Abstract
Background
This study aimed to investigate the association of diabetes duration with self-reported coronary heart disease (CHD) in Korea.
Methods
Among data from 34,145 persons compiled in the third Korean National Health and Nutrition Examination Survey in 2005, laboratory test and nutritional survey data from 5,531 persons were examined. The participants were asked to recall a physician's diagnosis of CHD (angina or myocardial infarction).
Results
Age- and sex-adjusted relative risk for CHD was 1.51 (95% confidence interval [CI], 0.64 to 3.59; not significant) for diabetes with duration of <1 year, 2.27 (95% CI, 1.14 to 4.54; P=0.020) for diabetes with a duration of 1 to 5 years, and 3.29 (95% CI, 1.78 to 6.08; P<0.001) for diabetes with a duration >5 years, compared with non-diabetes as a control. Even after adjusting for age, sex, current smoking status, waist circumference, hypertension, triglycerides, high density lipoprotein cholesterol, and fasting plasma glucose, relative risk for CHD was 2.87 (95% CI, 1.01 to 8.11; P=0.047) in diabetes with a duration of 6 to 10 years and 4.07 (95% CI, 1.73 to 9.63; P=0.001) in diabetes with duration of >10 years with non-diabetes as a control.
Conclusion
CHD prevalence increased with an increase in diabetes duration in Korean men and women. Recently detected diabetes (duration <1 year) was not significantly associated with CHD prevalence compared to non-diabetes. However, diabetes of a duration of >5 years was associated with an increase in CHD compared to non-diabetics after adjusting for several CHD risk factors.
Keywords: Coronary disease, Diabetes mellitus, Duration
INTRODUCTION
Cardiovascular disease (CVD) is well-known as a leading cause of death in patients with type 2 diabetes mellitus (T2DM) [1]. T2DM is associated with a 2-fold increase in the risk for CVD [2-4]. Similar to patterns seen in Western countries, coronary artery disease (CAD) is very prevalent in Koreans with T2DM. The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus performed a nationwide survey regarding the status of glycemic control and diabetic complications in 2006. The prevalence of CAD, including angina, myocardial infarction (MI), coronary artery bypass graft, and primary intervention was 8.7% in diabetic patients [5].
In several studies, diabetes without previous coronary heart disease (CHD) showed equivalent risk for future development of CHD when compared to non-diabetes with established CHD, supporting the view that diabetes is a coronary risk equivalent to previous history of CHD [6-9]. However, a recent meta-analysis established that patients with diabetes are at lower risk of developing total CHD events compared with non-diabetics with established CHD, indicating that diabetes is not a coronary risk equivalent [10]. Diabetes duration could be an important determinant for CHD in T2DM, as a longer duration of diabetes is associated with an increased risk of CVD [11-15].
Despite the rapidly growing prevalence of diabetes in Korea and the importance of CHD in the management of diabetes, there have been no reports regarding the association of the duration of diabetes with CHD in the general Korean population. Therefore, we investigated this issue using data obtained in a nationwide representative sample from the third Korea National Health and Nutrition Examination Survey (KNHANES III).
METHODS
Study population
This study was based on data obtained from the KNHANES III among non-institutionalized civilians in the Republic of Korea. The survey, which was conducted by the Korean Ministry of Health and Welfare in 2005, was a nationwide representative study using a stratified and multistage probability sampling design for the selection of household units. The survey consisted of health interview, health behavior, health examination, and nutrition components. A total of 34,145 individuals from these sampling frames were included in the health interview survey. Among them, 5,531 persons aged 18 to 99 years were identified as participants, and participated in laboratory tests and a nutritional survey.
Health examination survey and laboratory test
Trained interviewers visited each participant's dwelling and administered a standardized questionnaire on smoking and regular exercise. A dietary recall method was used to collect data on food items consumed by participants during the past 24 hours. The participants were also asked to recall a physician's diagnosis of CHD (angina or MI). Height and weight were obtained using standardized techniques and equipment. Height was measured to the nearest 0.1 cm using a portable standiometer (Seriter, Bismarck, ND, USA). Weight was measured to the nearest 0.1 kg using a Giant-150N calibrated balance-beam scale (Hana, Seoul, Korea). Body mass index (BMI) was calculated by dividing weight by height squared (kg/m2). Waist circumference (WC) was measured on standing participants with a soft tape midway between the lowest rib and the iliac crest. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured by standard methods using a sphygmomanometer with the patient in a sitting position. Three blood pressure measurements were made at 5-minute intervals and the average of the second and third measurements was used in the analysis. Blood samples were collected in the morning after fasting for at least 8 hours. Fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG), and high density lipoprotein cholesterol (HDL-C) levels were measured in a central and certified laboratory, using an Advia 1650 (Siemens, Tarrytown, NY, USA). Low density lipoprotein cholesterol (LDL-C) was estimated indirectly using the Friedwald formula: LDL-C=TC-[HDL-C+(TG/5)], for subjects with TG levels <400 mg/dL.
Statistical analyses
Data are presented as mean±standard deviation or percent. Statistical analysis was performed using SPSS for Windows (SPSS, Chicago, IL, USA). ANCOVA was used to estimate clinical and biochemical characteristics and the prevalence of CHD according to the presence of diabetes after adjusting for age, current smoking, WC, hypertension, TG, and HDL-C in each sex (Tables 1 and 2). ANCOVA was done for comparison of CHD according to diabetes duration in each sex (Table 3). Logistic regression analyses were done for CHD with age, sex, current smoking, WC, hypertension, HDL-C, TG, FPG, and duration of diabetes as covariates (Table 4). Statistical significance was defined as P<0.05.
Table 1.
Age and age-adjusted clinical characteristics of the study population of adult Korean men (n=2,368)
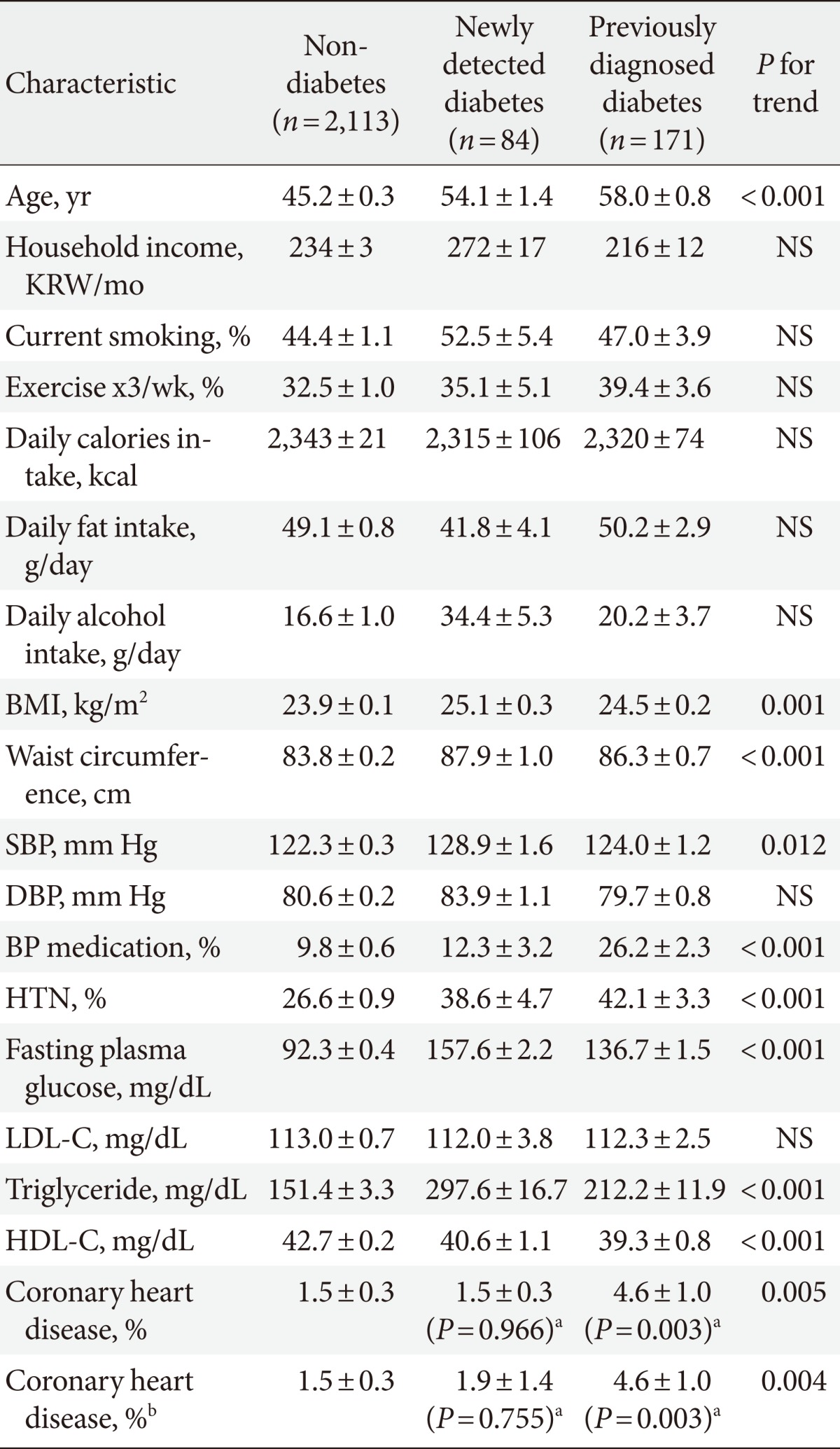
Values are presented as mean or %±SEM.
NS, not significant; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; BP, blood pressure; HTN, hypertension (current antihypertensive medication or SBP ≥140 mm Hg or DBP ≥90 mm Hg); LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
avs. non-diabetes, bPrevalence of coronary heart disease after adjusting for age, current smoking, waist circumference, HTN, triglyceride, and HDL-C.
Table 2.
Age and age-adjusted clinical characteristics of the study population of adult Korean women (n=3,163)
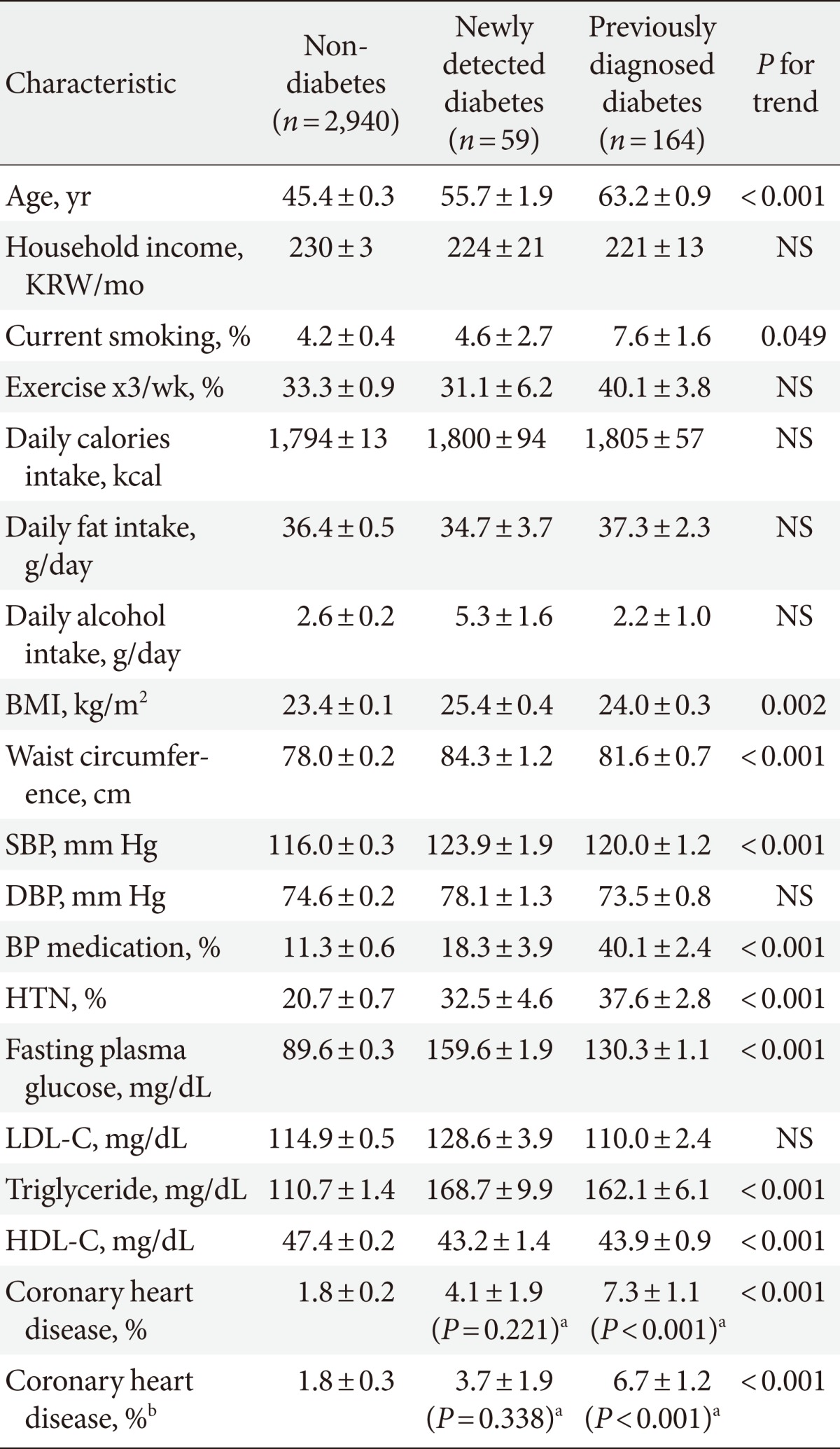
Values are presented as mean or %±SEM.
NS, not significant; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; BP, blood pressure; HTN, hypertension (current antihypertensive medication or SBP ≥140 mm Hg or DBP ≥90 mm Hg); LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
avs. non-diabetes, bPrevalence of coronary heart disease after adjusting for age, current smoking, waist circumference, HTN, triglyceride, and HDL-C.
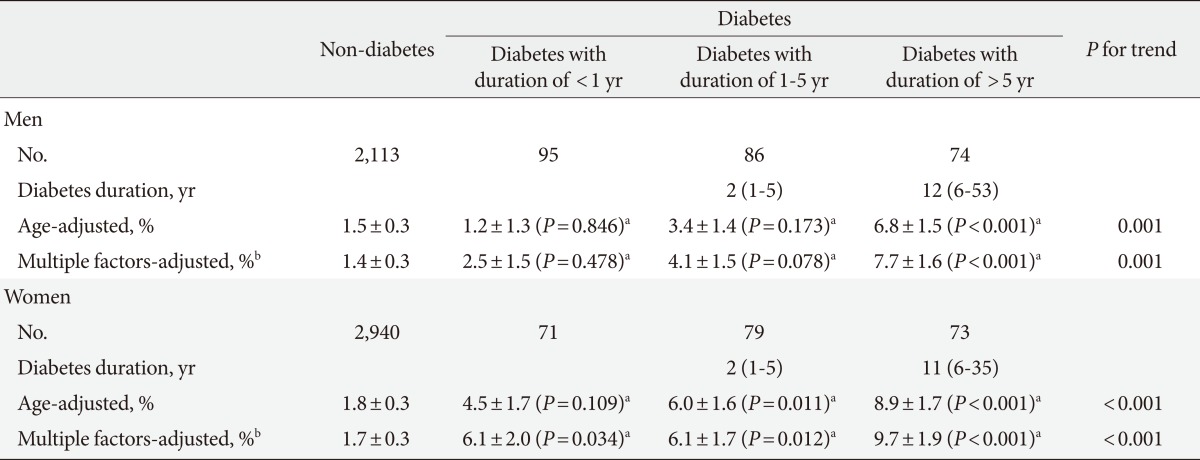
Table 3.
Coronary heart disease according to diabetes duration in each sex
Values are presented as mean or %±SEM.
avs. non-diabetes, bPrevalence of coronary heart disease after adjusting for age, current smoking, waist circumference, hypertension, triglyceride, high density lipoprotein cholesterol, and fasting plasma glucose.
Table 4.
Logistic regression analyses for coronary heart disease with age, sex, current smoking, waist circumference, HTN, HDL-C, triglyceride, fasting plasma glucose, and duration of diabetes as covariates
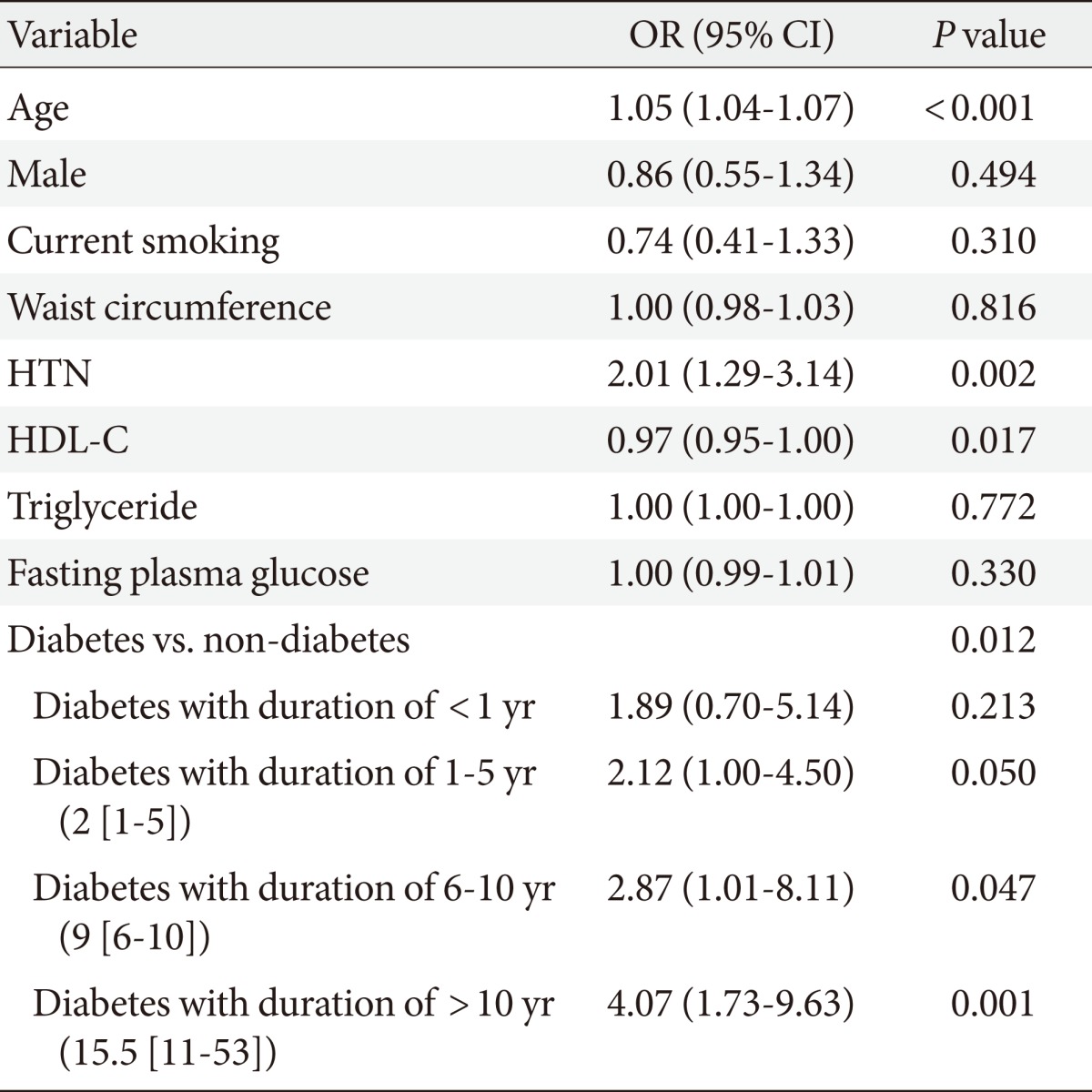
HTN, hypertension (current antihypertensive medication or SBP ≥140 mm Hg or DBP ≥90 mm Hg); HDL-C, high density lipoprotein cholesterol; OR, odds ratio; CI, confidence interval.
Ethics statement
This study was approved by the Institutional Review Board of the Ilsan Paik Hospital (IB-2-1112-047).
RESULTS
The study population ranged in age from 18 to 99 years and included 2,368 men and 3,163 women. Mean age was 45 years (46 years in men, 45 years in women). Mean BMI was 23.7±3.3 kg/m2 (24.0±3.1 kg/m2 in men, 23.5±3.4 kg/m2 in women). Prevalence of diabetes was 8.7% (10.8% in men, 7.2% in women). Prevalence of CHD was 1.9% (1.7% in men, 2.1% in women).
Table 1 presents the age and age-adjusted clinical characteristics of the study population of adult Korean men. The participants were divided into three groups: non-diabetes, newly-detected diabetes, and previously-diagnosed diabetes (diabetes duration, median 5 years [range, 0 to 53 years]). With increased diabetes duration, BMI, WC, BP, FPG, TG, and age all increased. Serum HDL-C decreased according to the extent of the increase in diabetes duration. CHD prevalence was increased according to the extent of increase in diabetes duration. This results was unchanged even after adjusting for age, current smoking, WC, hypertension (HTN), TG, and HDL-C.
Table 2 summarizes the findings concerning age and age-adjusted clinical characteristics of adult Korean women in the study population. The participants were divided into the aforementioned three groups (diabetes duration, 5 years [range, 0 to 35 years]). With increased diabetes duration, BMI, WC, BP, FPG, TG, age, and proportion of current smoking were in creased. CHD prevalence showed an increasing trend according to increased diabetes duration. After adjusting for several CHD risk factors, this increasing CHD trend was unchanged. There was no difference in self-reported CHD prevalence between non-diabetes and newly-detected diabetes by gender. However, the prevalence of self-reported CHD in previously-diagnosed diabetes was significantly higher compared to that in non-diabetes after adjusting for several risk factors (Tables 1 and 2).
Table 3 summarizes the CHD data according to diabetes duration in each sex. The participants were arbitrarily divided according to diabetes duration (non-diabetes and duration of <1 year, 1 to 5 years, and >5 years) to allow similar numbers in each diabetes group. After adjusting for age and several CHD risk factors, CHD showed an increasing trend according to diabetes duration in men. Diabetes of a duration of <1 year or 1 to 5 years did not differ in CHD prevalence compared to non-diabetes. However, CHD prevalence with diabetes of duration of >5 years was significantly higher than with non-diabetes after adjusting for several risk factors (7.7±1.6% vs. 1.4±0.3%, P<0.001). Women also presented an increasing trend in CHD according to diabetes duration. There was no difference in CHD prevalence between non-diabetes and diabetes of a duration of <1 year. However, CHD prevalence with diabetes of a duration of >5 years was significantly higher than that of non-diabetes after adjusting for several risk factors (9.7±1.9% vs. 1.7±0.3%, P<0.001). Contrary to the findings regarding men, women with diabetes of <1 year or 1 to 5 years in duration showed a significantly higher prevalence of CHD compared to those of non-diabetes after adjusting for several risk factors.
After adjusting for age and sex, logistic regression analysis showed that the relative risk for CHD was 1.51 (95% confidence interval [CI], 0.64 to 3.59; not significant) in diabetes with a duration of <1 year, 2.27 (95% CI, 1.14 to 4.54; P=0.020) in diabetes with a duration 1 to 5 years, and 3.29 (95% CI, 1.78 to 6.08; P<0.001) in diabetes with a duration >5 years, compared with non-diabetes as a control.
Table 4 summarizes the findings of logistic regression analyses for CHD with age, sex, current smoking, WC, HTN, HDL-C, TG, FPG, and duration of diabetes as covariates. After adjusting for all these factors, relative risk for CHD was 2.87 (95% CI, 1.01 to 8.11; P=0.047) in diabetes with a duration of 6 to 10 years and 4.07 (95% CI, 1.73 to 9.63; P=0.001) in diabetes with duration of >10 years with non-diabetes as a control. After adjusting for several parameters in addition to age and sex, participants with a diabetes duration of 1 to 5 years did not show a significant difference in CHD compared to non-diabetes.
DISCUSSION
The principal finding of the present study is that the prevalence of CHD increased with an increase in diabetes duration in Korean men and women. In particular, diabetes of a duration of 6 to 10 years showed about a 2.9-fold increase of CHD and diabetes with >10 years of duration showed about a 4.1-fold increase compared to non-diabetes, even after adjusting for several CHD risk factors. As far as we know, this is the first study reporting the association between diabetes duration and a risk of CHD in the general Korean population.
T2DM is associated with an increased risk of CVD [2-4]. It has been suggested that people with diabetes without a prior MI have a similar risk of CHD to those without diabetes who have had a MI [4]. Various studies from different population cohorts have provided varying conclusions regarding the validity of the concept of coronary risk equivalent in patients with diabetes [6-9,16-19], with the results of some studies supporting coronary risk equivalent [6-9], while others did not [16-19]. In a recent meta-analysis [10], patients with diabetes were at a lower risk of developing total CHD events compared with patients without diabetes with established CHD, indicating that diabetes is not a coronary risk equivalent. Due to the limitation of a cross-sectional study design, we could not examine this issue. However, the lack of a difference in self-reported CHD between non-diabetes and recently-detected diabetes supports the suggestion that the presence of diabetes itself, irrespective of severity or duration of diabetes, may not be an equivalent CHD risk factor when compared to a history of previous CHD in the Korean population.
In most studies to have examined the issue, diabetes duration was found to be associated with an increased risk of CVD [11-15,20,21]. Diabetes is associated with increases in traditional risk factors for CVD, including hypertension and dyslipidemia, increased oxidative stress, increased tissue glycosylation, and platelet and fibrinolytic disorders that can lead to a procoagulant state [22,23]. After adjusting for age, sex, and CHD risk factors, the risk of CHD found by the Framingham heart study was 1.38 times higher for each 10-year increase in the duration of diabetes (95% CI, 0.99 to 1.92) [20]. After adjusting for age, smoking, social class, BMI, physical activity, and alcohol intake, the relative risk of major CHD events in a British regional heart study was 1.67 (95% CI, 1.01 to 2.75) in participants with <7 years diabetes duration, 2.65 (95% CI, 1.31 to 5.35) in participants with 7 to 12 years diabetes duration, and 2.67 (95% CI, 1.46 to 4.88) in participants with >12 years diabetes duration as compared to non-diabetes (P for trend <0.0001) [21]. According to a United States-based study regarding the impact of diabetes mellitus and prior MI [11], when compared with non-diabetic men, patients with diabetes diagnosed ≤5 years previously had a relative risk of 1.48 (95% CI, 1.27 to 1.72) and those with a diagnosis exceeding 26 years had a relative risk of 1.91 (95% CI, 1.43 to 2.55). In this study, we observed an increase in self-reported CHD with a longer duration of diabetes. This was especially true in participants with the longest duration of diabetes (>10 years; median, 15.5 years) with an approximately 4.1-fold increase of CHD compared to non-diabetes, even after adjusting for several CHD risk factors. Despite the limitations of this study, the data strongly suggests that a longer duration of diabetes markedly increases the risk of CHD in the general Korean population, irrespective of other CHD risk factors.
The association of diabetes duration with severity of CAD has been reported previously. A positive significant correlation between CAD severity (Gensini score) and duration of diabetes mellitus (r=0.362, P=0.004) has been reported [24]. These factors had a positive linear relationship with the Gensini score, suggesting that as the duration of diabetes increases, the severity of CAD will increase with multiple and tighter lesions, especially if the diabetes is poorly controlled. A Korean study [25] reported the relationship between coronary arterial lesion on coronary angiogram and clinical CHD risk factors. The relative risk of CHD in participants with >10 years diabetes duration was 2.6 (95% CI, 1.4 to 5.1; P=0.003), as compared to participants with ≤10 years diabetes duration.
Presently, the prevalence of CHD according to increased diabetes duration was markedly increased in women compared to men. Traditional CHD risk factors were more prevalent in men. A study regarding gender difference and the effect of diabetes duration on CHD mortality was previously done using NHANES data [8]. After adjusting for age, race, smoking, HTN, serum cholesterol level, and BMI, the hazard ratio of fatal CHD was 1.5 (95% CI, 0.9 to 2.5) for a diabetes duration <0 years and 4.8 (95% CI, 3.0 to 7.8) for a diabetes duration ≥10 years in women. In men, the hazard ratio of fatal CHD was 2.0 (95% CI, 0.9 to 2.5) for a diabetes duration of <10 years, and 2.6 (95% CI, 3.0 to 7.8) for a diabetes duration of ≥10 years. The reason for the markedly increased CHD with increased diabetes duration in women is not clear. Several reports have suggested some possible explanations [26-30]. The first possibility is that CHD risk factors such as HTN and dyslipidemia could be more prominent in women than in men [26-29]. Another possibility is that diabetes may alter estrogen-related protective mechanisms [30].
A limitation of this study was that the history of CHD was not obtained from the hospital records, but was based on the questionnaire that required recall by participants of a physician's diagnosis of CHD (angina or MI). Due to the possibility of recall bias and the limitation of the cross-sectional study design, we could not confirm the results of this study. Therefore, another longitudinal study is warranted. Secondly, the reported duration of diabetes might be underestimated because the actual onset of diabetes frequently precedes clinical diagnosis by several years. Although the strength of our study was its nationally representative data, there could be some limitations in terms of generalization of these results to general the Korean population, because we did not account for the primary sampling units, stratification, and sampling weights of the KNHANES.
In conclusion, as diabetes duration increases, the prevalence of self-reported CHD increased in Korean men and women. Recently-detected diabetes was not associated with a difference in self-reported CHD prevalence compared to non-diabetes. However, diabetes with duration of 6 to 10 years showed an approximately 2.9-fold increase in self-reported CHD, and diabetes >10 years in duration showed an approximately 4.1-fold increase compared to non-diabetes, even after adjusting for several CHD risk factors. The data suggests that more active surveillance of CHD should be done as the duration of diabetes increases.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Porte D, Sherwin RS, Baron A, Ellenberg M, Rifkin H. Ellenberg and Rifkin's diabetes mellitus: theory and practice. 6th ed. New York: McGraw-Hill; 2003. Chapter 49, Heart disease in patients with diabetes; pp. 823–844. [Google Scholar]
- 2.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- 3.Gu K, Cowie CC, Harris MI. Diabetes and decline in heart disease mortality in US adults. JAMA. 1999;281:1291–1297. doi: 10.1001/jama.281.14.1291. [DOI] [PubMed] [Google Scholar]
- 4.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 5.Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: the committee of the Korean Diabetes Association on the epidemiology of diabetes mellitus. Korean Diabetes J. 2009;33:48–57. [Google Scholar]
- 6.Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Raiha P, Karja-Koskenkari P, Kuulasmaa K, Palomaki P, Mustonen J, Lehtonen A, Arstila M, Vuorenmaa T, Lehto S, Miettinen H, Torppa J, Tuomilehto J, Kesaniemi YA, Pyorala K, Salomaa V. Myocardial infarction in diabetic and non-diabetic persons with and without prior myocardial infarction: the FINAMI Study. Diabetologia. 2005;48:2519–2524. doi: 10.1007/s00125-005-0019-0. [DOI] [PubMed] [Google Scholar]
- 7.Natarajan S, Liao Y, Cao G, Lipsitz SR, McGee DL. Sex differences in risk for coronary heart disease mortality associated with diabetes and established coronary heart disease. Arch Intern Med. 2003;163:1735–1740. doi: 10.1001/archinte.163.14.1735. [DOI] [PubMed] [Google Scholar]
- 8.Natarajan S, Liao Y, Sinha D, Cao G, McGee DL, Lipsitz SR. Sex differences in the effect of diabetes duration on coronary heart disease mortality. Arch Intern Med. 2005;165:430–435. doi: 10.1001/archinte.165.4.430. [DOI] [PubMed] [Google Scholar]
- 9.Hu FB, Stampfer MJ, Solomon CG, Liu S, Willett WC, Speizer FE, Nathan DM, Manson JE. The impact of diabetes mellitus on mortality from all causes and coronary heart disease in women: 20 years of follow-up. Arch Intern Med. 2001;161:1717–1723. doi: 10.1001/archinte.161.14.1717. [DOI] [PubMed] [Google Scholar]
- 10.Bulugahapitiya U, Siyambalapitiya S, Sithole J, Idris I. Is diabetes a coronary risk equivalent? Systematic review and meta-analysis. Diabet Med. 2009;26:142–148. doi: 10.1111/j.1464-5491.2008.02640.x. [DOI] [PubMed] [Google Scholar]
- 11.Cho E, Rimm EB, Stampfer MJ, Willett WC, Hu FB. The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol. 2002;40:954–960. doi: 10.1016/s0735-1097(02)02044-2. [DOI] [PubMed] [Google Scholar]
- 12.Morgan CL, Currie CJ, Stott NC, Smithers M, Butler CC, Peters JR. The prevalence of multiple diabetes-related complications. Diabet Med. 2000;17:146–151. doi: 10.1046/j.1464-5491.2000.00222.x. [DOI] [PubMed] [Google Scholar]
- 13.Brun E, Nelson RG, Bennett PH, Imperatore G, Zoppini G, Verlato G, Muggeo M Verona Diabetes Study. Diabetes duration and cause-specific mortality in the Verona Diabetes Study. Diabetes Care. 2000;23:1119–1123. doi: 10.2337/diacare.23.8.1119. [DOI] [PubMed] [Google Scholar]
- 14.Sievers ML, Nelson RG, Knowler WC, Bennett PH. Impact of NIDDM on mortality and causes of death in Pima Indians. Diabetes Care. 1992;15:1541–1549. doi: 10.2337/diacare.15.11.1541. [DOI] [PubMed] [Google Scholar]
- 15.Nelson RG, Sievers ML, Knowler WC, Swinburn BA, Pettitt DJ, Saad MF, Liebow IM, Howard BV, Bennett PH. Low incidence of fatal coronary heart disease in Pima Indians despite high prevalence of non-insulin-dependent diabetes. Circulation. 1990;81:987–995. doi: 10.1161/01.cir.81.3.987. [DOI] [PubMed] [Google Scholar]
- 16.Evans JM, Wang J, Morris AD. Comparison of cardiovascular risk between patients with type 2 diabetes and those who had had a myocardial infarction: cross sectional and cohort studies. BMJ. 2002;324:939–942. doi: 10.1136/bmj.324.7343.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lotufo PA, Gaziano JM, Chae CU, Ajani UA, Moreno-John G, Buring JE, Manson JE. Diabetes and all-cause and coronary heart disease mortality among US male physicians. Arch Intern Med. 2001;161:242–247. doi: 10.1001/archinte.161.2.242. [DOI] [PubMed] [Google Scholar]
- 18.Vaccaro O, Eberly LE, Neaton JD, Yang L, Riccardi G, Stamler J Multiple Risk Factor Intervention Trial Research Group. Impact of diabetes and previous myocardial infarction on long-term survival: 25-year mortality follow-up of primary screenees of the Multiple Risk Factor Intervention Trial. Arch Intern Med. 2004;164:1438–1443. doi: 10.1001/archinte.164.13.1438. [DOI] [PubMed] [Google Scholar]
- 19.Hu G, Jousilahti P, Qiao Q, Katoh S, Tuomilehto J. Sex differences in cardiovascular and total mortality among diabetic and non-diabetic individuals with or without history of myocardial infarction. Diabetologia. 2005;48:856–861. doi: 10.1007/s00125-005-1730-6. [DOI] [PubMed] [Google Scholar]
- 20.Fox CS, Sullivan L, D'Agostino RB, Sr, Wilson PW. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes Care. 2004;27:704–708. doi: 10.2337/diacare.27.3.704. [DOI] [PubMed] [Google Scholar]
- 21.Wannamethee SG, Shaper AG, Lennon L. Cardiovascular disease incidence and mortality in older men with diabetes and in men with coronary heart disease. Heart. 2004;90:1398–1403. doi: 10.1136/hrt.2003.026104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sowers JR, Lester MA. Diabetes and cardiovascular disease. Diabetes Care. 1999;22(Suppl 3):C14–C20. [PubMed] [Google Scholar]
- 23.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–2581. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- 24.Saleem T, Mohammad KH, Abdel-Fattah MM, Abbasi AH. Association of glycosylated haemoglobin level and diabetes mellitus duration with the severity of coronary artery disease. Diab Vasc Dis Res. 2008;5:184–189. doi: 10.3132/dvdr.2008.030. [DOI] [PubMed] [Google Scholar]
- 25.Choi EK, Park YB, Oh S, Chae IH, Kim CH, Sohn DW, Oh BH, Lee MM, Choi YS. The relationship of coronary arterial lesion with clinical factors in type II diabetes. Korean Circ J. 2002;32:106–117. [Google Scholar]
- 26.Juutilainen A, Kortelainen S, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Gender difference in the impact of type 2 diabetes on coronary heart disease risk. Diabetes Care. 2004;27:2898–2904. doi: 10.2337/diacare.27.12.2898. [DOI] [PubMed] [Google Scholar]
- 27.Howard BV, Cowan LD, Go O, Welty TK, Robbins DC, Lee ET. Adverse effects of diabetes on multiple cardiovascular disease risk factors in women. The Strong Heart Study. Diabetes Care. 1998;21:1258–1265. doi: 10.2337/diacare.21.8.1258. [DOI] [PubMed] [Google Scholar]
- 28.Walden CE, Knopp RH, Wahl PW, Beach KW, Strandness E., Jr Sex differences in the effect of diabetes mellitus on lipoprotein triglyceride and cholesterol concentrations. N Engl J Med. 1984;311:953–959. doi: 10.1056/NEJM198410113111505. [DOI] [PubMed] [Google Scholar]
- 29.Siegel RD, Cupples A, Schaefer EJ, Wilson PW. Lipoproteins, apolipoproteins, and low-density lipoprotein size among diabetics in the Framingham offspring study. Metabolism. 1996;45:1267–1272. doi: 10.1016/s0026-0495(96)90246-2. [DOI] [PubMed] [Google Scholar]
- 30.Steinberg HO, Paradisi G, Cronin J, Crowde K, Hempfling A, Hook G, Baron AD. Type II diabetes abrogates sex differences in endothelial function in premenopausal women. Circulation. 2000;101:2040–2046. doi: 10.1161/01.cir.101.17.2040. [DOI] [PubMed] [Google Scholar]