Abstract
Background
Long-term surveillance comparing satisfaction between the early experience of Nuss procedure vs. Ravitch procedure.
Materials and Methods
A total of 100 patients that underwent surgical correction of a pectus excavatum between 2001 and 2004 and were followed for ≥2 years were included. Surveillance on the degree of satisfaction was performed using five-levels of the Likert scale and self-assessment scoring.
Results
Nuss or Ravitch surgery was performed in 63 and 37 patients, respectively. The Nuss procedure required a shorter operation time and shorter hospital stay than the Ravitch procedure (p<0.001). The surveillance demonstrated that 17.6% of the Nuss group and 35.7% of the Ravitch group were not satisfied with the outcome of the surgery (p=0.072). The most common causes of dissatisfaction were redepression in the Nuss group (n=5) and incomplete correction in the Ravitch group (n=7). The multivariate analysis showed that reoperation and a high postoperative pectus index were significant risk factors for a low satisfaction score.
Conclusion
The Nuss procedure had several advantages over the Ravitch procedure in the immediate postoperative period. However, the long-term satisfaction was determined by a complete correction without recurrence or need for re-intervention rather than by the operation type.
Keywords: Thoracic wall, Minimally invasive surgery, Outcome assessment, Quality of life, Funnel chest
INTRODUCTION
Pectus excavatum is one of the most common congenital chest wall deformities with an incidence of more than one per 1,000 births [1-3]. The degree of the deformity varies among patients. Many patients present with an asymptomatic, deformed sternum that can compress the underlying vital organs including the heart and lungs. Therefore, the correction of a pectus excavatum can improve cardiac and/or pulmonary function [4-7] and furthermore, in terms of the quality of life, the surgery can improve limitations on physical activity and the patients self-image [8,9].
Two types of surgery have been commonly performed for the correction of pectus excavatum, the Ravitch and Nuss procedures. The Ravitch procedure is an open surgical procedure that has been available for a long-period of time; the outcomes of this procedure are well established [10-13]. The Nuss procedure was introduced as a minimally invasive procedure that has a small skin wound compared to the Ravitch procedure [14-16]. There is no consensus on the indications for the use of these procedures. Although it is clear that the Nuss procedure has advantages as a minimally invasive procedure, disadvantages have also been reported in certain clinical situations; these include adult patients and in cases with asymmetrical types of a pectus excavatum [17-19]. Therefore, superiority of one procedure to the other remains controversial.
Most prior studies comparing the Ravitch and Nuss procedures have been performed from the medical perspective. The satisfaction of patients and their parents might be an important indicator of the success of the surgical correction. Therefore, this study was performed using a questionnaire to compare the Ravitch and Nuss procedures to identify common clinical factors associated with dissatisfaction after the repair of a pectus excavatum.
MATERIALS AND METHODS
A comparison of patients that underwent repair of a pectus excavatum during a 4-year period from 2001 to 2004 was performed. The institutional review board of our hospital approved this study. The inclusion criteria were: 1) the patient was less than 18 years of age, 2) underwent repair of a pectus excavatum by the Ravitch or Nuss procedure, 3) did not have any other major cardiac or thoracic surgery, 4) was followed for more than 2 years after the surgery, and 5) had completed bar removal after the Nuss procedure. The morphological indexes were measured during the preoperative period by a chest computed tomography (CT) scan. Calculation of each index was performed by the methods recommended by Fokin et al. [1]. The pectus index, depression index, asymmetry index, flatness index, and sternal torsion angle were measured during the preoperative period. A chest CT scan was not routinely recommended during the postoperative period. The postoperative pectus index was measured by simple chest X-rays. Chest X-rays were performed 2-years after the initial operation in both groups. In the Nuss group the chest X-ray after bar removal was used for the study. Postoperative pectus index was calculated by chest X-ray (posterior-anterior view and lateral view). Measuring method was same as that of CT measuring: the longest distance of lateral dimension and the shortest distance of anterior-posterior dimension.
The techniques used in the Ravitch operation were not changed during the study period. A small submammary skin incision was made and deformed cartilages were resected. A posterior sternal table osteotomy was made at the lower surface of the sternum and the fragments of resected cartilage or rib were carved as a wedge and inserted into the groove of the osteotomy to support distal sternum. For the Nuss procedure, a pectus bar was inserted just underneath the maximal point of the depression. A liberal design for the shape of the Nuss bar was made according to the shape of pectus excavatum, especially for the asymmetrical types. Asymmetrical bar was designed according to the shape of pectus excavatum for even elevation and depression of chest wall. Bar stabilization was performed by the simple suture technique with non-absorbable sutures in the early cases; however a steel wire was used for the later cases. A bar stabilizer was used in selected cases when bar rotation would have been expected in spite of steel wire fixation. Selection of operation type was performed by surgeons' preference. Two surgeons favored Nuss procedure and one surgeon favored Ravitch procedure. However, both procedures were performed by all three surgeons.
Surveillance of the degree of satisfaction was performed using five-levels of the Likert scale from 1 to 5 (e.g., 5=very satisfied, 4=satisfied, 3=neutral, 2=unsatisfied, and 1=very unsatisfied) and self-assessment scoring for the surgical outcome from 0 to 100 points (0 for the worst and 100 for the best result). The causes of dissatisfaction were also questioned and recorded. The questionnaire was administered by a clinical coordinator via telephone interview. Surveillance responses were obtained from the parents of patients. A total of 79 out of 100 candidates participated in the surveillance.
1) Statistical analysis
Continuous variables are expressed as the means±standard deviation. Nominal variables were expressed as numbers and proportions. Comparison between the two different groups was performed by the chi-square test or Student t-test. Univariate and multivariate analysis was performed by linear regression analysis. All factors with a value of <0.10 by univariate analysis were included in the multivariate analysis. Statistical significance was accepted at the p<0.05 level. Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
1) Demographic data
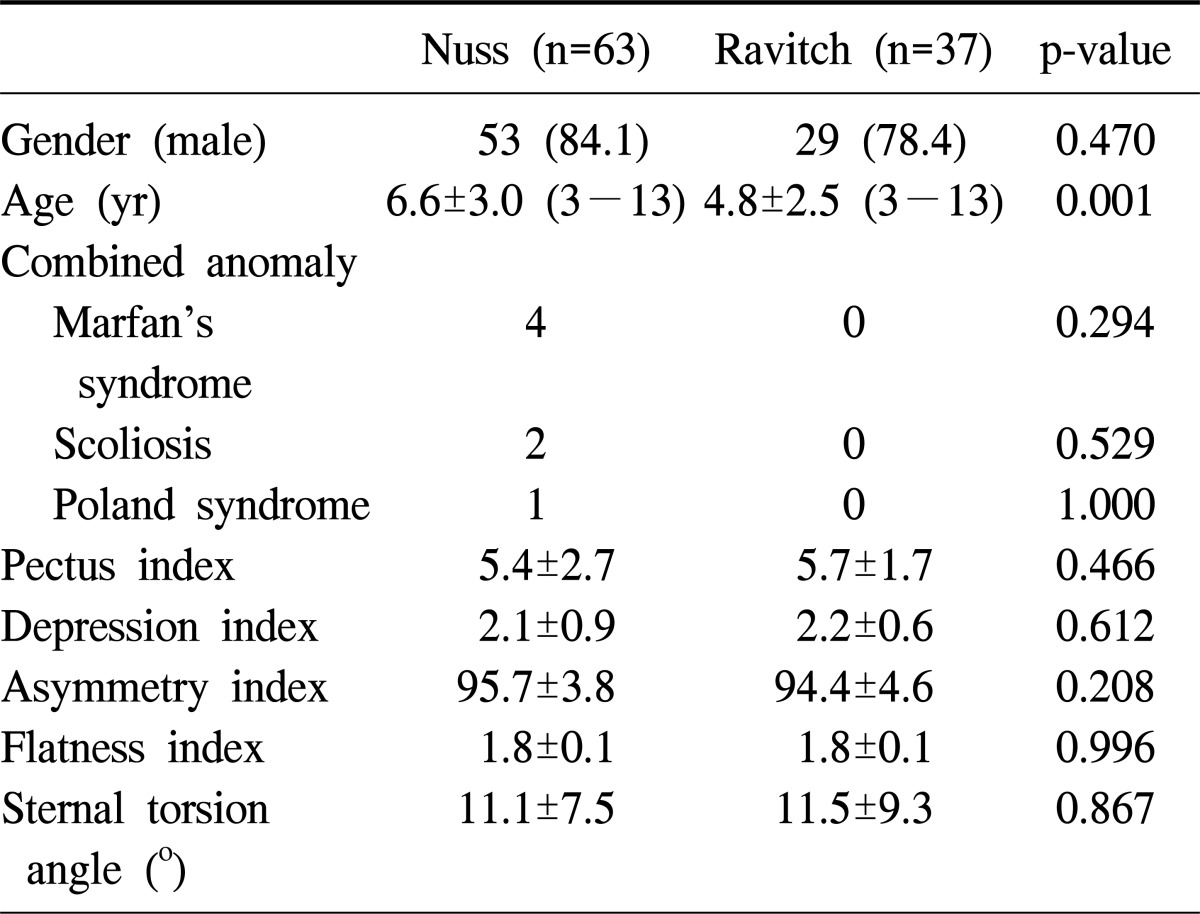
Among 100 patients included in this study, the Nuss and Ravitch procedures were performed in 63 and 37 patients, respectively. The gender ratio did not differ between the two groups. However, the mean age of the patients in the Nuss group was 6.6 years and was higher than that of the Ravitch group (mean, 4.8 years old; p=0.001). Additional anomalies that might have been related to the pectus excavatum were found in seven patients in the Nuss group; however, there were none in the Ravitch group. The pectus index, depression index, asymmetry index, flatness index, and sternal torsion angle were measured in both groups; there were no significant differences in these indexes between the two groups (Table 1).
Table 1.
Demographic data and measured indexes of pectus excavatum
Values are presented as number (%) or mean±standard deviation.
2) Surgical data
In the Nuss group, the double bar technique was used in two patients (3.2%) and a single bar was used in 61 patients (96.8%). Bar stabilizers were used in seven patients (11.1%). In the Ravitch group, a posterior sternal table osteotomy was performed in all patients. The operation time was significantly longer in the Ravitch group (213.8±60.3 minutes in Ravitch group vs. 53.8±19.4 minutes in Nuss group; p<0.001). The length of hospital stay was also significantly longer for the Ravitch group (9.9±5.0 days in Ravitch group vs. 4.4±2.0 days in Nuss group; p<0.001). Early postoperative complications occurred in 11 patients in the Nuss group (17.5%) and four patients in the Ravitch group (10.8%); these differences were not statistically significant. The early complications in Nuss group were pneumothorax (n=6), pleural effusion (n=3), and wound problems (n=2). In the Ravitch group, there were four wound problems (10.8%).
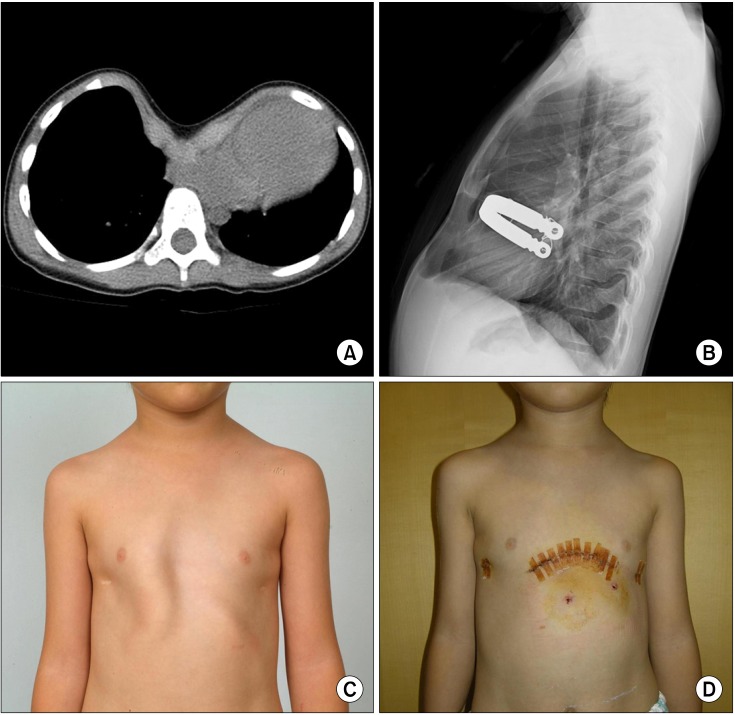
3) Reoperation and postoperative pectus index
Nine patients in the Nuss group (14.2%) and seven patients in the Ravitch group (18.9%) underwent reoperation. In the Nuss group, six patients received reoperation because of a bar displacement and two patients underwent the Ravitch type operation due to residual deformity (Fig. 1). Another patient underwent wound revision due to a wound problem. In the Ravitch group, the most common reason for reoperation was a wound problem (n=6). One patient in the Ravitch group received a redo Ravitch operation due to recurrent pectus excavatum. The postoperative pectus index measured in both groups showed a significant difference. The postoperative pectus index was 2.9±0.7 in the Nuss group and 3.4±1.1 in the Ravitch group; this difference was statistically significant (p=0.01).
Fig. 1.
(A) A 3-year-old boy had severe pectus excavatum with a pectus index of 11.1 on the preoperative chest computed tomography scan. (B) After the Nuss operation the pectus index was improved to 2.5. (C) However, the deformed cartilage was not corrected after the operation. (D) The boy underwent bar removal and a Ravitch type operation (deformed cartilage resection without sternal osteotomy) 2 years after the Nuss operation.
4) Survey of the degree of satisfaction
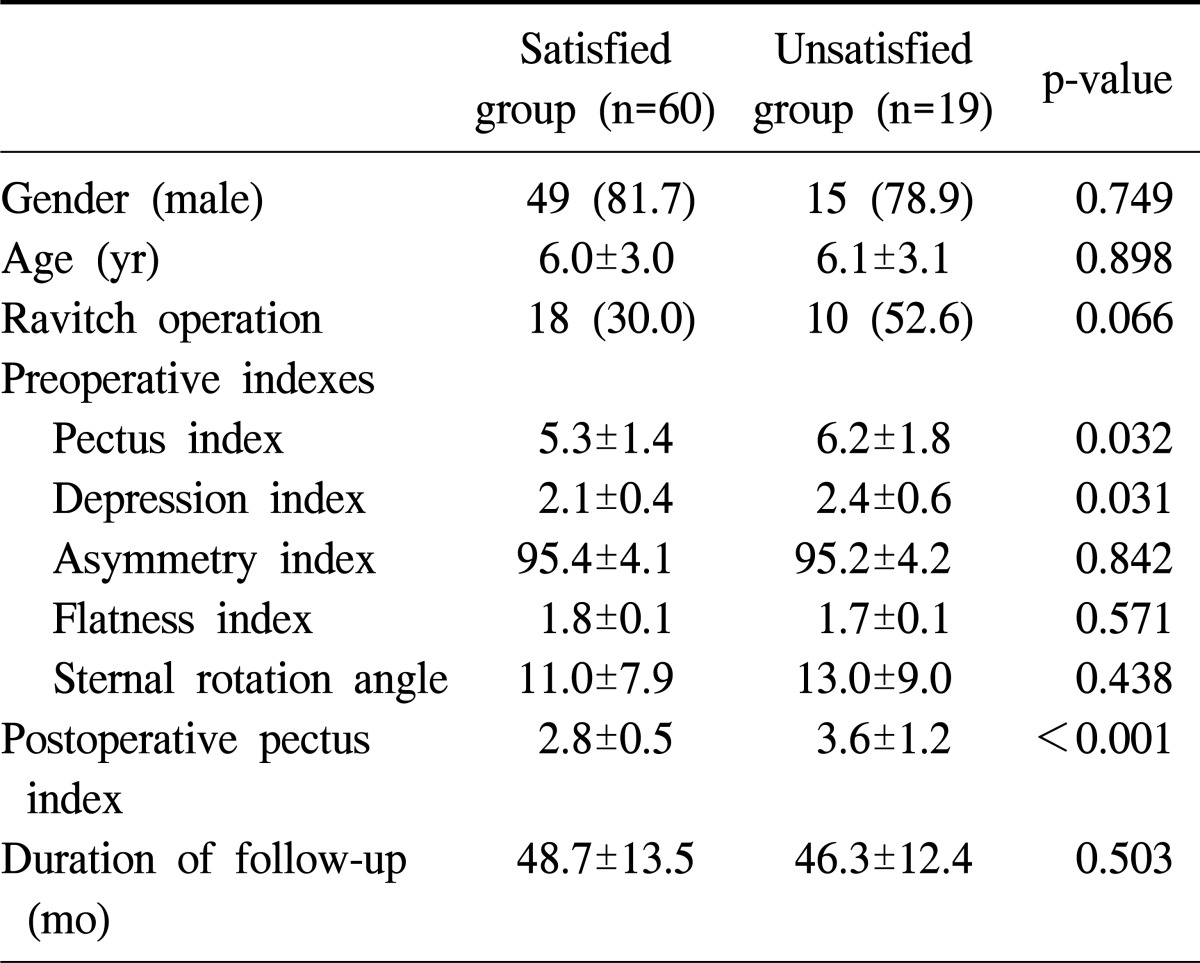
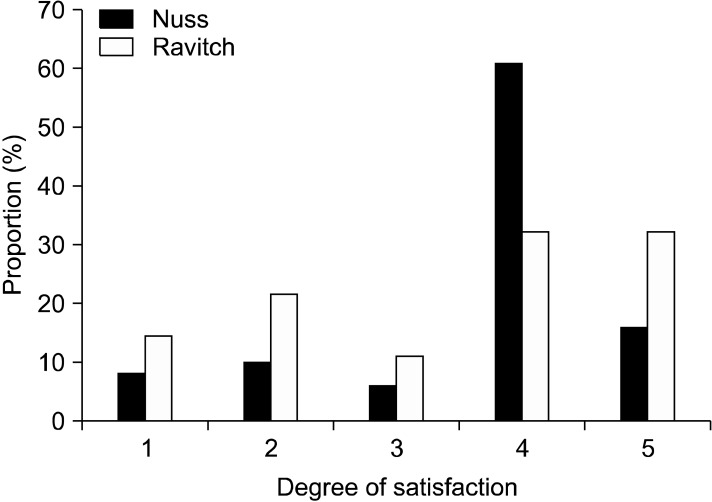
A total of 76 parents of patients participated in the survey. According to the replies on the questionnaire, the satisfied group (replied with grade 4 or more satisfaction on the scale) and the unsatisfied group (had grade 3 or lower on the satisfaction scale) were compared (Table 2). The unsatisfied group included patients with a higher frequency of reoperations, higher preoperative pectus index and depression index, and higher postoperative pectus index compared to the satisfied group. The survey showed that 17.6% of the Nuss group and 35.7% of the Ravitch group were not satisfied with the outcome of the surgery; this difference was not statistically significant (p=0.072) (Fig. 2).
Table 2.
Comparison between satisfied group and unsatisfied group
Values are presented as number (%) or mean±standard deviation.
Fig. 2.
Survey results of satisfaction grade by the Likert scale between the Nuss and Ravitch operation.
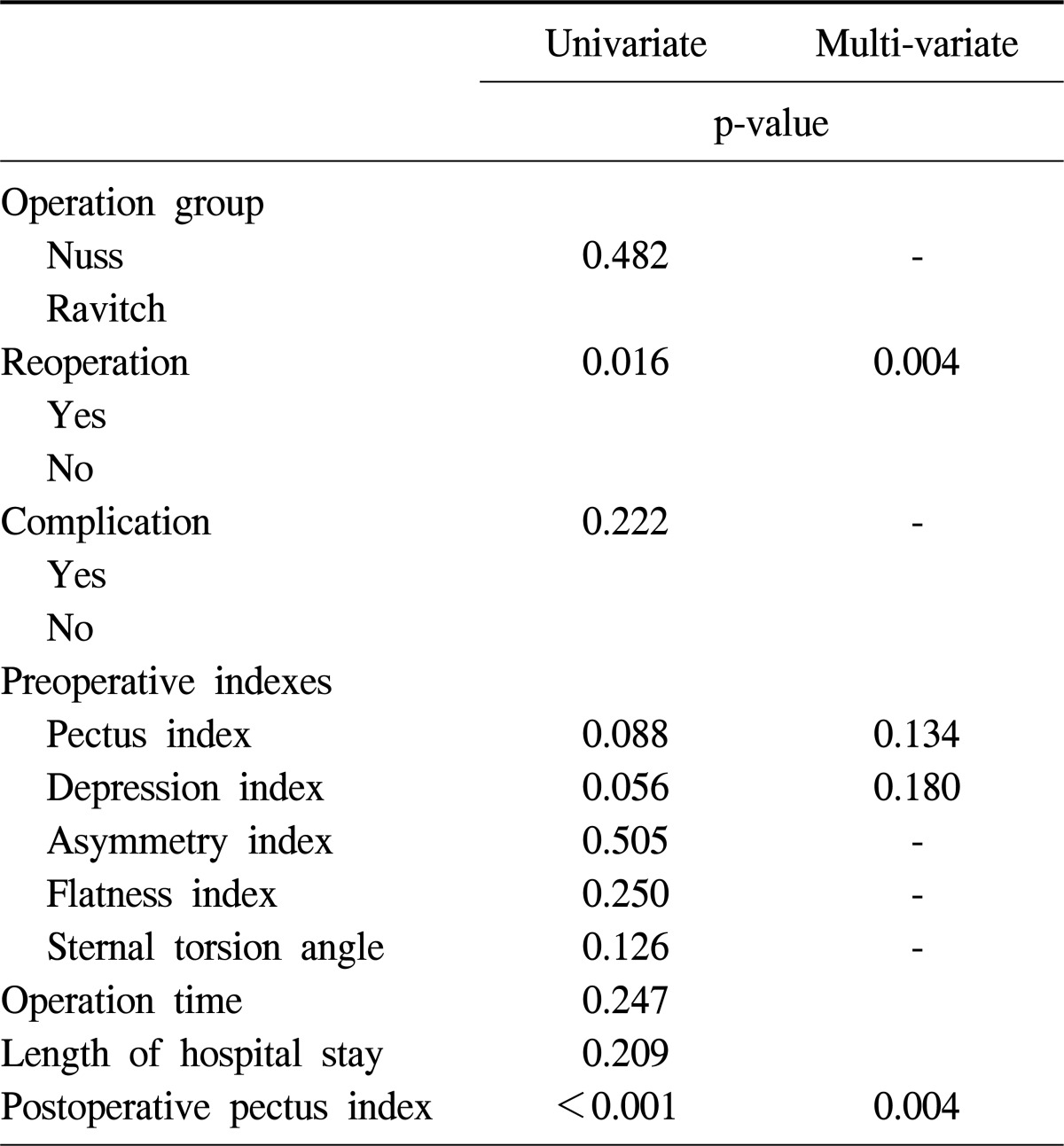
To determine the most important factor associated with patient dissatisfaction, the satisfaction scores were used as a dependent factor on the univariate and multivariate analysis. Four significant clinical factors were identified by the univariate analysis: reoperation, preoperative pectus index, preoperative depression index, and postoperative pectus index. The multivariate analysis with these four factors showed that reoperation (p=0.004; hazard ratio [HR], -4.0; 95% confidence interval [CI], -47.2 to -15.9) and the postoperative pectus index (p=0.004; HR, -4.3; 95% CI, -20.5 to -7.5) were significant risk factors for dissatisfaction (Table 3). The causes of dissatisfaction were recurrence of the depression after bar removal (n=5) (Fig. 3), initial incomplete correction (n=2), and conversion to the Ravitch operation (n=2) in the Nuss group. In the Ravitch group, an incomplete correction (n=7) and an unsatisfactory surgical wound (n=3) were the most common causes of dissatisfaction.
Table 3.
Univariate and multivariate analysis on the satisfaction score
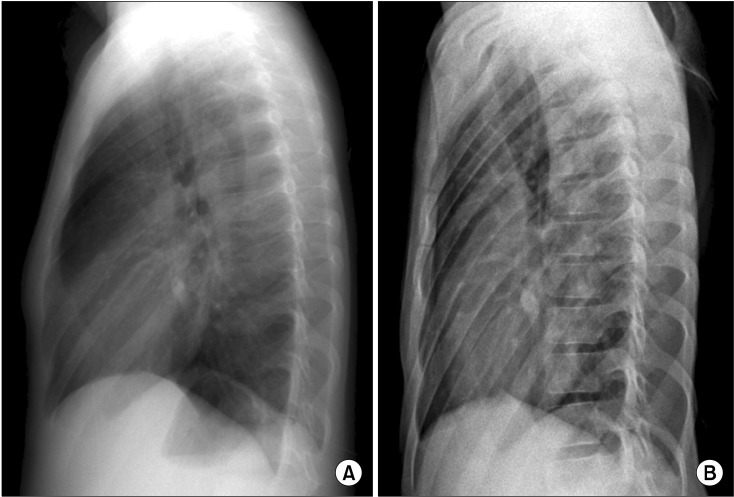
Fig. 3.
Re-depression after Nuss bar removal in a 6-year-old boy. (A) The pectus index just after bar removal was 2.3. (B) However 4 years after bar removal the sternum was depressed again and the pectus index was increased to 3.5.
DISCUSSION
During a 4-year period 100 repairs of pectus excavatum were performed. The Nuss and Ravitch procedures were performed in 63 and 37 patients, respectively. Although the mean age of the patients in the Nuss group was higher than in the Ravitch group, the morphological indexes were not different between the two groups. The early surgical outcomes favored the Nuss group because of the short operation time and short length of hospital stay. For the mid-term satisfaction survey, although the Nuss group demonstrated a trend toward a higher degree of satisfaction, the most important factor associated with late satisfaction was complete correction without recurrence of pectus excavatum rather than the type of operation.
As a minimally invasive surgical procedure, the Nuss operation has several advantages over the Ravitch operation in terms of operation time and length of hospital stay. However, the length of stay also depends on the patient care protocol provided by a hospital and the experience of the surgeon that performed the procedure. Recent studies on the Ravitch operation have reported shorter lengths of hospital stay compared to the prior results of the Ravitch operation [11,12,20]. These findings suggest that the Ravitch operation performed more recently is comparable to the Nuss operation in terms of length of hospital stay. The patients in Ravitch group in this study were managed by conventional methods without any fast-track protocol. Most of patients were discharged more than one week after operation because we tried to check the any delayed wound problems in Ravitch group. Therefore, we don't think that the longer length of stay in Ravitch group does not represent poorer postoperative course.
On the contrary, the complication rate of the Nuss group was higher than the Ravitch group in this study. Coelho et al. [19] reported that complications occurred in 15% of the Ravitch and 45% of the Nuss group; the complication rate was significantly higher in the Nuss group, consistent with the findings of this study. However, most complications were minor and could be managed without any significant residual defect. However the surveillance analysis showed that the early complications, operation time, and length of hospital stay were not related to the satisfaction score; this finding reflects the early results that did not affect the late outcome (contour of repaired pectus deformity or any disability) and was not related to the late satisfaction.
Wound problems were associated with the degree of satisfaction. Wounds and scar problems are major limitations of the Ravitch procedure. Many parents complained of wound problems. Fonkalsrud et al. [12] reported that 9.3% of patients developed hypertrophic scars after the Ravitch operation. In this study, six patients received additional minor surgery because of wound problems during the early and late postoperative period. An unfavorable wound was the most significant complaint in three parents in the Ravitch group; which was a definite disadvantage compared to the Nuss operation. After the introduction of the Nuss operation, we adopted a procedure with a small submammary incision for the Ravitch operation to decrease the size of the wound.
The Nuss procedure, as a minimally invasive operation, has several advantages over the Ravitch method especially with regard to the cosmetics of the surgical wound. However, the Nuss proceudre has problems not present with the Ravitch procedure. Bar displacement is a problem that can complicate the long-term outcome of the Nuss operation. In this study, six patients (9.5%) underwent reoperation because of bar displacement. There were five out of six patients that required additional surgery during the year 2001 when the suture fixation procedure was used. After the introduction of wire and a stabilizer, the frequency of bar displacement decreased dramatically. However, reoperation due to bar displacement continued to be one of the major complications points of dissatisfaction identified by the surveillance. The other problem in the Nuss operation was the inability to remove deformed cartilage. In contrast to the Ravitch operation, the postoperative cartilage contour in the Nuss operation relies on the secondary remodeling of cartilage after sternal lifting. However, in patients with an asymmetrical type of pectus excavatum the length of overgrown cartilage is different between the left and right side [21]; the simple lifting of the sternum can result in asymmetrical protrusion of the cartilage. In this study two patients received the Ravitch type operation after a failed Nuss operation. However, Kelly et al. [22] reported the bar displacement decreased as the surgical techniques evolved from 12% to 1% and excellent anatomical result could be achieved in 95% of patients. Park et al. [23] also reported the decreasing tendency of bar displacement and reoperation recently. They suggested the result of Nuss procedure improved as the experience had been accumulated.
Re-depression after bar removal was also a common complaint in the unsatisfied group. Five parents complained of re-depression in the Nuss group. Reoperation was necessary in two patients in the Nuss group and one patient in the Ravitch group, because of incomplete correction or recurrence of the pectus excavatum. Luu et al. [24] reported that an asymmetrical type and a higher pectus index were related to reoperation in the Nuss group. They suggested that severe pectus excavatum and the asymmetrical type may be better managed by the Ravitch operation. However, Park et al. [16] reported that a specially customized bar can correct the asymmetrical deformity satisfactorily. Therefore, use of the Nuss operation in such patients is controversial.
One of the most important points of dissatisfaction was incomplete correction of the original deformity. In this study, the most important factor related to the long-term satisfaction score was the postoperative pectus index. The preoperative indexes including the pectus index and depression index showed low power for a statistical relationship; however, the overall degree of satisfaction was determined by the postoperative degree of depression not by the preoperative degree of depression. Cartoski et al. [2] reported that an integrated interpretation of the index is necessary for the evaluation of pectus excavatum because no single index can represent all morphologic features of the pectus excavatum. Lawson et al. [25] also pointed out that the pectus index can be affected by the shape of the chest wall regardless of the degree of depression. However, comprehensive indexes in the postoperative period could not be evaluated as in the preoperative period in this study, because we did not perform a chest CT after the operation. The pectus index is a representative index of the degree of depression, which can also be easily measured by chest X-ray. In spite of the limitation of a single index, the chest X-ray can be used to estimate the overall correction of the degree of depression.
There are several limitations in this study. Because the Nuss group in this study is the series of early experience, the result of this study may not reflect the current practice and results of Nuss procedure and learning curve of surgeon might have influenced the overall outcome. Further study on this subject would be necessary for recently performed operations.
CONCLUSION
There was no significant difference in terms of satisfaction degree between the Nuss and Ravitch operation in this study. In this study the results of the Nuss group showed greater satisfaction with the surgical results; however, the difference was not statistically significant. In this study one of the most important factors was the completeness of the correction, which could be objectively confirmed by the difference in the pectus index. Another important factor identified was the need for reoperation. Both surgical methods have limitations; bar associated problems in the Nuss group and wound problems in the Ravitch group. These problems increased the risk for re-intervention and decreased the long-term patient satisfaction. These problems will have to be improved in each procedure to improve patient satisfaction with the outcome of surgery.
Footnotes
This paper was presented at the 46th annual meeting of the Society of Thoracic Surgeons, Fort Lauderdale, Florida, January 24-27, 2010.
References
- 1.Fokin AA, Steuerwald NM, Ahrens WA, Allen KE. Anatomical, histologic, and genetic characteristics of congenital chest wall deformities. Semin Thorac Cardiovasc Surg. 2009;21:44–57. doi: 10.1053/j.semtcvs.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Cartoski MJ, Nuss D, Goretsky MJ, et al. Classification of the dysmorphology of pectus excavatum. J Pediatr Surg. 2006;41:1573–1581. doi: 10.1016/j.jpedsurg.2006.05.055. [DOI] [PubMed] [Google Scholar]
- 3.Koumbourlis AC. Pectus excavatum: pathophysiology and clinical characteristics. Paediatr Respir Rev. 2009;10:3–6. doi: 10.1016/j.prrv.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Coln E, Carrasco J, Coln D. Demonstrating relief of cardiac compression with the Nuss minimally invasive repair for pectus excavatum. J Pediatr Surg. 2006;41:683–686. doi: 10.1016/j.jpedsurg.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Johnson JN, Hartman TK, Pianosi PT, Driscoll DJ. Cardiorespiratory function after operation for pectus excavatum. J Pediatr. 2008;153:359–364. doi: 10.1016/j.jpeds.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 6.Lawson ML, Mellins RB, Tabangin M, et al. Impact of pectus excavatum on pulmonary function before and after repair with the Nuss procedure. J Pediatr Surg. 2005;40:174–180. doi: 10.1016/j.jpedsurg.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 7.Malek MH, Berger DE, Housh TJ, Marelich WD, Coburn JW, Beck TW. Cardiovascular function following surgical repair of pectus excavatum: a metaanalysis. Chest. 2006;130:506–516. doi: 10.1378/chest.130.2.506. [DOI] [PubMed] [Google Scholar]
- 8.Kelly RE, Jr, Cash TF, Shamberger RC, et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics. 2008;122:1218–1222. doi: 10.1542/peds.2007-2723. [DOI] [PubMed] [Google Scholar]
- 9.Lam MW, Klassen AF, Montgomery CJ, LeBlanc JG, Skarsgard ED. Quality-of-life outcomes after surgical correction of pectus excavatum: a comparison of the Ravitch and Nuss procedures. J Pediatr Surg. 2008;43:819–825. doi: 10.1016/j.jpedsurg.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Haller JA, Jr, Scherer LR, Turner CS, Colombani PM. Evolving management of pectus excavatum based on a single institutional experience of 664 patients. Ann Surg. 1989;209:578–582. doi: 10.1097/00000658-198905000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis JT, Weinstein S. Repair of the pectus deformity: results of the Ravitch approach in the current era. Ann Thorac Surg. 2004;78:421–426. doi: 10.1016/j.athoracsur.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Fonkalsrud EW, Dunn JC, Atkinson JB. Repair of pectus excavatum deformities: 30 years of experience with 375 patients. Ann Surg. 2000;231:443–448. doi: 10.1097/00000658-200003000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mansour KA, Thourani VH, Odessey EA, Durham MM, Miller JI, Jr, Miller DL. Thirty-year experience with repair of pectus deformities in adults. Ann Thorac Surg. 2003;76:391–395. doi: 10.1016/s0003-4975(03)00441-7. [DOI] [PubMed] [Google Scholar]
- 14.Croitoru DP, Kelly RE, Jr, Goretsky MJ, Lawson ML, Swoveland B, Nuss D. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg. 2002;37:437–445. doi: 10.1053/jpsu.2002.30851. [DOI] [PubMed] [Google Scholar]
- 15.Hosie S, Sitkiewicz T, Petersen C, et al. Minimally invasive repair of pectus excavatum--the Nuss procedure. A European multicentre experience. Eur J Pediatr Surg. 2002;12:235–238. doi: 10.1055/s-2002-34486. [DOI] [PubMed] [Google Scholar]
- 16.Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg. 2004;77:289–295. doi: 10.1016/s0003-4975(03)01330-4. [DOI] [PubMed] [Google Scholar]
- 17.Kim DH, Hwang JJ, Lee MK, Lee DY, Paik HC. Analysis of the Nuss procedure for pectus excavatum in different age groups. Ann Thorac Surg. 2005;80:1073–1077. doi: 10.1016/j.athoracsur.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 18.Dzielicki J, Korlacki W, Janicka I, Dzielicka E. Difficulties and limitations in minimally invasive repair of pectus excavatum: 6 years experiences with Nuss technique. Eur J Cardiothorac Surg. 2006;30:801–804. doi: 10.1016/j.ejcts.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Coelho Mde S, Silva RF, Bergonse Neto N, et al. Pectus excavatum surgery: sternochondroplasty versus Nuss procedure. Ann Thorac Surg. 2009;88:1773–1779. doi: 10.1016/j.athoracsur.2009.07.051. [DOI] [PubMed] [Google Scholar]
- 20.Antonoff MB, Erickson AE, Hess DJ, Acton RD, Saltzman DA. When patients choose: comparison of Nuss, Ravitch, and Leonard procedures for primary repair of pectus excavatum. J Pediatr Surg. 2009;44:1113–1118. doi: 10.1016/j.jpedsurg.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 21.Nakaoka T, Uemura S, Yano T, Nakagawa Y, Tanimoto T, Suehiro S. Does overgrowth of costal cartilage cause pectus excavatum? A study on the lengths of ribs and costal cartilages in asymmetric patients. J Pediatr Surg. 2009;44:1333–1336. doi: 10.1016/j.jpedsurg.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 22.Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg. 2010;252:1072–1081. doi: 10.1097/SLA.0b013e3181effdce. [DOI] [PubMed] [Google Scholar]
- 23.Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg. 2010;139:379–386. doi: 10.1016/j.jtcvs.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Luu TD, Kogon BE, Force SD, Mansour KA, Miller DL. Surgery for recurrent pectus deformities. Ann Thorac Surg. 2009;88:1627–1631. doi: 10.1016/j.athoracsur.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Lawson ML, Barnes-Eley M, Burke BL, et al. Reliability of a standardized protocol to calculate cross-sectional chest area and severity indices to evaluate pectus excavatum. J Pediatr Surg. 2006;41:1219–1225. doi: 10.1016/j.jpedsurg.2006.03.003. [DOI] [PubMed] [Google Scholar]