Abstract
The ability of short injection duration of contrast material to reduce the total injection volume in 64-detector row CT coronary angiography was investigated. 45 patients were divided into three groups: (i) those receiving 0.8 ml kg–1 of contrast material (350 mgI ml–1) injected with a fixed duration of 14 s (Group A; n _ 16); (ii) those receiving 0.8 ml kg–1 of contrast material injected with a fixed duration of 10 s (Group B; n _ 15); and (iii) those receiving 0.7 ml kg–1 of contrast material injected with a fixed duration of 10 s (Group C; n _ 14). All patients then received 20 ml of saline. Contrast densities of the ascending aorta and proximal and distal coronary arteries were assessed where vessel diameters were >2.0 mm. The mean enhancement value in the ascending aorta for Group B was significantly higher than that for Groups A and C (p<0.05), whereas there was no significant difference between Groups A and C. All enhancement values in the coronary arteries were higher than 250 Hounsfield units. The mean enhancement value for each coronary artery in Group B was significantly higher than that for Group A (p<0.05), whereas there was no significant difference between Groups A and C. In conclusion, a short injection duration allows a reduction in the total volume of contrast material from 0.8 ml kg–1 to 0.7 ml kg–1 while a steady contrast enhancement is maintained in the ascending aorta and coronary arteries.
CT coronary angiography has become a standard tool for the non-invasive assessment of coronary arteries in the past few years [1–4]. In particular, the improved spatial and temporal resolution and short data acquisition period of 64-detector row CT has led to a further improvement in image quality [5].
In CT coronary angiography, high and consistent vascular enhancement is a prerequisite for sufficient evaluation [6–9]. As the coronary arteries are branches of the ascending aorta, enhancement of the ascending aorta plays a major role in the enhancement of the coronary arteries. Recently, it has been reported that aortic enhancement is closely related to injection duration when the contrast material dose is determined according to patient weight, and that a shorter injection duration contributes to higher aortic enhancement [10, 11]. To our knowledge, only a few studies have evaluated the optimal dose of contrast material on the basis of patient weight for a steady vessel enhancement in coronary CT examinations [9]. The purpose of this study is to investigate, on the basis of patient weight, whether it is possible to decrease the total injection volume of contrast material by shortening injection duration while maintaining adequate coronary vessel enhancement in 64-detector row CT coronary angiography.
Methods and materials
Patients
This study was performed according to the principles of the Declaration of Helsinki and approved by our institutional review board. Informed consent was obtained from all patients before the CT examination. Patients were recruited from June 2007 to August 2007. Initially, 52 patients who were scheduled to undergo 64-detector row CT coronary angiography were recruited consecutively in this study. Patients who had a previous allergic reaction to iodinated contrast material, renal failure (serum creatinine level >1.2 mg dl–1), respiratory failure, congestive heart failure or an inability to achieve a heart rate below 70 beats per minute with the use of metoprolol, as well as women who were potentially pregnant, were excluded. Patients were referred with typical angina pectoris (n _ 9), atypical chest pain (n _ 12), dyspnoea (n _ 7), high cardiovascular risk factors without specific symptoms (n _ 9) and after percutaneous coronary interventions (n _ 15). However, patients who were classified as non-evaluable owing to motion artefacts (n _ 2) or severe calcifications (n _ 5) were excluded.
The final study group consisted of 45 patients (27 men, 18 women) who were 40–85 years old (mean, 69.0 years) and weighed 43–68 kg (mean, 56.3 kg). Of these patients, nine had significant coronary artery stenosis (lumen obstruction of ≥50%) and two had previously implanted coronary artery stents. The patients were divided randomly into three groups using a table of random numbers and received either 0.8 ml kg–1 of contrast material injected with a fixed duration of 14 s (Group A; n _ 16), 0.8 ml kg–1 of contrast material injected with a fixed duration of 10 s (Group B; n _ 15) or 0.7 ml kg–1 of contrast material injected with a fixed duration of 10 s (Group C; n _ 14); all patients then received 20 ml of 0.9% saline solution at the same flow rate as the contrast material. All patients received non-ionic contrast material (Iomeprol, Iomeron (350 mgI ml–1); Eisai, Tokyo, Japan).
CT scanning
The CT scanner was a 64-detecter row CT Aquilion multiscanner (Toshiba Corporation Medical Systems, Tokyo, Japan). Patients with a pre-scanning heart rate of 65 beats per minute or higher were given 20–60 mg of metoprolol (Selokeen; AstraZeneca, Zoetermeer, Netherlands) orally 1 h before scanning. Using a dual-shot injector (Nemoto Kyorindo, Tokyo, Japan), the contrast material and saline solution were injected through a 20-gauge intravenous injection catheter (Termo, Tokyo, Japan) inserted into the antecubital vein. The scanning parameters were: a collimation of 64 × 0.5 mm, a voltage of 135 kV, a tube current of 360–530 mA, a helical pitch of 8.0–12.0 and a rotation time of 0.35 s or 0.40 s (depending on the heart rate). Each patient's electrocardiogram was digitised and monitored continuously during image acquisition.
The scanning delay was set with an automated bolus-tracking technology (Real Prep technique; Toshiba Corporation Medical Systems, Tokyo, Japan) [9]. As soon as the single density level in the ascending aorta enhanced to 150 Hounsfield units (HU) over the baseline, the patient was instructed to take a deep breath and hold it. 4 s after triggering, contrast-enhanced CT scanning was performed from the tracheal bifurcation to the bottom of the heart (∼120 mm).
For evaluation of the coronary arteries, data were reconstructed by using a segmented reconstruction algorithm at 75% of the R–R interval with a section thickness of 0.5 mm and a reconstruction interval of 0.3 mm. If motion artefacts were still present in this phase, additional reconstruction was explored to obtain the reconstruction phase with the fewest motion artefacts. For this purpose, images were reconstructed throughout the R–R interval every 20 ms at the midlevel of the heart, and the image with the fewest motion artefacts among all of the reconstructed images was chosen to analyse the coronary arteries. The reconstructed image data were transferred to a computer workstation (M900 Quadra; Ziosoft, Tokyo, Japan) for post-processing.
Methods of evaluation
Two observers (F.T. and G.N., with five years and three years of experience in cardiovascular radiology, respectively) who were blind to the injection technique independently collected all of the measurements at the workstation. The mean enhancement value of both observers was calculated for further evaluation. To assess intraobserver variability, one observer (F.T.) re-reviewed 25 randomly selected cases after eight months had elapsed since the first interpretation.
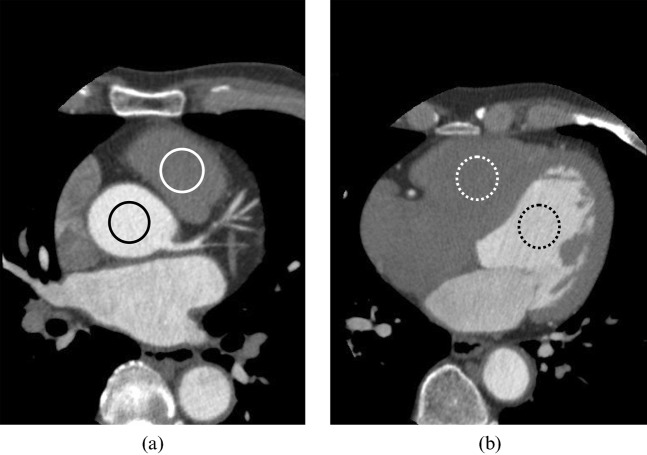
Enhancement values for the ascending aorta and right ventricular outflow tract were measured using a circular region of interest (ROI) cursor at the level of the left main artery branches from the ascending aorta (Figure 1a), and those for the left and right ventricle were measured at the level of the largest diameter of the heart in the transverse images (Figure 1b). The results of each measurement were averaged and compared among the three groups.
Figure 1.
(a,b) Enhancement values for the ascending aorta (black line), right ventricular outflow tract (white line), right ventricle (dotted white line) and left ventricle (dotted black line) were measured using a circular region of interest cursor.
Enhancement values for the proximal and distal coronary arteries, where vessel diameters were ≥2.0 mm, were then measured using a ROI cursor [6]. The enhancement values were measured at the foot of each arterial segment of the right coronary artery (segments 1 and 3), left main artery (segment 5), left anterior descending artery (segments 6 and 8) and left circumflex artery (segments 11 and 13) [9] according to the classification of the American Heart Association. ROIs were plotted on cross-sectional images of these segments in which the lumen was easily identified (Figure 2). Calcifications, coronary artery stents and soft plaques were carefully excluded from the ROI measurements. The measurements for each coronary artery were averaged and compared among the three groups.
Figure 2.
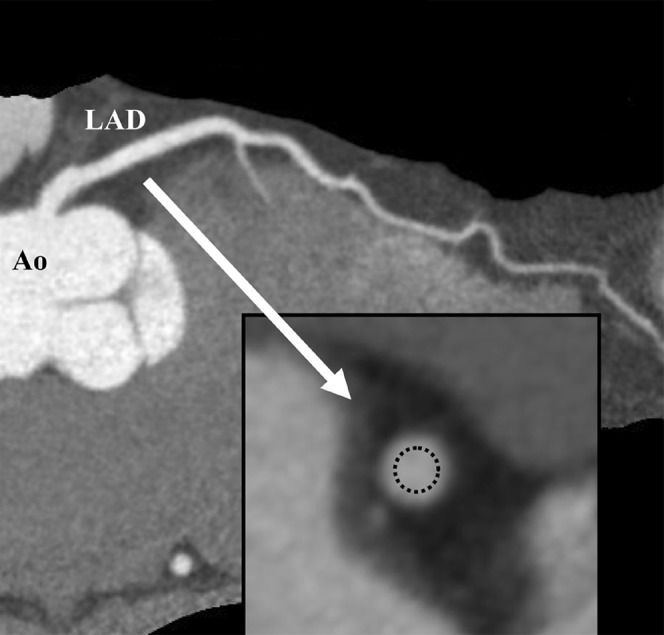
Enhancement values for each coronary artery segment were measured on the cross-sectional images using a circular region of interest cursor (dotted line). Ao, aorta; LAD, left anterior descending artery.
Statistical analyses
The age, body weight, heart rate during acquisition of CT scans and data acquisition time of patients were compared among the three groups with a one-way analysis of variance (ANOVA). The quantitative results for the three groups were compared using the Kruskal–Wallis test, and pairwise comparisons of groups were performed using the Mann–Whitney U test. Intra- and interobserver variability for CT measurements were assessed with Bland–Altman analysis. All data were expressed as the mean ± SD (standard deviation); differences were considered to be statistically significant at p<0.05.
Results
There were no statistically significant differences in age, body weight, mean heart rate during acquisition of CT scans or mean data acquisition time among the three groups (p>0.05) (Table 1). The mean total dose of contrast material was 46.5±5.25 ml in Group A, 44.3±4.71 ml in Group B and 39.3±5.41 ml in Group C. The mean flow rate was 3.3±0.37 ml s–1 in Group A, 4.4±0.48 ml s–1 in Group B and 4.0±0.55 ml s–1 in Group C. The mean enhancement values in the ascending aorta, right ventricular outflow tract and right and left ventricles are shown in Table 2; the numbers of coronary arteries assessed for enhancement values and the mean enhancement value in each coronary artery are shown in Table 3 and illustrated in Figure 3.
Table 1. Patient characteristics.
| Group A | Group B | Group C | ANOVA | |
| Age (years) | 68.2±10.6 | 69.1±10.3 | 69.6±9.6 | p _ 0.90 |
| Body weight (kg) | 57.4±6.0 | 55.3±5.9 | 56.2±7.8 | p _ 0.70 |
| Heart rate (beats per min) | 53.8±7.6 | 55.7±7.7 | 59.0±12.2 | p _ 0.46 |
| Data acquisition time (s) | 10.4±0.9 | 10.4±1.1 | 10.1±1.4 | p _ 0.48 |
Data are the mean ± standard deviation. ANOVA, analysis of variance.
Table 2. The mean enhancement values (Hounsfield units) for the ascending aorta, left ventricle, right ventricular outflow tract and right ventricle.
| Ascending aorta | Left ventricle | Right ventricular outflow tract | Right ventricle | |
| Group A | 362.1±66.9 | 347.5±63.8 | 217.0±107.9 | 103.0±34.2 |
| Group B | 427.9±47.5 | 340.7±77.6 | 127.5±54.9 | 73.1±20.0 |
| Group C | 391.0±46.6 | 278.2±63.1 | 100.3±23.7 | 74.4±10.1 |
| A vs B | p<0.05 | p _ 0.79 | p<0.05 | p<0.01 |
| B vs C | p<0.05 | p<0.05 | p _ 0.06 | p _ 0.31 |
| A vs C | p _ 0.73 | p<0.01 | p<0.01 | p<0.01 |
Data are the mean ± standard deviation.
Table 3. The mean enhancement values (Hounsfield units) for each coronary artery segment.
| RCA |
LM |
LAD |
LCX |
||||
| 1 (n _ 45) | 3 (n _ 40) | 5 (n _ 45) | 6 (n _ 45) | 8 (n _ 35) | 11 (n _ 43) | 13 (n _ 39) | |
| Group A | 332.5±47.8 | 310.3±36.6 | 332.4±63.3 | 310.6±48.4 | 286.3±33.4 | 304.5±45.5 | 274.8±34.8 |
| Group B | 369.2±57.6 | 342.9±40.5 | 380.5±45.3 | 362.0±36.8 | 314.8±27.6 | 345.8±42.8 | 324.7±48.4 |
| Group C | 338.1±44.4 | 294.5±36.7 | 362.8±46.8 | 332.1±34.8 | 295.9±41.9 | 339.2±53.4 | 306.2±42.8 |
| A vs B | p<0.05 | p<0.05 | p<0.05 | p<0.01 | p<0.05 | p<0.05 | p<0.01 |
| B vs C | p _ 0.13 | p<0.01 | p _ 0.21 | p _ 0.06 | p _ 0.07 | p _ 0.77 | p _ 0.38 |
| A vs C | p _ 0.90 | p _ 0.15 | p _ 0.56 | p _ 0.11 | p _ 0.47 | p _ 0.08 | p _ 0.09 |
Data are the mean ± standard deviation. n _ number of segments assessed for enhancement values. RCA, right coronary artery; LM, left main artery; LAD, left anterior descending artery; LCX, left circumflex artery.
Figure 3.
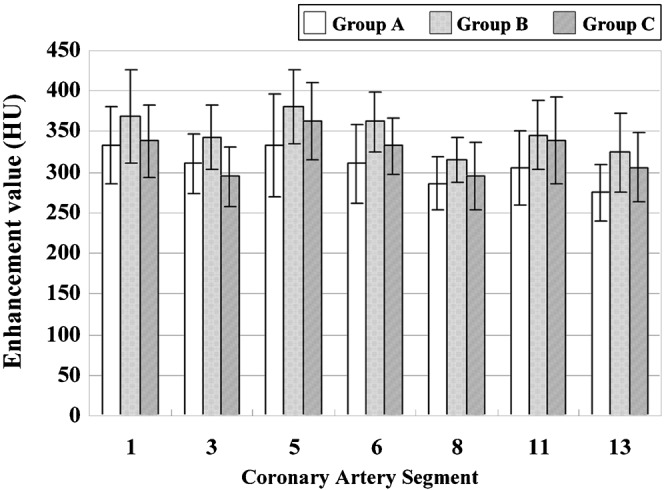
The mean enhancement values for each coronary artery segment.
The mean enhancement value in the ascending aorta for Group B was significantly higher than that for Groups A and C (Group A vs Group B, p<0.05; Group B vs Group C, p<0.05), whereas there was no significant difference between Groups A and C (p _ 0.73). The mean enhancement value in the left ventricle for Groups A and B was significantly higher than that for Group C (Group A vs Group C, p<0.01; Group B vs Group C, p<0.05), whereas there was no significant difference between Groups A and B (p _ 0.79).
The mean enhancement value in the right ventricular outflow tract for Group A was significantly higher than that for Groups B and C (Group A vs Group B, p<0.05; Group A vs Group C, p<0.01), whereas there was no significant difference between Groups B and C (p _ 0.06). Similar results were found for the mean enhancement value in the right ventricle (Group A vs Group B, p<0.01; Group A vs Group C, p<0.01; Group B vs Group C, p _ 0.31).
All enhancement values in the coronary arteries were higher than 250 HU. The mean enhancement value in each coronary artery for Group B was significantly higher than that for Group A, whereas there was no significant difference between Groups A and C.
Bland–Altman limits of agreement for intraobserver variability were –23.4 HU to 24.6 HU, with a mean difference of 0.6 HU, and those for interobserver variability were –30.5 HU to 32.8 HU, with a mean difference of 1.2 HU.
Discussion
CT coronary angiography has become the standard method for non-invasive assessment of coronary arteries in the past few years [1–4]. In 64-detecter row CT, the short scanning time allows a decreased breath-hold time and lower dose of applied contrast material [9, 12], in addition to improved spatial and temporal resolution. To achieve the desired high vascular enhancement, a high concentration of non-ionic contrast material, e.g. 350–400 mgI ml–1, should be injected with a fast injection rate of 3.5–5 ml s–1 [7–9]. However, the optimal dose of contrast material for 64-detector row CT coronary angiography remains a subject of controversy.
The coronary arteries are branches of the ascending aorta, so that the enhancement of the ascending aorta plays a major role in the enhancement of the coronary arteries. It is reported that aortic enhancement is closely related to injection duration when the contrast material dose is determined according to patient weight, and a shorter injection duration contributes to higher aortic enhancement [10, 11]. Yamamuro et al [9] reported that the enhancement of coronary arteries also depends on the total injection volume per kilogram of body weight. Indeed, comparing the two groups using 0.8 ml kg–1 of contrast material in this study showed that the mean enhancement values in both the ascending aorta and the coronary arteries increased significantly when the contrast material was injected with the shorter injection duration (10 s).
In CT coronary angiography, high and consistent vascular enhancement is a prerequisite for sufficient evaluation [6–9], and an optimal enhancement value in the coronary arteries is considered to be >250–350 HU [9, 13]. In this study, 0.7 ml kg–1 or 0.8 ml kg–1 of contrast material was injected with a fast injection rate (2.8–5.4 ml s–1; mean, 3.89 ml s–1) and all enhancement values for the coronary arteries whose vessel diameter was ≥2.0 mm measured >250 HU. In the report by Yamamuro et al [9], an injection volume of at least 0.9 ml kg–1 of contrast material was necessary to achieve a contrast enhancement >250 HU in every coronary artery [9]. In that study, the contrast material and saline solution were administered at a rate of 2.8–3.5 ml s–1 using three injection phases. However, this injection rate seems too slow for evaluating coronary artery enhancement.
It is necessary to reduce the total injection volume of contrast material for patients with congestive heart failure or renal impairment, especially when the impairment is due to diabetic nephropathy [14], in order to lower the risk of contrast material-induced nephropathy [15]. In this study, there were no significant differences in the mean enhancement value in the ascending aorta and coronary arteries among groups using 0.8 ml kg–1 of contrast material with a long injection duration (14 s) and 0.7 ml kg–1 of contrast material with a short injection duration (10 s). This indicates that a short injection duration allows a reduction in the total volume of contrast material from 0.8 ml kg–1 to 0.7 ml kg–1 for the assessment of coronary arteries. As a result, there was a 15.5% reduction in the total volume of contrast material from 46.5 ml (0.8 ml kg–1) to 39.3 ml (0.7 ml kg–1) in this study. Therefore, in these patients, short injection duration of contrast material is recommended to reduce the total injection volume of contrast material.
In this study, almost no contrast material remained in the right ventricular outflow tract or right ventricle in the two groups using shorter contrast material injection durations. By using short injection durations, it was considered that the occurrence of streak artefacts from dense contrast material in the right ventricle, which interfere with the evaluation of the right coronary artery [8], could be reduced. However, in those cases with a right ventricular tumour or thrombo-emboli manifestation, or when a functional analysis of the right ventricle is needed, it is necessary to have contrast enhancement present in the right ventricle. Therefore, in such cases, a biphasic or triphasic injection protocol could be useful for improving right ventricle visualisation [8].
This study has some potential limitations. Firstly, the mean body weight of patients examined in this study is smaller than those of American and European subjects. Therefore, further studies are required to see whether our results apply to heavier patients. Secondly, the patients who had congestive heart failure or were unable to achieve a heart rate below 70 beats per minute with the use of metoprolol were excluded from this study. However, these patients represent an important subset who are referred for CT coronary angiography in clinical practice. The data for patients with such conditions might be different from results obtained in this study.
In conclusion, short injection duration allows a reduction in the total volume of contrast material from 0.8 ml kg–1 to 0.7 ml kg–1 while a steady contrast enhancement is maintained in the ascending aorta and coronary arteries.
References
- 1.Achenbach S, Giesler T, Ropers D, Ulzheimer S, Derlien H, Schulte C, et al. Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation 2001;103:2535–8 [DOI] [PubMed] [Google Scholar]
- 2.Nieman K, Oudkerk M, Rensing BJ, van Ooijen P, Munne A, van Geuns RJ, et al. Coronary angiography with multi-slice computed tomography. Lancet 2001;357:599–603 [DOI] [PubMed] [Google Scholar]
- 3.Beck T, Burgstahler C, Kuettner A, Kopp AF, Heuschmid M, Claussen CD, et al. Clinical use of multislice spiral computed tomography in 210 highly preselected patients: experience with 4 and 16 slice technology. Heart 2005;91:1423–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bley TA, Ghanem NA, Foell D, Uhl M, Geibel A, Bode C, et al. Computed tomography coronary angiography with 370-millisecond gantry rotation time: evaluation of the best image reconstruction interval. J Comput Assist Tomogr 2005;29:1–5 [DOI] [PubMed] [Google Scholar]
- 5.Nikolaou K, Flohr T, Knez A, Rist C, Wintersperger B, Johnson T, et al. Advances in cardiac CT imaging: 64-slice scanner. Int Journal Cardiovascular Imaging 2004;20:535–40 [DOI] [PubMed] [Google Scholar]
- 6.Cademartiri F, Mollet NR, Lemos PA, Saia F, Midiri M, de Feyter PJ, et al. Higher intracoronary attenuation improves diagnostic accuracy in MDCT coronary angiography. AJR Am J Roentgenol 2006;187:W430–3 [DOI] [PubMed] [Google Scholar]
- 7.Cademartiri F, Mollet NR, van derLugt A, McFadden EP, Stijnen T, de Feyter PJ, et al. Intravenous contrast material administration at helical 16-detector row CT coronary angiography: effect of iodine concentration on vascular attenuation. Radiology 2005;236:661–5 [DOI] [PubMed] [Google Scholar]
- 8.Schoepf UJ, Zwerner PL, Savino G, Herzog C, Kerl JM, Costello P. Coronary CT angiography. Radiology 2007;244:48–63 [DOI] [PubMed] [Google Scholar]
- 9.Yamamuro M, Tadamura E, Kanao S, Wu YW, Tambara K, Komeda M, et al. Coronary angiography by 64-detector row computed tomography using low dose of contrast material with saline chaser: influence of total injection volume on vessel attenuation. J Comput Assist Tomogr 2007;31:272–80 [DOI] [PubMed] [Google Scholar]
- 10.Awai K, Hiraishi K, Hori S. Effect of contrast material injection duration and rate on aortic peak time and peak enhancement at dynamic CT involving injection protocol with dose tailored to patient weight. Radiology 2004;230:142–50 [DOI] [PubMed] [Google Scholar]
- 11.Ichikawa T, Erturk SM, Araki T. Multiphasic contrast-enhanced multidetector-row CT of liver: contrast-enhancement theory and practical scan protocol with a combination of fixed injection duration and patients' body- weight-tailored dose of contrast material. Eur J Radiol 2006;58:165–76 [DOI] [PubMed] [Google Scholar]
- 12.Wintersperger BJ, Nikolaou K. Basics of cardiac MDCT: techniques and contrast application. Eur Radiol 2005;15:B2–9 [DOI] [PubMed] [Google Scholar]
- 13.Becker CR, Hong C, Knez A, Leber A, Bruening R, Schoepf UJ, et al. Optimal contrast application for cardiac 4-detector-row computed tomography. Invest Radiol 2003;38:690–4 [DOI] [PubMed] [Google Scholar]
- 14.Parfrey PS, Griffiths SM, Barrett BJ, Paul MD, Genge M, Withers J, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med 1989;320:143–9 [DOI] [PubMed] [Google Scholar]
- 15.Solomon R. Contrast media nephropathy—how to diagnose and how to prevent? Nephrol Dial Transplant 2007;22:1812–5 [DOI] [PubMed] [Google Scholar]