Abstract
Objective
Accurate determination of right ventricular volume and ejection fraction (RVEF) is established using MRI. Automatic contour detection of the right ventricular endocardial border is not established in clinical practice, resulting in considerable manual efforts to quantify RVEF. Using transthoracic echocardiography (TTE), the tricuspid annular plane systolic excursion (TAPSE) has proved its worth for quantification of RVEF and risk prediction. Therefore, the aim of this study was to clarify whether TAPSE assessed with MRI as a fast and easily obtainable parameter correlated with volumetric quantification of RVEF.
Methods
Right ventricular volumes and RVEF were measured with the standardised slice-summation method at MRI. MRI-TAPSE was defined as maximum apical excursion of lateral tricuspid annular plane and measured in a four-chamber view using steady-state free precession sequences. Additionally, MRI-TAPSE was compared with TAPSE assessed using TTE.
Results
76 consecutive patients (aged 58±17 years) were examined. At MRI, right end-diastolic volumes were 97±36 ml, right end-systolic volumes were 57±27 ml and the mean RVEF was 42±14%. MRI-TAPSE was determined with 19±6 mm and correlated well at linear regression analysis with volumetric RVEF (r=0.72, p<0.001). Furthermore, MRI-TAPSE discriminated sufficiently between patients with impaired and normal RVEF. Multiplying MRI-TAPSE by 2.5 led to values close to the RVEF by volumetry. Additionally, MRI-TAPSE correlated well with TAPSE determined using TTE. The inter- and intra-observer variabilities of MRI-TAPSE determination were low (3.1% and 1.8%).
Conclusion
TAPSE assessed with MRI is a fast and easily obtainable parameter which correlates well with volumetric quantification of RVEF.
In the past decade, improved determination of right ventricular volume and function has enabled understanding of the pathophysiology of the right ventricle (RV), and favoured new therapeutic options in patients with pulmonary hypertension, myocardial infarction, acute and chronic heart failure, cardiac transplantation or congenital heart disease [1-7].
Today, echocardiography presents the most widely used non-invasive technique for right ventricular imaging. However, exact echocardiographic evaluation of the right ventricular function is limited by the complex geometrical shape and the reduced endocardial border delineation of the RV. A simplified echocardiographic method to estimate right ventricular ejection fraction (RVEF) by means of analysing the tricuspid annular plane systolic excursion (TAPSE) towards the cardiac apex has been described by Kaul et al [8]. Despite the fact that TAPSE presents only a one-dimensional echocardiographic method, previously published studies have demonstrated an accurate and easy estimation of RVEF [9-13] and the prognostic impact of RVEF as assessed by TAPSE [14,15].
On the other hand, cardiac MRI has been shown to be the gold standard for the assessment of RVEF [16]. MRI permits precise determination of the right ventricular volume, function and mass, with good reproducibility [16-18]. Nevertheless, the routine use of cardiac MRI for determination of right ventricular volume and function remains a time-consuming procedure. In recent years, sophisticated software tools which perform reliable automatic contour detection algorithms for the right ventricular endocardial border have become available. However, these software applications are not currently in widespread clinical use. Therefore, we investigated tricuspid annular plane systolic excursion assessed by cine mode MRI sequences (MRI-TAPSE) as a parameter for estimation of RVEF and right ventricular function.
The aim of this study was to clarify whether MRI-TAPSE as a fast and easily obtainable parameter correlated with volumetric estimation of normal-to-impaired RVEF determined by MRI. In addition, we analysed the inter- and intra-observer variabilities of this method.
Methods and materials
Study population
76 consecutive patients (26 females and 50 males) with normal to severely impaired RVEF were prospectively included from May 2009 until April 2010 at Heart Center Dresden, University Hospital, Dresden, Germany. Before undergoing MRI, all patients gave written informed consent. The study protocol was approved by the institutional ethical board. Eligible patients were aged ≥18 years. Those with known contraindications to MRI (e.g. a pacemaker or a defibrillator), impaired echocardiographic windows which did not allow adequate visualisation or atrial fibrillation were excluded.
Transthoracic echocardiography
Two-dimensional colour Doppler transthoracic echocardiography was performed on the same day as MRI by an experienced echocardiographer using an iE33® Echocardiography System (Philips, Amsterdam, Netherlands). Patients were examined in a supine, left lateral position. TAPSE presents the systolic motion of the tricuspid annulus towards the cardiac apex expressing the RV contraction along the longitudinal axis of the right ventricular free wall. By pointing the motion-mode (M-mode) cursor to the junction of the lateral annulus of the tricuspid valve in the apical four-chamber view, the excursion of the valve annulus was imaged. TAPSE was measured in the M-mode image as the height difference of the valve annulus excursion (in millimetres), which represents RV shortening. A value of >20 mm suggested normal systolic right ventricular function, whereas a TAPSE value of <20 mm was associated with RV dysfunction [19]. The echocardiographic investigator was blinded from the MRI results.
MRI
MRI was performed for determination of RV volumes and function. Patients were placed head-first in a supine position using an eight-channel cardiac coil. From the ventricular apex to the base, electrocardiogram (ECG)-triggered, breath-hold, balanced steady-state free precession sequences (Signa® 3T; GE Healthcare, Waukesha, WI) were obtained in the short-axis view. Parameters were as follows: echo time, 3.8 ms; repeat time, R–R interval; slice thickness, 10 mm; field of view, 35×35 cm; read matrix, 256; phase matrix, 128; number of frames, 26; flip angle, 40°; phase encode grouping, 6–10 and 8–12 short-axis slices, which were needed to encompass the entire RV. Manual tracing of the endocardial borders of the contiguous short-axis slices at end-diastole (the first cine phase of the R-wave-triggered acquisition) and end-systole (the image phase with the smallest cavity area) stages allowed for calculation of right ventricular end diastolic volume and right ventricular end-systolic volume, from which RVEF was derived.
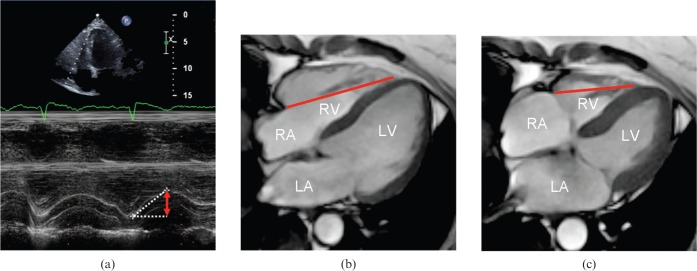
Furthermore, MRI was performed for determination of MRI-TAPSE. A stack of four-chamber views using ECG-triggered, breath-hold, balanced steady-state free precession sequences was obtained. The largest distance between the lateral tricuspid annulus and the right ventricular apex was defined at the end-systolic and end-diastolic stages. MRI-TAPSE (measured in millimetres) was defined as the difference between those two measurements (Figure 1). All images were evaluated with a commercially available computer software program (ReportCard® 4.0; GE Healthcare).
Figure 1.
(a) TAPSE measurement using TTE. The red arrow in the motion mode image delineates maximum systolic excursion of the lateral tricuspid annulus in millimetres. (b) End-diastolic and (c) end-systolic four-chamber view of a balanced steady-state free precession sequence with distance measurements between the lateral tricuspid ring and the right ventricular apex. The difference between the end-diastolic and end-systolic measurements was defined as MRI-TAPSE. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; TAPSE, tricuspid annular plane systolic excursion; TTE, transthoracic echocardiography.
The blinded data set of all subjects was re-analysed by a second experienced observer to assess interobserver variability. This observer was blinded to the previous results. To analyse intra-observer variability, the primary observer re-evaluated measurements 7 days after the first analysis.
Statistical analysis
Demographic data and results are provided as mean values±standard deviation (SD). The correlation between RVEF and MRI-TAPSE was determined using linear regression analysis, including standard errors of the estimate. Agreement between measurements was evaluated using the standard paired t-test. Furthermore, Bland–Altman analysis was used to determine the mean of the difference with 95% limits of agreement (±1.95 SD) in a prospective cohort. A two-tailed p-value of <0.05 was considered to be statistically significant.
Results
In all subgroups, diagnostic quality data sets were obtained. The mean age of the 76 patients was 58±17 years. The RVEF was measured using MR volumetry from the end-diastolic and end-systolic volumes, as described previously. The mean RVEF for the total study population was 42±14%. 57 of the 76 patients (75%) showed an impaired RVEF (<50%). The most frequent causes of right ventricular dysfunction were coronary artery disease (27 patients); valvular heart disease (severe mitral regurgitation or aortic stenosis; 22 patients); pulmonary hypertension after a history of thrombo-embolic events (6 patients); and hypertensive heart disease with diastolic left ventricular dysfunction (21 patients).
Table 1 shows the clinical characteristics of the patients along with MR volumetric measurements.
Table 1. Clinical characteristics.
| Characteristics | Results |
| Patients | 76 |
| Women | 26 (34) |
| Men | 50 (67) |
| Age at closure (years) | 58±17 |
| CAD | 27 |
| VHD | 22 |
| PHT after thrombo-embolic event | 6 |
| LVDD | 21 |
| TAPSE at TTE (mm) | 22±5 |
| TAPSE at MRI (mm) | 19±6 |
| RVEF at MRI (%) | 42±14 |
CAD, coronary artery disease; LVDD, left ventricular diastolic dysfunction; PHT, pulmonary hypertension; RVEF, right ventricular ejection fraction; TAPSE, tricuspid annular plane systolic excursion; TTE, transthoracic echocardiography; VHD, valvular heart disease.
Data are given as number, number (percentage) or mean ± standard deviation.
In linear regression analysis, proper correlation between TAPSE assessed with TTE and TAPSE calculated with MRI over the RVEF range was obvious (r=0.85, p<0.001; data not shown). Bland–Altman plots showed no relevant bias between the imaging techniques for TAPSE.
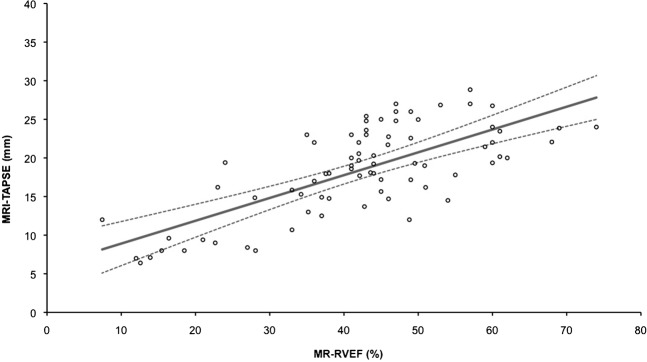
Furthermore, MRI-TAPSE showed suitable correlation with RVEF assessed using MR volumetry in patients with both normal ejection fraction and severe RV dysfunction (r=0.72, p<0.001).
Figure 2 shows the quantification of RVEF using MR volumetry. Figure 3 depicts the correlation between MRI-TAPSE and MR-RVEF.
Figure 2.

Manual tracing of the endocardial borders of contiguous short-axis slices at end-diastole and end-systole at right ventricular base. (a, b) Midventricular and (c, d) apex of right ventricle allowed for calculation of (e, f) right ventricular end-diastolic volume and right ventricular end systolic volume, from which right ventricular volume and ejection fraction were derived.
Figure 3.
Correlation between MRI-TAPSE and RVEF, r=0.72. MRI-TAPSE, MRI-tricuspid annular plane systolic excursion; RVEF, right ventricular end-diastolic volume.
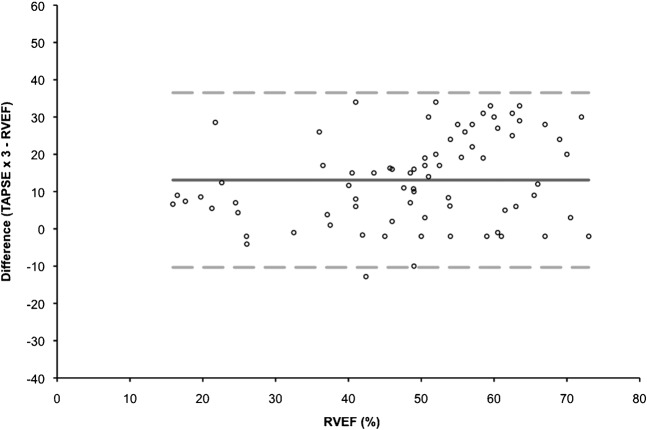
A Bland–Altman analysis was performed to compare the MRI-TAPSE method with the MR-RVEF volumetry technique. For this purpose, the MRI-TAPSE value was multiplied by 3 to match the values suggested by Kaul et al [8]. However, this led to a bias of 13.1% (Figure 4), indicating an overestimation of RVEF assessed with TAPSE. Different factors multiplied with MRI-TAPSE were evaluated for RVEF quantification. The lowest bias was reached in Bland–Altman analysis when MRI-TAPSE was multiplied by 2.5. Figure 5 presents the Bland–Altman analysis by using a factor of 2.5. In this analysis, a bias of 3.9% was reached.
Figure 4.
Bland–Altman analysis of MRI-TAPSE and MR volumetry using a factor of 3. The discontinuous lines show the standard deviation and the continuous line illustrates the bias of 13.1%. MRI-TAPSE, MRI-tricuspid annular plane systolic excursion; RVEF, right ventricular end-diastolic volume.
Figure 5.
Bland–Altman analysis of MRI-TAPSE and MR volumetry using a factor of 2.5. The discontinuous lines show the standard deviation and the continuous line illustrates the bias of 3.9%. MRI-TAPSE, MRI-tricuspid annular plane systolic excursion; RVEF, right ventricular end-diastolic volume.
In addition, the inter- and intra-observer variabilities of MRI-TAPSE determination were low (3.1% and 1.8%, respectively). The inter- and intra-observer variabilities of the right ventricular volumetry were also low (1.9% and 1.4%, respectively).
Discussion
The salient finding of the present study is that a reliable estimation of RVEF is possible with the assessment of TAPSE using MRI. For MRI-TAPSE calculation, the largest distance between the lateral tricuspid annulus and the right ventricular apex was defined at the end-systolic and end-diastolic stages, and the difference between those two measurements was obtained. A good correlation between MRI-TAPSE and MRI right ventricular volumetry was also obvious in patients with normal and impaired right ventricular function (<50%).
Bland–Altman analysis revealed that by multiplying MRI-TAPSE by 2.5, a close estimation of RVEF is possible (Figure 5). Using echocardiography and radionuclide angiography, Kaul et al [8] showed that RVEF is approximately equivalent to TAPSE multiplied by 3. However, according to the Bland–Altman analysis, multiplying MRI-TAPSE by 3 in the present study resulted in an overestimation of RVEF, with a bias of 13.1% (Figure 4). Using the suggested multiplication of 2.5, the bias was reduced to 3.9%. Therefore, we recommend multiplying MRI-TAPSE by 2.5 to semi-quantify RVEF at MRI. In light of these results, we propose 20 mm as the threshold value for MRI-TAPSE, below which TAPSE should be considered abnormal. This confirms the threshold of TAPSE derived by echocardiography to determine impaired right ventricular function (20 mm) using MRI.
In both TAPSE and right ventricular volumetry, intra-observer variability was slightly higher than interobserver variability, although both were very low. Compared with data in the literature regarding inter- and intra-observer variability of left ventricular volumetry [17], measurement of right ventricular volumetry seems to be more error prone, owing to the complex geometry and the thin wall of the RV.
Despite TAPSE presenting only a one-dimensional echocardiographic method and disregarding the dysfunction of the middle and apical segments of the RV [18], previously published studies have demonstrated a good estimation of RVEF assessed using TASPE [9,15,19-20]. In these studies, TAPSE had an even better correlation to MRI-RVEF than assessment of RVEF with three-dimensional echocardiography [15]. Recently, Saxena et al [9] showed an excellent correlation between tricuspid annular systolic velocity and TAPSE in an assessment of RVEF in patients with pulmonary artery hypertension. Moreover, previous studies showed the prognostic impact of RVEF as assessed by TAPSE in patients with congestive heart failure and in patients with inferior myocardial infarction [20].
In the present study, echocardiographic TAPSE correlated well with TAPSE assessed with MRI, with low inter- and intra-observer variabilities.
The small patient number was a limitation of the present study; as a result, the statistical power was limited. However, significant results may be obtained with even a small population.
TAPSE does not take regional wall motion abnormalities of the RV into consideration. TAPSE measurement must be captured in the same four-chamber view at the exact end-systolic and end-diastolic positions of the apex and lateral tricuspid annulus, considering the fact that, in reality, the heart often translates within the four-chamber view. In the present study, cases where normal TAPSE in patients with a very large RV reflected normal RVEF or even overestimated RVEF were not drawn out of the data because the number of patients with severely dilated RVs was too small to give a reliable statement. Patients with congenital heart diseases were not included. Whether the correlation between TAPSE and volumetric RVEF is transferable to these patients should be investigated further.
The present data demonstrate a reliable estimation of RVEF determined by MRI-TAPSE in patients with normal to severely impaired ventricular function. Therefore, TAPSE primarily established as an echocardiographic parameter can be considered as an easy method to obtain routine MRI measurements to assess RVEF in clinical settings.
References
- 1.Shah PK, Maddahi J, Staniloff HM, Ellrodt AG, Pichler M, Swan HJ, et al. Variable spectrum and prognostic implications of left and right ventricular ejection fractions in patients with and without clinical heart failure after acute myocardial infarction. Am J Cardiol 1986;58:387–93 [DOI] [PubMed] [Google Scholar]
- 2.Zehender M, Kasper W, Kauder E, Schonthaler M, Geibel A, Olschewski M, et al. Right ventricular infarction as an independent predictor of prognosis after acute myocardial infarction. N Engl J Med 1993;328:981–8 [DOI] [PubMed] [Google Scholar]
- 3.Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol 1995;25:1143–53 [DOI] [PubMed] [Google Scholar]
- 4.Juilliere Y, Barbier G, Feldmann L, Grentzinger A, Danchin N, Cherrier F. Additional predictive value of both left and right ventricular ejection fractions on longterm survival in idiopathic dilated cardiomyopathy. Eur Heart J 1997;18:276–80 [DOI] [PubMed] [Google Scholar]
- 5.Gavazzi A, Berzuini C, Campana C, Inserra C, Ponzetta M, Sebastiani R, et al. Value of right ventricular ejection fraction in predicting short-term prognosis of patients with severe chronic heart failure. J Heart Lung Transplant 1997;16:774–85 [PubMed] [Google Scholar]
- 6.Piran S, Veldtman G, Siu S, Webb GD, Liu PP. Heart failure and ventricular dysfunction in patients with single or systemic right ventricles. Circulation 2002;105:1189–94 [DOI] [PubMed] [Google Scholar]
- 7.Schoen SP, Kittner T, Bohl S, Braun MU, Simonis G, Schmeisser A, et al. Transcatheter closure of atrial septal defects improves right ventricular volume, mass, function, pulmonary pressure, and functional class: a magnetic resonance imaging study. Heart 2006;92:821–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 1984;107:526–31 [DOI] [PubMed] [Google Scholar]
- 9.Saxena N, Rajagopalan N, Edelman K, López-Candales A. Tricuspid annular systolic velocity: a useful measurement in determining right ventricular systolic function regardless of pulmonary artery hypertension. Echocardiography 2006;23:750–5 [DOI] [PubMed] [Google Scholar]
- 10.Ghio S, Recusani F, Klersy C, Sebastiani R, Laudisa ML, Campana C, et al. Prognostic usefulness of the tricuspid annular plane systolic excursion in patients with congestive heart failure secondary to ideopathic or ischemic dilated cardiomyopathy. Am J Cardiol 2000;85:837–42 [DOI] [PubMed] [Google Scholar]
- 11.Alam M, Wardell J, Anderson E, Samad BA, Nordlander R. Right ventricular function in patients with first inferior myocardial infarction: assessment by tricuspid annular motion and tricuspid annular velocity. Am Heart J 2000;139:710–15 [DOI] [PubMed] [Google Scholar]
- 12.Meluzín J, Ŝpinarová L, Bakala J, Toman J, Krejĉí J, Hude P, et al. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion. Eur Heart J 2001;22:340–8 [DOI] [PubMed] [Google Scholar]
- 13.Ueti OM, Camargo EE, Ueti Ade A, de Lima-Filho EC, Nogueira EA. Assessment of right ventricular function with doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart 2002;88:244–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karatasakis GT, Karagounis LA, Kalyvas PA, Manginas A, Athanassopoulos GD, Aggelakas SA, et al. Prognostic significance of echocardiographically estimated right ventricular shortening in advanced heart failure. Am J Cardiol 1998;82:329–34 [DOI] [PubMed] [Google Scholar]
- 15.Samad BA, Alam M, Jensen-Urstad K. Prognostic impact of right ventricular involvement as assessed by tricuspid annular motion in patients with acute myocardial infarction. Am J Cardiol 2002;90:778–81 [DOI] [PubMed] [Google Scholar]
- 16.Helbing WA, Bosch HG, Maliepaard C, Rebergen SA, van derGeest RJ, Hansen B, et al. Comparison of echocardiographic methods with magnetic resonance imaging for the assessment of right ventricular function in children. Am J Cardiol 1995;76:589–95 [DOI] [PubMed] [Google Scholar]
- 17.Sievers B, Kirchberg S, Franken U, Puthenveettil BJ, Bakan A, Trappe HJ. Visual estimation versus quantitative assessment of left ventricular ejection fraction: a comparison by cardiovascular magnetic resonance imaging. Am Heart J 2005;150:737–42 [DOI] [PubMed] [Google Scholar]
- 18.Lorenz CH, Walker ES, Graham TP, Jr, Powers TA. Right ventricular performance and mass by use of cine MRI late after atrial repair of transposition of the great arteries. Circulation 1995;92Suppl. 9:II233–9 [DOI] [PubMed] [Google Scholar]
- 19.Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennel DJ. Interstudy reproducibility of right ventricular volume, function, and mass with cardiovascular magnetic resonance. Am Heart J 2004;147:218–23 [DOI] [PubMed] [Google Scholar]
- 20.Lopez-Candales A, Rajagopalan N, Saxena N, Gulyasy B, Edelman K, Bazaz R. Right ventricular systolic function is not the sole determinant of tricuspid annular motion. Am J Cardiol 2006;98:973–7 [DOI] [PubMed] [Google Scholar]