Hill, Chapel Hill, NC. 27514, Phone: 919-966-2536, Fax: 919-966-6714, mscohen@med.unc.edu.
Marybeth McCauley, FHI360, 1825 Connecticut Avenue, NW, Washington, DC 20009, Phone: 202-884-8000, MMcCauley@fhi360.org.
Jeremy Sugarman, Harvey M. Meyerhoff Professor of Bioethics and Medicine, Johns Hopkins Berman Institute of Bioethics, 1809 Ashland Ave. Deering Hall, Room 203, Baltimore, MD 21205, Phone: 410-614-5634, Fax: 410-614-5360, jsugarman@jhu.edu.
REFERENCES
- 1.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Curr Opinion HIV AIDS. 2012 doi: 10.1097/COH.0b013e32834f5cf2. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. ‘Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach’. [accessed September 2011];WHO Press. 2006 http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf. [PubMed]
- 4.Emanuel EJ, Wendler D, Grady C. What makes clinical research ethical? JAMA. 2000;283:2701–2711. doi: 10.1001/jama.283.20.2701. [DOI] [PubMed] [Google Scholar]
- 5.Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317:141–145. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]
- 6.Miller FG, Brody H. A critique of clinical equipoise: therapeutic misconception in the ethics of clinical trials. Hastings Center Report. 2003;33:19–28. [PubMed] [Google Scholar]
- 7.van der Graafand R, van Delden JJM. Equipoise should be amended, not abandoned. Clin Trials. 2011;8:408–416. doi: 10.1177/1740774511409600. [DOI] [PubMed] [Google Scholar]
- 8.Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342:921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 9.Cohen J. HIV treatment as prevention. Science. 2011;334:1628. doi: 10.1126/science.334.6063.1628. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins JS, Emanuel EJ. Clarifying confusions about coercion. Hastings Cent Rep. 2005;35:16–19. [PubMed] [Google Scholar]
- 11.Emanuel EJ. Ending concerns about undue inducement. J Law Med Ethics. 2004;32:100–105. doi: 10.1111/j.1748-720x.2004.tb00453.x. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. The 3 by 5 initiative. Available at: http://www.who.int/3by5/en/
- 13.Global Fund to Fight AIDS, Tuberculosis, and Malaria. Available at: http://www.theglobalfund.org/en/
- 14.The United States President’s Emergency Plan for AIDS Relief. Available at http://www.pepfar.gov/.
- 15.Randomized, Open-Label Evaluation of Efficacy of Once-Daily Protease Inhibitor and Once-Daily Non-Nucleoside Reverse Transcriptase Inhibitor-Containing Therapy Combinations for Initial Treatment of HIV-1 Infected Persons From Resource-Limited Settings (PEARLS) Trial. Available at: http://clinicaltrials.gov/ct2/show/NCT00084136.
- 16.Rennie S, Sugarman J. ‘HPTN Ethics Working Group, preparers. Ethics guidance document for research’. [accessed September 2011];HIV Prevention Trials Network. 2009 http://www.hptn.org/web%20documents/EWG/HPTNEthicsGuidanceV10Jun2009.pdf.
- 17.Severe P, Juste MA, Ambroise A, Eliacin L, Marchand C, Apollon S, et al. Early versus standard antiretroviral therapy for HIV-infected adults in Haiti. N Engl J Med. 2010;363:257–265. doi: 10.1056/NEJMoa0910370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organisation. Geneva: 2010. Mar, [accessed March 2012]. WHO handbook for guideline development. Available at: http://www.who.int/en/ [Google Scholar]
- 19.Donnell D, Baeten JM, Kiarie J, Thomas KK, Stevens W, Cohen CR, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–2098. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Del Romero J, Castilla J, Hernando V, Rodríguez C, García S. Combined antiretroviral treatment and heterosexual transmission of HIV-1: cross sectional and prospective cohort study. BMJ. 2010;340:c2205. doi: 10.1136/bmj.c2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Das M, Chu PL, Santos GM, Scheer S, Vittinghoff E, McFarland W, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dukers NH, Goudsmit J, de Wit JB, Prins M, Weverling GJ, Coutinho RA. Sexual risk behaviour relates to the virological and immunological improvements during highly active antiretroviral therapy in HIV-1 infection. AIDS. 2001;15:369–378. doi: 10.1097/00002030-200102160-00010. [DOI] [PubMed] [Google Scholar]
- 23.Jin F, Jansson J, Law M, Prestage GP, Zablotska I, Imrie JC, et al. Per-contact probability of HIV transmission in homosexual men in Sydney in the era of HAART. AIDS. 2010;24:907–913. doi: 10.1097/QAD.0b013e3283372d90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.When To Start Consortium. Sterne JA, May M, Costagliola D, de Wolf F, Phillips AN, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373:1352–1363. doi: 10.1016/S0140-6736(09)60612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith K, Powers KA, Meussig KE, Miller WC, Cohen MS. ART and population-level HIV transmission: ecology, observation, and interpretation. PloS Medicine. 2012 invited and under review. [Google Scholar]
- 26.Eaton LA, Kalichman S. Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies. Curr HIV/AIDS Rep. 2007;4:165–172. doi: 10.1007/s11904-007-0024-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kitahata MM, Gange SJ, Abraham AG, Merriman B, Saag MS, Justice AC, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–1826. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cain LE, Logan R, Robins JM, et al. When to initiate combined antiretroviral therapy to reduce mortality and AIDS-defining illness in HIV-infected persons in developed countries: an observational study. Ann Intern Med. 2011;154:509–515. doi: 10.1059/0003-4819-154-8-201104190-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sterne JA, Hernan MA, Ledergerber B, et al. Long-term effectiveness of potent antiretroviral therapy in preventing AIDS and death: a prospective cohort study. Lancet. 2005;366:378–384. doi: 10.1016/S0140-6736(05)67022-5. [DOI] [PubMed] [Google Scholar]
- 30.Writing Committee for the CASCADE Collaboration. Timing of HAART initiation and clinical outcomes in Human Immunodeficiency Virus Type 1 seroconverters. Arch Intern Med. 2011;171:1560–1569. doi: 10.1001/archinternmed.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. ‘Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents’. [accessed September 2011];WHO Press. 2009 http://www.who.int/hiv/pub/arv/rapid_advice_art.pdf.
- 32.Thompson MA, Aberg JA, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2010 recommendations of the International AIDS Society – USA Panel. JAMA. 2010;304:321–333. doi: 10.1001/jama.2010.1004. [DOI] [PubMed] [Google Scholar]
- 33.Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services; 2011. Oct 14, [Accessed January 2012]. Panel on Antiretroviral Guidelines for Adults and Adolescents; pp. 1–167. Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. [Google Scholar]
- 34.World Health Organization. Scaling up antiretroviral therapy in resource-limited settings: guidelines for a public health approach. [accessed January 2012];2002 Available at: http://www.who.int/hiv/pub/guidelines/pub18/en/index.htm. [PubMed]
- 35.PEPFAR Scientific Advisory Board, et al. PEPFAR Scientific Advisory Board Recommendations for the Office of the US Global AIDS Coordinator: Implications of HPTN 052 for PEPFAR’s Treatment Programs. [accessed January 2012];2011 Available at: www.pepfar.gov/documents/organization/177126.pdf.
- 36.WHO Consultation: The Strategic Use of Antiretrovirals for Treatment and Prevention of HIV Geneva, Switzerland, 14–16 November 2011. Executive summary. [accessed March 2012];2011 Available at: http://www.who.int/hiv/pub/meetingreports/consultation_20111116/en/index.html.
- 37.Hughes J, Hudelson S, Redd A, Wang L, Debes R, Chen Y, et al. Analysis of genetic linkage of HIV from couples enrolled in the HIV Prevention Trials Network 052 trial. Proceedings of the 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention; 2011 July 17–20; Rome, Italy. [Abstract]; [Google Scholar]
- 38.Eshleman SH, Hudelson S, Redd AD, Wang L, Debes R, et al. Analysis of genetic linkage of HIV from couples enrolled in the HIV Prevention Trials Network 052 trial. J Infect Dis. 2011;204:1918–1926. doi: 10.1093/infdis/jir651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor HA, Chaisson L, Sugarman J. Enhancing communication among data monitoring committees and institutional review boards. Clinical Trials. 2008;5:277–282. doi: 10.1177/1740774508091262. [DOI] [PubMed] [Google Scholar]


