Abstract
Persistent fifth aortic arch (PFAA), also known as congenital double-lumen aortic arch, is a rare developmental anomaly of the aortic arch. A 5-month-old baby who presented with congestive cardiac failure was diagnosed to have a large patent ductus arteriosus with PFAA. Although this arch anomaly had no hemodynamic relevance in this case, preoperative diagnosis prevented surprises “on table.”
Keywords: Patent ductus arteriosus, persistent fifth aortic arch, arch anomalies
INTRODUCTION
Persistent fifth aortic arch (PFAA) is thought to be an extremely rare congenital heart disease (CHD). Most of the previous reported cases were associated with major cardiac anomalies and were diagnosed coincidentally.[1] We report a case of PFAA with patent ductus arteriosus (PDA) that caused congestive cardiac failure in a 5-month-old baby.
CASE REPORT
A 5-month-old boy weighing 3500 g presented with history of fast breathing, diaphoresis during feeding and recurrent respiratory tract infections since birth. He was born at 32 weeks of gestation with a birth weight of 2070 g.
Physical examination revealed heart rate of 140 beats per minute, respiratory rate of 60 per minute with subcostal retractions and blood pressure of 80/40 mmHg in the right arm. Oxygen saturation in room air was 95% in the right upper limb and 93% in the lower limb. The peripheral pulses were bounding with no radio-femoral delay. The precordium was hyperdynamic and the apex beat was located in the left fifth intercostal space at the mid-clavicular line. On auscultation, first heart sound was normal and second heart sound was narrowly split with loud pulmonary component. No murmurs were audible.
Chest radiography demonstrated cardiomegaly (cardiothoracic ratio 65%) with right atrium and right ventricle enlargement. Lung fields were plethoric. Electrocardiogram demonstrated biventricular hypertrophy with QRS axis of 90°. Echocardiography revealed a large PDA with predominant right to left shunt and severe pulmonary arterial hypertension. On suprasternal view, the aortic arch was left sided with transverse arch measuring 7 mm. Only two arch vessels were seen, with the first vessel probably trifurcating. Isthmus just after the second vessel measured 4 mm; hence, coarctation was suspected [Figure 1].
Figure 1.

Suprasternal view on two-dimensional echocardiogram showing suspicion of arch anomaly with two lumina arising from the arch
The coarctation segment did not look narrow enough to explain predominant right to left shunting of PDA. To delineate the severity of coarctation and the arch anatomy, cardiac computed tomographic angiography (CT angiography) was planned. CT angiography showed a large left-sided PDA with left aortic arch. The arch had two lumina and the left carotid and subclavian arteries were originating from the upper lumen [Figure 2]. The diagnosis of double-lumen aortic arch was made. There was no coarctation of aorta.
Figure 2.

Three-dimensional reconstructed computed tomography image showing left-sided patent ductus arteriosus with double-lumen aortic arch
Although the PDA seemed to be shunting right to left, the lower limb saturations were 93%. In view of his symptoms and chest X-ray suggestive of increased pulmonary blood flow, he was planned for surgical ligation of PDA. Intraoperatively, CT angiographic findings were confirmed. He underwent successful PDA ligation and was discharged on the seventh postoperative day. On follow-up 3 months later he is doing well with no evidence of pulmonary arterial hypertension.
DISCUSSION
The fifth aortic arch almost always involutes in normal embryological development. PFAA was first reported in man by van Praagh et al. in 1968 as a sizable subway beneath the fourth arch, forming a congenital double-lumen aortic arch. This double lumen extends from the level of the innominate artery proximally to the level of the left subclavian artery and ductus arteriosus distally.[2]
Embryologically, endothelial sprouts arise from the aortic sac and the descending aorta corresponding to the upper-and lower-end of the fifth arch. This fifth arch is inconstant, being found in only 50% of the human embryos at the time of establishment of the six (pulmonary) arches, from the fourth week of development. Although PFAA is a very rare finding, analysis of the records of cardiopathological collections reveals an incidence of approximately 1 in 330.[3] The condition may be underrecognised. PFAA has to be distinguished from a retroesophageal right subclavian artery and from double aortic arch surrounding the tracheoesophageal axis.[4]
PFAA may be hemodynamically inconsequential and is diagnosed coincidentally.[1] This anomaly presents in two forms. With the first type, the fifth aortic arch connects the ascending and descending aorta, running underneath the (fourth) aortic arch from the innominate artery to the left subclavian artery and giving origin to a congenital double-lumen aortic arch [Figure 3]. This systemic-to-systemic connection has no functional relevance and may be associated with various congenital cardiovascular anomalies, the most frequent being aortic coarctation, PDA and bicuspid aortic valve. With the second type, the fifth aortic arch connects the ascending aorta and a derivative of the embryonic sixth arch, forming a systemic-to-pulmonary connection. This situation has usually been described in association with pulmonary atresia and ventricular septal defect. Here, the PFAA is not only an anatomic finding but has an important functional role as a source of blood supply to the lung, and may be misdiagnosed as the arterial duct.[5]
Figure 3.
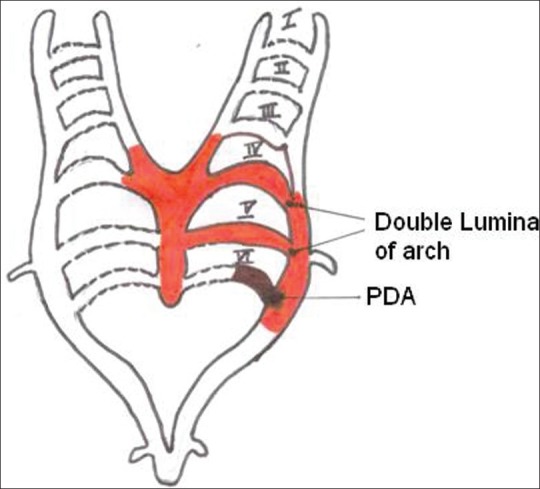
Persistence of left-sided fifth arch with normal arch arising from the fourth branchial arch and patent ductus arising from the distal sixth arch
Most of the previously reported cases were associated with major CHD such as tetralogy of Fallot,[5] truncus arteriosus,[6] coarctation of aorta[4,6] and anomalous origin of left pulmonary artery from ascending aorta.[7] Although frequently associated with major cardiac anomalies, it can also be an incidental finding without any cardiac anomalies.[8,9] The persistent arch can be either left or right sided. There is only one reported case of bilateral involvement.[4] It can rarely present with isolated systemic to pulmonary arterial connection causing severe congestive cardiac failure.[1]
In our case, this PFAA was a systemic-to-systemic connection and both the lumina were patent; hence, there was no functional relevance [Figure 3]. PDA was diagnosed on echocardiography and the arch was suspected to be abnormal. The arch anomaly was confirmed on CT scan. The visualization of great vessels by echocardiography is limited, while cine angiography requires cardiac catheterization with ionizing radiation. Contrast-enhanced magnetic resonance angiography (MRA) and multi-slice CT angiography are noninvasive modalities suitable for visualization of congenital aortic arch anomalies.[10]
This case highlights the importance of arch evaluation on echo in suprasternal view so as to prevent surprises “on table” and modify the surgical management if needed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hwang MS, Chang YS, Chu JJ, Su WJ. Isolated persistent fifth aortic arch with systemic-to-pulmonary arterial connection. J Thorac Cardiovasc Surg. 2003;126:1643–4. doi: 10.1016/s0022-5223(03)00954-1. [DOI] [PubMed] [Google Scholar]
- 2.van Praagh R, van Praagh S. Persistent fifth arterial arch in man: congenital double lumen aortic arch. Am J Cardiol. 1969;24:279–82. doi: 10.1016/0002-9149(69)90417-2. [DOI] [PubMed] [Google Scholar]
- 3.Gerlis LM, Ho SY, Anderson RH, Da Costa P. Persistent 5th aortic arch-a great pretender: Three new covert cases. Int J Cardiol. 1989;23:239–47. doi: 10.1016/0167-5273(89)90253-2. [DOI] [PubMed] [Google Scholar]
- 4.Lambert V, Blaysat G, Sidi D, Lacour-Gayet F. Double-lumen aortic arch by persistence of fifth aortic arch: A new case associated with coarctation. Pediatr Cardiol. 1999;20:167–9. doi: 10.1007/s002469900431. [DOI] [PubMed] [Google Scholar]
- 5.Donti A, Soavi N, Sabbatani P, Picchio FM. Persistent left fifth aortic arch associated with tetralogy of Fallot. Pediatr Cardiol. 1997;18:229–31. doi: 10.1007/s002469900159. [DOI] [PubMed] [Google Scholar]
- 6.Lim C, Kim WH, Kim SC, Lee JY, Kim SJ, Kim YM. Truncus arteriosus with coarctation of persistent fifth aortic arch. Ann Thorac Surg. 2002;74:1702–4. doi: 10.1016/s0003-4975(02)04011-0. [DOI] [PubMed] [Google Scholar]
- 7.Wang JN, Wu JM, Yang YJ. Double-lumen aortic arch with anomalous left pulmonary artery origin from the main pulmonary artery:bilateral persistent fifth aortic arch – a case report. Int J Cardiol. 1999;69:105–8. doi: 10.1016/s0167-5273(99)00011-x. [DOI] [PubMed] [Google Scholar]
- 8.Einzig S, Steelman R, Pyles LA, Balian A, Millman E. Radiological case of the month. Persistent left fifth aortic arch in a child without congenital heart disease. Arch Pediatr Adolesc Med. 1997;151:1259–60. doi: 10.1001/archpedi.1997.02170490085016. [DOI] [PubMed] [Google Scholar]
- 9.Park HJ, Oh JM, Park SE, Nam SO, Kim CW, Kim KI. Isolated persistent fifth aortic arch in a patient with cornelia de lange syndrome. Pediatr Cardiol. 2005;26:112–4. doi: 10.1007/s00246-004-9012-5. [DOI] [PubMed] [Google Scholar]
- 10.Zhong Y, Jaffe RB, Zhu M, Sun A, Li Y, Gao W. Contrast-enhanced magnetic resonance angiography of persistent fifth aortic arch in children. Pediatr Radiol. 2007;37:256–63. doi: 10.1007/s00247-006-0385-x. [DOI] [PubMed] [Google Scholar]


