Abstract
Little attention has been given to factors contributing to firefighters' psychosomatic well-being.
Objective
The purpose of this descriptive study was to examine such contributing factors in a sample of professional firefighters.
Methods
Measures assessing sleep, depression, substance use, social bonding, and quality of life were examined in 112 firefighters.
Results
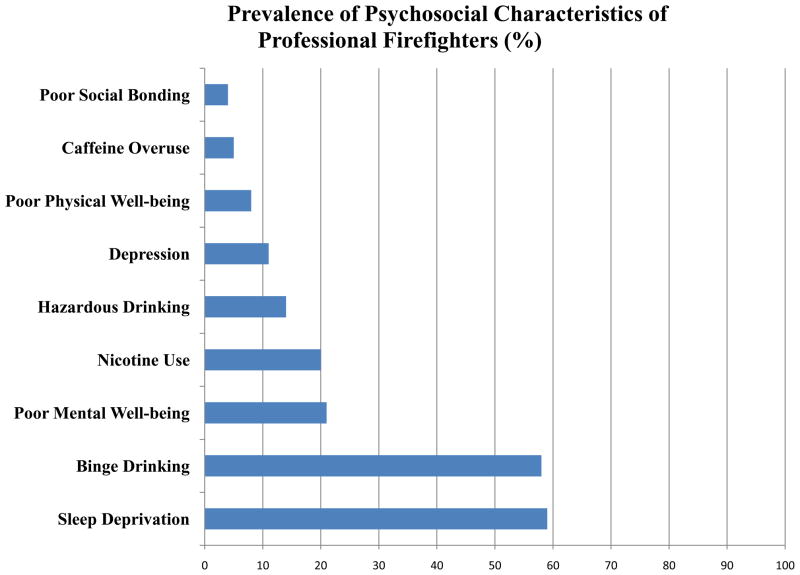
Overall, many firefighters reported sleep deprivation (59%), binge drinking behavior (58%), poor mental well-being (21%), current nicotine use (20%), hazardous drinking behavior (14%), depression (11%), poor physical well-being (8%), caffeine overuse (5%), or poor social bonding (4%).
Conclusions
Small-to-medium correlations were identified between sleep deprivation, depression, physical/mental well-being, and drinking behaviors. High-risk behaviors that impact psychosomatic well-being are prevalent in professional firefighters, which require environmental and individual-based health promotion interventions. The inter-correlation relationships between such behaviors, therefore, need to be explored in further details.
BACKGROUND
Professional firefighting is a strenuous and unique occupation due to the high levels of stress and risk involved as well as the low control nature of the job [1]. Anxiety and posttraumatic stress disorders (PTSD) are prevalent in the professional firefighters’ population and constitute a dominant area of investigation [6]. Limited attention has been given to describing factors that can contribute to firefighters’ job performance and overall well-being, such as sleep problems, depression, substance use, social bonding, and quality of life.
Sleep disturbance, fatigue, and work-related accidents are common among shift workers [2] who typically work 8-hour rotating shifts (e.g., daytime/night time) . However, in many fire departments, extended rotating shift of 10 hour (h) days / 14 h nights are common instead of the standard three 8 h-shift rotating schedule. Evidence suggests that although extended rotating shifts do not add any additional health hazards beyond that of the standard 8 h shift [3], fatigue, decreased alertness, and poor mood scores were more prevalent among firefighters working night shifts [4]. In fact, working time was found to be more predictive of impaired alertness and increased occupational accidents. For instance, sleep disturbance was prevalent beyond working time exceeding 50 h/week and occupational accidents were four-fold more prevalent beyond working time exceeding 70 h/week [2]. Current research indicates that sleep deprivation (<4–6 h of sleep in 24 h) is associated with decreased vigilance, alertness, and mental performance; increased sleepiness; fatigue, and depression; poor quality of life; and increased risk for cardiovascular events, digestive disorders, obesity, diabetes, obstructive sleep apnea, altered immune response, and malignancies [5]. However, the association between patterns of sleep and substance use within the social context of firefighters’ population and the overall impact on depression, quality of life and social bonding need further investigation.
In general population, the rates of PTSD and depression might be as low as 1.9% and 10%, respectively. Yet higher rates are seen in firefighters and other rescue workers exposed to human disasters, 17% and 22% for PTSD and depression, respectively [6]. Experienced firefighters are more likely to be exposed to human disasters given their time in the role. Yet, it has been found that there is a linear positive relationship between years of job experience as a firefighter and levels of traumatic stress and depression when comparing experienced firefighters with new recruits [7]; that is experienced firefighters were more likely to report lower levels of social support and self-esteem. Amount and variance of workload, group conflicts, social support, role ambiguity, and self-esteem were all found to be predictive of depressive symptoms among firefighters [8]. Nevertheless, job strain and depression has been repeatedly linked to increased risk of cardiovascular mortality [9], which was found to be as high as 44% in professional firefighters and four-fold risk when compared to other first responders [10, 11]. Assessing depressive symptoms in firefighters, therefore, is an important initial step in understanding the mental health needs of this population and preventing adverse physical and psychosocial health-related events. Additional concerns is that depression, as well as susceptibility to stress, might increase the risk of suicidal behavior, but may also have reciprocal influences with alcohol drinking patterns [12].
Low levels of alcohol consumption have been associated with relief of anxiety [13]. A concern, however, is when alcohol consumption becomes a hazardous behavior. Hazardous drinking places the firefighter and others at risk. Alcohol consumption behavior among persons and those in their social networks is highly correlated [14], concerning for a group of firefighters who are joined together for extended periods of time. In similar populations (e.g. military), heavy drinking pattern can be as high as 67% prevalent among men and 9% among women, with binge drinking pattern occurring in 48% of men and 31% of women [15], both patterns were higher than the general population. Little attention has been given to the prevalence and pattern of alcohol consumption in the social network of firefighters. Other modifiable risk behaviors among firefighters include cigarette smoking and coffee consumption. As central nervous system stimulants, caffeine and nicotine use result in increased alertness, mild euphoria, muscle relaxation and increased psychomotor activity [16]. Caffeine doses ranging from 2.5 to 7 mg-kg seem to improve high-intensity exercises performance [1], however, given the unpredictability of the job emergencies combined with rotation duty shifts that may span 16 hours at a time, the normal sleep patterns of firefighters can be disrupted by caffeine.
The concept of brotherhood as social bonding and connection is deeply rooted among firefighters [17]. Brotherhood has been defined by firefighters as a historical, traditional, and universal ideal characterized by inherent dedication, love, respect, and support for one another, living by a code of unspoken duty, trust, honor, and loyalty, and the establishment of membership and close relationships, connections, and bonds [17]. Firefighters develop close social bonds and connections with one another as a result of living in the firehouse and working closely together for extended periods of time when scheduled for duty. The social bonds and connections among firefighters and within the firehouse are important factors in ameliorating distress [7]. Ironically, some studies still suggest that experienced firefighters might have lower levels of social support making them more vulnerable to depression and stress [7, 8]. It is important to note however that despite understanding among firefighters regarding the significance of brotherhood as social bonding and connection, studies exploring social bonds and connection among firefighters are limited.
In summary, the assessment of high-risk behaviors that can be modified to promote health and well-being among firefighters has received little attention. The impact of sleep deprivation, depression, substance use (alcohol and caffeine consumption, nicotine use), social bonding and connection, and quality of life on the psychosomatic well-being of professional firefighters needs further exploration. Therefore, this descriptive study was conducted to examine the prevalence and complex relationships between sleep deprivation, depression, substance use, social bonding, and quality of life in professional firefighters.
METHODS
Subjects for this investigation were enrolled in the SAFFE study (Surveying and Assessing Firefighters Fitness and Electrocardiogram), a National Institute of Health-funded cross-sectional descriptive study to characterize firefighters hemodynamic responses while on-duty [18]. The SAFFE study drew professional firefighters from 13 firehouses in a metropolitan area of nearly 300,000 residents. Each firehouse had approximately 45 firefighters in 4 platoons that work in extended rotating shifts schedule, 2 day shifts (10 hours), 2 night shifts (14 hours), followed by 4 off-duty days.
All professional firefighters were eligible to participate. Recruitment was based on non-probability sampling; however, to minimize sampling bias, every possible effort was made to approach all eligible firefighters until the full sample was obtained. With Institutional Review Board’s approval, the research team composed of the principal investigator and four research assistants, travelled among the firehouses and recruited from all platoons. In a quiet, private room, consent was obtained and six paper-and-pencil surveys were completed. The surveys were used to assess sleep problems, depressive symptoms, substance use (alcohol, caffeine, and nicotine), social bonding, and quality of life (physical and mental well-being).
Measures
1. Sleep problems
the previously validated Pittsburgh Sleep Quality Index (PSQI) [19] and Epworth Sleepiness Scale (ESS) [5] were used to subjectively evaluate sleep quality in firefighters. Firefighters reporting disturbed sleep pattern (PSQI score ≥5) and/or decreased daytime alertness (ESS score >10) were considered sleep deprived. To objectively evaluate sleep pattern in professional firefighters, a small cohort completed a sleep diary, and continuously wore a motionlogger actigraph (Ambulatory Monitoring Inc., NY, USA) on their non-dominant wrist for 3 days, during which all activities including fire and medical calls were monitored. Four objective indices were obtained from the actigraph: sleep duration, sleep efficiency, sleep latency, and wake after sleep onset (WASO). Sleep pattern was considered disturbed if the firefighter had at least 2 of the following: sleep duration <6 h, sleep efficiency <85%, sleep latency >30 min, or WASO >30 min.
2. Depression
the Beck Depression Inventory (BDI-II) [20] was used to measure depressive behavior. BDI-II, a 21-question multiple-choice survey, is the most widely used self report inventory to screen for depressive symptoms. The 5 minute inventory includes items related to symptoms of depression including hopelessness, irritability, mood, and fatigue. The validity and reliability of BDI-II has been extensively studied [20]. Firefighters scoring ≥14 points (possible range 0–63) on the BDI-II were considered mild-to-moderately depressed.
3. Substance Use (Alcohol, Caffeine, & Nicotine)
The Time Line Follow Back (TLFB) [21] survey was used to characterize substances use behaviors. TLFB uses a calendar to estimate the daily alcohol, caffeine, and nicotine use over the past two weeks, beginning from the day of recruitment. Working backwards, the firefighters recorded for every day the (1) number of alcoholic drinks (as a standard drink), (2) number of caffeinated drinks (coffee, cola) consumed (in fluid ounces), and (3) number of cigarettes, cigars, and/or pipe bowls smoked, and/or dips of smokeless nicotine (as number of cigarettes). A consumption of ≥4 (men) or ≥3 (women) standard alcoholic drinks per day was considered a binge drinking behavior, with those who repeat the binge drinking behavior 2 or more times per week (≥p8 times per month) were considered hazardous drinkers. Also, a consumption of 700mg (~40 ounce coffee) of caffeine per day was considered caffeine overuse behavior. For this study, firefighters who reported the use of cigarettes, cigars, and/or pipe bowls smoked, and/or dips of smokeless nicotine at least once were considered nicotine users.
4. Social Bonding
a 30-item, 6-subscale survey, Spirituality in Everyday Life (SEL) [22], was developed for this study and used to measure social bonds and connections. Items reflected activities related to feeling supported by others, thinking about relationships with others, feeling a sense of belongingness, thinking about bonds with others, showing support for others, and being involved with others. A 5-point Likert-type scale (1=never to 5=repeatedly) was used to determine the frequency with which respondents experienced the activity within the past year.
5. Quality of Life (Physical and Mental Well-Being)
SF-12 Health Survey [23] was used to evaluate quality of life in the current study. The 2-min SF-12 survey is a shorter version of the SF-36 Health Survey designed to reproduce the physical (PHC) and the mental (MHC) health component summary scores of the overall subject’s health quality status. The reliability of SF-12 has been previously reported to be adequate (test-retest reliability > 0.76) [23]. In the current analysis, PHC and MHC scores <50% were considered indicators of poor physical and mental well-beings, respectively.
Statistical Analysis
All values are mean ± standard deviation. The degree of association between the constructs was determined using Pearson’s correlation coefficient (r) and partial correlation. Categorical values were compared using χ2 test and z-test for proportion differences to compare the prevalence of high-risk behaviors in different subgroups. All statistical analyses were performed using SPSS (Version 17) and a p <0.05 was considered statistically significant.
RESULTS
A convenient sample of one hundred and twelve professional firefighters (n=112, 16% of target population) was enrolled from six different fire houses from fire department. All firefighters (n=112, age 43.6±7.7 years, 95.5% men, 81% Caucasian, 13% African American, 6% Hispanic) completed the six paper-and-pencil surveys. The sample’s demographics were similar to that of fire department as a whole. Of note, the firefighters were experienced with the mean job duration of firefighting experience 15.5±7.0 years. On self-report, 11.6% were current smokers (reporting 17±12 cigarettes/day for 10.8±11.0 years), 11.6% previously quit smoking, and 18% were currently receiving medical treatment for cardiac or respiratory conditions (of note: 9% for hypertension, 5% for dyslipidemia, 5% for sleep apnea, and 4% for coronary artery disease).
The most prevalent problems were sleep disturbances and binge drinking (nearly 60%) followed by nicotine use and poor mental well-being (20%). Lower rates were found for depressive symptoms, hazardous drinking, caffeine overuse, poor physical well-being and poor social bonding which were less prevalent (Figure 1).
Figure 1. Prevalence of Psychosocial Characteristics of Professional Firefighters.
Sleep deprivation and binge drinking are the most prevalent followed by nicotine use and poor mental well-being. Other high-risk health behaviors were less prevalent.
The Cronbach’s alpha for the BDI-II survey in the sample was 0.86. Among the 112 firefighters in the sample, 89.2% (n=100) reported no depression, 10.8% (n=12) had some degree of depression (6.2% mild depression, 3.6% moderate depression, 1% severe depression), 59% (n=64) were sleep deprived (PSQI score =6.02±3.08, ESS score =5.22±2.84), 8% had poor physical well-being (n=9, PHC= 62%±13%), 21% had poor mental well-being (n=23, MHC= 56%±12%), 80% used alcohol (1.6±1.7 standard alcoholic drinks per day, range 0.0–9.7), 56% had binge alcohol drinking behavior, 14% had hazardous drinking behavior, 20% used nicotine, and 5.4% overused caffeine. Additionally, the overall Cronbach’s alpha for the newly developed SEL scale was 0.95. The exploratory factor analysis for SEL showed that the six subscales explained 72% of the expected variance. The mean total score for the overall scale was 95±20 (possible range 30 [worst] - 150 [best], observed range 30–143). Using receiver operator characteristics curve, a logical cutoff point of 55 (2 SD below the mean) was selected to identify those with low level of social bonding. Given that cutoff point, ~4% of firefighters had low level of social bonding within the social network of firefighters. Of note, the lowest mean subscale score (3.3±0.9) was related to feeling a sense of belongingness, and the highest (4.2±0.95) was related to feeling supported by others.
Compared to those who were not depressed, depressed firefighters were more likely to be sleep deprived (54% vs 100%, χ2=9.48, p=0.002), and to have hazardous drinking behavior (12% vs 33%, χ2=3.98, p=0.046). On the other hand, firefighters who were sleep deprived were more likely to report poor physical well-being when compared to those who were not sleep deprived (11% vs 0%, p<0.05 using z-test for proportion difference) but not poor mental-well-being. Those with hazardous drinking behavior were more likely to report nicotine use (50% vs 15%, χ2=10.9, p=0.001). Interestingly, comparing firefighters with caffeine overuse behavior to those without, firefighters with caffeine overuse behavior were more likely to have poor physical (50% vs 7%) and poor mental (66% vs 22%) well-being (p<0.05 using z-test for proportion difference). Interestingly, those with poor mental well-being were also more likely to report poor social bonding (13% vs 2%, p<0.05 using z-test for proportion difference).
A zero ordered correlation matrix shows the extent between the prevalence of the nine constructs: depressive symptoms, sleep deprivation, binge and hazardous alcohol drinking behaviors, caffeine overuse, nicotine use, poor physical and mental well-beings, and poor social bonding (Table 1). Overall, small-to-medium correlations (0.25–0.35) were identified between sleep deprivation, depressive symptoms, poor physical/mental well-beings, and drinking behaviors. To avoid misleading correlations between constructs due to a third causal construct, also known as a ‘spurious variable,’ partial correlation was used to examine significant correlations [24]. All significant correlations in Table 1 remained independent after controlling for other relevant constructs except depression and hazardous drinking that was insignificant after controlling for sleep deprivation and/or nicotine use. There was no relationship between sleep deprivation and hazardous drinking behavior (controlling for depression and/or poor physical well-being); or depression and poor mental well-being (controlling for sleep deprivation and/or hazardous drinking behavior). The distribution of these nine constructs among different demographics of firefighters (i.e., age, race, sex, years of experience as a firefighter, presence of obesity, hypertension and cardiac history) was only statistically significant in three: age, race and hypertension (Table 2).
Table 1.
Correlation Matrix between Psychosocial Characteristics of Professional Firefighters (n=112)
| Depressive Symptoms |
Sleep Deprivation |
Binge Drinking |
Hazardous Drinking |
Caffeine Overuse |
Nicotine Use |
Poor Physical Well-being |
Poor Mental Well-Being |
Poor Social Bonding |
|
|---|---|---|---|---|---|---|---|---|---|
| Depressive Symptoms | - | 0.30** | −0.06 | 0.19* | 0.05 | 0.05 | 0.16 | 0.18 | 0.09 |
| Sleep Deprivation | - | - | 0.17 | 0.17 | 0.04 | 0.03 | 0.26** | 0.14 | 0.07 |
| Binge Drinking | - | - | - | 0.35** | 0.08 | 0.15 | −0.07 | 0.02 | 0.07 |
| Hazardous Drinking | - | - | - | - | -0.01 | 0.31** | 0.08 | 0.06 | 0.06 |
| Caffeine Overuse | - | - | - | - | - | −0.02 | 0.36** | 0.26** | 0.17 |
| Nicotine Use | - | - | - | - | - | - | 0.12 | 0.04 | 0.03 |
| Poor Physical Well-being | - | - | - | - | - | - | - | 0.15 | −0.07 |
| Poor Mental Well-Being | - | - | - | - | - | - | - | - | 0.25** |
| Poor Social Bonding | - | - | - | - | - | - | - | - | - |
p<0.05,
p<0.01
Table 2.
The Prevalence of Psychosocial Characteristics of Firefighters among Different Demographics
| PREVALENCE RATE (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Depressive Symptoms |
Sleep Deprivation |
Binge Drinking |
Hazard Drinking |
Caffeine Overuse |
Nicotine Use |
Poor Physical Well- being |
Poor Mental Well- Being |
Poor Social Bonding |
||
| Age (yrs) | ≤40 | 31 | 9.7 | 74.2 | 61.3 | 12.9 | 3.2 | 25.8 | 11.1 | 22.2 | 6.5 |
| 41–47 | 41 | 19.5* | 66.7 | 61.1 | 14.6 | 4.9 | 19.5 | 9.4 | 28.1 | 4.9 | |
| ≥48 | 40 | 2.5 | 38.5* | 52.5 | 15.0 | 7.5 | 15.0 | 8.8 | 23.5 | 0 | |
| Race | White | 91 | 9.9 | 60.2 | 64.8* | 15.4 | 6.6 | 19.8 | 10.5 | 26.3 | 4.4 |
| Black | 15 | 20 | 60.0 | 26.7 | 13.3 | 0 | 13.3 | 8.3 | 25.0 | 0 | |
| Others | 6 | 0 | 33.3 | 33.3 | 0 | 0 | 33.3 | 0 | 0 | 0 | |
| Sex | Male | 107 | 11.2 | 57.7 | 57.0 | 15.0 | 5.6 | 19.6 | 10.0 | 23.3 | 3.7 |
| Female | 5 | 0 | 80.0 | 80.0 | 0 | 0 | 20 | 0 | 60.0 | 0 | |
| Obesity | Yes | 46 | 6.5 | 51.1 | 58.7 | 13.0 | 8.7 | 21.7 | 13.5 | 29.7 | 6.5 |
| No | 66 | 13.6 | 64.1 | 57.6 | 15.2 | 3.0 | 18.2 | 7.1 | 21.4 | 1.5 | |
| Hypertension | Yes | 40 | 2.5 | 53.8 | 60.0 | 20.0 | 2.5 | 20.0 | 8.1 | 13.5 | 5.0 |
| No | 72 | 15.3* | 61.4 | 56.9 | 11.1 | 6.9 | 19.4 | 10.7 | 32.1* | 2.8 | |
p<0.05.
Obesity = body mass index >30 kg/m2, Hypertension = blood pressure ≥135 (systole) or ≥85 (diastole) mmHg
Sleep Pattern (Actigraph)
While on night duty, a random cohort of firefighters (n=22) wore the motion logger actigraph continuously for 72 h. The demographics of this cohort was similar to that of the sample and general firefighters population (age=42±6 years, 86% men, 82% white, 18% black). Actigraph’s results showed that sleep duration was 6.1±1.8 h, sleep efficiency 89%±10%, sleep onset latency 38±39 minutes, and WASO 37±25 minutes. Approximately, 36% of firefighters (n=8/22) had a disturbed sleep pattern; there was no difference in PSQI score between the two groups, however, those with disturbed sleep pattern had higher ESS scores (10.3±4.1 vs 5.9±2.9, p=0.01).
DISCUSSION
This prospective descriptive study reports that high-risk behaviors that impact psychosomatic well-being are prevalent in professional firefighters, which require environmental and individual-based health promotion interventions. Humans are physiologically programmed to be awake during the day and sleep at night. Prolonged deviation from that pattern may result in adverse effects on performance and health. Almost sixty percent of firefighters in this study met our acceptable criteria for sleep deprivation. Thirty-eight percent of the subsample of firefighters that wore the motionlogger actigraph had also disrupted sleep patterns and reported excessive daytime sleepiness. Individuals differ in their ability to tolerate night work, adjust to shift work and sleep deprivation. For example, after a single night of work (acute sleep deprivation), half of adults meet performance expectations, a third demonstrate moderate impairments, and the remaining individuals have marked decrement in performance [25]. A person’s ability to tolerate night work may vary over time, unrelated to any identifiable factor. Laboratory experiments on chronic sleep deprivation have demonstrated that cognitive deficits accumulate to severe levels over time without full awareness by the affected individual [26]. Chronic sleep deprivation reduces the ability to think clearly, handle complex mental tasks, solve problems and form new memories [5]. Firefighters, most at risk for chronic sleep deprivation, must be educated about their need for and maximize their ability to achieve adequate restorative sleep. Identifying workers at higher risk for coping with extended work shifts, such as those with undiagnosed sleep disorders (i.e. obstructive sleep apnea) is a beginning. In the meantime, a stop gap from the sleep lab involves educating firefighters about the judicious use of caffeine as a stimulant and a 10 minute nap that can improve subjective sleepiness, fatigue, vigor, and cognitive performance [27].
Research exploring stress and depression among firefighters has received little attention and is therefore lacking in nursing and health related literature. As an initial step to increase knowledge and understanding regarding the mental health care needs of firefighters, it was important to explore stress and depressive symptoms in this particular population to help health care providers plan and implement early interventions aimed at preventing adverse physical and psychosocial health-related events. While the prevalence of depression and hazardous drinking were relatively low in this sample, statistically significant correlations were found for depressive symptoms, sleep problems, and hazardous drinking; albeit not strong correlations (r< 0.60). Importantly, critical firefighter duties may be compromised if firefighters suffer from by even one of these problems, let alone all three. Alcohol-use disorders are associated with depressive episodes, severe anxiety, insomnia, suicide, and abuse of other drugs; continued heavy alcohol use also shortens the onset of heart disease, stroke, cancers, and liver cirrhosis, by affecting the cardiovascular, gastrointestinal, and immune systems [28]. Identification of this at-risk group of firefighters and intervening to address these triune problems is critical given the health and safety consequences.
Firefighters in this study reported higher rates of alcohol use compared to what has been previously described in the literature (80% used alcohol with average of >10 drinks/wk compared to only 62% with average ~5 drinks/wk) [29]. For most adults, moderate alcohol (up to two drinks per day for men and one drink per day for women) causes few problems, yet drinking in any amount may be contraindicated for engaging in activities that require alertness and skill (such as firefighting). There is evidence that regular moderate drinking reduces performance and reaction time, with the potential to increase accident risk and desynchronize circadian rhythms [30]. Additionally, the comorbid use of cigarettes and alcohol also constitutes serious health risks. In this study, 17.7% reported that they currently smoked an average of 1.06 packs per day. Interestingly, there was a discrepancy on how many firefighters self reported as smokers (11.4%) versus reporting smoking a cigarette over the two weeks in the TLFB survey (20%). In other words, although some firefighters actually did smoke cigarettes, they did not self identify as smokers, a phenomenon that reflects improper perception of high-risk health behaviors which demonstrate the appropriateness of education and awareness in this population.
Despite the need for further psychometric testing, the results from the initial administration of the Spirituality in Everyday Life (SEL) are promising. The SEL assessed how frequently firefighters engaged in activities related to feeling supported by others, thinking about relationships with others, feeling a sense of belongingness, thinking about bonds with others, showing support for others, and being involved with others. The large proportion of the sample (96%) with high scores for social bonding supports the concept of brotherhood among firefighters [17]. The United States military has recognized that a soldier's spiritual fitness is a crucial element in the total force fitness of service members [31]. As with firefighters, the solidarity of the military platoon is essential for the safety and welfare of fellow soldiers. It is important to note that among the firefighters who participated in this study, feeling a low level of social bonding and connection was correlated with poor mental well-being. These findings suggest that social bonding, belongingness, and connection may impact firefighter’s physical and mental well-being and overall quality of life. Qualitative research is lacking regarding how firefighters define brotherhood, sense of belonging, and connection, and how these principles can promote physical, mental, emotional, and social well-being among professional firefighters. Firefighters with poor mental well-being and poor social bonding deserve particular attention as they may place themselves and others at risk in the line of duty. Educational programs should be provided for fire departments to assist them in identifying signs of mental distress and distancing from the social bonds of the brotherhood.
CONCLUSION
This study adds to the understanding of the prevalence of modifiable risk factors among an urban brotherhood of firefighters. High-risk health behaviors that impact psychosomatic well-being are prevalent in professional firefighters, which require environmental and individual-based health promotion interventions. The inter-correlation relationships between such behaviors need to be explored in further details. Sleep patterns are disrupted probably because of the duration of the shifts and unpredictability of the emergency calls. Substance use, whether alcohol, nicotine, or caffeine may provide relief from the physical and mental demands of the job, or may be an acceptable norm of the social bonding. Finally, little has been studied regarding the significance of brotherhood among firefighters as it relates to social bonding and connection. Building on the possibility that social bonding may be a protective factor, health promotion and intervention programs could be implemented to help fire departments take a more active role in helping firefighters improve their health.
Acknowledgments
Supported by a Grant from the National Institutes of Health, R21 NR-011077 (MGC)
References
- 1.Astorino TA, Roberson DW. Efficacy of Acute Caffeine Ingestion for Short-term High-Intensity Exercise Performance: A Systematic Review. The Journal of Strength & Conditioning Research. 2010;24(1):257–265. doi: 10.1519/JSC.0b013e3181c1f88a. [DOI] [PubMed] [Google Scholar]
- 2.Lusa S, et al. Perceived physical work capacity, stress, sleep disturbance and occupational accidents among firefighters working during a strike. Work and Stress. 2002;16(3):264–274. [Google Scholar]
- 3.Paley MJ, Price JM, Tepas DI. The impact of a change in rotating shift schedules: A comparison of the effects of 8, 10 and 14 h work shifts. International Journal of Industrial Ergonomics. 1998;21(3–4):293–305. [Google Scholar]
- 4.Paley MJ, Tepas DI. Fatigue and the Shiftworker: Firefighters Working on a Rotating Shift Schedule. Human Factors: The Journal of the Human Factors and Ergonomics Society. 1994;36:269–284. doi: 10.1177/001872089403600208. [DOI] [PubMed] [Google Scholar]
- 5.Elliot DL, Kuehl KS. The effects of sleep deprivation on fire fighters and EMS responders : final report. International Association of Fire Chiefs; 2007. [Google Scholar]
- 6.Fullerton CS, Ursano RJ, Wang L. Acute Stress Disorder, Posttraumatic Stress Disorder, and Depression in Disaster or Rescue Workers. Am J Psychiatry. 2004;161(8):1370–1376. doi: 10.1176/appi.ajp.161.8.1370. [DOI] [PubMed] [Google Scholar]
- 7.Regehr C, et al. Social support, self-efficacy and trauma in new recruits and experienced firefighters. Stress and Health. 2003;19(4):189–193. [Google Scholar]
- 8.Saijo Y, Ueno T, Hashimoto Y. Twenty-four-hour shift work, depressive symptoms, and job dissatisfaction among Japanese firefighters. American Journal of Industrial Medicine. 2008;51(5):380–391. doi: 10.1002/ajim.20571. [DOI] [PubMed] [Google Scholar]
- 9.Lichtman JH, et al. Depression and Coronary Heart Disease: Recommendations for Screening, Referral, and Treatment: A Science Advisory From the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation. 2008;118(17):1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 10.Kales SN, et al. Emergency duties and deaths from heart disease among firefighters in the United States. New England Journal of Medicine. 2007;356(12):1207–15. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- 11.Kales SN, et al. Firefighters and on-duty deaths from coronary heart disease: a case control study. Environmental Health Perspectives. 2003;2(1):14. doi: 10.1186/1476-069X-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pompili M, et al. Suicidal Behavior and Alcohol Abuse. International Journal of Environmental Research and Public Health. 2010;7:1392–1431. doi: 10.3390/ijerph7041392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review. 2000;20(2):149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- 14.Rosenquest JN, et al. The spread of alcohol consumption in a large social network. Annals of Internal Medicine. 2010;152(7):426–433. doi: 10.1059/0003-4819-152-7-201004060-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fear NT, et al. Patterns of drinking in the UK Armed Forces. Addiction. 2007;102(11):1749–1759. doi: 10.1111/j.1360-0443.2007.01978.x. [DOI] [PubMed] [Google Scholar]
- 16.Colrain IM, Trinder J, Swan GE. The impact of smoking cessation on objective and subjective markers of sleep: Review, synthesis, and recommendations. Nicotine and Tobacco Research. 2004;6(6):913–925. doi: 10.1080/14622200412331324938. [DOI] [PubMed] [Google Scholar]
- 17.Crosby F. The Real Meaning of Brotherhood. Fire Engineering. 2007 Retrieved on January 16, 2011 from: http://www.fireengineering.com/index/articles.
- 18.Carey MG, et al. Characteristics of the Standard 12-lead Holter ECG in Professional Firefighters. Computing in Cardiology. 2011 in press. [Google Scholar]
- 19.Janet SC, Michael AA. Psychometric evaluation of the pittsburgh sleep quality index. Journal of psychosomatic research. 1998;45(1):5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. [Google Scholar]
- 21.Sobell LC, et al. Reliability of alcohol abusers' self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17(2):157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- 22.Sessanna L, Finnell D, Jezewski MA. Spirituality in Nursing and Health-Related Literature. Journal of Holistic Nursing. 2007;25(4):252–262. doi: 10.1177/0898010107303890. [DOI] [PubMed] [Google Scholar]
- 23.Ware J, Kosinski M, Keller S. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Marmol F. Correlation theory of spuriously related higher order integrated processes. Economics Letters. 1996;50(2):169–173. [Google Scholar]
- 25.Dinges D. Probing the limits of functional capacity: The effects of sleep loss on short- duration tasks. In: Broughton RB, Ogilvie R, editors. Sleep, Arousal and Performance. Birkhauser-Boston, Inc; 1992. pp. 176–188. [Google Scholar]
- 26.Durmer JS, Dinges DF. Neurocognitive Consequences of Sleep Deprivation. Semin Neurol. 2005;25(01):117, 129. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 27.Brooks A, Lack L. A brief afternoon nap following nocturnal sleep restriction: which nap duration is most recuperative? Sleep. 2006;29(6):831–40. doi: 10.1093/sleep/29.6.831. [DOI] [PubMed] [Google Scholar]
- 28.Schuckit M. Alcohol-use disorders. Lancet. 2009;373:492–501. doi: 10.1016/S0140-6736(09)60009-X. [DOI] [PubMed] [Google Scholar]
- 29.Scanlon P, Ablah E. Self-Reported Cardiac Risks and Interest in Risk Modification Among Volunteer Firefighters: A Survey-Based Study. J Am Osteopath Assoc. 2008;108(12):694–698. [PubMed] [Google Scholar]
- 30.Reinberg A, et al. Habitual Moderate Alcohol Consumption Desynchronizes Circadian Physiologic Rhythm and Affects Reaction-Time Performance. Chronobiology International. 2010;27(9–10):1930–1942. doi: 10.3109/07420528.2010.515763. [DOI] [PubMed] [Google Scholar]
- 31.Hufford DJ, Fritts MJ, Rhodes JE. Spiritual Fitness. Military Medicine. 2010;175:73–87. [Google Scholar]