SUMMARY
Interactions of cancer cells with the primary tumor microenvironment are important determinants of cancer progression towards metastasis but it is unknown whether additional prometastatic signals are provided during the intravascular transit to the site of metastasis. Here, we show that platelet-tumor cell interactions are sufficient to prime tumor cells for subsequent metastasis. Platelet-derived TGFβ and direct platelet-tumor cell contacts synergistically activate the TGFβ/Smad and NF-κB pathways in cancer cells, resulting in their transition to an invasive mesenchymal-like phenotype and enhanced metastasis in vivo. Inhibition of NF-κB signaling in cancer cells or ablation of TGFβ1 expression solely in platelets protects against lung metastasis in vivo. Thus, cancer cells rely on platelet-derived signals outside of the primary tumor for efficient metastasis.
INTRODUCTION
The dynamic crosstalk between tumors and their microenvironment is increasingly recognized as a key regulator of malignant progression. Tumor cells are known to secrete several cytokines, which activate stromal fibroblasts and induce the recruitment of immune cells to the tumor. In turn, signals provided by the local microenvironment promote the ability of tumor cells to invade and metastasize (Joyce and Pollard, 2009). In primary carcinomas, secreted growth factors and cytokines contributed by stromal cells are key in inducing epithelial-mesenchymal transition (EMT), a transient and reversible process that promotes cell motility, invasion, and dissemination of cancer cells out of the tumor microenvironment (Scheel et al., 2007; Thiery, 2002). Subsequently, tumor cells travel through the bloodstream before arresting and extravasating in a new microenvironment (secondary site). Some current models of tumor progression propose that the metastatic potential of tumor cells is entirely shaped at the primary tumor site, with few or no signaling events occurring during the intravascular transit of tumor cells. Considering that multiple growth factors and cytokines are released in the bloodstream, cancer cells may sense additional signaling cues outside of the primary microenvironment. However, it is unclear whether circulating cancer cells require additional instructive signals for effective metastasis, either while in the circulation or on arrival at the secondary site.
Among the multitude of different signaling molecules found in the blood, transforming growth factor-beta (TGFβ) is known to promote metastasis by enhancing EMT and invasiveness in primary carcinomas (Oft et al., 1998). Furthermore, inhibition of the ability of tumor cells to respond to TGFβ (by overexpression of dominant-negative TGFβ receptor II) reduces intravasation and metastatic seeding in the lungs (Biswas et al., 2007; Padua et al., 2008; Siegel et al., 2003) as well as the development of bone metastases (Yin et al., 1999). In particular, upon dissemination to the bones, tumor cells activate osteoclasts to degrade the bone matrix and release the stored TGFβ, which in turn leads to enhanced tumor cell malignancy (Kang et al., 2005). However, in the case of metastasis to other tissues such as the lungs, the source of TGFβ bioavailable to tumor cells at the site of metastatic seeding remains unknown.
Platelets contain a plethora of growth factors and cytokines, including high concentrations of TGFβ (Assoian et al., 1983). Thus, platelet-derived factors could potentially be involved in the promotion of a metastatic phenotype. Consistent with a role of platelets in metastasis, defective platelet function or reduced platelet counts have been associated with decreased metastasis formation in various transgenic mouse models (Bakewell et al., 2003; Camerer et al., 2004; Gasic et al., 1968; Kim et al., 1998). The prometastatic effects of platelets have so far been attributed to their ability to promote adhesion or to their capacity to prevent cell death in the circulation by forming a physical shield around tumor cells. This shield protects tumor cells from natural killer cell-mediated lysis (Nieswandt et al., 1999; Palumbo et al., 2005), limits their exposure to shear stress, and promotes their adhesion to the endothelium (Erpenbeck and Schon, 2010; Gay and Felding-Habermann, 2011; Im et al., 2004; Jain et al., 2007; Karpatkin et al., 1988; Sierko and Wojtukiewicz, 2007). In addition, it is possible that platelets provide instructive signals that affect tumor cell behavior and metastatic potential.
In this study, we have tested whether platelets can provide a signaling platform for cancer cells outside of the primary tumor in the context of metastasis.
RESULTS
Platelets Prime Tumor Cells For Metastasis
To investigate whether platelets can have a direct impact on tumor cell behavior, we tested whether platelets could prime tumor cells for metastasis. Colon carcinoma cells (MC38GFP; isolated from a grade III carcinoma chemically induced in a C57BL/6 mouse; Corbett et al., 1975) or breast carcinoma cells (Ep5 (EpRas); spontaneously immortalized mouse mammary epithelial cell line transformed by the v-Ha-Ras oncogene; Oft et al., 1996) were coincubated with purified platelets for 40h in vitro. Platelets were then washed away, and tumor cells (substantially devoid of any platelets; Fig. S1A) were injected into the tail veins of mice. Pretreating either MC38GFP or Ep5 cells with platelets led to a marked increase in the number of metastatic foci in the lungs 14 days after tail-vein injection (Fig. 1A). The increase in metastasis was presumably due to the enhanced capacity of MC38GFP and Ep5 cells to seed the lungs as demonstrated by increased numbers of cells present after 48h (Fig. 1B). These results indicate that a transient interaction between tumor cells and platelets in vitro is sufficient to increase tumor cell metastatic seeding.
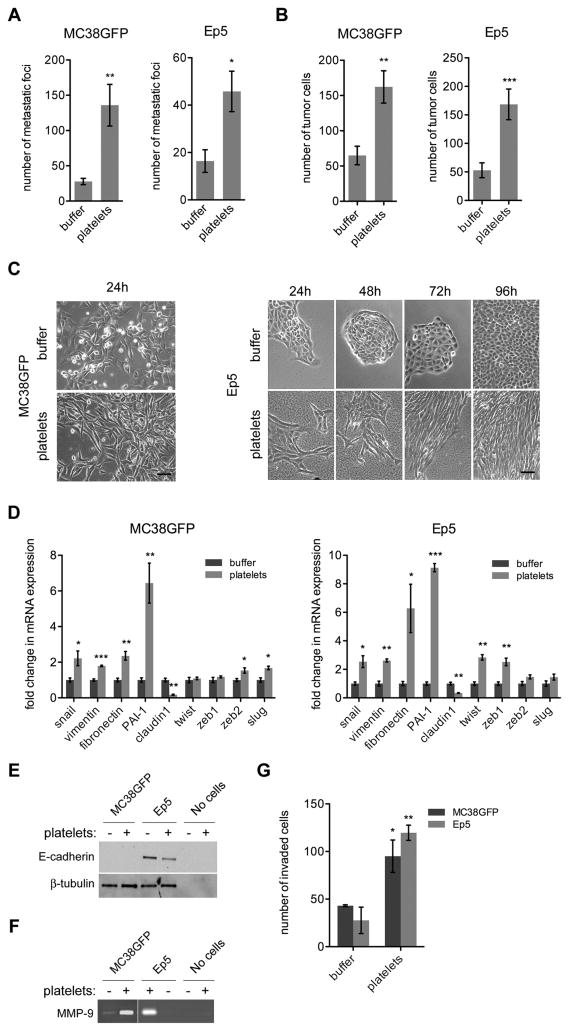
Figure 1. Pretreatment of Tumor Cells with Platelets Promotes Lung Metastasis by Increasing Tumor Cell Seeding and Inducing an EMT-Like Invasive Phenotype.
(A) Numbers of metastatic foci at the surface of lungs (2 largest lobes) 14 days after tail-vein injection of MC38GFP cells or Ep5 cells stably expressing ZsGreen (Ep5-ZsGreen) pretreated with buffer (vehicle) or platelets for 40h (n=5–12).
(B) Numbers of tumor cells at the surface of lungs 48h after tail-vein injection of MC38GFP or Ep5-ZsGreen cells pretreated with buffer or platelets for 40h (n=6–11).
(C) Phase-contrast micrographs of MC38GFP or Ep5 cells treated with buffer or platelets for the times indicated. Scale bar=50μm.
(D) Relative fold change in mRNA expression in MC38GFP or Ep5 cells treated with buffer or platelets for 40h (n=3). Values are normalized to Gapdh expression.
(E) Detection of E-cadherin protein levels by immunoblotting of lysates of MC38GFP or Ep5 cells treated as in (D). Amounts of platelets equal to those used to treat cells were also loaded as control (no cells). β-tubulin was used as loading control.
(F) Zymography for MMP-9 in the conditioned medium of MC38GFP or Ep5 cells treated as in (D). Amounts of platelets equal to those used to treat cells were also loaded as control (no cells).
(G) MC38GFP and Ep5 cells were added at the top of transwells coated with Matrigel and treated with buffer or platelets. The total number of cells that invaded to the bottom of the transwell was counted after 48h (n=3).
For panels A, B, D and G bars represent the mean ± SEM. *p<0.05, **p<0.01, ***p<0.001 were determined by Student’s t-test.
See also Figure S1.
Treatment of Tumor Cells with Platelets Induces an Invasive Mesenchymal-Like Phenotype
We next sought to define the molecular mechanisms induced by platelet-tumor cell interactions that could mediate the increased metastatic capacity of tumor cells. In tissue culture, both MC38GFP and Ep5 tumor cell lines underwent morphological changes reminiscent of an epithelial-mesenchymal transition (EMT) when treated with platelets for 24h (Fig. 1C). Analysis of mesenchymal markers and transcription factors involved in EMT revealed that the mRNA expression of snail (Snai1), vimentin (Vim), fibronectin (Fn1), and plasminogen activator inhibitor-1 (PAI-1; Serpine1) was consistently upregulated, whereas the epithelial marker claudin 1 (Cldn1) was downregulated in platelet-treated cells (Fig. 1D). E-cadherin protein levels were also reduced in platelet-treated Ep5 cells in comparison with controls (Fig. 1E, and Fig. S1B), while N-cadherin was relocalized from cell-cell juctions to the cytoplasm (Fig. S1B). In addition, zymography revealed increased matrix metalloproteinase-9 (MMP-9) secretion following exposure to platelets (Fig. 1F), suggesting a higher capacity to degrade the extracellular matrix (ECM) and to invade the surrounding environment. In agreement with these findings, the human breast epithelial cell lines MCF10A and HMLER also displayed a more mesenchymal morphology upon exposure to platelets (Fig. S1C), together with increased expression of EMT-associated genes and MMP-9 secretion (Fig. S1D, E). Thus, platelets induce EMT-like features also in epithelial cells of human origin.
To test directly whether EMT-like morphological and molecular changes promote an invasive behavior, we seeded platelet-treated MC38GFP and Ep5 cells on Matrigel-coated transwells and detected increased invasion in comparison with untreated cells (Fig. 1G). Altogether these results show that platelets promote the adoption of a more mesenchymal and invasive phenotype by tumor cells.
Platelets Promote Activation of the TGFβ/Smad Pathway in Tumor Cells
To gain better insight into the signaling pathways involved in platelet-to-tumor cell communication, we defined the platelet-induced gene expression signature by microarray analysis. For this purpose, gene expression profiles of Ep5 cells treated for 24h with platelets or buffer alone (untreated) were compared. Any contribution of platelet mRNA was excluded from the platelet-induced gene signature by performing a microarray with platelets alone (see Experimental Procedures; Fig. 2A). Only 21 mRNAs were contributed at significant levels by the platelets and were excluded from subsequent analyses. Among the most highly upregulated genes in tumor cells, we found several genes known to play prominent roles in EMT, ECM remodeling, and the promotion of metastasis (for example: Mmp9, Serpine1 (PAI-1), Fn1, Jag1, Vegfc, Vim, Edn1, Vegfa, Ctgf ; Table S1 and Table S2). Bioinformatic analysis using GeneGo canonical pathway maps (Fig. 2B) and gene set enrichment analysis (GSEA; Table 1) confirmed that platelets strongly activate EMT-related genes and revealed TGFβ-dependent pathways as being the most significantly upregulated following platelet treatment (Fig. 2B). Interestingly, GSEA analyses further revealed that previously defined gene signatures associated with cancer stem cells, poor prognosis and metastasis are also enriched in platelet-treated cells, suggesting that platelets induce an overall more aggressive phenotype in tumor cells (Table 1).
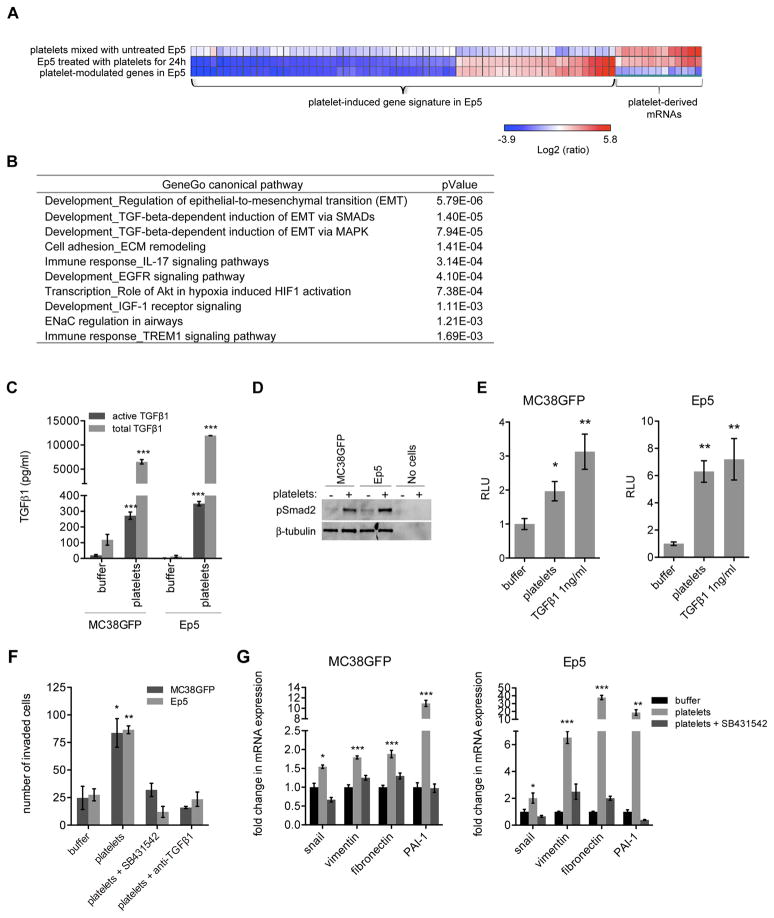
Figure 2. Platelet-Induced Gene Expression Signature Reveals Increased Expression of Prometastatic Genes and Activation of the TGFβ Pathway in Tumor Cells.
(A) Heat map of genes regulated by more than 4 fold (p<0.05) in Ep5 cells treated with platelets in comparison with untreated Ep5 cells (line 2). Line 1 and line 2 show Log2 ratios of gene expression compared to untreated Ep5 cells. mRNAs present in platelets (line1) were removed from the list of genes modulated upon platelet treatment of Ep5 cells (line 2) to generate a platelet-induced gene signature (line 3), which is listed in Table S2.
(B) Canonical signaling pathways most significantly associated with the list of genes differentially expressed by Ep5 cells upon platelet treatment (platelet-induced gene signature; Table S1; threshold = 2 fold, up and down regulated genes considered, p<0.05) as determined with GeneGo canonical pathway maps. The ten pathways with the lowest p values are shown.
(C) Concentration of active and total TGFβ1 in conditioned medium from MC38GFP or Ep5 cells treated with buffer or platelets for 40h. The conditioned medium was collected, centrifuged to remove platelets, and the presence of TGFβ1 in the supernatant measured by ELISA. Each bar represents the mean ± SEM of n=2–6. ***p<0.001 as determined by Student’s t-test.
(D) Detection of phospho-Smad2 protein levels by immunoblotting of Ep5 or MC38GFP cells treated as in (C). Amounts of platelets equal to those used to treat cells were also loaded as control (no cells). β-tubulin is used as loading control.
(E) Relative luciferase activity (RLU) in MC38GFP or Ep5 cells stably expressing a luciferase reporter under the control of an SBE promoter and treated for 40h with buffer, platelets or 1ng/ml TGFβ1 (positive control) (n=5–6).
(F) MC38GFP and Ep5 cells were added at the top of transwells coated with Matrigel and treated with buffer, platelets, platelets + SB431542 (10μM) or platelets + TGFβ1 blocking antibody (6μg/ml). The total numbers of cells that invaded to the bottom of the transwell were counted after 48h (n=3).
(G) Relative fold change in mRNA expression in MC38GFP or Ep5 cells treated with buffer, or platelets +/− SB431542 (10μM) for 40h (n=3). Values are normalized to Gapdh expression.
For panels E, F and G bars represent the mean ± SEM, and *p<0.05, **p<0.01, ***p<0.001 vs buffer were determined by one-way ANOVA followed by Tuckey’s post test.
Table 1.
Gene Set Enrichment Analysis (GSEA) for Ep5 Cells Treated with Platelets
| Gene sets | NES | Nominal p-value | FDR |
|---|---|---|---|
| EMT Signatures | |||
| BLICK_EMT-SIG_UP | 1.993 | <0.001 | <0.001 |
| TAUBE_EMT_UP | 1.328 | 0.060 | 0.060 |
| TAUBE_EMT_DN | −2.081 | <0.001 | <0.001 |
| ONDER_CDH1_TARGETS_2_UP | 1.526 | <0.001 | 0.044 |
| ONDER_CDH1_TARGETS_2_DN | −1.832 | <0.001 | 0.006 |
| TGFβ Signatures | |||
| GIAMPIERI_TGFB_UP | 1.992 | <0.001 | <0.001 |
| GIAMPIERI_TGFB_DN | −2.576 | <0.001 | <0.001 |
| VALCOURT_TGFB_UP | 1.813 | <0.001 | 0.005 |
| VALCOURT_TGFB_DN | −1.926 | <0.001 | <0.001 |
| Cancer Stem Cell Signatures | |||
| CREIGHTON_CSC_UP | 1.675 | <0.001 | <0.001 |
| CREIGHTON_CSC_DN | −1.778 | <0.001 | <0.001 |
| Tumor progression and Metastasis Signatures | |||
| VANTVEER_BREAST_CANCER_POOR_PROGNOSIS | 1.953 | <0.001 | <0.001 |
| JAEGER_METASTASIS_UP | 1.875 | <0.001 | 0.003 |
Enrichment of gene sets from the literature (see supplementary information for references). Positive normalized enrichment score (NES) indicates enrichment in platelet-treated Ep5 cells; negative NES indicates enrichment in untreated Ep5 cells. FDR (false discovery rate).
Considering that a prolonged exposure to TGFβ promotes EMT in many cancer cell lines, including Ep5 cells (Derynck and Akhurst, 2007; Maschler et al., 2005; Oft et al., 1996), we investigated whether platelet-derived TGFβ could activate TGFβ/Smad signaling in tumor cells. We found increased levels of active and latent TGFβ1 in the medium derived from the co-culture of tumor cells and platelets, after the platelets were removed (Fig. 2C). Ep5 and MC38GFP cells treated with platelets also showed increased phosphorylation of the TGFβ signaling effector Smad2 (Fig. 2D) and Smad-binding element (SBE)-dependent transcription (Fig. 2E) compared with controls, demonstrating that interaction with platelets induces TGFβ/Smad signaling in tumor cells. We next investigated whether platelet-induced tumor cell invasion is dependent on TGFβ signaling. Interestingly, adding a TGFβRI inhibitor (SB431542) or a TGFβ1 blocking antibody abolished platelet-induced cell invasion (Fig. 2F). Treatment with SB431542 also inhibited the upregulation of EMT markers induced by platelets in Ep5 and MC38GFP cells (Fig. 2G). Thus, platelet-derived TGFβ induces a prometastatic invasive phenotype in tumor cells via activation of the TGFβ/Smad signaling pathway.
Platelet-Derived TGFβ1 is Necessary for Metastasis In Vivo
To test directly the specific contribution of platelet-derived TGFβ1 to metastasis in vivo, Pf4-cre mice (Tiedt et al., 2007) were crossed with TGFβ1fl/fl mice (Li et al., 2007) to generate mice lacking TGFβ1 specifically in their megakaryocytes and platelets. Pf4-cre+; TGFβ1fl/fl mice had normal bleeding times and platelet counts (Table S3), showing that platelet hemostatic functions are not impaired in these mice. ELISA for TGFβ1 showed that platelets from Pf4-cre+; TGFβ1fl/fl mice contained less than 1% of the amount of TGFβ1 present in platelets from wild-type (WT) mice (Fig. 3A), confirming that Pf4-cre+; TGFβ1fl/fl mice could be used to study the role of platelet-derived TGFβ1 in metastasis. Furthermore, the concentration of TGFβ1 was significantly lower in platelet-rich plasma from Pf4-cre+; TGFβ1fl/fl mice compared with plasma from WT mice (Fig. 3A), suggesting that platelets are a major source of TGFβ1 in the circulation.
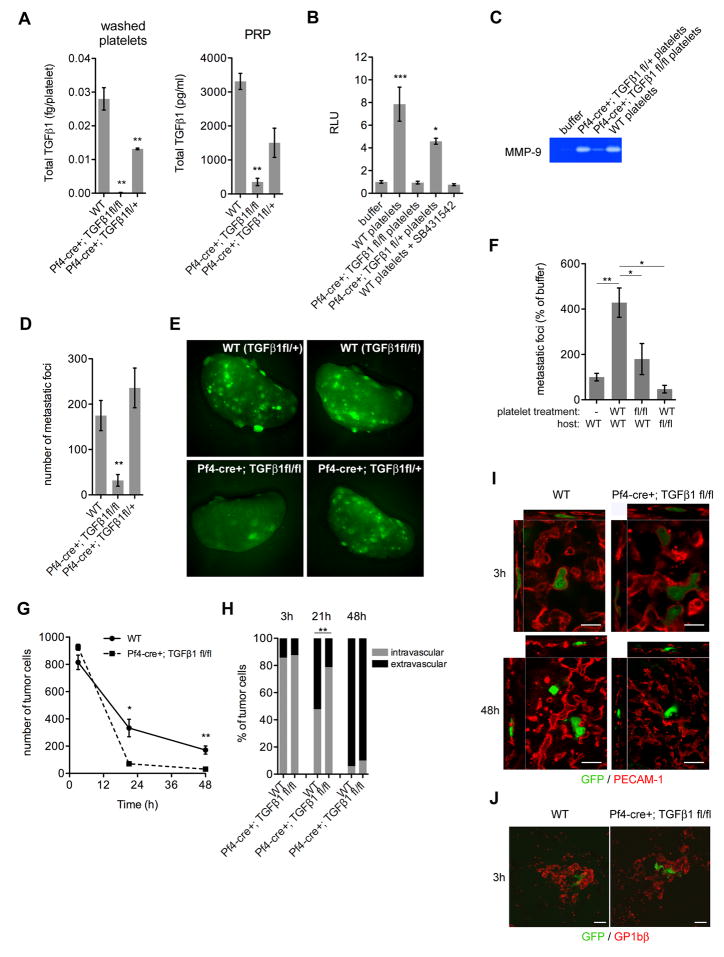
Figure 3. Platelet-Derived TGFβ Promotes Lung Metastasis.
(A) Concentration of TGFβ1 in washed platelets and platelet-rich plasma (PRP) from wild-type (WT), Pf4-cre+; TGFβ1fl/fl or Pf4-cre+; TGFβ1fl/+ mice measured by ELISA (n=2).
(B) Relative luciferase activity (RLU) in Ep5 cells stably expressing a luciferase reporter under the control of the SBE promoter and treated with buffer, platelets from wild-type (WT), Pf4-cre+; TGFβ1fl/fl, Pf4-cre+; TGFβ1fl/+, or with wild-type platelets + SB431542 (10μM) for 20h (n=3).
(C) Zymography for MMP-9 in the conditioned medium from Ep5 cells treated with buffer, platelets from wild-type (WT), Pf4-cre+; TGFβ1fl/fl or Pf4-cre+; TGFβ1fl/+ mice for 40h.
(D–E) Numbers of metastatic foci at the surface of lungs (2 largest lobes) 14 days after tail-vein injection of MC38GFP cells in wild-type (WT), Pf4-cre+; TGFβ1fl/fl or Pf4-cre+; TGFβ1fl/+ mice (n=7–9), and representative pictures of lungs (E).
(F) Numbers of metastatic foci at the surface of lungs (2 largest lobes) 14 days after tail-vein injection of MC38GFP cells pretreated with buffer (−), platelets from WT mice (WT) or platelets from Pf4-cre+; TGFβ1fl/fl (fl/fl) and injected into WT or Pf4-cre+; TGFβ1fl/fl mice (n=9–14).
(G) Numbers of tumor cells at the surface of lungs 3h, 21h and 48h after tail-vein injection of MC38GFP cells in wild-type (WT) or Pf4-cre+; TGFβ1fl/fl mice. Each point represents the mean ± SEM number of cells/view field (3X) (n=3–14). *p<0.05, **p<0.01 were determined by Student’s t-test.
(H) Percentage of intravascular and extravascular MC38GFP cells in lungs of wild-type (WT) or Pf4-cre+; TGFβ1fl/fl mice 3h, 21h and 48h after tail-vein injection of tumor cells (n=16–46 cells). **p<0.01 as determined by Fisher’s exact test.
(I–J) Confocal microcopy of lungs of wild-type (WT) or Pf4-cre+; TGFβ1fl/fl mice 3h and 48h after tail-vein injection of tumor cells for MC38GFP cells (green) and either blood vessels (H; PECAM-1 staining; red) or platelets (I; GP1bβ staining; red. Note platelet aggregates surrounding tumor cells.). Scale bar=50μm.
For panels A, B, D, and F bars represent the mean ± SEM, and *p<0.05, **p<0.01, ***p<0.001 vs WT or buffer were determined by one-way ANOVA followed by Tuckey’s post test.
We next tested whether platelets lacking TGFβ1 could induce Smad signaling and EMT markers in vitro and found a decrease in SBE-dependent luciferase reporter activity (Fig. 3B) and MMP-9 secretion by Ep5 cells, in comparison with treatment with WT platelets (Fig. 3C). Thus, while other members of the TGFβ family might be secreted by platelets, these results suggest that platelet-derived TGFβ1 is key for the platelet-induced activation of Smad signaling in cancer cells.
To test the role of platelet-derived TGFβ1 during metastasis in vivo, MC38GFP cells were injected into Pf4-cre+; TGFβ1fl/fl or WT mice via the tail vein. Fourteen days after injection, the numbers of metastases present in the lungs of Pf4-cre+; TGFβ1fl/fl mice were greatly reduced compared with those in littermate controls (WT and Pf4-cre+; TGFβ1fl/+ mice; Fig. 3D,E). Importantly, cells pretreated with platelets from WT mice and injected into Pf4-cre+; TGFβ1fl/fl mice also formed significantly fewer metastases than platelet-treated cells injected into WT mice (Fig. 3F). Conversely, pretreating tumor cells with TGFβ1-deficient platelets led to the formation of significantly fewer metastases in WT mice, in comparison to cells pretreated with platelets from WT mice (Fig. 3F; see Fig. S1A for micrographs of injected cells). Thus, while a platelet pretreatment primes tumor cells for metastasis in WT mice in a TGFβ1-dependent manner, the presence of platelet-derived TGFβ1 in the host bloodstream is also required for efficient metastasis.
We next investigated the role of platelet-derived TGFβ1 in the early steps in the seeding of metastases. Whereas equivalent numbers of cells were found in the lungs 3h after injection for both WT and Pf4-cre+; TGFβ1fl/fl mice (Fig. 3G), significantly lower numbers of cells remained in the lungs after 21h or 48h in Pf4-cre+; TGFβ1fl/fl mice (Fig. 3G). Closer inspection by confocal microscopy and 3D-rendering of lungs revealed that, at 3h post-injection, tumor cells were mainly present within the blood vessels (Fig. 3H,I) in association with platelets (Fig. 3J), while after 48h they were found mainly outside of the blood vessels in both WT and Pf4-cre+; TGFβ1fl/fl mice (Fig. 3H,I). Interestingly, at the intermediate time point of 21h, tumor cells were found both in the intravascular and extravascular compartments, and a smaller proportion of cells were localized extravascularly in the lungs of Pf4-cre+; TGFβ1fl/fl mice compared with WT, suggesting that tumor cell extravasation is impaired in Pf4-cre+; TGFβ1fl/fl mice (Fig. 3H).
Because another gene (stumpy) was also targeted in the TGFβ1fl/fl mice (Li et al., 2007; Town et al., 2008), we generated Pf4-cre+; TGFβ1fl/− and TGFβ1fl/− mice, with one null allele of TGFβ1, which allows expression of one WT allele of stumpy in these mice. The numbers of metastases observed in lungs of TGFβ1fl/− mice after 14 days were similar to those obtained for WT or Pf4-cre+; TGFβ1fl/+ mice, whereas Pf4-cre+; TGFβ1fl/− mice had reduced numbers of metastases (Fig. S2). These results show that the reduction in metastasis is not due to the deletion of stumpy, but attributable to the lack of TGFβ1. Altogether, our data reveal that platelet-derived TGFβ1 plays an important role in promoting metastatic seeding in the lungs possibly by inducing extravasation and invasion into the lung parenchyma.
Platelet-Derived TGFβ1 and Platelet-Bound Factors Cooperate to Promote Metastasis
Considering that TGFβ1 is a secreted factor released by platelets upon activation (Assoian and Sporn, 1986), we next asked whether exposure to the releasate from activated platelets would be sufficient to prime tumor cells for metastasis in vivo. Platelets were therefore activated with thrombin and the releasate was separated from the exhausted platelets by centrifugation (Neither thrombin nor its inhibitor hirudin affected tumor cell behavior in our system; Fig. S3A, B, C). Higher concentrations of active TGFβ1 were measured in the conditioned medium of tumor cells treated with the releasate than with the pellet from activated platelets, while similar amounts of total TGFβ1 were found in the conditioned medium of tumor cells treated with either fraction (Fig. 4A). Furthermore, similar levels of Smad2 phosphorylation (Fig. 4B) and SBE-based TGFβ reporter activity were induced in tumor cells incubated with the releasate or the pellet (Fig. 4C), demonstrating that the concentration of TGFβ1 present in either fraction is sufficient to induce Smad signaling to comparable levels.
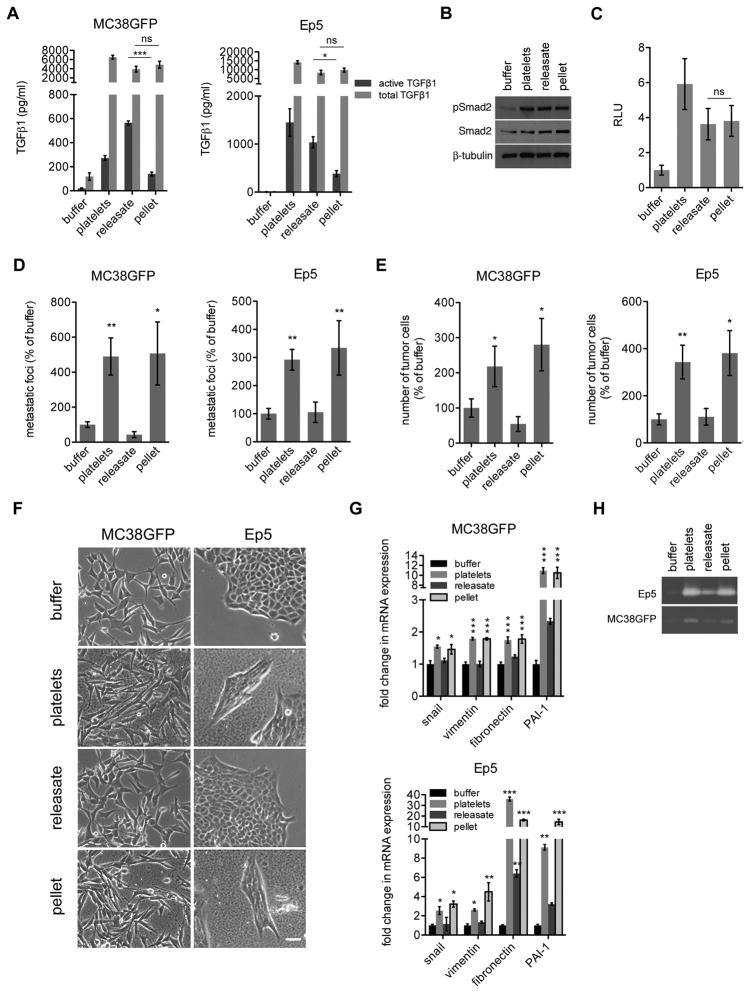
Figure 4. Platelet-Derived TGFβ1 and Platelet-Bound Factors Cooperate to Promote Metastasis.
(A) Concentration of TGFβ measured by ELISA in the conditioned medium of MC38GFP or Ep5 cells incubated with buffer, platelets, releasate from activated platelets (releasate), or the pellet fraction from activated platelets (pellet) for 40h (n=4–6).
(B) Detection of phospho-Smad2 and total Smad2 protein levels by immunoblotting in Ep5 cells treated as in (A). β-tubulin was used as loading control.
(C) Relative luciferase activity (RLU) in Ep5 cells stably expressing a luciferase reporter under the control of the SBE promoter and treated as in (A) for 20h (n=2).
(D) Numbers of metastatic foci at the surface of lungs (2 largest lobes) 14 days after tail-vein injection of MC38GFP or Ep5-ZsGreen cells pretreated with buffer, platelets, releasate from activated platelets (releasate), or the pellet fraction from activated platelets (pellet) for 40h (n=5–17).
(E) Numbers of tumor cells at the surface of lungs 48h after tail-vein injection of MC38GFP or Ep5-ZsGreen cells pretreated as in (D). Each bar represents the mean ± SEM number of cells/view field (3X) (n=5–13). *p<0.05, **p<0.01 vs buffer were determined by Student’s t-test.
(F) Phase-contrast micrographs of MC38GFP and Ep5 cells treated as in (A) for 24h. Scale bar=50μm.
(G) Relative fold change in mRNA expression in MC38GFP or Ep5 cells treated as in (A) for 40h. Values are normalized to Gapdh expression (n=3).
(H) Zymography for MMP-9 in the conditioned medium from Ep5 cells treated as in (A) for 40h.
For panels A, C, D and G, bars represent the mean ± SEM, and ns (p>0.05), *p<0.05, **p<0.01, ***p<0.001 vs buffer were determined by one-way ANOVA followed by Tuckey’s post test.
However, despite the higher concentrations of TGFβ1 present in the conditioned medium of tumor cells treated with the platelet releasate (Fig. 4A), increased numbers of lung metastases were observed only when tumor cells were preincubated with the pellet fraction but not with the releasate from activated platelets (Fig. 4D). Additionally, tumor cell retention in the lungs was increased 48h after tail-vein injection when cells were pretreated with platelets or the pellet fraction but not after treatment with the releasate (Fig. 4E). Consistent with these results, cells adopted a more mesenchymal morphology (Fig. 4F) and showed higher expression of prometastatic genes (Fig. 4G and Fig. S3D), increased secretion of MMP-9 (Fig. 4H), and increased invasion (Fig. S3E) upon incubation with the platelet pellet fraction but not with the platelet releasate. Furthermore, microarray analysis of pellet- or releasate-treated Ep5 cells revealed that treatment with the pellet fraction induced gene expression changes very similar to those observed upon platelet treatment (Fig. S3F, G). However, treatment with the platelet releasate resulted in only partial gene expression changes in comparison with treatment with either platelets or the pellet fraction (Fig. S3F-I). Gene expression signatures associated with EMT and tumor progression were also robustly enriched in the pellet-treated cells but not in the releasate-treated cells (Table S4). Thus, platelet-induced effects on EMT, invasion, and metastasis are not mediated by secreted TGFβ alone, but also require additional platelet-bound factors. These data also suggest that these platelet-bound factors synergize with TGFβ to enhance metastasis.
TGFβ1 and Direct Platelet-Tumor Cell Contact Synergize to Promote Prometastatic Gene Expression
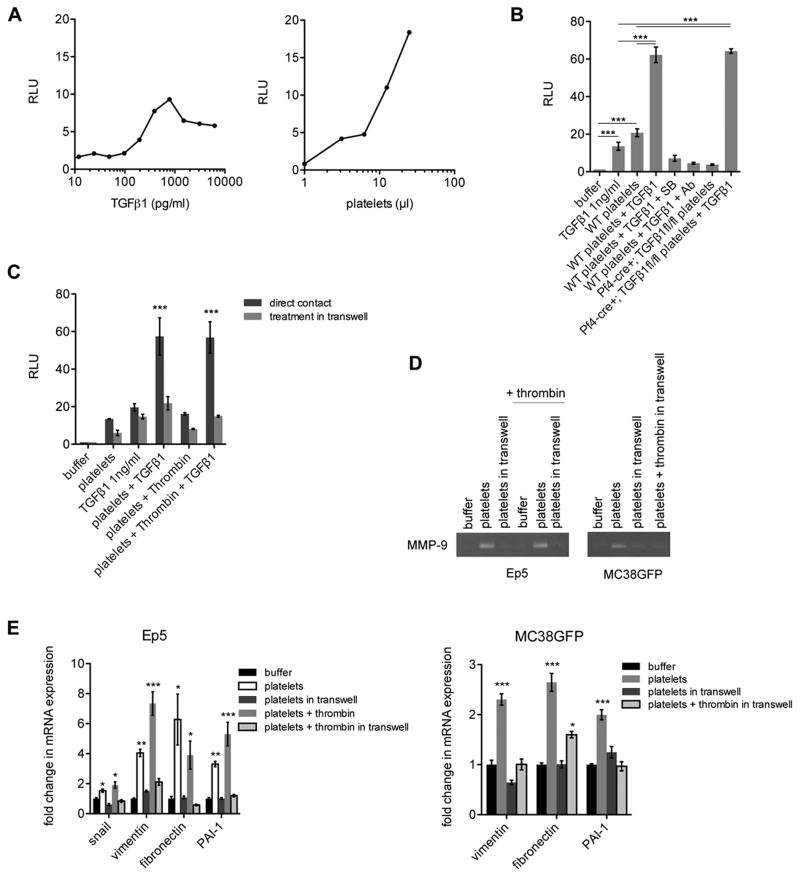
To test further whether platelets synergize with TGFβ signaling, we used the MLEC cell line stably expressing a luciferase reporter based on the promoter region of the TGFβ target gene PAI-1 (Abe et al., 1994). These cells provide a specific readout for exogenous TGFβ bioavailability and signaling activity, and were therefore used to dissect the specific contribution of TGFβ signaling to the effects observed upon platelet treatment. Interestingly, we found that platelets induced higher luciferase activity than achievable with TGFβ1 treatment alone (Fig. 5A). Furthermore, adding TGFβ1 together with platelets from either WT or Pf4-cre+; TGFβ1fl/fl mice resulted in a synergistic activation of the PAI-1 reporter that was completely blocked by adding either a TGFβRI inhibitor (SB431542) or an anti-TGFβ1 blocking antibody (Fig. 5B). Moreover, separation of platelets (either resting or activated with thrombin) from the cancer cells by a semipermeable membrane blocked the synergistic activation of the PAI-1 promoter (Fig. 5C), inhibited the secretion of MMP-9 (Fig. 5D), and abolished the upregulation of prometastatic genes in Ep5 and MC38GFP cells (Fig. 5E). Taken together, these results show that platelet-derived TGFβ1 is necessary to induce the expression of several prometastatic genes and to promote metastasis in vivo but that, in addition, platelets provide other prometastatic signals that synergize with TGFβ signaling upon direct platelet-tumor cell contact.
Figure 5. TGFβ1 and Direct Platelet-Tumor Cell Contact Synergize to Promote Prometastatic Gene Expression.
(A) Relative luciferase activity (RLU) in MLEC cells stably expressing a luciferase reporter under the control of a TGFβ responsive PAI-1 promoter construct and treated with different concentrations of TGFβ1 (left panel) or platelets (right panel). Note that the y-axis scale is the same for both panels and that platelets give higher stimulation than achievable with TGFβ1 alone.
(B) Relative luciferase activity (RLU) in MLEC cells stably expressing a luciferase reporter under the control of a PAI-1 promoter construct treated with buffer, platelets from WT or Pf4-cre+; TGFβ1fl/fl mice, TGFβ1 1ng/ml or with combinations of platelets + TGFβ1 1ng/ml, +/− SB431542 (SB; 10μM) or +/− TGFβ1 blocking antibody (Ab; 6μg/ml)(n=3–16).
(C) Relative luciferase activity (RLU) in MLEC cells stably expressing a luciferase reporter under the control of a PAI-1 promoter construct treated with buffer, platelets, or thrombin-activated platelets +/− 1ng/ml TGFβ1 seeded either at the bottom (direct contact with tumor cells) or in the upper chamber of a transwell (0.4μm pore size) to prevent direct contact between platelets and tumor cells (n=2–3).
(D) Zymography for MMP-9 in the conditioned medium from Ep5 or MC38GFP cells treated with buffer, platelets, or thrombin-activated platelets seeded either at the bottom or in the upper chamber of a transwell (0.4μm pore size).
(E) Relative fold change in mRNA expression in Ep5 or MC38GFP cells treated as in (D) (n=3). Values are normalized to Gapdh expression.
For panels B, C and E, bars represent the mean ± SEM, and *p<0.05, **p<0.01, ***p<0.001 vs buffer (unless otherwise indicated) were determined by one-way ANOVA followed by Tuckey’s post test.
The NF-κB Signaling Pathway is Activated by Platelets in a Contact-Dependent Manner and Cooperates with TGFβ Signaling to Enhance Metastasis
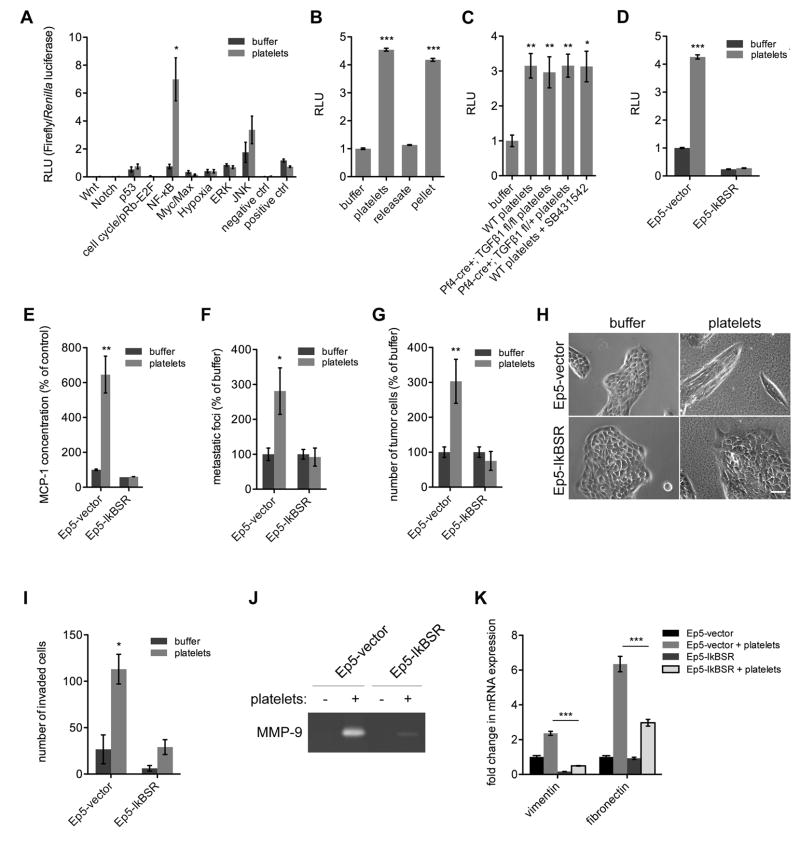
We next sought to define the molecular pathway(s) induced upon platelet contact that cooperate with TGFβ to induce prometastatic gene expression and behavior. Using a set of luciferase reporter assays for several pathways involved in cancer, we screened for their activation in cancer cells in response to interaction with platelets. Interestingly, coincubation with platelets increased activation of the JNK and NF-κB pathways in Ep5 cells (Fig. 6A). While the JNK pathway seemed to be activated by the releasate, activation of the NF-κB pathway was increased only when cells were incubated with either platelets or the pellet fraction from activated platelets (Fig. S4A). Ep5 cells stably expressing an NF-κB luciferase reporter also displayed increased luciferase activity upon treatment with platelets or activated platelet pellets but not if treated with the releasate (Fig. 6B). Furthermore, secretion of MCP-1, a known target of the NF-κB pathway, was increased in the supernatant of Ep5 and MC38GFP tumor cells treated with platelets or the pellet fraction, further showing that platelet-bound factors activate the NF-κB pathway in tumor cells (Fig. S4B). Notably, many of the genes found to be highly upregulated in the platelet-induced gene signature, such as Ccl2 (MCP-1), Mmp9, Vegfc, Tnc, Serpine1, Jag1 and Ncam1 have been previously reported as NF-κB target genes (Fig. 2A and Table S1). Furthermore, GSEA analysis revealed that NF-κB-related gene signatures are enriched in platelet- or platelet pellet-treated Ep5 cells, but not in platelet releasate-treated cells (Table S4). Importantly, treatment of tumor cells with either TGFβ1-deficient platelets or with wild-type platelets together with the TGFβRI inhibitor SB431542 still led to activation of the NF-κB pathway reporter (Fig. 6C), ruling out the possibility that activation of the NF-κB pathway is TGFβ1-dependent in this context.
Figure 6. The NF-κB Signaling Pathway is Activated by Platelets in a Contact-Dependent Manner and Cooperates with TGFβ Signaling to Induce an EMT-Like Transition and Promote Metastasis.
(A) Ep5 cells were transfected with pathway-specific firefly luciferase reporters and constitutively expressed control Renilla luciferase reporters. 24h after transfection, cells were treated with buffer or platelets for 20h, and the relative luciferase activity (RLU) was measured. Firefly luciferase activity was normalized to Renilla luciferase activity. Each bar represents the mean ± SEM of n=3. *p<0.05 was determined by Student’s t-test.
(B) Relative luciferase activity (RLU) in Ep5 cells stably expressing an NF-κB luciferase reporter and treated with buffer, platelets, releasate from activated platelets (releasate), or the pellet fraction from activated platelets (pellet) for 20h (n=2).
(C) Relative luciferase activity (RLU) in Ep5 cells stably expressing a NF-κB luciferase reporter and treated with buffer, platelets from wild-type (WT), Pf4-cre+; TGFβ1fl/fl, Pf4-cre+; TGFβ1fl/+ mice or with wild-type platelets + SB431542 (10μM) for 20h (n=5).
(D) Relative luciferase activity (RLU) in Ep5 cells stably expressing a NF-κB luciferase reporter and either a IκB super-repressor (Ep5-IkBSR) or a control vector (Ep5-vector) and treated with buffer or platelets for 20h (n=4).
(E) MCP-1 concentration in the conditioned medium from Ep5 cells stably expressing an IκB super-repressor (Ep5-IkBSR) or a control vector (Ep5-vector) and treated with buffer or platelets for 20h (n=2).
(F) Numbers of metastatic foci at the surface of lungs (2 largest lobes) 14 days after tail-vein injection of Ep5-IkBSR and Ep5-vector cells pretreated with buffer or platelets for 40h. Each bar represents the mean ± SEM of n=5–7. *p<0.05 was determined by Student’s t-test.
(G) Numbers of tumor cells at the surface of lungs 48h after tail-vein injection of Ep5-IkBSR and Ep5-vector cells pretreated with buffer or platelets for 40h. Each bar represents the mean ± SEM of n=4–7 **p<0.01 was determined by Student’s t-test.
(H) Phase-contrast micrographs of Ep5-IkBSR and Ep5-vector cells treated with buffer or platelets for 24h. Scale bar=50μm.
(I) Ep5-IkBSR and Ep5-vector cells were added at the top of transwells coated with Matrigel and treated with buffer or platelets. The total numbers of cells that invaded to the bottom of the transwell were counted after 48h (n=2).
(J) Zymography for MMP-9 in the conditioned medium from Ep5-IkBSR and Ep5-vector cells treated with buffer or platelets for 40h.
(K) Relative fold change in mRNA expression in Ep5-IkBSR and Ep5-vector cells treated as in (J) (n=3). Values are normalized to Gapdh expression.
For panels B, C and K, bars represent the mean ± SEM, and *p<0.05, **p<0.01, ***p<0.001 vs buffer were determined by one-way ANOVA followed by Tuckey’s post test. For panels D, E and I, bars represent the mean ± SEM, and *p<0.05 vs buffer was determined by two-way ANOVA followed by Bonferroni’s post test.
See also Figure S4.
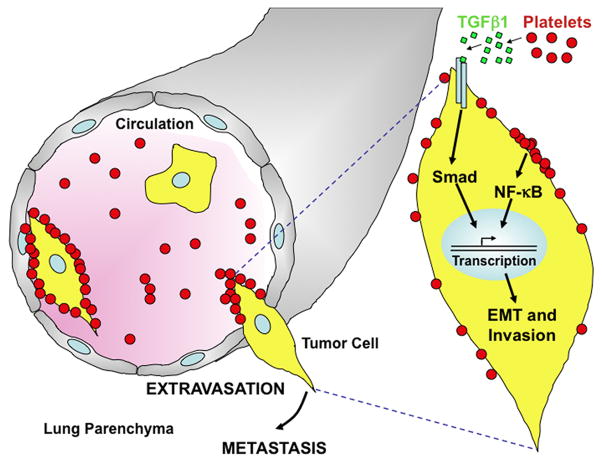
To study whether NF-κB signaling contributes to the prometastatic phenotype observed upon platelet contact, we established Ep5 cells stably expressing an IκBα mutant (IκBαS32A/S36A) which cannot be phosphorylated or degraded and therefore irreversibly sequesters NF-κB in the cytoplasm, and inhibits its function (IκBα super-repressor; Ep5-IkBSR; Brown et al., 1995). In contrast to Ep5 expressing a control vector (Ep5-vector), Ep5-IkBSR cells failed to activate an NF-κB-dependent luciferase reporter and did not express increased levels of MCP-1 following platelet treatment, demonstrating that the NF-κB signaling is blocked in these cells (Fig. 6D,E). Importantly, pretreatment of Ep5-vector cells with platelets prior to tail-vein injection led to increased numbers of metastases, while it failed to enhance metastasis of Ep5-IkBSR cells (Fig. 6F). Similarly, retention of Ep5-IkBSR cells in the lungs after 48h was not enhanced by a pretreatment with platelets, showing that the NF-κB pathway is necessary for the prometastatic effects of platelets on tumor cells (Fig. 6G). Furthermore, Ep5-IkBSR cells did not acquire a mesenchymal morphology (Fig. 6H) and did not display increased invasion (Fig. 6I) in response to treatment with platelets. These results correlated with lower levels of MMP-9 secretion (Fig. 6J) and lower vimentin and fibronectin gene expression (Fig. 6K) by Ep5-IkBSR cells following platelet treatment. The inhibition of platelet prometastatic effects was not due to an impairment of TGFβ/Smad signaling pathway by the IkBSR construct because Smad2 phosphorylation levels were intact in Ep5-IkBSR cells (Fig. S4C). In addition, inhibition of MMP-9 secretion and vimentin protein expression induced upon platelet treatment were also observed when Ep5 cells were treated with JSH-23, a pharmacological inhibitor of the NF-κB pathway (Fig. S4D,E). JSH-23 treatment also abolished the synergy observed on PAI-1 reporter activity between TGFβ1 and platelets (Fig. S4F), but had no effect on SBE-reporter activity (Fig. S4G). This finding further demonstrates that platelets activate NF-κB independently of TGFβ/Smad signaling, and cooperate with TGFβ1 to induce an EMT-like transformation in cancer cells. Thus, the ability of platelets to prime tumor cells for metastasis depends on the synergistic interaction between the NF-κB and TGFβ signaling pathways, which is triggered by direct platelet-tumor cell contact (Fig. 7).
Figure 7. Platelet-Tumor Cell Contact and Platelet-Derived TGFβ1 Synergize to Promote an EMT-Like Transition and Metastasis.
Platelets secrete TGFβ1, which activates the TGFβ/Smad pathway in tumor cells. Upon direct platelet-tumor cell contact, the NF-κB pathway is also activated in tumor cells and synergizes with TGFβ/Smad signaling to induce a rapid EMT, enhance invasiveness and promote metastasis. Activation of neither the TGFβ/Smad nor the NF-κB pathway alone is sufficient to promote metastasis. Thus, platelet-tumor cell contact triggers a synergistic interaction between TGFβ/Smad and NF-κB pathways that is necessary for efficient metastasis. The metastatic potential of tumor cells therefore continues to evolve outside of the primary tumor site in response to platelet-to-tumor cell signaling.
DISCUSSION
Signals provided by the primary tumor microenvironment are important modulators of the capacity of tumor cells to invade, access the vasculature, and metastasize (Joyce and Pollard, 2009; Nguyen et al., 2009). However, the metastatic potential of tumor cells may be further defined in response to signals provided during their intravascular transit. Here, we have tested this hypothesis and show that platelets present in the bloodstream actively signal to tumor cells to promote their metastatic potential outside of the primary microenvironment. This effect is independent of any direct contribution of platelets to immunosurveillance, adhesion, or physical shielding functions, as tumor cells can be primed for metastasis by a transient exposure to purified platelets in vitro. Mechanistically, a transient contact between platelets and tumor cells is sufficient to induce a prometastatic gene expression signature, induce an EMT-like transformation and invasive behavior in vitro, and promote extravasation and metastatic seeding in the lungs in vivo (Fig. 7). Considering that tumor cells would normally interact with platelets once in the bloodstream, these results suggest that tumor cells could gain a more mesenchymal phenotype and increased metastatic capacities after leaving the primary tumor microenvironment. This implies that cells that have intravasated without losing their epithelial properties either via leaky blood vessels (Carmeliet and Jain, 2000; Mazzone et al., 2009) or via collective invasion mechanisms (Friedl and Gilmour, 2009) could acquire a mesenchymal phenotype during their transit in the vasculature. In support of this idea, circulating tumor cells have been found to express epithelial markers (EpCAM, cytokeratins), suggesting that EMT is not absolutely required to access the blood flow (Nagrath et al., 2007). Thus, interactions with platelets may be particularly important in mediating extravasation of circulating epithelial tumor cells, and to maintain or further enhance the extravasation potential of circulating mesenchymal tumor cells. In this respect, it would be interesting to define the impact of platelets on gene expression and metastatic potential of circulating tumor cells from cancer patients.
Several signaling molecules, including TGFβ, PDGF, VEGF and angiopoietin are abundant in platelets (Erpenbeck and Schon, 2010; Sierko and Wojtukiewicz, 2007) and may therefore impact tumor cell behavior and induce EMT. Our results show that the prometastatic effects of platelets are in large part mediated via activation of the TGFβ signaling pathway, and that abrogating either TGFβ signaling in tumor cells or TGFβ expression by platelets is sufficient to inhibit metastasis and EMT. While TGFβ has been implicated in the induction of a prometastatic phenotype in many contexts (Padua et al., 2008; Siegel et al., 2003), the relevant cellular source of TGFβ bioavailable to circulating tumor cells, particularly at the site of metastatic extravasation, was previously unclear.
Our results strongly indicate that platelets are an important source of bioavailable TGFβ for tumor cells in the circulation and at the site of extravasation. This finding is supported by the observation that platelets contain concentrations of TGFβ1 many-fold higher than most cell types (Assoian et al., 1983). Furthermore, the amount of TGFβ1 produced by other cells and taken up by platelets seems minimal, as purified platelets from Pf4-cre+; TGFβ1fl/fl mice contained less than 1% of the amount of TGFβ1 present in platelets from WT mice.
Most importantly, we show that abrogation of TGFβ1 expression solely in platelets and megakaryocytes is sufficient to inhibit metastasis and prevent the seeding of tumor cells in the lungs. Furthermore, the presence of platelet-derived TGFβ1 “in situ” in the host bloodstream is crucial for metastasis, since pretreating tumor cells with platelets from WT mice fails to enhance metastasis formation in mice lacking TGFβ1 in their platelets. Because platelet-tumor cell interactions are transient and occur only within the first 24h ((Laubli et al., 2006), and data not shown), we propose that platelets could provide a pulse of TGFβ1 to circulating tumor cells, which would allow them to gain a more invasive, mesenchymal-like phenotype and extravasate. Along these lines, previous studies have shown that tumor cells transiently exposed to TGFβ1 have an enhanced capacity to seed the lungs, whereas cells that are continuously exposed to TGFβ1 have decreased metastatic capacity due to the cytostatic effect of TGFβ1 (Giampieri et al., 2009; Padua et al., 2008). In this respect, specific therapeutic inhibition of platelet-derived TGFβ1 might result in the impairment of tumor cell extravasation at the metastatic site. Importantly, Pf4-cre+; TGFβ1fl/fl mice maintain normal platelet counts and hemostatic functions, suggesting that pharmacological inhibition of platelet-derived TGFβ could inhibit metastasis without adverse effects on physiological hemostasis.
We also find that, although required for metastasis, activation of TGFβ signaling alone is unable to generate effects of the magnitude of those observed with platelets. Indeed, while tumor cells treated for 24h with platelets or with the pellet fraction from activated platelets undergo EMT, cells treated with the releasate of activated platelets (which contained a similar concentration of TGFβ1) do not. In line with this result, a prolonged treatment with TGFβ1 – typically 1 week or longer – is needed to induce EMT in several epithelial cancer cell lines including Ep5 cells (Labelle et al., 2008; Mani et al., 2008; Maschler et al., 2005). Our data further support the existence of additional platelet-bound factors synergizing with TGFβ1. First, platelets induce the TGFβ-responsive PAI-1 reporter to levels higher than achievable with TGFβ1 alone. Second, combining exogenous TGFβ1 with platelets from either WT or Pf4-cre+; TGFβ1fl/fl mice results in a synergistic activation of the PAI-1 reporter. Lastly, the synergistic effects on PAI-1 reporter activity as well as the induction of prometastatic genes are blocked if platelets are separated from tumor cells by a semipermeable membrane. Thus, our results clearly demonstrate that additional platelet-bound factors synergize with TGFβ1 to promote metastasis, and to induce a prometastatic EMT program in tumor cells. In particular, we show that this synergy is dependent on the activation of the NF-κB pathway, which is specifically triggered upon direct contact between tumor cells and platelets independently from TGFβ activity.
NF-κB regulates the expression of proinflammatory genes and has been associated with increased metastasis and EMT induction (Huber et al., 2004; Lin and Karin, 2007). For example, NF-κB promotes osteolytic bone metastasis by inducing the proinflammatory cytokine GM-CSF (Park et al., 2007). Notably, the activation of NF-κB has also been proposed to be part of the mechanism allowing TGFβ signaling to switch from a cytostatic to a prometastatic signal (Neil and Schiemann, 2008). In support of this idea, we found that NF-κB activation potentiates TGFβ-induced prometastatic gene expression, and that NF-κB signaling is necessary for the induction of EMT and efficient metastatic seeding upon platelet-cancer cell interactions. Thus, platelet-tumor cell contacts during metastasis potentiate tumor cell transcriptional responses to TGFβ via NF-κB activation.
In conclusion, we establish platelets as a crucial source of TGFβ bioavailable to tumor cells in the vasculature and necessary for tumor cell extravasation and metastasis formation. Importantly, our study reveals that platelets are more than physical shields and actively signal to tumor cells via the TGFβ and NF-κB pathways to potently induce a prometastatic phenotype. We thus propose a model whereby the metastatic potential of tumor cells continues to evolve outside of the primary tumor site, in response to tumor-host interactions in the bloodstream and at the site of metastasis. In particular, we identify platelet-tumor cell interactions and the signaling pathways that they trigger as fundamental determinants of cancer metastasis that may provide the basis for developing effective anti-metastatic therapies.
EXPERIMENTAL PROCEDURES
Mice
Mice homozygous for the TGFβ1 floxed allele (TGFβ1fl/fl; obtained from R. Flavell; Li et al., 2007) on a C57BL/6 genetic background were crossed with Pf4-cre mice on a C57BL/6 background (obtained from S. Shattil; Tiedt et al., 2007). To obtain mice with TGFβ1-deficient platelets, Pf4-cre+; TGFβ1fl/+ mice were bred with TGFβ1fl/fl or TGFβ1fl/+ mice. TGFβ1+/− mice (the null allele was obtained by egfp knockin, which disrupted TGFβ1 without affecting stumpy; Li et al., 2007) were crossed with Pf4-cre+; TGFβ1fl/fl mice to obtain Pf4-cre+; TGFβ1fl/− mice. For genotyping primers, see Supplemental Experimental Procedures. All mice were housed and handled in accordance with approved Massachusetts Institute of Technology Division of Comparative Medicine protocols.
Generation of Cell Lines Stably Expressing ZsGreen, IkBSR and Luciferase-based Reporters
Retroviral vectors coding for ZsGreen or IκBα super-repressor plus GFP (IkBSR) were transduced into Ep5 cells as described previously (Stern et al., 2008) and in Supplemental Experimental Procedures. Ep5 and MC38GFP cell lines stably expressing SBE (AGCCAGACA tandem repeats)-luciferase and NF-κB (GGGACTTTCC tandem repeats)-luciferase reporter constructs were generated by infecting cells with Cignal Lenti Reporter vectors (SABiosciences) according to manufacturers’ instructions.
Preparation of Platelets and Platelet Fractions
Mouse blood was collected by cardiac puncture and washed platelets were prepared as described previously (Frenette et al., 1995; Hartwell et al., 1998). To prepare platelet fractions, platelets were activated with thrombin 0.5U/ml for 15 min at 37°C. The pellet fraction was separated from the releasate (supernatant) by centrifugation at 2,800g for 7 min.
Treatment of Tumor Cells with Platelets
Cells were seeded in DMEM 10% FCS and incubated overnight. Immediately prior to treatment the medium was changed for fresh DMEM. 150,000 platelets/μl and equivalent volumes of releasate and pellet fractions were added. Where indicated, cells were treated with 1 or 10ng/ml of recombinant TGFβ1 (R&D Systems), 10μM SB431542 (Sigma), or 6μg/ml anti-TGFβ1 blocking antibody (R&D systems).
In vivo Metastasis Assays
For lung metastasis assays, cells treated with platelets for 40h were washed in PBS, and either trypsinized (Ep5) or lifted with 2mM EDTA in PBS (MC38GFP). Cells were then washed and centrifuged twice to remove platelets, and resuspended in HBSS at a constant number of cells for all mice in a given experiment (250,000 to 1,000,000 cells/injection). 100μl of cell suspension were then injected via the tail vein of syngeneic mice. The numbers of single cells and metastatic foci were determined as described in Supplemental Experimental Procedures.
Microarray Analysis
Total RNA was isolated from platelet-treated or untreated Ep5 cells (n=5). In order to detect mRNAs contributed by platelets, RNA was also isolated from platelet lysates mixed with untreated Ep5 cells lysates immediately prior to RNA isolation (n=3)(The concentration of RNA isolated from platelets alone was below detection limits and could therefore not be used for microarray analysis). cRNA was then synthesized and hybridized onto GeneChip Mouse Exon 1.0 ST Arrays (Affymetrix).
Luciferase Assay
15,000 Ep5 cells/50 μl Opti-MEM well were plated in a 96-well Cignal Finder Multi Pathway reporter Array plate as recommended by the manufacturer (SABiosciences) and incubated for 24h. The medium was then changed and cells were treated with platelets or platelet fractions. The ratios of Firefly to Renilla Luciferase activities (Relative Light Units; RLU) were measured in cell lysates with the Dual Luciferase Reporter Assay System (Promega) 24h after treatment with platelets.
TGFβ1 ELISA
TGFβ1 levels were detected in tissue-culture-conditioned medium (40h), washed platelets or platelet-rich plasma either by direct assay (active TGFβ1) or following acid treatment to activate latent TGFβ1 (total TGFβ1) with the Quantikine TGFβ1 immunoassay kit (R&D Systems).
MCP-1 Detection
Concentration of MCP-1 in conditioned medium of Ep5 or MC38GFP cells was analyzed with CBA soluble Flex Set cytometric beads, following manufacturer’s instructions (BD Biosciences).
Statistics
Statistical analyses were performed with the GraphPad Prism Software following guidelines found in (Bremer and Doerge, 2010) and in GraphPad Prism. Briefly, the Student’s t-test was used to compare means of two independent groups to each other, while one-way ANOVA followed by Tuckey’s post test was used to compare the means of more than two independent groups. Two-way ANOVA followed by Bonferroni’s post test was used to compare the means of groups influenced by two independent factors.
Accession Number
Microarray data are deposited in Gene Expression Omnibus under accession number GSE27456.
Supplementary Material
HIGHLIGHTS.
Platelet-tumor cell contacts induce a mesenchymal-like metastatic phenotype
Platelet-derived TGFβ1 is necessary but not sufficient for efficient metastasis
NF-κB signaling is also necessary but not sufficient and synergizes with TGFβ
Signals provided outside the primary tumor microenvironment promote metastasis
SIGNIFICANCE.
The host-to-tumor signaling events governing cancer metastasis are poorly understood. We explored the possibility that the metastatic potential of tumor cells is modulated during their transit through the bloodstream. Our findings indicate that direct contact with platelets primes tumor cells for metastasis, and induces an epithelial-mesenchymal-like transition via synergistic activation of both the TGFβ and NF-κB pathways. Specific ablation of platelet-derived TGFβ or NF-κB signaling in cancer cells prevents metastasis. Globally, our study reveals that the metastatic potential of tumor cells continues to evolve outside the primary tumor site, in response to tumor-host interactions in the bloodstream. Platelet-tumor cell interactions and the signaling pathways that they trigger are therefore crucial determinants of cancer metastasis and potential targets for anti-metastatic therapies.
Acknowledgments
We are grateful to Patrick Stern for viral vectors driving ZsGreen and IkBSR expression, and to Richard Flavell and Sanford Shattil for mouse strains. We thank Charlie Whittaker (Swanson Biotechnology Center, Koch Institute) for assistance with microarray analysis, members of the Hynes lab for advice, and John Lamar and Patrick Stern for critically reading the manuscript. This work was supported by the Ludwig Center for Molecular Oncology at MIT, by the Koch Institute at MIT and by the Howard Hughes Medical Institute of which ROH is an Investigator. ML was supported by a postdoctoral fellowship from the Anna Fuller Fund.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abe M, Harpel JG, Metz CN, Nunes I, Loskutoff DJ, Rifkin DB. An assay for transforming growth factor-beta using cells transfected with a plasminogen activator inhibitor-1 promoter-luciferase construct. Anal Biochem. 1994;216:276–284. doi: 10.1006/abio.1994.1042. [DOI] [PubMed] [Google Scholar]
- Assoian RK, Komoriya A, Meyers CA, Miller DM, Sporn MB. Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J Biol Chem. 1983;258:7155–7160. [PubMed] [Google Scholar]
- Assoian RK, Sporn MB. Type beta transforming growth factor in human platelets: release during platelet degranulation and action on vascular smooth muscle cells. J Cell Biol. 1986;102:1217–1223. doi: 10.1083/jcb.102.4.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakewell SJ, Nestor P, Prasad S, Tomasson MH, Dowland N, Mehrotra M, Scarborough R, Kanter J, Abe K, Phillips D, et al. Platelet and osteoclast beta3 integrins are critical for bone metastasis. Proc Natl Acad Sci U S A. 2003;100:14205–14210. doi: 10.1073/pnas.2234372100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas S, Guix M, Rinehart C, Dugger TC, Chytil A, Moses HL, Freeman ML, Arteaga CL. Inhibition of TGF-beta with neutralizing antibodies prevents radiation-induced acceleration of metastatic cancer progression. J Clin Invest. 2007;117:1305–1313. doi: 10.1172/JCI30740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremer M, Doerge RW. Statistics at the bench: A step-by step handbook for biologists. Cold Spring Harbor: Cold Spring Harbor Laboratory Press; 2010. [Google Scholar]
- Brown K, Gerstberger S, Carlson L, Franzoso G, Siebenlist U. Control of I kappa B-alpha proteolysis by site-specific, signal-induced phosphorylation. Science. 1995;267:1485–1488. doi: 10.1126/science.7878466. [DOI] [PubMed] [Google Scholar]
- Camerer E, Qazi AA, Duong DN, Cornelissen I, Advincula R, Coughlin SR. Platelets, protease-activated receptors, and fibrinogen in hematogenous metastasis. Blood. 2004;104:397–401. doi: 10.1182/blood-2004-02-0434. [DOI] [PubMed] [Google Scholar]
- Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407:249–257. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- Corbett TH, Griswold DP, Jr, Roberts BJ, Peckham JC, Schabel FM., Jr Tumor induction relationships in development of transplantable cancers of the colon in mice for chemotherapy assays, with a note on carcinogen structure. Cancer Res. 1975;35:2434–2439. [PubMed] [Google Scholar]
- Derynck R, Akhurst RJ. Differentiation plasticity regulated by TGF-beta family proteins in development and disease. Nat Cell Biol. 2007;9:1000–1004. doi: 10.1038/ncb434. [DOI] [PubMed] [Google Scholar]
- Erpenbeck L, Schon MP. Deadly allies: the fatal interplay between platelets and metastasizing cancer cells. Blood. 2010;115:3427–3436. doi: 10.1182/blood-2009-10-247296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenette PS, Johnson RC, Hynes RO, Wagner DD. Platelets roll on stimulated endothelium in vivo: an interaction mediated by endothelial P-selectin. Proc Natl Acad Sci U S A. 1995;92:7450–7454. doi: 10.1073/pnas.92.16.7450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedl P, Gilmour D. Collective cell migration in morphogenesis, regeneration and cancer. Nat Rev Mol Cell Biol. 2009;10:445–457. doi: 10.1038/nrm2720. [DOI] [PubMed] [Google Scholar]
- Gasic GJ, Gasic TB, Stewart CC. Antimetastatic effects associated with platelet reduction. Proc Natl Acad Sci U S A. 1968;61:46–52. doi: 10.1073/pnas.61.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay LJ, Felding-Habermann B. Contribution of platelets to tumour metastasis. Nat Rev Cancer. 2011;11:123–134. doi: 10.1038/nrc3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giampieri S, Manning C, Hooper S, Jones L, Hill CS, Sahai E. Localized and reversible TGFbeta signalling switches breast cancer cells from cohesive to single cell motility. Nat Cell Biol. 2009;11:1287–1296. doi: 10.1038/ncb1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartwell DW, Mayadas TN, Berger G, Frenette PS, Rayburn H, Hynes RO, Wagner DD. Role of P-selectin cytoplasmic domain in granular targeting in vivo and in early inflammatory responses. J Cell Biol. 1998;143:1129–1141. doi: 10.1083/jcb.143.4.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber MA, Azoitei N, Baumann B, Grunert S, Sommer A, Pehamberger H, Kraut N, Beug H, Wirth T. NF-kappaB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J Clin Invest. 2004;114:569–581. doi: 10.1172/JCI21358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im JH, Fu W, Wang H, Bhatia SK, Hammer DA, Kowalska MA, Muschel RJ. Coagulation facilitates tumor cell spreading in the pulmonary vasculature during early metastatic colony formation. Cancer Res. 2004;64:8613–8619. doi: 10.1158/0008-5472.CAN-04-2078. [DOI] [PubMed] [Google Scholar]
- Jain S, Zuka M, Liu J, Russell S, Dent J, Guerrero JA, Forsyth J, Maruszak B, Gartner TK, Felding-Habermann B, et al. Platelet glycoprotein Ib alpha supports experimental lung metastasis. Proc Natl Acad Sci U S A. 2007;104:9024–9028. doi: 10.1073/pnas.0700625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y, He W, Tulley S, Gupta GP, Serganova I, Chen CR, Manova-Todorova K, Blasberg R, Gerald WL, Massague J. Breast cancer bone metastasis mediated by the Smad tumor suppressor pathway. Proc Natl Acad Sci U S A. 2005;102:13909–13914. doi: 10.1073/pnas.0506517102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpatkin S, Pearlstein E, Ambrogio C, Coller BS. Role of adhesive proteins in platelet tumor interaction in vitro and metastasis formation in vivo. J Clin Invest. 1988;81:1012–1019. doi: 10.1172/JCI113411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YJ, Borsig L, Varki NM, Varki A. P-selectin deficiency attenuates tumor growth and metastasis. Proc Natl Acad Sci U S A. 1998;95:9325–9330. doi: 10.1073/pnas.95.16.9325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labelle M, Schnittler HJ, Aust DE, Friedrich K, Baretton G, Vestweber D, Breier G. Vascular endothelial cadherin promotes breast cancer progression via transforming growth factor beta signaling. Cancer Res. 2008;68:1388–1397. doi: 10.1158/0008-5472.CAN-07-2706. [DOI] [PubMed] [Google Scholar]
- Laubli H, Stevenson JL, Varki A, Varki NM, Borsig L. L-selectin facilitation of metastasis involves temporal induction of Fut7-dependent ligands at sites of tumor cell arrest. Cancer Res. 2006;66:1536–1542. doi: 10.1158/0008-5472.CAN-05-3121. [DOI] [PubMed] [Google Scholar]
- Li MO, Wan YY, Flavell RA. T cell-produced transforming growth factor-beta1 controls T cell tolerance and regulates Th1- and Th17-cell differentiation. Immunity. 2007;26:579–591. doi: 10.1016/j.immuni.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117:1175–1183. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maschler S, Wirl G, Spring H, Bredow DV, Sordat I, Beug H, Reichmann E. Tumor cell invasiveness correlates with changes in integrin expression and localization. Oncogene. 2005;24:2032–2041. doi: 10.1038/sj.onc.1208423. [DOI] [PubMed] [Google Scholar]
- Mazzone M, Dettori D, Leite de Oliveira R, Loges S, Schmidt T, Jonckx B, Tian YM, Lanahan AA, Pollard P, Ruiz de Almodovar C, et al. Heterozygous deficiency of PHD2 restores tumor oxygenation and inhibits metastasis via endothelial normalization. Cell. 2009;136:839–851. doi: 10.1016/j.cell.2009.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagrath S, Sequist LV, Maheswaran S, Bell DW, Irimia D, Ulkus L, Smith MR, Kwak EL, Digumarthy S, Muzikansky A, et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature. 2007;450:1235–1239. doi: 10.1038/nature06385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil JR, Schiemann WP. Altered TAB1:I kappaB kinase interaction promotes transforming growth factor beta-mediated nuclear factor-kappaB activation during breast cancer progression. Cancer Res. 2008;68:1462–1470. doi: 10.1158/0008-5472.CAN-07-3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen DX, Bos PD, Massague J. Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer. 2009;9:274–284. doi: 10.1038/nrc2622. [DOI] [PubMed] [Google Scholar]
- Nieswandt B, Hafner M, Echtenacher B, Mannel DN. Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res. 1999;59:1295–1300. [PubMed] [Google Scholar]
- Oft M, Heider KH, Beug H. TGFbeta signaling is necessary for carcinoma cell invasiveness and metastasis. Curr Biol. 1998;8:1243–1252. doi: 10.1016/s0960-9822(07)00533-7. [DOI] [PubMed] [Google Scholar]
- Oft M, Peli J, Rudaz C, Schwarz H, Beug H, Reichmann E. TGF-beta1 and Ha-Ras collaborate in modulating the phenotypic plasticity and invasiveness of epithelial tumor cells. Genes Dev. 1996;10:2462–2477. doi: 10.1101/gad.10.19.2462. [DOI] [PubMed] [Google Scholar]
- Padua D, Zhang XH, Wang Q, Nadal C, Gerald WL, Gomis RR, Massague J. TGFbeta primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell. 2008;133:66–77. doi: 10.1016/j.cell.2008.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palumbo JS, Talmage KE, Massari JV, La Jeunesse CM, Flick MJ, Kombrinck KW, Jirouskova M, Degen JL. Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood. 2005;105:178–185. doi: 10.1182/blood-2004-06-2272. [DOI] [PubMed] [Google Scholar]
- Park BK, Zhang H, Zeng Q, Dai J, Keller ET, Giordano T, Gu K, Shah V, Pei L, Zarbo RJ, et al. NF-kappaB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat Med. 2007;13:62–69. doi: 10.1038/nm1519. [DOI] [PubMed] [Google Scholar]
- Scheel C, Onder T, Karnoub A, Weinberg RA. Adaptation versus selection: the origins of metastatic behavior. Cancer Res. 2007;67:11476–11479. doi: 10.1158/0008-5472.CAN-07-1653. discussion 11479–11480. [DOI] [PubMed] [Google Scholar]
- Siegel PM, Shu W, Cardiff RD, Muller WJ, Massague J. Transforming growth factor beta signaling impairs Neu-induced mammary tumorigenesis while promoting pulmonary metastasis. Proc Natl Acad Sci U S A. 2003;100:8430–8435. doi: 10.1073/pnas.0932636100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sierko E, Wojtukiewicz MZ. Inhibition of platelet function: does it offer a chance of better cancer progression control? Semin Thromb Hemost. 2007;33:712–721. doi: 10.1055/s-2007-991540. [DOI] [PubMed] [Google Scholar]
- Stern P, Astrof S, Erkeland SJ, Schustak J, Sharp PA, Hynes RO. A system for Cre-regulated RNA interference in vivo. Proc Natl Acad Sci U S A. 2008;105:13895–13900. doi: 10.1073/pnas.0806907105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- Tiedt R, Schomber T, Hao-Shen H, Skoda RC. Pf4-Cre transgenic mice allow the generation of lineage-restricted gene knockouts for studying megakaryocyte and platelet function in vivo. Blood. 2007;109:1503–1506. doi: 10.1182/blood-2006-04-020362. [DOI] [PubMed] [Google Scholar]
- Town T, Breunig JJ, Sarkisian MR, Spilianakis C, Ayoub AE, Liu X, Ferrandino AF, Gallagher AR, Li MO, Rakic P, et al. The stumpy gene is required for mammalian ciliogenesis. Proc Natl Acad Sci U S A. 2008;105:2853–2858. doi: 10.1073/pnas.0712385105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin JJ, Selander K, Chirgwin JM, Dallas M, Grubbs BG, Wieser R, Massague J, Mundy GR, Guise TA. TGF-beta signaling blockade inhibits PTHrP secretion by breast cancer cells and bone metastases development. J Clin Invest. 1999;103:197–206. doi: 10.1172/JCI3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.