Abstract
Objective
The aim of this study was to evaluate the effect of monochrome liquid crystal displays (LCDs) with different resolutions on observer performance during detection of small solitary pulmonary nodules.
Methods
Chest images of digital radiography were selected online from the hospital's picture archiving and communication system. Of the 164 images selected, small solitary non-calcified pulmonary nodules were present in 63 images and absent in 101 images. Observer performance was assessed among 3 extremely experienced, 3 very experienced and 3 moderately experienced radiologists, who independently interpreted these images on 2, 3 and 5 megapixel greyscale LCDs. A five-point confidence level rating scale was used to represent the presence of nodules: definite absence, probable absence, indetermination, probable presence and definite presence. The observers were requested to rank each image on the given display according to the presence of the pulmonary nodule. Observer performance was analysed in terms of receiver operating characteristics (ROCs).
Results
The areas under the ROC curves which represented the observer performance for the 2, 3 and 5 megapixel LCDs were found to be 0.705, 0.722 and 0.764, respectively, for the extremely experienced radiologists; 0.687, 0.712 and 0.721, respectively, for the very experienced radiologists; and 0.689, 0.696 and 0.711, respectively, for the moderately experienced radiologists. These differences were not statistically significant.
Conclusion
The observer performances for detection of small solitary non-calcified pulmonary nodules by radiologists with varying degrees of experience were comparable between the 2, 3 and 5 megapixel monochrome LCDs.
Advances in digital imaging technology and manufacturing have decreased the cost of digital display devices. Consequently, such displays are commonly used for the soft-copy reading of digital radiological images. Owing to the improved physical properties and performances of greyscale liquid crystal displays (LCDs) in luminance, contrast ratio, modulation transfer function (MTF), resolution and dynamic range, as well as susceptibility to light reflections [1-6], greyscale LCDs are highly recommended in diagnostic radiology practices. The pixel matrix size of the display is one of the main perceptual factors that affects the diagnostic quality of soft-copy reading [7,8] and directly determines the price of the LCD. However, the clinical performance of greyscale LCDs is not simply a function of its resolution, but also depends on the visual capability of the user, as well as the extent of the reader's work experience [8]. While concerns still remain as to which type of professional display and resolution can provide optimised diagnostic performance in routine diagnostic radiology practice, a considerable number of studies have been conducted to determine whether an LCD is an acceptable alternative to cathode ray tube (CRT) monitors with respect to their radiodiagnostic accuracy [1-2,6]. To date, a comparison between the different resolutions of greyscale LCDs alone has not been conducted. Thus, evaluation of the greyscale LCDs using an observer performance study may provide valuable information.
As a continuation of previous studies [1-4,6], our preliminary study aimed to compare the observer performances on three greyscale LCDs by the same manufacturer at different resolutions. As image diagnosis might be significantly influenced by the aptitude of the radiologist, behavioural differences of the observers and the extent of the radiologist's experience were taken into account in this image-reading study.
Methods and materials
Monitors
Three professional LCDs with different display pixel arrays were used in this study. Their properties are listed in Table 1. All monitors were greyscale and of portrait type. The displays were calibrated to DICOM-14 (Digital Imaging and Communications in Medicine part 14) greyscale display function standard [4,9]. To ensure that the image appearance on these monitors was consistent, the same software was used for test image viewing. Since the pixel number of each digital image was greater than the inherent display pixel count, a bilinear interpolation method was used to display the images by downsampling the horizontal-line and vertical-line data. The monitors were adjusted to the same calibrated luminance of 500 cd m−2 (supplier recommendation) and all had automatic adjustment function to maintain brightness stability. They were located adjacent to each other and at a similar height from the floor.
Table 1. Physical properties of the greyscale liquid crystal displays.
| LCD type | Display models | Resolution | Pixel pitch (mm) | Active screen diagonal (mm) | Calibrated luminance (cd m−2) |
| 2 megapixel | Barco MDNG-2121a | 1600×1200 | 0.270 | 540.0 | 500 |
| 3 megapixel | Barco E-3620a | 2048×1536 | 0.207 | 528.0 | 500 |
| 5 megapixel | Barco MDNG-5121a | 2560×2048 | 0.165 | 540.9 | 500 |
aManufactured by Barco, Kortrijk, Belgium.
Test image preparation
All test images were captured with a flat-panel digital radiography (DR) system (DR7500; Kodak, Rochester, NY). The pixel diameter was 143 μm, the exposure parameters were 115 kVp and 2.0–2.5 mAs, and the focus–detector distance was 180 cm. CT (BrillianceTM CT 64-channel scanner; Philips, Best, Netherlands) confirmation of the same patient served as the reference point for presence of a pulmonary nodule, and all examinations were performed at a pitch of 1.1, section thickness of 0.3 cm, and exposure parameters of 120 kVp and 150–180 mAs.
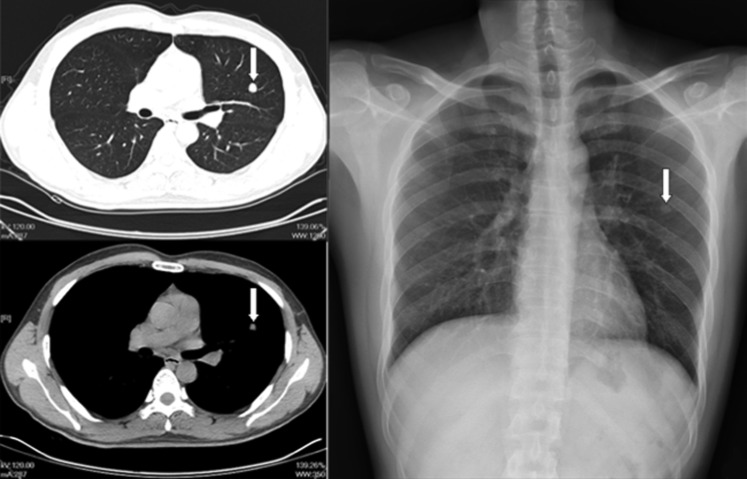
Erect posteroanterior DR images of the chest obtained at Shengjing Hospital of China Medical University, Shenyang, Liaoning, China, between October 2007 and November 2008 were carefully reviewed by two extremely experienced radiologists with at least 20 years of clinical experience, who did not participate in the subsequent image-reading study. The chest DR images, which were normal or revealed a solitary nodule measuring <1.0 cm in diameter, were unanimously reviewed and selected by these two senior radiologists. Each selected image was confirmed by CT scan, with the interval between CT and DR examination no more than 1 week (Figure 1). Images that were not suitable for this study, including images with poor or unacceptable image quality or images that showed either an overabundance of lesions or lesions that were too prominent, were eliminated.
Figure 1.
An example of a digital radiography chest image demonstrating a target nodule (arrow).
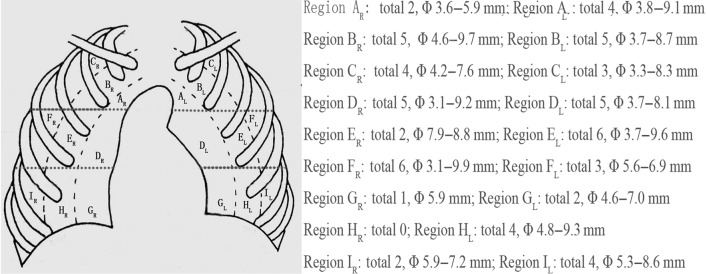
Consequently, 164 images (comprising 101 normal images representing the control group and 63 positive images representing the disease group) were selected from more than 130 000 chest DR images. Among the 63 patients with nodules, 33 were male and 30 were female, and among the 101 patients without nodules, 59 were male and 42 were female. Their ages ranged from 3.0 to 76.0 years (mean age, 48.7±19.7 years) and the median age was 52.0 years. For the 63 positive cases, all the pulmonary nodules were non-calcified, with diameters ranging between 0.31 and 0.99 cm (mean size, 0.71±0.24 cm; Figure 2). Interestingly, the mean size of the lesions chosen in this study was lower than that used in previous studies [3,5,9-10].
Figure 2.
Cartoon illustration of a posteroanterior chest image showing the regional distribution of the nodules for the 63 positive images.
Image interpretation
Three groups of radiologists with varying degrees of experience participated in this observer performance study. The first group consisted of three extremely experienced radiologists, with work experience of 38.0, 20.0 and 17.0 years. The second group consisted of three very experienced radiologists, with work experience of 11.0, 11.0 and 13.0 years. The third group consisted of three moderately experienced radiologists, with work experience of 1.0, 1.0 and 1.5 years. All participating radiologists were accustomed to using greyscale LCDs in their daily practice with appraisal of consistent capabilities among their peers in the same department.
Participants were not informed about the experimental objective, test protocol, clinical information and proportion of cases containing abnormalities prior to the study. For each observer, the image reading consisted of three sessions, in which all images were independently read on each of the three types of monitors. The observers were asked to estimate the probability of the presence of a nodule. A five-point confidence level rating scale was used to represent the confidence level of each observer [1,10-13] as follows: 1, definite absence; 2, probable absence; 3, indetermination; 4, probable presence; 5, definite presence.
In order to minimise the readers' learning effect, the 164 images were randomly displayed to each reader during each reading session. For each observer, the order of evaluation of the monitor types in the three reading sessions was also varied randomly [1,5,7]. 2 months elapsed between each interpreting session. In our study, the period between each reading session was longer than that used in previous studies [5,7,9,11,14] in an attempt to reduce the effects of memory. Prior to the study, the readers observed 10 images (6 normal cases and 4 that were positive for small solitary non-calcified pulmonary nodules) not included in the study population and assigned scores in consensus to ensure consistency of the test reading.
To simulate a normal environment used during routine clinical interpretation, no time constraint was imposed on any observer during the reading session [3,9]. However, readers were not provided with image post-processing tools, such as magnification and window-level adjusting [1]. In other words, with the exception of the test variable (the image resolution), the images shown on the three monitors were identical. To ensure that the ambient illuminance was identical for each reading session, the image reading was conducted in the same soft-copy reading room with the ambient room light set at a dim level (<40 lux) to reduce reflection [1-2,4,8-9].
The hospital's institutional review board approved the use of the test images and the participation of radiologists in the observer performance study. The study was in accordance with the Helsinki Declaration of the World Medical Association; all patient-related information remained confidential during interpretation.
Data analysis
In order to average out the behavioural differences of radiologists of the same aptitude, all 4428 observations (164 images ×99 readers ×93 displays) required pre-treatment. The scores given by radiologists with the same aptitude were averaged for the 2, 3 and 5 megapixel LCDs. Thus, we obtained nine groups of mean data.
The observer performance for detection of small solitary pulmonary nodules was determined by the means of receiver operating characteristics (ROC) analysis of the averaged data using the multireader–multicase ROC approach [10,15,16]. The area under the ROC curve (AUC) was considered to be the index of diagnostic accuracy. The statistical significance of the results for different reading modalities was reported as 95% confidence intervals (CIs) for mean differences in AUC values for observer performance. Mean differences were regarded as statistically significant at the 5% level when the corresponding CI did not encompass zero [10,13].
Results
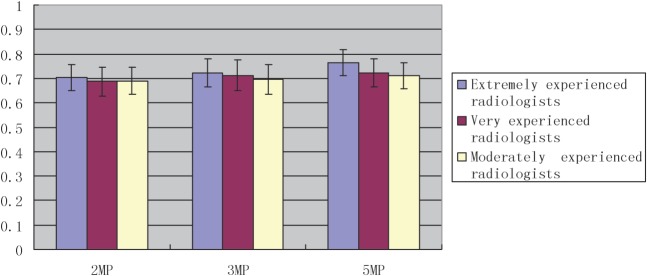
The results of the ROC study examining the observer performance for different display modalities are summarised in Table 2 and Figures 3 and 4. The AUCs for the extremely experienced radiologists were 0.705, 0.722 and 0.764 for the 2, 3 and 5 megapixel LCDs, respectively, compared with 0.687, 0.712 and 0.721, respectively, for the very experienced radiologists, and 0.689, 0.696 and 0.711, respectively, for the moderately experienced radiologists (Table 2).
Table 2. AUCs for different reading modalities.
| LCD type | Extremely experienced radiologists | Very experienced radiologists | Moderately experienced radiologists |
| 2 megapixel | 0.705±0.053 | 0.687±0.058 | 0.689±0.055 |
| 3 megapixel | 0.722±0.057 | 0.712±0.063 | 0.696±0.060 |
| 5 megapixel | 0.764±0.054 | 0.721±0.057 | 0.711±0.052 |
AUC, area under the receiver operating characteristics curve; LCD, liquid crystal display.
Figure 3.
Bar chart of the mean area under the receiver operating characteristics curves with standard errors for all observer groups.
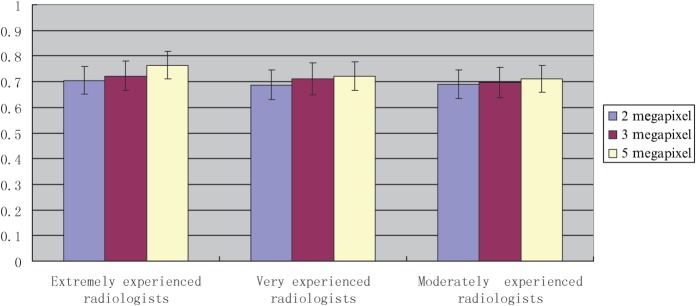
Figure 4.
Bar chart of mean area under the receiver operating characteristics curves with standard errors for different types of displays.
Figure 3 depicts the comparison of average AUCs for all the observer groups. The results show that the AUCs generally increased as a function of the radiologists' aptitude, especially on the 5 megapixel LCD. One exception included the AUC value for the moderately experienced radiologists, which was slightly higher than that of the very experienced radiologists for the 2 megapixel LCD. This might be purely incidental, and not a result of the radiologists' aptitude. Although diagnostic performance showed slight improvement with the increasing aptitude of the radiologists, the observed differences in AUCs among the three different groups of readers were small. Statistical analysis of the results indicated that all 95% CIs encompassed zero, which means that all p-values were higher than 0.05 and that no statistically significant differences in diagnostic performance were found among the observers of different aptitudes on any type of display. As shown in Figure 4, the AUCs, representing detection performance of small solitary non-calcified pulmonary nodules by radiologists of the same aptitude, increased as the display resolution increased, with a maximum AUC for the 5 megapixel LCD. However, differences in observer performance between any two of the three greyscale LCDs, for the three groups of radiologists, did not reach the desired level (all p-values >0.05).
Discussion
Recently, many studies have attempted to determine the applicability of new display devices in digital image-reading practice as compared with legacy display devices, such as screen-film systems vs CRT monitors, CRT monitors vs LCDs, and monochrome vs colour monitors [1,2,4,9,10,17-19]. However, to date, no studies have reported any significant differences between the different types of display devices used in diagnostic imaging practices. Shiraishi et al [14] suggested that it would be challenging to differentiate between observer performances obtained by using different displays, because of the difficulties involved in collecting a sufficient number of cases that contain lesions which are subtle enough to allow such a study on observer performances and display devices to be carried out. In addition, it is difficult to design a study that includes a sufficient number of radiologists who can detect such subtle lesions. Our hospital has a turnover rate of more than 8000 patients a day in the outpatient and emergency department, which might be the highest number of cases seen per day in all of the hospitals in China. Thus, we had access to an adequate number of cases with controlled test images, as well as a sufficient number of radiologists with different aptitudes, which we were able to use in the ROC study described here.
We show that the AUC, as an index of diagnostic accuracy, increased with an increase in the display resolution. This finding was not surprising, since more image information is available on the highest-resolution display. However, the study indicates that, at least for nodule detection, there were no significant differences among the three types of displays used in this experiment. The observer performance data described here are in agreement with previous similar reports. More recently, Yamada et al [9] reported that soft-copy reading using 3 megapixel and 5 megapixel LCDs is comparable with hard-copy reading for detecting breast cancer. Park et al [20] also showed that, for each reader, the observer performance of 5 megapixel LCD and 5 megapixel CRT monitors, under both bright and subdued ambient light conditions, showed no significant statistical differences for detecting nodules, pneumothorax and interstitial lung disease. In addition, there was no significant statistical difference in the average performance when the two monitor displays, under both bright and subdued ambient light conditions, were compared [20]. Another recent study by Kamitani et al [3] reported that observer performances for detecting masses of breast cancers were comparable among the hard-copy readings and soft-copy readings using 3 megapixel and 5 megapixel LCDs [3]. Furthermore, Uematsu and Kasami [21] showed that soft-copy reading of a digital mammography of mass with 3 megapixel LCD monitors was similar in diagnostic performance to 5 megapixel CRT monitors and 3 megapixel LCD monitors can replace 5 megapixel CRT monitors without any loss in the ability to diagnose digital mammograms. Some other reports are also congruent with the above results of our study [6,17-19,20-25]. Therefore, we believe that the results are generally applicable.
To date, the radiodiagnostic accuracy of displays with different resolutions has been compared between CRT displays and LCDs, colour and monochrome displays, as well as consumer and medical-grade displays [1,4,6,10,12,17]. The findings obtained from these previous studies were influenced not only by the display resolution, but by other display properties, such as luminance, MTFs and veiling glares. However, in our study we were able to focus on the effects of the resolution alone, since we used medical-grade monochrome LCDs from the same manufacturer. All of the displays used in this study had similar physical dimensions, MTFs and veiling glare, as well as uniform display luminance. In addition, all displays were calibrated according to DICOM-14 to obtain similar image presentation. Real-time adjustments of post-processing were not included in this study set-up. This exclusion could reduce the influence of confounding factors such as the varying practice habits of individual interpretation and variable familiarity with the use of post-processing tools, which could directly affect the detection performance. Thus, the conclusions drawn from this study were predominantly determined by differences in the resolutions of the test displays, as well as differences in the aptitude of the radiologists. The data obtained from our study were more significant and conclusive than findings from previous studies because of our high level of stringency, which ensured that factors other than the display resolution and radiologists' aptitude did not affect the results. On the other hand, since our study only included one series of LCDs from one manufacturer, our data cannot be extrapolated to include all LCDs used in every hospital worldwide.
The costs and performance capabilities of monochrome LCDs vary widely. In our hospital, the appropriate selection of radiodiagnostic displays is very important and requires balancing between the total cost of ownership and its performance. Our study, as well as other reports, suggests that it is practical to combine diagnostic systems with high-, mid- and low-resolution monochrome LCDs for use by a group of radiologists with a range of professional experience. Although preliminary diagnostic reports can be made by very experienced and moderately experienced radiologists using low-resolution displays, the final report by a senior radiologist should use the highest-resolution display in order to achieve maximal AUC values. This is not likely to reduce the overall diagnostic accuracy, but will reduce the cost. In our hospital, the above-described scheme has been adopted to allocate soft-copy reading displays, which have been proven to be feasible and efficient in practice.
We have addressed several limitations in our experimental design. First, a potential performance bias could not be completely eliminated since the participants were easily able to identify the different types of displays used in this study. Second, our study may undermine the benefits of soft-copy reading by prohibiting the observer from changing windows or making contrast adjustments, which are advantageous features of soft-copy reading [3]. In other words, using image post-processing might achieve a higher diagnostic performance in soft-copy reading. Third, although the participants were provided with 10 training cases initially, this number was probably not sufficient. Fourth, the overall applicability of the results of this study is somewhat limited since only one abnormality (i.e. non-calcified pulmonary nodules) was investigated. Thus, our results are not generally applicable for the routine interpretation of chest images until other abnormalities are also evaluated. For example, different types of pulmonary lesions have different requirements of display in terms of spatial resolution. Additional investigations using more subtle parenchyma or rib lesions on chest images should be evaluated. Fifth, the location of decision should be fully considered, otherwise it will leave a problem about statistical analysis and the results of detection performance will most likely be overestimated. Finally, another aspect worth considering is the impact of off-angle viewing. Generally, LCDs are more susceptible to off-axis viewing than CRT displays [2]. Reportedly, an off-axis angle of 30° might result in a 30% loss of luminance with the LCD screen [1]. The effect of off-angle viewing is still not well understood, although it is thought that it can be effectively eliminated by a correct viewing angle to be adopted by readers, and this viewing angle issue might not have a highly detrimental effect on observer performance [5,7].
Previous perception studies have divided interpretation errors of radiology into two categories: detection error and decision-making error. These studies indicate that detection errors occur when the radiologist does not focus on the abnormality, or briefly examines a potential abnormality, but dismisses it very quickly; and decision-making errors arise after the radiologist has searched the image and recognised the area as a potential abnormality, but then incorrectly classifies the area as not containing a lesion [26]. Decision-making errors can be more difficult to avoid than detection errors because while improving the conspicuity of lesions can be expected to reduce detection errors, it would not necessarily improve decision-making performance. In fact, decision-making errors have been suggested to be the primary perceptual errors in chest radiography [27]. Saunders and Samei [28] investigated the potential for using interpretation time as a means of improving accuracy in diagnostic tasks. Detection errors and classification errors had longer interpretation times than correct detection and classification decisions. The same authors also reported that interpretation time can be incorporated into mammographic decision-making in order to identify cases with higher probabilities of perceptual error that require further review [28]. Krupinski [29] reported that true- and false-positive decisions were associated with prolonged gaze durations; false-negative decisions were associated with longer gaze durations than true-negatives; and readers with more experience tended to detect lesions earlier than readers with less experience, but those with less experience tended to spend more time overall reading the images and cover more image area than did those with more experience. In our study, in order to simulate the actual environment of clinical practice, we did not consider the influence of the reader's reading time and eye positions on the results of observer performance.
Despite these limitations, to our best knowledge, this investigation is the first to compare differences in observer performance for the detection of pulmonary nodules among soft-copy reading using 2, 3 and 5 megapixel greyscale LCDs by the same manufacturer, and have some differences compared with some previous similar reports, such as adequate consideration to the aptitude of radiologists, selection of smaller lesions as the observation target, suggestion about rational allocation of the professional monochrome LCDs with different resolutions to improve the cost performance, and so on. We found that the observer performances for detection of small solitary non-calcified pulmonary nodules by radiologists with varying degrees of experience were comparable between the 2, 3 and 5 megapixel monochrome LCDs. Further studies should be performed to verify the limiting effects described above.
References
- 1.Oschatz E, Prokop M, Scharitzer M, Weber M, Balassy C, Schaefer-Prokop C. Comparison of liquid crystal versus cathode ray tube display for the detection of simulated chest lesions. Eur Radiol 2005;15:1472–6 [DOI] [PubMed] [Google Scholar]
- 2.Balassy C, Prokop M, Weber M, Sailer J, Herold CJ, Schaefer-Prokop C. Flat-panel display (LCD) versus high-resolution gray-scale display (CRT) for chest radiography: an observer preference study. AJR Am J Roentgenol 2005;184:752–6 [DOI] [PubMed] [Google Scholar]
- 3.Kamitani T, Yabuuchi H, Soeda H, Matsuo Y, Okafuji T, Sakai S, et al. Detection of masses and microcalcifications of breast cancer on digital mammograms: comparison among hard-copy film, 3-megapixel liquid crystal display (LCD) monitors and 5-megapixel LCD monitors: an observer performance study. Eur Radiol 2007;17:1365–71 [DOI] [PubMed] [Google Scholar]
- 4.Geijer H, Geijer M, Forsberg L, Kheddache S, Sund P. Comparison of color LCD and medical-grade monochrome LCD displays in diagnostic radiology. J Digit Imaging 2007;20:114–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Usami H, Ikeda M, Ishigaki T, Fukushima H, Shimamoto K. The influence of liquid crystal display (LCD) monitors on observer performance for the detection of nodular lesions on chest radiographs. Eur Radiol 2006;16:726–32 [DOI] [PubMed] [Google Scholar]
- 6.Scharitzer M, Prokop M, Weber M, Fuchsjager M, Oschatz E, Schaefer-Prokop C. Detectability of catheters on bedside chest radiographs: comparison between liquid crystal display and high-resolution cathode-ray tube monitors. Radiology 2005;234:611–16 [DOI] [PubMed] [Google Scholar]
- 7.Fukushima H, Ikeda M, Ishigaki T, Usami H, Shimamoto K. Influence of liquid crystal display monitors on observer performance for detection of diffuse pulmonary disease on chest radiographs. Radiat Med 2007;25:211–17 [DOI] [PubMed] [Google Scholar]
- 8.Graf B, Simon U, Eickmeyer F, Fiedler V. 1K versus 2K monitor: a clinical alternative free-response receiver operating characteristic study of observer performance using pulmonary nodules. AJR Am J Roentgenol 2000;174:1067–74 [DOI] [PubMed] [Google Scholar]
- 9.Yamada T, Suzuki A, Uchiyama N, Ohuchi N, Takahashi S. Diagnostic performance of detecting breast cancer on computed radiographic (CR) mammograms: comparison of hard copy film, 3-megapixel liquid-crystal-display (LCD) monitor and 5-megapixel LCD monitor. Eur Radiol 2008;18:2363–9 [DOI] [PubMed] [Google Scholar]
- 10.Hwang SA, Seo JB, Choi BK, Do KH, Ko SM, Lee SH, et al. Liquid-crystal display monitors and cathode-ray tube monitors: a comparison of observer performance in the detection of small solitary pulmonary nodules. Korean J Radiol 2003;4:153–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SY, Hwang YJ, Han YH, Seo JW, Lee JY, Kim YH, et al. An ROC study of chest radiographs: 2K versus 4K high-resolution soft-copy images. J Digit Imaging 2007;20:347–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langer S, Fetterly K, Mandrekar J, Harmsen S, Bartholmai B, Patton C, et al. ROC study of four LCD displays under typical medical center lighting conditions. J Digit Imaging 2006;19:30–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uematsu T. Detection of masses and calcifications by soft-copy reading: comparison of two postprocessing algorithms for full-field digital mammography. Jpn J Radiol 2009;27:168–75 [DOI] [PubMed] [Google Scholar]
- 14.Shiraishi J, Abe H, Ichikawa K, Schmidt RA, Doi K. Observer study for evaluating potential utility of a super-high-resolution LCD in the detection of clustered microcalcifications on digital mammograms. J Digit Imaging 2010;23:161–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metz CE. ROC methodology in radiologic imaging. Invest Radiol 1986;21:720–33 [DOI] [PubMed] [Google Scholar]
- 16.Metz CE, Starr SJ, Lusted LB. Observer performance in detecting multiple radiographic signals. Radiology 1976;121:337–47 [DOI] [PubMed] [Google Scholar]
- 17.Araki Y, Sanada S, Kobayashi T, Hashimoto N, Funabasama S. Evaluation of the perceptional performance of high resolution flat panel displays. Nippon Hoshasen Gijutsu Gakkai Zasshi 2005;61:1151–7 [DOI] [PubMed] [Google Scholar]
- 18.Ikeda R, Katsuragawa S, Shimonobou T, Hiai Y, Hashida M, Awai K, et al. Comparison of LCD and CRT monitors for detection of pulmonary nodules and interstitial lung diseases on digital chest radiographs by using receiver operating characteristic analysis. Nippon Hoshasen Gijutsu Gakkai Zasshi 2006;62:734–41 [DOI] [PubMed] [Google Scholar]
- 19.Buls N, Shabana W, Verbeek P, Pevenage P, De Mey J. Influence of display quality on radiologists' performance in the detection of lung nodules on radiographs. Br J Radiol 2007;80:738–43 [DOI] [PubMed] [Google Scholar]
- 20.Park CM, Lee HJ, Goo JM, Han DH, Kim JH, Lim KY, et al. Comparison of observer performance on soft-copy reading of digital chest radiographs: high resolution liquid-crystal display monitors versus cathode-ray tube monitors. Eur J Radiol 2008;66:13–18 [DOI] [PubMed] [Google Scholar]
- 21.Uematsu T, Kasami M. Soft-copy reading in digital mammography of mass: diagnostic performance of a 5-megapixel cathode ray tube monitor versus a 3-megapixel liquid crystal display monitor in a diagnostic setting. Acta Radiol 2008;49:623–9 [DOI] [PubMed] [Google Scholar]
- 22.Kim AY, Cho KS, Song KS, Kim JH, Kim JG, Ha HK. Urinary calculi on computed radiography: comparison of observer performance with hard-copy versus soft-copy images on different viewer systems. AJR Am J Roentgenol 2001;177:331–5 [DOI] [PubMed] [Google Scholar]
- 23.Langer S, Bartholmai B, Fetterly K, Harmsen S, Ryan W, Erickson B, et al. SCAR R&D Symposium 2003: comparing the efficacy of 5-MP CRT versus 3-MP LCD in the evaluation of interstitial lung disease. J Digit Imaging 2004;17:149–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pärtan G, Mayrhofer R, Urban M, Wassipaul M, Pichler L, Hruby W. Diagnostic performance of liquid crystal and cathode-ray-tube monitors in brain computed tomography. Eur Radiol 2003;13:2397–401 [DOI] [PubMed] [Google Scholar]
- 25.Cha JH, Moon WK, Cho N, Lee EH, Park JS, Jang MJ. LCD versus CRT monitors for digital mammography: a comparison of observer performance for the detection of clustered microcalcifications and masses. Acta Radiol 2009;50:1104–8 [DOI] [PubMed] [Google Scholar]
- 26.Nodine CF, Mello-Thoms C, Kundel HL, Weinstein SP. Time course of perception and decision making during mammographic interpretation. AJR Am J Roentgenol 2002;179:917–23 [DOI] [PubMed] [Google Scholar]
- 27.Manning DJ, Ethell SC, Donovan T. Detection or decision errors? Missed lung cancer from the posteroanterior chest radiograph. Br J Radiol 2004;77:231–5 [DOI] [PubMed] [Google Scholar]
- 28.Saunders RS, Samei E. Improving mammographic decision accuracy by incorporating observer ratings with interpretation time. Br J Radiol 2006;79:S117–22 [DOI] [PubMed] [Google Scholar]
- 29.Krupinski EA. Visual scanning patterns of radiologists searching mammograms. Acad Radiol 1996;3:137–44 [DOI] [PubMed] [Google Scholar]