Abstract
Diabetes mellitus has reached epidemic proportions and continues to be a major burden on society globally. The International Diabetes Federation (IDF) estimated the global burden of diabetes to be 366 million in 2011 and predicted that by 2030 this will have risen to 552 million. In spite of newer and effective treatment options, newer delivery and diagnostic devices, stricter glycaemic targets, better treatment guidelines and increased awareness of the disease, baseline glycosylated hemoglobin remains relatively high in subjects diagnosed and treated with type 2 diabetes. The search continues for an ideal anti diabetic drug that will not only normalize blood glucose but also provide beta cell rest and possibly restoration of beta cell function. The development of anti diabetic drugs is riddled with fundamental challenges. The concept of beta cell rest and restoration is yet to be completely understood and proven on a long term. The ideal therapeutic approach to treating type 2 diabetes is not yet determined. Our understanding of drug safety in early clinical development is primarily limited to “Type A” reactions. Until marketing authorization most drugs are approved based on the principle of confirming non-inferiority with an existing gold standard or determining superiority to a placebo. The need to obtain robust pharmaco-economic data prior to marketing authorization in order to determine appropriate pricing of a new drug remains a major challenge. The present review outlines some of the challenges in drug development of anti-diabetic drugs citing examples of pulmonary insulin, insulin analogues, thiazolidinediones and the GLP1 analogues.
Keywords: Anti diabetic drugs, drug development, GLP1 analogues, insulin analogues, pulmonary insulin, type 2 diabetes mellitus
INTRODUCTION
While India emerges as a strong and sustainable developing economy it continues to grapple with the dual burden of communicable and non communicable diseases. Amongst the long list of non communicable diseases the burden of type 2 diabetes mellitus has grown disproportionately in India over the last two decades. King H, et al.; in 2004 made a shocking prediction that the overall global burden of diabetes mellitus was estimated to be 366 million by 2030.[1] India was stated to be the major contributor to this global burden in the year 2000 with an estimated number of adult diabetics to be 31.7 million. The predicted number of diabetics in India over the next three decades was estimated to reach 80 million adults. Unless something dramatic was done at the individual, family and societal level the global burden of diabetes were likely to reach or exceed the predictions made by King H, et al.
Late last year the Diabetes Atlas of the IDF published an article on the overall burden of Diabetes.[2] Paradoxically and rather alarmingly the global prevalence of diabetes had reached the predicted target of 366 million by 2011! It stated that by 2030 this number would have risen to 552 million. India has and will continue to be a major contributor to the overall burden of diabetes globally. The diabetes epidemic can be curtailed and possibly reversed if we incorporate a culture of healthier eating and regular exercise in our society. For subjects with diabetes mellitus optimal use of existing therapeutic options and the search for newer more effective and safer therapies will go a long way in reducing the complications of diabetes thereby reducing morbidity and overall mortality. The present review outlines some of the major challenges faced by researchers in developing drugs for diabetes mellitus.
Diabetes mellitus
Lab to clinic to market!
While our understanding of the patho-physiology of diabetes has grown significantly, gaps in our knowledge still exist. The concept of β-cell rest and restoration has been much discussed over the last several decades but the concept has yet to be proven. Several short to medium term studies have demonstrated the possibility of beta-cell rest but long term studies have yet to emerge to prove this concept.[3] The drug or treatment modality that permits long-term β cell rest (if such a scientific concept is proven) is likely to be the mainstay of therapy for type 2 diabetes.
Although metformin has emerged as the ideal choice of starting treatment in type 2 diabetes, the optimal therapeutic approach over time is yet to be determined. This question can only be answered by conducting long term studies using different therapeutic options and to determine their impact on hard clinical endpoints i.e.; long term diabetic complications, mortality.
Given our limited understanding of drug safety particularly early in development have resulted in a large number of anti-diabetic drugs that have fallen by the way-side in its lifecycle. Typical examples of these being Phenformin, Troglitazone, Rosiglitazone, pulmonary insulin, etc;
An unusual paradox exists in our attempt to develop new drugs today. In order to achieve regulatory approvals globally studies are designed to either compare or confirm non-inferiority to the existing gold-standard or superiority to the placebo. While this approach generally permits regulatory approvals if the primary objective is met, data obtained however promising does limit the pharmaco-economic evaluation of the drug.
Landmark studies like the Diabetes Control and Complications Trial (DCCT)[4] and United Kingdom Prospective Diabetes Study (UKPDS)[5] have determined the need for good glycaemic control to minimize or delay the onset of late diabetic complications. New and effective treatment options, newer insulin delivery and self monitored blood glucose devices, stricter glycaemic targets and guidelines[6] and the “treat to target” approach has helped some patients achieving the target of normoglycaemia.[7] However for the vast majority of patients glycaemic levels continue to be relatively high before and after treatment in spite of rather efficient blood glucose lowering.[8]
Given the magnitude of the problem diabetes will have on society and in spite of the existing limitations of various anti-diabetic medications, the anti-diabetic therapeutic class has emerged within the top 4 contributors in global pharmaceutical sales.[9]
Challenges in diabetes drug development
The story of inhaled insulin
One of the greatest milestones in the history of medicine was the discovery of injectable insulin in the early 1920's. A few years after this discovery, an early publication on inhaled insulin appeared in a German journal in 1925.[10] It took over 80 years to “prove the concept” that inhaled insulin could possibly replace injectable insulin as an alternative and more convenient route of administration. All through these several decades of research, several issues on pulmonary insulin did arise i.e.; long term safety, rising titer's of antibodies, diminished lung function in some patients, use of short acting human insulin (when in most countries globally the starter insulin was a long acting or premixed insulin), need for at least one injection of a long acting insulin (to support the basal bolus concept), low bioavailability (less than 10%), high costs and limited to no insurance coverage.[11] In addition insulin pen devices with micro fine needles made insulin delivery almost painless and therefore did not justify the cost of pulmonary insulin. The first pulmonary insulin i.e.; Exubera® therefore emerged in the US market in 2006 only to be withdrawn in 2007.[12] Following the failure of Exubera® all other pharmaceutical companies developing pulmonary insulin decided to stop development of their pulmonary insulin projects with the exception of Afreeza® (MannKind Inc). Based on recent reports it appears that Afreeza® is also caught up in the difficult web of developing pulmonary insulin.[13]
“Perception versus reality”: The story of the once versus twice daily basal insulin analogues
Two long acting insulin analogues exist in the world market today i.e; insulin glargine and insulin detemir. Both insulin glargine and insulin detemir were developed on the principle of a once daily basal insulin analogue that could serve as both an ideal start to insulin therapy for those type 2 diabetes subjects who were inadequately controlled on two or more oral hypoglycaemic agents and in type 1 diabetes as part of a basal bolus regimen. The approach to development of these two analogues was however different. Insulin glargine entire clinical development program was built on the sole platform of once daily insulin. Insulin detemir on the other hand was developed on the primary platform of once daily insulin with the flexibility of using it twice daily for those patients needing a twice daily injection. The scientific basis for permitting the twice daily injection option for insulin detemir was built on two important scientific facts. Firstly in a quarter to a third of diabetic patients receiving either insulin detemir or glargine required a second injection on the same day as it was not possible to optimize glycaemic control with a once daily injection.[14] Moreover, conventional wisdom on the use of NPH insulin over several decades dictated the need to have the option for a once or twice a day basal insulin. Several studies comparing the PK and PD profiles of glargine and detemir have found these two insulins’ similar and therefore have a similar duration of action.[15] Strangely even today many physicians still perceive insulin glargine as a “once daily insulin” and insulin detemir a “twice daily insulin” rather than the flexible option of a “once and/or twice daily insulin”.
Can short and long acting insulin analogues be mixed prior to administration?
During the development of the long acting insulin analogues it was clinically meaningful to explore the possibility of self mixing it with the short acting analogues i.e.; aspart, lispro and glulisine prior to administration. This self mixing process could potentially optimize the proportion of short and long acting insulin administered and reduce the number of injections which would therefore be significantly beneficial in children and the elderly.
However, based on outcome on clinical studies it is now recommended not to mix insulin glargine or insulin detemir with any other insulin or solution. If insulin glargine or insulin detemir is diluted or mixed, the pharmacokinetic or pharmacodynamic profile i.e; onset of action and time to peak effect of insulin glargine and insulin detemir and the mixed insulin may be altered in an unpredictable manner.[16,17]
GLP1 analogues
Will they revolutionize the way we treat type 2 diabetes today?
One of the most promising therapeutic classes of anti diabetic that has emerged in the last few years is the GLP1 analogues i.e.; Exenitide and Liraglutide. The mechanism of action is unique for this class of drugs as they target multiple sites that affect the patho-physiology of type 2 diabetes.[18] Given the beneficial effects it has on glycaemic control, minimal risk of hypoglycaemia and potential benefit on body weight this class is likely to be the mainstay of therapy in type 2 diabetes. Liraglutide is also likely to emerge as a major drug in the treatment of obesity in the next few years.[19]
The GLP1 analogues have not escaped the challenges of drug safety. The ability of these drugs to stimulate calcitonin release and consequently enhance calcitonin synthesis, induce hyperplasia and possibly neoplasia in rodents resulted in a major safety signal being raised during drug development. Further studies in primates confirmed that this phenomenon was unique in rodents and not in primates like monkey or man.[20] This was because GLP1 receptors were predominant in rodents and not so in primates.
A few cases of acute pancreatitis have been observed in subjects exposed to the GLP1 analogues during clinical development. As part of the Risk Evaluation and Mitigation strategies (REMS), a medication guide is required to be dispensed with each liraglutide prescription to inform providers and patients about the risk of acute pancreatitis and the potential risk of medullary thyroid carcinoma. Should this signal be negative drugs emerging in this therapeutic class are likely to be major blockbusters in the years to come.
The rise and fall of the Thiozolindiones (TZD's)
The TZD's entered the world market with the blockbuster prototype Troglitazone. The class was considered unique because of its’ novel mechanism of action and its ability to address the problem of insulin resistance. In spite of an extensive development program Troglitazone lasted in the world market for only a few years before the association of Troglitazone use and severe liver disease sometimes resulting in death was determined.[21] The frequency of severe liver disease with Troglitazone use was identified as 1 in 10,000 and therefore not identified during routine clinical development.
Rosiglitazone faced the same fate only several years after its launch globally due to the occurrence of increased cardiovascular events with its use and was associated with a significantly increased risk of heart attack (odds ratio = 1.43, (95% confidence interval, 1.03 to 1.98; P = 0.03)), and an even higher risk of death from all cardiovascular diseases (odds ratio = 1.64)[22] eventually leading to the withdrawal of Rosiglitazone from the world market. The association of Pioglitazone and bladder cancer[23] has probably put the “nail in the coffin” for this entire therapeutic class of drugs.
Back to basics
Table 1 below outlines some of the major pharmacokinetic (PK) reasons for failure of anti diabetic medications.
Table 1.
Major pharmacokinetic reasons for failure of anti diabetic medications
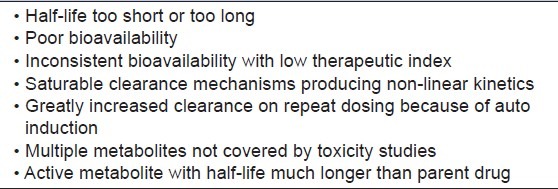
Identifying these PK shortcomings early in the drug development process, will go a long way in killing projects early and help save significant time, money and effort within organizations developing anti diabetic drugs.
Late development strategies
As the safety information is accrued at a slower rate than for efficacy, one could consider taking more than one dose into phase III. In this case, a decision to discontinue one of the arms can be made at an interim analysis during the confirmatory stage when more safety data are available.
Another approach would be to combine phase IIb and phase III in one adaptive design trial, with a more robust phase IIb stage.
We understand that it is equally important to review the data from the trials to make sure efficacy and non-cardiac safety are also being met. Thus a balance must be struck between conducting short term early phase trials with longer early phases trials.
CONCLUSION
Developing anti diabetic drugs is not without challenges. However, having a robust drug development process with stringent “Go-No Go” decisions will go a long way in terminating projects early or bringing superior drugs in the market. Novel drugs having multiple sites of action and positively targeting several elements of the metabolic syndrome are likely to be the drugs of the future in type 2 diabetics. Insulin analogues that mimic physiological insulin secretion, that are convenient to administer in state of the art delivery devices are likely to be the insulin's of the future for both type 1 and type 2 diabetes. As our understanding of drug safety increases and with the incorporation of robust risk management plans in our projects the future is likely to see safer and more effective therapeutic options to treat subjects with diabetes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.IDF Diabetes Atlas. 5th edn. Brussels, Belgium: International Diabetes Federation; 2011. International Diabetes Federation. [PubMed] [Google Scholar]
- 3.Meier JJ. Beta cell mass in diabetes: A realistic therapeutic target? Diabetologia. 2008;51:703–13. doi: 10.1007/s00125-008-0936-9. [DOI] [PubMed] [Google Scholar]
- 4.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 6.American Diabetes Association. Executive Summary: Standards of Medical Care in Diabetes-2012. [Last accessed on 2012 Mar 13];Diabetes Care. 2012 35(Suppl 1):S4–S10. doi: 10.2337/dc12-s004. Available from: http://care.diabetesjournals.org/content/35/Supplement_1/S4.full.pdf+html . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, Keenan JF, et al. 4-T Study Group. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–47. doi: 10.1056/NEJMoa0905479. [DOI] [PubMed] [Google Scholar]
- 8.Sharma SK, Joshi SR, Vaz JA, Kumar A, Unnikrishnan AG, Hoskote SS, et al. PRESENT Study Group. Efficacy, safety and acceptability of biphasic insulin aspart 30 in Indian patients with type 2 diabetes: Results from the PRESENT study. J Assoc Physicians India. 2008;56:859–63. [PubMed] [Google Scholar]
- 9.Sales of anti-diabetics 2010. IMS Health Midas. 2010 [Google Scholar]
- 10.Klinische Wochenschrift 4. Jahrgang Nr.2. 1925 Jan 8; [Google Scholar]
- 11.Wadher K, Kalsait R, Umekar M. Pulmonary insulin delivery: Challenges and current status. Journal of Pharmaceutical Sciences and Research. 2011. [Last accessed on 2012 Mar 12]. Available from: http://readperiodicals.com/201102/2279502051.html .
- 12.Siekmeier R, Scheuch G. Diabetes treatment by inhalation of insulin - shine and decline of a novel type of therapy. In: Esquinas AM, editor. Applied technologies in Pulmonary Medicine. Basel: Karger; 2011. pp. 77–83. [Google Scholar]
- 13.MannKind says FDA wants two new clinical trials of its insulin inhaler. January 19, 2011|By Nathan Olivarez-Giles, Los Angeles Times. [Last accessed on 2012 Mar 12]. Available from: http://articles.latimes.com/2011/jan/19/business/la-fi-mannkind-diabetes-20110119 .
- 14.Clement S, Bowen-Wright H. Twenty-four hour action of insulin glargine (Lantus) may be too short for once-daily dosing: A case report. Diabetes Care. 2002;25:1479–80. doi: 10.2337/diacare.25.8.1479-a. [DOI] [PubMed] [Google Scholar]
- 15.Klein O, Lynge J, Endahl L, Damholt B, Nosek L, Heise T. Albumin-bound basal insulin analogues (insulin detemir and NN344): Comparable time-action profiles but less variability than insulin glargine in type 2 diabetes. Diabetes Obes Metab. 2007;9:290–9. doi: 10.1111/j.1463-1326.2006.00685.x. [DOI] [PubMed] [Google Scholar]
- 16.Prescribing Information-Insulin Detemir. [Last accessed on 2012 Mar 12]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021536s029lbl.pdf .
- 17.Prescribing Information – Insulin Glargine. [Last accessed on 2012 Mar 12]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021081s034lbl.pdf .
- 18.Drucker DJ, Sherman SI, Gorelick FS, Bergenstal RM, Sherwin RS, Buse JB. Incretin-based therapies for the treatment of type 2 diabetes: Evaluation of the risks and benefits. Diabetes Care. 2010;33:428–33. doi: 10.2337/dc09-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simonyi G, Pados G, Medvegy M, Bedros JR. [The pharmacological treatment of obesity: Past, present and future] Orv Hetil. 2012;153:363–73. doi: 10.1556/OH.2012.29317. [DOI] [PubMed] [Google Scholar]
- 20.Liraglutide PB. Drug monograph, June 2010. [Last accessed on 2012 Mar 13]. Available from: http://www.pbm.va.gov/Clinical%20Guidance/Drug%20Monographs/Liraglutide%20monograph.pdf .
- 21.Henney JE. Withdrawal of troglitazone and cisapride. JAMA. 2000;283:2228. [Google Scholar]
- 22.Nissen SE, Wolski K. “Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes”. N Engl J Med. 2007;356:2457–71. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 23.Hillaire-Buys D, Faillie JL, Montastruc JL. Pioglitazone and bladder cancer. Lancet. 2011;378:1543–4. doi: 10.1016/S0140-6736(11)61662-0. [DOI] [PubMed] [Google Scholar]


